Translate this page into:
Addressing Obstetrical Challenges at 12 Rural Ugandan Health Facilities: Findings from an International Ultrasound and Skills Development Training for Midwives in Uganda
*Corresponding author email: ckinnevey@gmail.com
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Background:
Like much of Sub-Saharan Africa, Uganda is facing significant maternal and fetal health challenges. Despite the fact that the majority of the Uganda population is rural and the major obstetrical care provider is the midwife, there is a lack of data in the literature regarding rural health facilities’ and midwives’ knowledge of ultrasound technology and perspectives on important maternal health issues such as deficiencies in prenatal services.
Methodology:
A survey of the current antenatal diagnostic and management capabilities of midwives at 12 rural Ugandan health facilities was performed as part of an international program initiated to provide ultrasound machines and formal training in their use to midwives at antenatal care clinics.
Results:
The survey revealed that the majority of pregnant women attend less than the recommended minimum of four antenatal care visits. There were significant knowledge deficits in many prenatal conditions that require ultrasound for early diagnosis, such as placenta previa and macrosomia. The cost of providing ultrasound machines and formal training to 12 midwives was $6,888 per powered rural health facility and $8,288 for non-powered rural health facilities in which solar power was required to maintain ultrasound.
Conclusions and Global Health Implications:
In order to more successfully meet Millennium Development Goal 4 (reduce child mortality), 5 (improve maternal health) and 6 (combat HIV) through decreasing maternal to child transmission of HIV, the primary healthcare provider, which is the midwife in Uganda, must be competent at the diagnosis and management of a wide spectrum of obstetrical challenges. A trained ultrasound-based approach to obstetrical care is a cost effective method to take on these goals.
Keywords
Ultrasound
Uganda
Maternal Health
Fetal Health
Rural
Sub-Saharan Africa
Antenatal Care
Introduction
Uganda, like much of Sub-Saharan Africa, is facing critical maternal and fetal health challenges. According to the 2011 Uganda Health Assessment, the Ugandan infant mortality rate is 76 infant deaths per 1,000 live births, which is over 10 times the infant mortality rate as the United States.[1,2] According to the 2012-13 State of Uganda Children Report, Uganda’s maternal mortality ratio is 438 per 100,000 live births, which is one of the highest rates in the world.[3]
The lack of antenatal care (ANC) is a contributing factor to Uganda’s maternal and fetal health challenges. It is estimated that 6% of Ugandan women receive no antenatal care and the majority (68%) of women receive less than the World Health Organization (WHO) recommended four antenatal care visits.[1] In fact, the minority (39%) of Ugandan women deliver at health facilities.[1] While the problem is severe in the country of Uganda as a whole, it is even worse in rural areas because of additional barriers faced in rural areas including the cost and reliability of transportation,[4,5] inadequate nutritional education,[6] long wait times caused by high patient volumes,[5] and lack of imaging capabilities in rural areas.[7]
According to the 2011 Ugandan Health Assessment, 84% of women receive their antenatal care from midwives.[1] Since midwives comprise the majority of the antenatal care providers, there is compelling reason to seek their perspectives in facing Uganda’s critical maternal and fetal health challenges. Despite the rich first-hand knowledge of the field conditions of the rural Ugandan midwives, the rural Ugandan midwives perspectives are not represented in the literature. The purpose of this paper was five-fold: 1) to assess the perspectives of rural Ugandan clinics on current barriers to antenatal care (ANC); 2) identify deficiencies in prenatal services and anticipated new demands with the addition of ultrasound; 3) to assess rural Ugandan midwives’ perspectives on the perceived challenges they would face by adding ultrasound to their health facilities and identifying knowledge deficiencies in the management of prenatal conditions primarily diagnosed with ultrasound; and 4) to conduct a cost analysis for ultrasound training and equipping of midwives at rural Ugandan health facilities.
