Translate this page into:
Maternal Mortality in the Main Referral Hospital in Angola, 2010-2014: Understanding the Context for Maternal Deaths Amidst Poor Documentation
*Correspondence author: ausadiq@yahoo.com
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Background:
Increasing global health efforts have focused on preventing pregnancy-related maternal deaths, but the factors that contribute to maternal deaths in specific high-burden nations are poorly understood. The aim of this study was to identify factors that influence the occurrence of maternal deaths in a regional maternity hospital in Kuando Kubango province of Angola.
Methods:
The study was a retrospective cross-sectional analysis of case notes of all maternal deaths and deliveries that were recorded from 2010 to 2014. The information collected included data on pregnancy, labor and post-natal period retrieved from case notes and the delivery register.
Results:
During the period under study, a total of 7,158 live births were conducted out of which 131 resulted in maternal death with an overall maternal mortality ratio of 1,830 per 100,000 live births. The causes of death and their importance was relatively similar over the period reviewed. The direct obstetric causes accounted for 51% of all deaths. The major causes were hemorrhage (15%), puerperal sepsis (13%), eclampsia (11%) and ruptured uterus (10%). In addition, indirect non-obstetric medical causes such as Malaria, Anemia, hepatitis, AIDs and cardiovascular diseases accounted for 49% of all maternal deaths. There is poor documentation of personal data and clinical case management of cases. The factors of mutual instability of statistical significance associated with maternal death are: place of domicile (P=0.0001) and distance to the hospital (P=0.0001).
Conclusion and Global Health Implication:
The study demonstrated that the MMR in maternity hospital is very high and is higher than the WHO 2014 estimates and the province is yet to achieve the desired MDG 5 target by the end of 2015. A reversal of the present state requires data driven planning in order to improve access and use of Maternal Health Services (MHS) and ultimately lower the number of pregnancy-related maternal deaths.
Keywords
Maternal Mortality
Causes
Determinants
Poor Documentation
Angola
Introduction
Childbirth, even though a normal physiological process has been associated with a number of risks, which may, in extreme cases, lead to loss of life. This concern was underscored by the Millennium Development Goal 5 (MDG) which focused on improving maternal health services (MHS) to reduce morbidity, disability, and mortality due to pregnancy and delivery. Worldwide, it has been estimated that 289,000 cases of maternal deaths were recorded in 2013, indicating a raising trend by 2000 deaths compared to the figure obtained in 2011, with 99 % of these deaths occurring in the developing countries.[1,2]
Although it is the wealthiest nation in the central African sub-region, with an impressive economic growth since the end of the country’s civil war in 2002, the Republic of Angola has a higher life time risk of 1 in 39 women dying as a result of pregnancy and its related complications compared to neighboring Republic of Namibia with a life time risk of 1 in 160.[3] The current Maternal Mortality Ratio (MMR) for Angola[1] was reported to be 460 per 100,000 live births in 2013, which is still far above the desired MDG 5 goal of 300 per 100,000 live births by the year 2015.[4] The high MMR (460 per 100,000 live births) is partly due to low utilization of maternal health services.[1] For instance, between 2006-2013, only 47% and 49% of pregnant women had at least four ante natal care visits as recommended by the World Health Organization (WHO) and delivered under the supervision of a skilled health worker respectively.[1] More disturbing is the fact that only 32% of rural pregnant women were reported to have had their delivery supervised by a skilled health worker compared to 82% of their urban cohort.[5] Hence, there exists wide disparities between the rural and urban populations of Angola. This scenario is further worsened by the fact that many pregnancies end up as stillbirths or neonatal deaths.
