Translate this page into:
Empowering Midwives in Humanitarian Settings: Integrating Heat-Stable Carbetocin and Tranexamic Acid into Postpartum Hemorrhage Training
Nguyen Toan Tran

*Corresponding author: Alice Rosmini, Piazza VII Novembre 1944 n 6 CAP, Bologna, Italy. Tel: 00393402285329 alicerosminiprofessional@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Rosmini A, Mugerwa K, Ochan AW, Muwanguzi S, Sake JB, Mwesigwa R, et al. Empowering midwives in humanitarian settings: Integrating heat-stable carbetocin and tranexamic acid into postpartum hemorrhage training. Int J MCH AIDS. 2024;13:S72-80. doi: 10.25259/IJMA_10_2023
Abstract
Background and Objective
Maternal mortality remains extremely high in fragile settings, with hemorrhage as the leading cause. This study describes a new model for more effective training on postpartum hemorrhage (PPH) prevention and treatment.
Methods
Using a low-dose (of information) and high-frequency (of repetitions) approach (LDHF), the strategy comprised an introductory webinar, self-paced study, 2-day in-person workshops, cascade training, continuous facility-based skills drills, and a WhatsApp community of practice and supervision (CoP). Innovations consisted of the practical, midwifery-centered, and short-duration training, and the integration of tranexamic acid (TXA) and heat-stable carbetocin (HSC) into existing modules from the “Bleeding-After-Birth-Complete” toolkit. Effects were assessed through mixed-methods evaluation. Confidentiality and “do-not-harm” principles were respected.
Results
Nine training sessions were conducted in South Sudan and Uganda combined, engaging 126 participants. Average knowledge increases of 21% in South Sudan and 18% in Uganda were recorded. Feedback also indicated changes in practices and attitudes: enhanced competency, teamwork, clinical protocols adherence, appreciation for midwife-led practical sessions, the LDHF method, and continuous support through the WhatsApp CoP. In post-workshop action plans, facility teams outlined steps to apply acquired knowledge and skills. These included training colleagues, establishing quality improvement projects, conducting skill drills, ensuring job aid visibility, and systematically reporting on PPH in the data collection templates of the facilities.
Conclusion and Global Health Implications
This case study highlights the value of a practical, LDHF refresher training strategy. This strategy bolstered providers’ skills, knowledge, and confidence in using HSC and TXA for PPH prevention and treatment. Findings can guide future training in similar fragile, low-resource, and humanitarian settings. Strengthening midwifery leadership, fostering interdisciplinary collaboration, and using the LDHF training approach can contribute to resilient health systems and taskforce, aligning with global efforts to reduce maternal mortality.
Keywords
Postpartum Hemorrhage
Refresher Training
Midwifery Education
Humanitarian Settings
Low Dose
High Frequency
Heat-Stable Carbetocin
Tranexamic Acid
Sudan
Uganda
Introduction
Background of the Study
The sustainable development goal of reducing maternal mortality ratio to less than 70 per 100,000 live births by 2030 remains a significant challenge. In 2020, maternal causes led to the death of 1 woman every 2 minutes.[1] While progress has been made globally to address maternal mortality, substantial disparities persist across and within countries, exacerbated by conflicts, instability, and multifaceted inequities. About 70% of global maternal deaths in 2020 occurred in Sub-Saharan Africa alone, while Central and Southern Asia accounts for nearly 17%.[1] Hemorrhage is a leading cause of maternal deaths, with over two-thirds of fatal cases occurring postpartum.[2,3]
The Minimum Initial Service Package for Reproductive Health in Crisis (MISP) was established in 1995.[4] Internationally recognized,[5,6] the MISP has a specific focus on the prevention and management of postpartum hemorrhage (PPH) within the emergency obstetric and newborn care (EmONC) objective.
Historically, misoprostol and oxytocin have been employed successfully in fragile settings for PPH prevention and treatment, but acceptability and logistic challenges persist.[7,8] In 2019, WHO added heat-stable carbetocin (HSC) and tranexamic acid (TXA) to its list of essential medicines as additional options, potentially revolutionizing PPH management.[9] However, these drugs remain underused and understudied.[10,11] To explore the feasibility of HSC and TXA in low-resource and cold-chain-challenged settings, the United Nations Population Fund (UNFPA) initiated in 2021 an implementation research studying HSC and TXA introduction in Basic EmONC (BEmONC) facilities, in crisis-affected regions in Uganda and South Sudan.