Methods
Subjects
This study included a prospective survey of 12 midwives at 12 rural Ugandan health facilities that provide antenatal care at 11 districts in Uganda including Kanungu, Kampala, Manafwa, Wakiso, Rukungiri, Lira, Bugiri, Arua, Kisoro, Kabale, and Nebbi (Figure 1). Two of the facilities were level IV and the remaining 10 facilities were level III facilities. According to the Ugandan Health Sector Strategic Plan,[8] a Health Center IV is the county-level health facility that employs a physician and is equipped with an operating theatre and blood transfusion services. A Health Center III is a sub-county level health facility, which is run by mid-level providers and offers basic maternity services and diagnostic services.
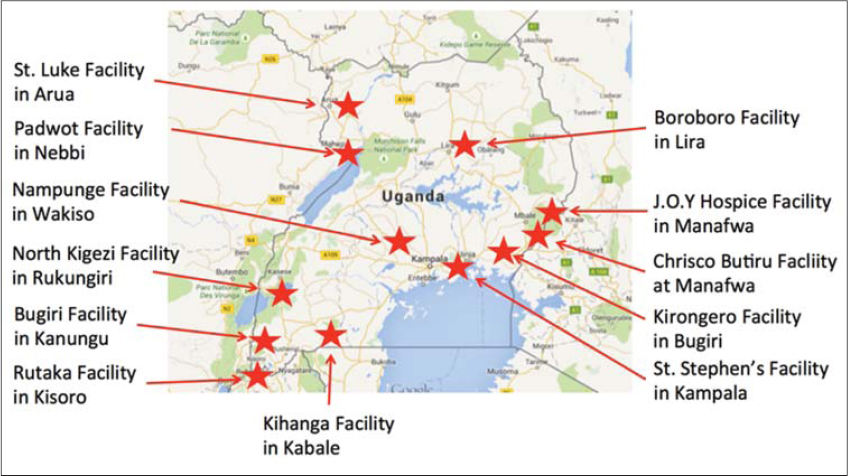
- Location of 12 clinics where ultrasound machines were donated and midwives were recruited and trained
Procedures
The Uganda Protestant Medical Bureau (UPMB) has worked with a 501(c)(3) Non-Profit organization called Rad Impact and arranged for equipping of ultrasound at 12 UPMB clinics. The 12 UPMB health facilities were selected based on three criteria: being in a rural area; not having ultrasound access; and having low antenatal care (ANC) rates relative to other UPMB health facilities. One midwife from each clinic volunteered to complete a 6-week obstetrical ultrasound educational course taught by Radiologists and certified radiology technicians at the Ernest Cook Ultrasound Research and Education Institute (ECUREI) in Kampala, Uganda in January 2016. The training curriculum included ultrasound physics, normal maternal and fetal anatomy and pathology, report writing, image archiving, equipment maintenance, and patient communication skills.
A self-assessment survey developed by the research team was administered to 12 midwives on the first day of their ultrasound training at ECUREI in January 2016. The survey assessed the midwives’ average responses using rating scale of 1 to 3. In the understanding of diagnosis and clinical significance, scores were as follows: 1 represented “I do not know what this diagnosis is”; 2 represented “I have a limited understanding”; 3 represented “I am very knowledgeable.” Similarly, in the comfort level in managing the diagnosis, scores were as follows: 1 represented “not at all comfortable”; 2 represented “somewhat comfortable; 3 represented “very comfortable.” The survey responses were anonymous and primarily consisted of questions regarding the midwives’ practices with the majority of the questions centered on their practice parameters and capabilities in diagnosis and management of a variety of prenatal conditions.
The cost estimate for the use of ultrasound technology in rural areas was calculated as the sum of the ultrasound equipment including shipping and import tax fees plus the midwives’ ultrasound training fees including tuition, transportation, and room and board. Given that five of the 12 health facilities were solar powered, additional costs were incurred for providing additional solar panels. The ultrasound equipment was selected and tested for suitability for limited obstetrical ultrasound by the team.
Statistical analysis
The descriptive statistics of frequency and percentage were used to report the following variables of interest: years in practice as midwife; years in midwifery training; whether the midwife assisted with vaginal deliveries; number of ANC visits per day; gestational age at first ANC visit; number of ANC visits during pregnancy; OB consultation referrals; C-Section referral number prior to and during active labor; and number of HIV patients seen per month. The descriptive statistics of mean with 95% confidence intervals were used to reports on midwives’ self-assessment on the diagnosis and management of eleven obstetrical diagnoses.