One of the major reasons for sub-Saharan African countries having the highest life time risk of dying due to pregnancy related issues and poor pregnancy outcomes such as still births and neonatal deaths is lack of systematic search for the root causes of these deaths as being done in the industrialized countries where confidential inquiries is the norm rather than an exception.[6] Unfortunately, the findings of these confidential inquiries in the developed countries are used to set out downstream public health intervention strategies in the developing nations notwithstanding their small sample sizes (pregnancy related deaths are rare event in Europe and North America) and differences in terms of socio-economic, cultural and political systems including health care financing mechanisms between the developed and the underdeveloped countries. Concerns about the lack of use of area-specific data have been referred to as “inverse information and care law.” [6] This concern is legitimate in terms of the need for the utilization of local information in order to come up with the root causes that lead to poor utilization of maternal and child care services, which will subsequently guide local interventions at provincial/state and district levels. Unfortunately, there is a lack of Angolan based studies on maternal health status. For instance, of the 2,500 articles on maternal mortality reviewed by Gil-González and colleagues,[7] and another 5,575 articles on maternal health services utilization and pregnancy outcomes reviewed by Say and Raine,[8] and 54 articles on the effectiveness of interventions on maternal mortality in low income countries reviewed by Burchette and Mayhew,[9] there was no single article from the Republic of Angola despite the country’s high MMR of 460 per 100,000 live birth,[1] and a life time risk of a woman dying from pregnancy and its related complications over 1000 times higher when compared to Canada and Scandinavian countries.[3] This dearth of data on MHS utilization and maternal mortality in Angola and many other high burden countries was further reported to have neither timely nor complete data on maternal deaths surveillance system.[10] Surveillance for maternal mortality was launched in 2004 with the aim not just to estimate the burden of the problem but, also to provide better insights on the why, how and where these deaths occur. Nearly, a third of all districts in sub-Saharan Africa have not integrated maternal mortality among the immediate notifiable events/diseases in their Integrated Disease Surveillance and Response (IDSR) program. [11] Furthermore, a review of the status of maternal mortality surveillance in 2012 showed that data on maternal deaths are lacking or incomplete in 48.9% of the 180 countries reviewed including Angola.[12] A recent review on status of implementation of maternal death surveillance and response among African countries has shown that the Republic of Angola was among the countries with no available data on Maternal Death Surveillance and Response.[13] The country still relies on traditional non-electric surveillance information tools that focus on clinical causes of maternal deaths such as hemorrhage, ruptured uterus, sepsis, eclampsia etc., which does not provide insights on what transpired at home, on the way to health facility and appropriateness of treatment received.[13] These issues indicate the need for area specific studies in order to complement the weak surveillance system and also to guide interventions that are in context of the local issues which forms the objective of this study.
Independent autonomous decision making on reproductive health desires of women in many developing countries is defined not only by a woman’s level of education or personal income but also by the norms in her community as dictated by cultural and religious beliefs.[14,15] In order to identify the underlying root causes of utilization behavior and how they impact pregnancy outcomes, the Anderson medical care utilization model was used as the theoretical framework of this study. [16] The model is made up of three constructs namely: 1) the predisposing characteristics of women such as biological, cultural, social, and economic; 2) the enabling characteristics such as health system and health care financing mechanisms; and 3) the need characteristics which is the individual pregnant woman’s perceived need to use modern health services and the perceptions of the health care worker.[17] The constructs of the model are highly adaptable attested by its application in numerous research studies. This unique characteristic of the Anderson’s model was underscored by its use in various health.[18-20] and other social issues.[21-23]
We examined the associations between women’s bio-socio demographic and health system characteristic (independent variables) and pregnancy outcome (mother is dead or alive) as the outcome/dependent variables. This study will bridge the existing current gap of evidence-based information noted above and highlight areas that require further research in order to come up with interventions that are specific to local context in Angola and in other sub-Saharan African countries.
Methodology
Study area
Kuando Kubango is one of the 18 provinces of Angola, situated in the southern part of the country. It has a common international boundary with the Republic of Namibia to the South and the Republic of Zambia to the southeast. It also shares local boundaries with Moxico province to the North east, Bie to the north, Huila and Cunene provinces to the West. It has an estimated population of 510, 369 with 60% living in urban areas based on the 2014 census.[24] It has a total of 102 health facilities out of which 10 provided obstetric services. The population of women in the reproductive age group is 104,342 with an estimated annual number of pregnancies of 24,843 based on the 2014 census. [24] This study was conducted in the main regional referral center due to the availability of better skilled workers and diagnostic services in this center. All hospitals have a functional ambulance to facilitate the transfer of cases to the provincial maternity hospital. Subsistence farming, petty trading, fishing, and hunting are the main occupations of the indigenes.
Study population
The target population of this study was women that received obstetric services (antenatal, delivery or post-natal) in the provincial main referral maternity hospital Menongue, Kuando Kubango Province of Angola, between 2010 and 2014.