South Sudan has the highest maternal mortality ratio in the world (MMR): 1,223 maternal deaths per 100,000 live births.[1] Uganda, with an MMR of 284 per 100,000[1] is the African country with the highest number of refugees,[12,13] leading to high inequalities in care across geographical areas.[14] Midwives are at the forefront of BEmONC services, particularly in underserved and insecure areas, where emergency referrals and physicians’ presence are not guaranteed. Introducing TXA and HSC and investing in training midwives on its safe and appropriate use could be pivotal in mitigating PPH in these contexts. However, this requires comprehensive capacity-building, revised policies and guidelines, as well as strengthened infrastructure, supplies, and data collection.
Objectives of the Study
To our knowledge, there is no published literature on capacity-building best practices and lessons learned on the integration of HSC and TXA into PPH prevention and treatment algorithms in humanitarian settings.[10,11] Therefore, we focused on the capacity development aspect of the HSC and TXA implementation research, detailing strategies to enhance the knowledge and skills of providers, particularly midwives, at the BEmONC level. Both the innovative LDHF approach and the practical design consider the professionals’ workload and limited availability to be away from their facilities. The training strategy to refresh and expand clinical expertise is presented as a case study so that lessons learned, feedback from stakeholders and researchers, and recommendations can be used for replication and scale-up.
Methods
Training Strategy
The program was designed for health professionals who had prior training in PPH and were actively engaged in BEmONC services within humanitarian contexts, as an advanced refresher to provide updates on the application of HSC and TXA. While reinforcing existing PPH knowledge, attitudes, and skills, the training was not suitable for students or professionals lacking practical experience. It focused primarily on midwives (64% of participants), who are, globally, the professionals capable of addressing approximately 90% of sexual, reproductive, maternal, neonatal, and adolescent health (SRMNAH) issues.[15] Central to this curriculum was the strategic integration of existing modules from the Helping Mothers Survive (HMS) Bleeding After Birth Complete (BABC). This interagency toolkit aligns with international guidelines and can be delivered in 2 days. The choice of this package was deliberate, as it is well-designed, open source, and available in several languages, presenting an excellent option for adaptation and rapid scale-up in low-resource and fragile settings, where the range of health professionals and availability of the SRMNAH workforce is limited.
Key competencies encompassed active management of the third stage of labor, early PPH detection, and basic and advanced PPH management. Effective communication, respectful care, teamwork, and quality of care were also emphasized. Adaptations were made to contextualize the training, for instance by covering the mechanisms of action and the use of HSC and TXA as per WHO guidelines, which was necessary for the selected audience. Conversely, the Nonpneumatic Antishock Garment (NASG) and cervical laceration repair were not systematically presented, since they were not used in most of the study settings.
The methodology, presented in Figure 1, employed a low-dose, high-frequency (LDHF) approach, focusing on concise information and repetitive drills, which has demonstrated successful implementation in similar contexts.[16] Combined with a short in-person training and a WhatsApp-based community of practice (CoP), it granted continuity in clinical development, while minimizing potential disruptions in services. This approach unfolded across five phases.
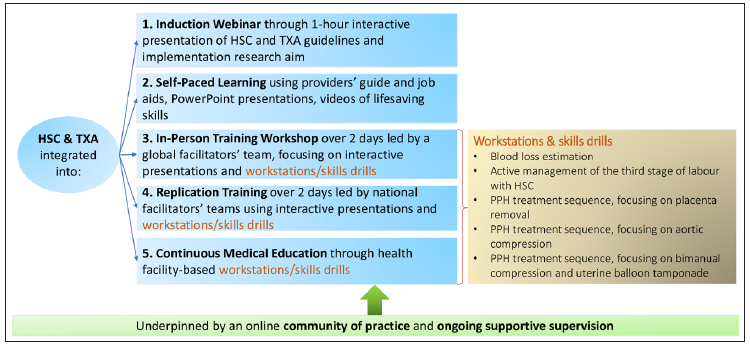
- HSC and TXA-inclusive, low dose, high frequency PPH training strategy. HSC: Heat-stable carbetocin, TXA: Tranexamic acid, PPH: Postpartum hemorrhage.
Phase 1: Introductory Webinar
A 1-hour introductory webinar for health professionals and stakeholders outlined current PPH management guidelines and introduced HSC and TXA.
Phase 2: Self-Paced Learning
Using a reverse classroom strategy,[17] the BABC posters and providers’ guide were shared prior to the webinar, while PowerPoint presentations, videos, and job aids were provided at the end. Participants independently studied these materials at their own pace, before meeting in the workshop “classroom.”