Ethical approval
Our study included survey data obtained from 12 midwives at 12 rural UPMB health facilities. This study was performed with two indigenous authors. An IRB did not exist in this rural setting at UPMB facilities; however, this survey research falls under the IRB exemption category 2 of Section 46.101 b of the Office of Human Research Protections Code of Federal Regulations in the United States. The midwives voluntarily completed the survey and there was no monetary compensation in accordance with ethical practice.
Results
All 12 midwives completed the survey on the first day of their ultrasound training course. The 12 midwives completed their clinical training at 10 different programs across Uganda. All 12 midwives see patients for antenatal appointments. All the midwives reported that all HIV positive pregnant women received anti-retrovirals (ARVs) provided free of charge to the patients. None of the midwives had ever received obstetrical ultrasound training as part of their curriculum. Further questionnaire results are reported in Table 1. The second portion of the survey included a knowledge assessment of the diagnosis and comfort level in managing 11 prenatal diagnoses primarily made with ultrasound as shown in Figure 2.
| Demographic variable | Frequency | Percentage |
|---|---|---|
| Years in practice as midwife | N=12 | |
| 0-5 | 10 | 83 |
| 6-10 | 1 | 8.3 |
| 11-15 | 1 | 8.3 |
| Years of midwifery training | N=12 | |
| < 2.5 | 1 | 8.3 |
| 2.5-3 | 9 | 75 |
| >3 | 2 | 1.7 |
| Assist with vaginal deliveries? | N=12 | |
| Yes | 11 | 91.7 |
| No | 1 | 8.3 |
| Women seen at ANC per day | N=12 | |
| 1-5 | 7 | 58.3 |
| 6-15 | 3 | 25 |
| 16-30 | 2 | 1.7 |
| Gestational age at first ANC visit (weeks) | N=12 | |
| 15-19 | 5 | 41.7 |
| 20-22 | 6 | 50 |
| 23-28 | 1 | 8.3 |
| ANC visits attended in pregnancy | N=12 | |
| 1-2 | 4 | 33.3 |
| 3 | 3 | 25 |
| 4 | 5 | 41.7 |
| OB consultation referrals per month | N=12 | |
| 0-2 | 5 | 41.7 |
| 3-5 | 6 | 50 |
| >5 | 1 | 8.3 |
| CSection referrals during active labor | N=11 | |
| 0-2 | 6 | 54.5 |
| 3-4 | 3 | 27.3 |
| >5 | 2 | 18.2 |
| CSection referrals prior to labor | N=11 | |
| 0-2 | 9 | 81.8 |
| 3-4 | 2 | 18.2 |
| >5 | 0 | 0 |
| HIV+patients seen per month | N=12 | |
| 0-2 | 4 | 33.3 |
| 3-5 | 3 | 25 |
| >6 | 5 | 41.7 |
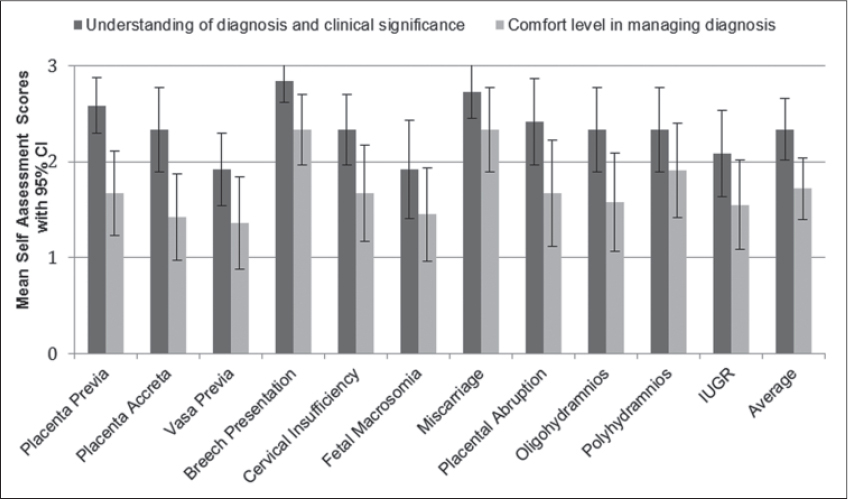
- Midwives’ Self-Assessment. Response averages of 12 midwives using rating scale of 1 to 3.