Study design
The study is a retrospective study using information from obstetric case notes. It is basically the analysis of data on pregnancy, labor and puerperium from patient case notes and the delivery register for a period of five years (2010-2014). Only maternal deaths that meet the World Health Organization’s (WHO) definition of maternal mortality were included in the study. According to WHO maternal mortality is “the death of any woman while pregnant or within 42 days of termination of pregnancy, from any cause related to or aggravated by pregnancy or its management, irrespective of the duration and site of the pregnancy, but not from accidental or incidental causes.”[10] No sampling method was adopted since all cases within the study period were analyzed.
The data collection instruments were case files kept in the medical records department, labor ward (delivery) register, and a form designed to keep records for data extracted from each case file. The tool documented data on personal, and clinical information such as age, tribe, religion, marital status, place of domicile, parity, occupation of husband, occupation of cases, mode of admission (self or referred), booking status, indication for admission, date of admission, duration of labor, interval between onset of labor and admission to hospital, place of delivery (as indicated in the referral letter or case notes), previous obstetric operations, interval between admission and maternal death, cause of maternal death and date of death.
Data analysis
Maternal mortality ratio was calculated for each of the five years (2010-2014) and for the overall study period. The causes of death were examined under two heading viz: direct obstetric causes and indirect non obstetric medical causes. Cross tabulations of variables, where feasible, were done. The chi square test of association and Fisher Exact test were conducted with the level of statistical significance set at p<0.05 at 95% confidence interval.
Results
During the period under study (2010-2014), 131 maternal deaths were recorded, out of 7,158 live births, giving a maternal mortality ratio (MMR) of 1830 per 100,000 deliveries. The annual and overall maternal mortality ratio The denominator of the former (ratio) is live births while the later (rate) is women in the reproductive age group 15-49 years. In this study we used live births as the denominator to calculate the annual and overall mortality ratio is shown in Table 1.
| Year | Live births | Maternal deaths | MMR/100000 Live births |
|---|---|---|---|
| 2010 | 1691 | 24 | 1419 |
| 2011 | 948 | 18 | 1899 |
| 2012 | 1166 | 29 | 2487 |
| 2013 | 1873 | 34 | 1815 |
| 2014 | 1480 | 26 | 1757 |
| Overall (2010-2014) | 7158 | 131 | 1830 |
The peak incidence of MMR was recorded in 2012 with MMR of 2,487 per 100,000 live births (Figure 1). The overall trend although decreasing between 2013 and 2014, however, the 2014 MMR of 1,757 per 100,000 live births is still higher than the figure of 1,360 per 100,000 live births recorded in 2010 (Figure 1).
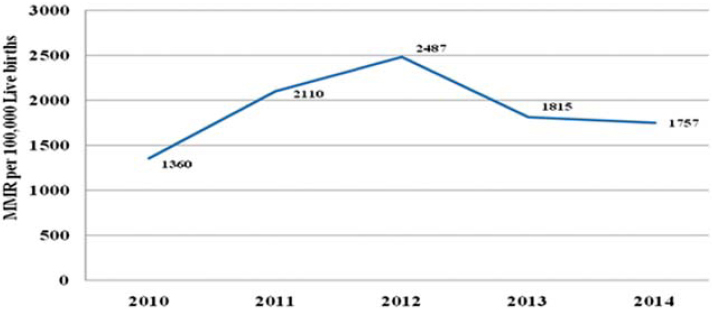
- Trend of MMR per 100,000 live births, 2010 - 2014, Menongue, Kuando Kubango Province
Out of the 131 maternal deaths, 31 (24%) of these cases had inadequate documentation on working diagnosis, presenting complain, history of presenting complain and or management outline and therefore were not included in analysis of direct and indirect causes of maternal death. Of the remaining 100 deaths that had information on diagnoses, 51 (51%) and 49 (49%) were as a result of direct and indirect causes respectively (Table 2). The three leading direct causes of maternal deaths are hemorrhage (15%), puerperal sepsis (13%) and eclampsia (11%) which combined accounted for 39% of all deaths (Table 2).