Phase 3: In-Person Training Workshop
In each country, a two-day in-person workshop was built on participants’ self-learning: theoretical aspects were interactively discussed, but the main focus was on practical skills drills and simulations using anatomical models. Midwives were encouraged to take leadership during the practical sessions. The standard PPH facilitator guide was organized as an interactive presentation, complemented with additional information on HSC and TXA, and on the implementation research project. Pre and post tests assessed knowledge acquisition, while the workstations [Figure 1] provided an opportunity to observe skills improvement. While Objective Structured Clinical Examination (OSCE) evaluation sheets were not systematically employed for each participant, facilitators used them for guidance in the overall assessment of the groups’ skills improvement. Post simulation debriefing fostered self-reflection beyond strictly clinical interventions, encompassing the implementation of respectful maternity care throughout the simulations. Following the workshop, participants engaged in group discussions and presented action plans to implement the acquired knowledge and skills within their respective facilities.
Phase 4: Replication Training
The country teams who attended the workshop were then responsible for transferring skills to others, aligning with training standards. In South Sudan, the national team undertook each of the replication training. In Uganda, the study team facilitated an additional workshop and then selected the most performing participants to cascade the training to their colleagues. Passing on knowledge and skills also reinforced participants’ competencies and confidence in the post training phase. Feedback from the first round of training was considered in rolling out the repetitions, compatibly with the training standards.
Phase 5: Continuous Skills Drills and Supportive Supervision
Remote and visit-based mentorship, supportive supervision, continuous facility-based skills drills, and sustained monitoring were coordinated by the country teams. This was done through bilateral interactions with the mentors and greatly benefitted from the establishment of the CoP. In this phase, the role of the country team and facility-based midwives in supporting continuous learning and follow-up of recommendations were crucial.
Data Collection and Statistical Analysis
For knowledge assessment, the same 20-question knowledge questionnaire was administered for pre and post tests. The BABC module template was slightly modified to incorporate questions on HSC and TXA. Individual scores were compiled for each training, paired-sampled t-tests and average scores were computed, and confidence intervals were calculated.
The end-of-workshop evaluation forms consisted of 24 close-ended questions, covering workshop facilitation, organization, and content. The evaluation also enquired about training’s impact on satisfaction and confidence in performing tasks related to PPH prevention and treatment. Answers were graded on a 1 to 5 agreement scale and individual scores were compiled, aggregated, and analyzed for each training session. Participants were also asked to list the three most useful topics, which were then ranked in order of preference; additional comments were also grouped by categories and presented by frequency.
To gain qualitative insights into their experience, we invited participants to engage in focus-group and in-depth discussions during the training and at the end of the overall implementation study. Their perspectives were audio-recorded and transcribed. Analysis involved the manual identification of recurring themes and the evaluation of convergence within the mixed-method data, undertaken by the respective country training teams. The global study team collated and reviewed the training data and reports from both countries to identify shared insights. Findings were further corroborated through validation by the country teams, including self-reflective interviews.
This mixed-method study aligns with the following reporting guidelines: STROBE[18] for the quantitative aspects and COREQ[19] for the qualitative aspects.
Ethical Approval
Institutional Review Board approval was obtained in both countries. Participation in the workshops and in-depth discussions was entirely voluntary and without financial compensation, except for reimbursement of associated expenses. Anonymity and confidentiality were maintained in handling participant feedback. No patients were involved in skills drills or any other activities related to the training study.
Results
Sociodemographic Characteristics of the Training Participants
Between May and August 2022, a total of nine workshops were conducted (seven in South Sudan and two in Uganda). The participants came from BEmONC facilities located in humanitarian areas of these countries.
Workshops accommodated anywhere from 6 to 32 participants per session. In total, 126 attended: 68 from South Sudan and 58 from Uganda. Priority was given to clinical professionals from maternities (90%). Midwives were the majority (64%), general physicians constituted 13%, while nurses and other clinical profiles accounted for 12%. A small minority were public health or reproductive health officers and program managers (8%) and obstetricians (2%).
Knowledge Increase
One hundred and twenty four participants took both pre- and post tests, revealing a marked knowledge increase in both countries. In South Sudan, average scores increased by 21% (pre-test: 64%, post test: 85%, p < 0.05); in Uganda by 18% (pre-test: 74%, post test: 92%, p < 0.05).
This shows that new information on TXA and HSC and the correction of outdated knowledge on PPH, although introduced in the self-study phase, were consolidated during in-person activities.