Cost analysis
A portable ultrasound machine (Mindray DP-10; Shenzhen, China),[9] which costs $3,219 USD/unit, was selected by the team. The cost of the education was $3,669 per midwife. Thus, the total cost of implementing ultrasound equipment and training a midwife at a rural health facility in Uganda was $6,888. The solar panels selected were the JLR 500 Watt Solar Generator system, which was an additional $1,400 per unit. Rad Impact, who funded this project, worked with Rad Connect, LLC who provided free telecommunication service so the midwives can consult with experts.
Discussion
The 12 midwives at the rural Ugandan health facilities in this study reported managing over 6,700 ANC visits and performing over 2,100 deliveries annually. Their referral rate to a physician was only 3.2%. This underscores the fact that the midwives are primarily managing their patients[1] and emphasizes the importance of gaining their in-the-field perspectives on obstetrical challenges in rural Uganda.
The rural midwives’ self assessment of clinical management skills demonstrated scores ranging between “not at all comfortable” to “somewhat comfortable” in 9 of 11 (81.8%) selected diagnoses despite their mean 2.5 years of education and an additional 2.5 years of experience in the field. This is attributable to the lack of ultrasound training in their practices. Ultrasound is generally required to diagnoze all 11 conditions surveyed and has many other uses, including dating the pregnancy, second trimester fetal screening, and in labor and delivery, to predict whether vaginal delivery will be successful.[10-12] The utility of ultrasound is key in timely diagnosis, which allows for labor management preparation, delivery route planning, and early appropriate referral of certain conditions, especially those that might otherwise be fatal. According to the data, fetal macrosomia was one of the least understood diagnoses among the midwives in the study. However, according to recent literature, diabetes and obesity in women of reproductive age is increasing in developing countries, including Uganda, leading to a rise in macrosomic births and adverse birth outcomes.[13] Antenatal ultrasound diagnosis of macrosomia and attendance at delivery by a midwife who is prepared for potential shoulder dystocia could dramatically decrease the morbidity and mortality of such deliveries.
With respect to the critical issue of antenatal care attendance rates, 7 out of 12 (58%) of the midwives reported that women typically attended less than the recommended four ANC visits, which is similar to published ANC rates in the literature[1] and highlights the fact that low ANC attendance is still a problem in rural areas. In addition to the major barrier to ANC attendance of lack of transportation,[4, 5] lack of ultrasound is also a barrier to women seeking ANC services. This has been substantiated in prior studies which suggested that technology increases trust in the care provided and husbands were even more likely to accompany their wives to visits in order to see the scan.[13,14] The midwives reported caring for an average of 9.8 HIV positive patients per month and the increase in ANC attendance that might result with the addition of ultrasound technology, may potentially help ensure appropriate treatment to decrease maternal child HIV transmission.
Additionally, it has been shown that ultrasound implementation at antenatal visits increases the referral rate to obstetricians who can provide care for higher risk pregnancies, in one study, as high as a 41% rate.[15] If applied to the statistics provided by the midwives, this would mean an average of an additional 2-3 obstetrics referrals per midwife per month. The need for increased human resources is also supported by the 2006 World Health Report, which estimated that an additional 1.5 million health care workers would be needed in Africa to meet the health care demands.[16] In fact, 36 out of the 46 countries in Africa were identified as having a “critical shortage” of doctors, nurses and midwives.[16]
Conclusions and Global Health Implications
Improvement of ANC rates and diagnostic capabilities through ultrasound will contribute toward reaching the Millennium Development Goal 4, 5 and 6 of reducing childhood mortality, improving maternal health and reducing maternal to child transmission of HIV.[17] This study highlights the lack of ultrasound as a significant barrier in the obstetrical care of patients in rural Uganda. The midwives’ self-assessment revealed a complete absence of ultrasound training in midwifery education and significant knowledge deficits in the management of prenatal conditions primarily diagnosed with ultrasound. This information prompted that the midwives who were to receive ultrasound machines at their clinics not only receive extensive formal ultrasound training, but also a “Field Guide” with concise information on the key management points for each condition mentioned in the survey. Additionally, a team of five United States physicians is planning to travel to Uganda in January 2017 to teach Advanced Life Support in Obstetrics (ALSO) and Helping Babies Survive (HBS) courses to the 12 midwives. During that time, it is planned that the midwives will receive refresher training in the use of the ultrasound machines. Follow-up of this cohort of health facilities and midwives should be performed to assess the impact on ANC attendance rates, maternal and fetal mortality rates. This project of equipping health facilities with ultrasound machines and training midwives on obstetrical ultrasound use is a cost effective way to significantly improve maternal and child health in Uganda and perhaps other similar regions. With continued availability of funding and success, Rad Impact will continue to facilitate the distribution of more ultrasound machines and annual training of more midwives to improve care for both pregnant women and their babies.