| Cause of death | Total Maternal deaths (N=100) | % |
|---|---|---|
| Direct obstetric causes of deaths (n=51) | ||
| Hemorrhage | 15 | 15 |
| Puerperal sepsis | 13 | 13 |
| Eclampsia | 11 | 11 |
| Ruptured uterus | 10 | 10 |
| Abortion | 1 | 1 |
| Ectopic pregnancy | 1 | 1 |
| Indirect non-obstetric causes of deaths (n=49) | ||
| Malaria | 14 | 14 |
| Anemia | 13 | 13 |
| Pneumonia | 5 | 5 |
| Cardiovascular diseases | 4 | 4 |
| Hepatitis | 4 | 4 |
| AIDS | 3 | 3 |
| Liver cirrhosis | 1 | 1 |
| Pulmonary Tuberculosis | 1 | 1 |
| Renal failure | 1 | 1 |
| Chriocarcinoma | 1 | 1 |
| Drug over dose | 1 | 1 |
| Steven Johson Syndrome | 1 | 1 |
Indirect non-obstetric medical causes, accounted for 49% of all maternal deaths. Malaria in pregnancy (14%), anemic heart failure (13%) and pneumonia (5%) were the leading cause of indirect non obstetric medical causes of maternal death, accounting for 32% of all deaths (Table 2).
The age distribution of maternal deaths indicated that more than half of all deaths were accounted by women between the ages of 15-19 and those > 35 years with Age Specific MMR (ASMMR) of 1,058 and 1,354 per 100,000 live births respectively. Women between the ages of 20-34 years had the lowest ASMMR of 876 per 100,000 live births. However, the difference is not statistically significant (χ2=4.572; df 2; P>0.05) (Table 3).
| Independent variable | Pregnancy outcome (N=12,705) | Bivariate analysis Chi Square | |
|---|---|---|---|
| Safe deliveries | Maternal deaths | ||
| n=12573 | n=131 | ||
| Age in years | |||
| <20 | 4023 | 50 | p=0.1016 |
| 20 – 34 | 7239 | 63 | |
| 35 – 49 | 1311 | 18 | |
| Place of domicile* | |||
| Rural | 5394 | 126 | p=0.0001 |
| Urban | 7179 | 5 | |
| Distance to health facility | |||
| <5 km | 4212 | 98 | p=0.0001 |
| >5 km | 8361 | 33 | |
One hundred and seventeen out of the 131 cases of deaths were from Comuna sede of Menongue district accounting for 89% of all deaths recorded during the review period. Additionally, Caiundo and Missombo comunas of Menongue district accounted for another 2.7% indicating that about 93% of all deaths were from Menongue district. The districts of Cuito Cuanavale and Cuchi accounted for only 3.8% and 1.5% of all deaths respectively. Four cases representing (3%) lack information on place of domicile.
Women living in rural areas accounted for 96.2% of all deaths and the difference in the place of domicile (rural versus urban) was significantly associated with maternal deaths (p < 0.0001) (Table 3).
Distance to the nearest health facility that provides Maternal Health Services (MHS) was significantly associated maternal mortality (p < 0.0001), with women who responded that distance is not an obstacle accounting for only 30% of all maternal deaths during the period under review (Table 3).
Out of the 131 maternal deaths, 52 (40%) occurred within the first 24 hours of been admitted in the hospital, 29 (22%) deaths occurred 24-48 hours after admission, while 47 (35.6%) occurred between 2 to 11 days after admission. Four deaths lacked information on the time of death.
The maternity hospital has two medical doctors in 2010 which increased to four in 2014. With an estimated 62, 736 women in the reproductive age group and 14,937 annual pregnancies for Menongue district where the hospital is located, the ratio of Midwife per 1000 women in the reproductive age group for Menongue district is 1 per 2,134 pregnancies per annum. The study hospital has no ultrasound services that could aid in gynecological and obstetric diagnoses.
Discussion
The mean MMR of 1830 per 100,000 live births recorded in this study is five times higher than the desired MDG 5 goal of 300 per 100,000 live births by the year 2015,[4] and four times higher than the WHO estimate for Angola. [1] As earlier pointed out above, there is a general lack of published journal articles on maternal mortality (hospital or community based) in Angola. The official report by the health authorities of Cabinda province of Angola indicated in 2012 the MMR was 234.3/100,000 live births.[25] However, a review of records in all the 10 health facilities that provide obstetric care in Cabinda province by Rodrigues (2013) concluded that the provincial official MMR is an under estimation and that the magnitude of the problem is unknown because data is generally incomplete or not available in all the 10 health facilities.[26]
However, when compared with published studies (2010-2015) from Central Africa region to which Angola belongs, the MMR of this study (1,830 per 100,000) was higher than other hospital based study in Cameroon (287.57100, 000). [27] The huge difference in MMR between our finding and the Cameroonian study may partially be due to the fact that more than half of all the cases of maternal mortality in our study area was among women who were less than 20 years or more than 35 years and presented with complicated pregnancies that resulted in maternal deaths. Moreover, the difference in MMR could also be as a result of a general lack of high skilled medical doctors who have not yet specialized in obstetrics and the lack of basic obstetric diagnostic equipment’s like ultrasound machine which might have limit the quality of case management in our study area compared to the Cameroonian study that was conducted in a tertiary, research and training hospital and therefore more capable to deal with high risk pregnancies.
When compared with hospital based studies that were conducted between 2010-2015 from other regions of Africa, a high level of MMR was also reported from Nigeria, West Africa, ranging from 866 to 1,791 per 100, 0000 live births in the Southern[28,29] and Northern parts of Nigeria respectively.[30,31] However, lower figures of between 124 and 492 per 100,000 live births was reported East African countries - Kenya[32,33] and Tanzania[34,35] respectively. It is important to note that since 2010, Tanzania and Kenya were reported to have made significant progress in the implementation of emergency obstetric care and maternal death surveillance and response compared to Angola and therefore may partly account for their lower MMR.[36] Similar disparity was observed in hospital based studies among South East Asian countries with Nepal[37] and Pakistan[38] both having lower MMR of 357 and 1007 per 100,000 live births respectively compared to the 1,830 per 100,000 live births reported in this study.
However, when compared with the MMR from Northern Europe and North America, the figure obtained in this study is 167 times higher and hence, reinforces the huge disparity in population health outcome between developed and developing countries.[1] This is driven, in part, by differences in socioeconomic, cultural and political development of these developed countries compared to under developed countries like Angola.
Overall, the MMR obtained in this series is far higher than Angola’s 2014 estimated MMR of 460 per 100,000 live births by the WHO.[3] This might not be unrelated to the fact that, the data used in this study were largely incomplete with more than a third of all cases of maternal deaths lacking information on the working diagnosis or clinical management and hence could be a marker for possible under estimation. The possibility of under estimation is further reinforced by the reports on the status of implementation of maternal death Surveillance and Response which rated it to be low in Angola. [10,26,36] The dearth of published information on maternal deaths in Angola, which could have provided additional information on the state of maternal mortality, is also a big challenge. For instance, extensive systematic reviews of over 7000 articles on maternal mortality, reproductive health and female autonomy, there was no single article from Angola,[7,8] despite having a higher than the desired MDG 5 goal of 300 per 100,000 live births by the year 2015.[1,4] Although, hospital based studies are likely to limited by misrepresentation or selection bias, we believe that the likelihood of under estimation cannot be easily dismissed without conducting large scale community based quantitative and qualitative studies. The available data for this study were characterized by the lack of basic information on some or all of the following variables such as parity, birth order, booking status and number of Ante natal care visits in majority of the cases. This was further compounded by none of the cases have information on well-established drivers of utilization of maternal health services such as the level of education, income, religion, ethnicity, and occupation as was reported by several studies.[39-41] The lack of information on these variables makes it difficult to estimate the risk of dying from pregnancy and its related complications based on parity, education, income, and religion, which invariably compromises the appropriateness and quality of any population based public health intervention that is currently being implemented in the province. Furthermore, although a maternal mortality review committee was established, however, during the period under review (2010-2014), not a single review meeting was held. This further reinforces the likelihood of the current plans directed to address maternal deaths are not data driven and could be contributory to the high MMR recorded in this study.
The causes of direct obstetric death (Table 2) in this study were the same to those reported from various regions of the developing countries. However, although, literature on direct obstetric causes of maternal death was reported to account for 80% of all maternal deaths in the developing countries,[4] however, a much lower figure (51%) was recorded in this study. The reason been largely attributable to the poor documentation with at least a quarter of cases had no working diagnosis. Nevertheless, hemorrhage, puerperal sepsis, eclampsia, and ruptured uterus were the major causes of direct deaths as was similarly reported from several developing countries.[42-44] The high proportion of these causes in this study may be because many of the cases were teenagers (37.8%) and had delivered at home (27.2%) before seeking help in a health facility. Thus, teenage pregnancy, lack of prenatal care and delay in seeking early medical intervention increase the risk of ruptured uterus due cephalo-pelvic disproportion/malpresentation, and undiagnosed preeclampsia that resulted in eclampsia, hemorrhage and sepsis due to unhygienic condition associated with home delivery. These risk factors were similarly reported from studies elsewhere.[42,43]
Limitation of the study
Our study has a number of limitations. First, this study is essentially hospital based and therefore, estimates calculated, tend to be very high. Thus, women who died or deliver in this hospital are not the true representation of the entire country.