Acknowledgement
The authors thank the midwives working in rural Uganda who provided the information used for this study. Additionally, Fred Kirumira should be acknowledged for his extensive help in the distribution and collection of the surveys. Finally, the authors thank the American Academy of Family Medicine Emerging Leaders Institute, the Uganda Protestant Medical Bureau and the Ernest Cook Ultrasound Research and Education Institute for their support in this project.
Conflict of Interest: None.
Ethical Consideration:: This study was performed independently and impartially under ethical practice with integrity in research, voluntary midwife participation and anonymity of individual midwives’ responses. Additional details provided in the ethical approval section.
References
- 2011. Uganda Health System Assessment 2011.
- M.S. International Comparisons of Infant Mortality and Related Factors: United States and Europe, 2010. Center for Disease Control, Editor 2010
- [Google Scholar]
- The State of Uganda Population Report 2013. Minister of State for Finance Planning and Economic Development, Editor. 2013
- [Google Scholar]
- Can she make it? Transportation Barriers to Accessing Maternal and Child Health Care Services in Rural Ghana. BioMed Central Health Services Research. 2015;15:333.
- [Google Scholar]
- Barriers to Health Care in Rural Mozambique: A Rapid Ethnographic Assessment of Planned Mobile Health Clinics for ART. Global Health, Science and Practice. 2015;3(1):109-116.
- [Google Scholar]
- Barriers to Infant and Child-feeding Practices: A Qualitative Study of Primary Caregivers in Rural Uganda. Journal of Health, Population, and Nutrition. 2015;33(1):106-116.
- [Google Scholar]
- Training for Rural Radiology and Imaging in Sub-Saharan Africa: Addressing the Mismatch Between Services and Population. Journal of Clinical Imaging Science. 2012;2:37.
- [Google Scholar]
- 2015. Mindray Medical International. DP-10 Ultrasound System [Internet]. Available from: http://www.mindray.com/en/products/DP-10-NEW.html?series=General%20Imaging
- Should Second Trimester Ultrasound be Routine for All Pregnancies? Seminars in Perinatology. 2013;37(5):323-326.
- [Google Scholar]
- Ultrasound for Fetal Assessment in Early Pregnancy. The Cochrane Database of Systematic Reviews. 2015;7:CD007058.
- [Google Scholar]
- Macrosomia in 23 Developing Countries: An Analysis of a Multicountry, Facility-based, Cross-sectional Survey. Lancet. 2013;381(9865):476-483.
- [Google Scholar]
- A Low-Cost Ultrasound Program Leads to Increased Antenatal Clinic Visits and Attended Deliveries at a Health Care Clinic in Rural Uganda. PLoS One. 2013;8(10):e78450.
- [Google Scholar]
- Impact of Introducing Routine Antenatal Ultrasound Services on Reproductive Health Indicators in Mpigi District, Central Uganda. Ultrasound Quarterly. 2015;31(4):285-289.
- [Google Scholar]
- The World Health Report 2006: Working Together for Health. Education for Health. 2006;19(3):385-387.
- [Google Scholar]
- 2015. Millennium Development Goals and Beyond. Available from: http://www.un.org/millenniumgoals/bkgd.shtml