Second, patients referred to this hospital, are high risk women who had presented themselves for prenatal care at other health institutions, but were referred here for delivery. This means that, among the women giving birth in these hospitals, there will be a disproportionate number of women with obstetric complication and women who die here which may partly explain the high MMR recorded.
Third, a large proportion of women who died might have been admitted as an emergency and in moribund condition; but whose deaths will swell the number of total hospital deaths.
Conclusions and Global Health Implication
With an MMR of 1,830 per 100,000 live births, the scourge of pregnancy and childbearing are enormous in this environment. This study demonstrated that, MMR is higher than the estimates by WHO [1] and the province is not likely to achieve the desired MDG 5 target of MMR 300 per 100,000 live births. Although, hospital based studies suffer from Berksonian bias, however, the lack of periodic reviews or community based surveys made this study useful by highlighting the lack of documentation of basic information that constituted the WHO framework on social determinants of disparities in population health,[42] and documentation is the starting point of evidence based planning. Hence, the result of the study is an indictment on the policy standard operating procedures for maternal health services and the likelihood of using plans that are not data driven. The fact that the hospital operates without an ultrasound machine to enhance appropriate diagnosis and management of cases, further underscores the likelihood of minimal impact of clinical intervention to avert maternal deaths. This study also sheds more light on the need for operational and community based quantitative and qualitative studies, in order to provide better insights on what operates in the community from the time when danger signs of pregnancy are recognized at household level to the time when appropriate management has commence in a health facility. Such approach will provide basis for the development of holistic multi-prong evidence based intervention that will improve the quality of service with subsequent reduction in MMR.
Recommendations
Based on the findings above, the following recommendations were made:
-
Measure progress, by way of provision of funds for research and evaluation, so that lapses will be easily detected and corrected through policy formulation. This process should include review of all cases of maternal death by the maternal mortality review committee. Findings should be use to come up with minimal documentation required, development of standard operating procedures and the creation of a simple Microsoft excel data based. There is need to consider the involvement of communities and the use of mobile telephone to send messages to the nearest health facility on maternal morbidity and mortality.
-
Discourage teenage marriage and early childbearing. This should be through community mobilization; giving them basic information about pregnancy and childbearing. Another approach is to provide compulsory formal education up to Secondary School level for all children. This will delay marriage and hence childbearing. The overall effect is the modification of the young woman’s behavior towards health and ultimately enhance female autonomy and empowerment.
Acknowledgement
We thank the Director of the Maternity Hospital Menongue, Dr Delfina Jamba, for providing the necessary approval for the research and access to the data.
Ethical Consideration:: An approval was given by the Director of the maternity hospital on behalf of the ethical, research and publication committee.
Funding:: The authors have no support or funding to report.
Conflict of Interest: The author declare that they have no competing interests.
References
- 2014. World Health Statistics. Retrieved on 10th April 2015 from http://www.who.int/gho/publications/world_health_statistics/2014/en/
- World Health Statistics 2013 2013a Retrieved on 10th April 2015 from http://www.who.int/gho/publications/world_health_statistics/2013/en/
- 2014. State of the world children 2014 in numbers: Every child counts-Revealing disparities and advancing children’s rights. Retrieved on 18th October 2015 from http://www.unicef.org/gambia/SOWC_report_2014.pdf
- 2010. United Nations Children’s Fund, United Nations Population Fund & the World Bank. Trends in Maternal Mortality: 1990 to 2008 – Estimates developed by WHO, UNICEF, UNFPA, and the World Bank’. Geneva, Switzerland: WHO; Retrieved on 10th March 2014 from http://whqlibdoc.who.int/publications/2010/9789241500265_eng.pdf
- Chr Michelsen Institute and Centro de Estudos e Investigação Cientifica. Angola health survey: Opportunities to reduce maternal and new-born deaths. 2012. Angola Brief. 2:1-4. Retrieved from http://www.cmi.no/publications/file/4492-angola-health-survey.pdf
- [Google Scholar]
- 2005. Four million neonatal deaths: when where, why? The Lancet Neonatal Survival Series. 1:18. Retrieved from http://www.who.int/maternal_child_adolescent/documents/pdfs/lancet_neonatal_survival_paper1.pdf
- Knowledge gaps in scientific literature on maternal mortality: a systematic review. Bulletin of the World Health Organization. 2006;84(11):903-909.
- [Google Scholar]
- A systematic review of inequalities in the use of maternal health care in developing countries: examining the scale of the problem and the importance of context. Bulletin of the World Health Organization. 2007;85:812-819.
- [Google Scholar]
- Maternal mortality in low income Countries: What interventions have been evaluated and how the evidence base be developed further? International Journal of Gynecology and Obstetrics. 2009;105:78-81.
- [Google Scholar]
- 2013b. Maternal death surveillance and response: Technical guidance. Information for action to prevent maternal death. Geneva, Switzerland: WHO; Retrieved from http://www.who.int/maternal_child_adolescent/documents/maternal_deathsurveillance/en/
- 2010. Technical Guidelines for Integrated Disease Surveillance and Response in the African Region, Brazzaville, Republic of Congo and Atlanta, USA. Retrieved from http://www.afro.who.int/en/clusters-a- programmes/dpc/integrateddisease-surveillance/features/2775-technicalguidelines-for-integrated-disease-surveillance-andresponse-in-the-african-region.html
- 2012. Improving maternal mortality and other aspects of women’s health: The United States’ global role. A report of the Center of Strategic and International Studies, Washington D. C. Retrieved from https://www.google.com.ng/?gws_rd=cr#q=Nieburg%2C+P.+%282012%29.+Improving+maternal+mortality+and+other+aspects+of+women%E2%80%99shealth% 3A+The+United +States% E2% 80%99+global+role
- 2015. Assessment of Maternal Death Audit Systems in Africa Level of Implementation & Gaps. Retrieved from http://sa.au.int/en/sites/default/files/2014_Status_Report_on%20MNCH%20-%20 English_1.pdf
- Maternal mortality in Herat Province, Afghanistan, in 2002: An indicator of women’s human rights. 2002. Journal of the American Medical Association. 288:1284-1291. Retrieved from http://jama.jamanetwork.com/article.aspx?articleid=195273
- [Google Scholar]
- Dimensions of women’s autonomy and the influence on maternal health care utilization in a north Indian city. 2001. Demography. 38:67-68. Retrieved from http://link.springer.com/article/10.1353/dem2001.0001
- [Google Scholar]
- Revisiting the behavioral model and access to medical care: does it matter? Journal of Health and Social Behavior. 1995;36:1-10.
- [Google Scholar]
- Societal and individual determinants of medical care utilization in the United States. The MillBank Quarterly. 2005;83(4):1-28.
- [Google Scholar]
- Determinants of dental care utilization for diverse ethnic and age groups. Advances in Dental Research. 1997;11(2):254-262.
- [Google Scholar]
- Understanding the context of healthcare utilization: Assessing environmental and provider related variables in the behavioral model of utilization. Health Services Research. 1998;33(3):571-596.
- [Google Scholar]
- The use of health services by older adults. Journals of Gerontology Series B-Psychological Sciences and SocialSciences. . 1991;46(6):S345-S357.
- [Google Scholar]
- Intended use of informal long-term care: The role of race and ethnicity. Ethnicity & Health. 2004;9(1):37-54.
- [Google Scholar]
- Socio-economic status differences in older people’s use of informal and formal help: A comparison of four European countries. Ageing and Society. 2006;26(5):745-766.
- [Google Scholar]
- Informal help in the assisted living setting: A 1-year analysis. Family Relations. 2001;50(4):335-347.
- [Google Scholar]
- Resultados preliminares do Censo. Instituto Nacional de Estatistica, Luanda, Angola 2015 Retirado de http://www.geohive.com/cntry/angola.aspx
- Annual Activities Report for the Province Health Units, Cabinda Provincial Health Secretary. 2013.
- Maternal Mortality in Cabinda, Angola: Description of the Reproductive Health Care Available. Being a dissertation to the Faculty of Medicine the University of Porto, in partial fulfillment of the requirements for the Master’s degree in Epidemiology at the Faculty of Medicine of the University of Porto 2013
- Maternal Mortality in Cameroon: A University teaching hospital report. Pan African Medical Journal. 2015;21:16. Doi: 10.11604/pamj.2015.21.16.3912
- [Google Scholar]
- Maternal deaths where do they occur: A survey of health facilities in Abia state, South East Nigeria. Journal of Nursing Education and Practice. 2013;3(3):139-148. Doi: 10.5430/jnep.v3n3p139
- [Google Scholar]
- Maternal mortality trend in South East Nigeria: Less than a decade to the Millenium Development Goals. Journal of Women’s Health. 2010;19(2):323-327. Doi: 10.1089/jwh.2008.1028
- [Google Scholar]
- Trends in maternal mortality in a tertiary institution in Northern Nigeria. Annals of African Medicine. 2009;8(4):221-4. doi: 10.4103/1596-3519.59575
- [Google Scholar]
- High maternal and neonatal mortality rates in Northern Nigeria: an 8 month observational study. International Journal of Women’s Health. 2013;5:495-499. Doi: http://dx.org/10.2147/IJWH.S48179
- [Google Scholar]
- A retrospective analysis of maternal and neonatal mortality at a teaching and referral hospital in Kenya. Reproductive health. 2013;10:13. Doi: 10.1186/1742-4755-10-13
- [Google Scholar]
- Maternal mortality in central province, Kenya. Pan Afr Med J. 2014;17:201. Doi: 10.11604/pamj.2014.17.201.3694
- [Google Scholar]
- Maternal near-miss and mortality in a rural referral hospital in northern Tanzania: A cross sectional study. BMC Pregnancy &Child Birth. 2013;13:141. Retrieved from http//:biomedcentral.com/1471-2393/13141
- [Google Scholar]
- Ten years trend in maternal mortality at Kilimanjaro Christian Medical Centre Tanzania; 2003-2012. A descriptive retrospective hospital based study. Asian Pacific Journal of reproduction. 2016;5(3):214-220. Doi: 10.1016/japjr.2016.04.012
- [Google Scholar]
- Maternal mortality for 181 countries, 1980-2008: a systematic analysis of progress towards Millennium Development Goal 5. Institute for Health Metrics and Evaluation. Doi:10.1016/S0140-6736(10)60518-1 Retrieved from http://cdrwww.who.int/pmnch/topics/maternal/20100402_ihmearticle.pfd
- Maternal death review of a tertiary care hospital Nepal. Journal of Nepal Medical Association. 2014;52(193):713-718.
- [Google Scholar]
- Trends in maternal mortality in tertiary care hospital in Peshawar Pakistan. J Postgrad Med Inst. 2012;26(4):422-427.
- [Google Scholar]
- Economic status, education and empowerment: Implication for maternal health services utilization in Developing countries. PLoS ONE. 2010;5(6):e1190. doi: 10.1371/journal.pone.0011190
- [Google Scholar]
- Factors influencing the selection of delivery with no one present in Northern Nigeria: implications for policy and programs. InternationalJournal of Women’s Health. 2014;6:171-183. Doi: 10.2147/IJWH.S54628
- [Google Scholar]
- Where do Poor women in developing countries give birth?A multi-country analysis of demographic and health survey data. PLoS One. 2011;6(2):1-8.
- [Google Scholar]
- 2008. Inequities are killing people on a grand scale: The Reports WHOs commission on health inequalities. News Release WHO/29, August 28, WHO, Geneva, Switzerland. Retrieved from http://www.who.int/mediacentre/news/releases/2008/pr29/en/index.html
- Predictors of maternal mortality in institutional deliveries in Nigeria. 2012. African Health Science. 12:32-40. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/23066417
- [Google Scholar]
- 2012. What are the effects of different models of delivery for improving maternal and infant health outcomes for poor people in urban areas in low income and lower middle income countries? Department for International Development, London. Retrieved from http://eprints.lse.ac.uk/41908/1/What_are_the_effects_of_different_models_of_delivery_for_improving_maternal_and_infant_outcomes_for_poor_people_in_urban_areas_in_low_income_and_lower_middle_income_countries_%28LSERO%29.pdf