Skills Drills
During the Arua training in Uganda, participants’ skills in estimating blood loss were assessed through six distinct simulations, each involving varying quantities of blood loss, and yielded a 24% average increase in scores (48%–72%). Two participants exhibited remarkable improvements of 65% (from 17% to 82%). This confirms the importance of practical sessions in PPH training.
Observations and participants’ feedback revealed that repetitive drills notably improved skills, adherence to the sequence of actions, and confidence in performing tasks. However, certain critical steps were occasionally omitted. Facilitators also noticed the necessity of first “unlearning” outdated practices to adopt correct ones. In some instances, providers struggled to accurately articulate interventions, such as placental inspection, PPH diagnosis, and blood loss estimation, highlighting the importance of repeated practice guided by visibly displayed clinical algorithms and communication with other team members. Moreover, debriefing with learners confirmed the observation by facilitators that professionals who were not physicians (e.g., midwives) were waiting for the doctor to act first. Consequently, midwives, who are usually at the frontline during labor and delivery, were urged to lead the workstations and skill drills. This midwifery leadership was well received by trainees and acknowledged as innovative and transformative:
“The practical parts of the regional training were led by the midwives. This is an innovation… And the response the colleagues give to a midwife is different from the one they would give to a doctor.” – Uganda.
The LDHF approach and humanistic simulations were also highly appreciated and recognized as innovative:
“Low-dose high-frequency was fitting very well in helping build capacity of midwives, reinforcing a specific piece of knowledge, and dwell on it until everybody absorbs it. And everybody is now working with it in a more relaxed way.” – Uganda.
“The [humanistic] models were also very useful during the practical parts…Usually, the common way to do training is to theorize about things...” – Uganda.
Action Plans
Another output of the workshop was the action plans by facility teams, outlining steps to operationalize, apply, and share the newly acquired skills and knowledge at their facilities. This was also a new approach for most of the teams. The plans included training colleagues, holding periodic skill drills, ensuring job aid visibility, assembling supplies into a PPH readiness kit, and systematically capturing information on PPH in the existing maternity registers. This indicates that participants interiorized the essential components for effective PPH interventions and included them in future action. Many facilities integrated these activities as part of quality improvement projects, such as enhancing the objectivity of blood loss measurement. This was illustrated in the reflective meetings:
“…[The action plan] has helped us to set a PPH kit because you need to set it before something occurs, and we didn’t have that…” – Uganda.
“…continuous refresher training for our staff is also very important because training makes us not to forget and it makes us more effective in case management.” – South Sudan.
Community of Practice
According to reports, the WhatsApp CoP significantly enhanced mutual support and sharing of experiences among the participants. This facilitated a collaborative learning environment across providers and facilities, and consolidated newfound skills and knowledge, including through benchmarking.
To our knowledge, post training action plans and CoP, which constitute an important outcome of this study, have not been integrated into previous PPH training interventions.
Workshop Evaluation
Across South Sudan and Uganda, 98 end-of-workshop evaluations were collected. Feedback was overall positive. The highest-rated aspects were workshop facilitation, organization, sessions on respectful maternity care, and skills drills. These elements reportedly bolstered participants’ confidence in detecting and managing PPH, fostering teamwork, and improving patient interaction. Areas with relatively lower but still good ratings included time allocation for practical sessions and understanding of balloon tamponade. The request for longer training is indicative of interest and importance attributed to the topic. The different components of the LDHF learning strategy (e.g., self-paced learning, webinar, and continuous supervision) balanced out the short duration of the workshops, which was dictated by feasibility and resource constraints.
Active Management of the Third Stage of Labor (AMTSL) was the most appreciated topic, followed by the utilization of HSC and TXA and manual placenta removal. Training materials were highly regarded, particularly the provider’s guide and PPH sequence demonstration videos.
Suggestions from participants included incorporating more hands-on activities, extending workshop duration, cascading training to others, and adding neonatal resuscitation to the curriculum.
Regarding operationalization, participants emphasized the importance of promptly providing facilities with all necessary supplies for PPH prevention and management. In refugee settings, the need for translated materials to ensure patient understanding and consent was highlighted.
Discussion
A mixed-method evaluation converged to indicate that an LDHF strategy used to integrate HSC and TXA in PPH training effectively enhanced participants’ knowledge, practical skills, and confidence in applying systematic steps to prevent and treat PPH. Beyond merely concentrating on HSC and TXA, the training adopted adult learning principles to enhance and broaden the existing knowledge and skills of participants. Our findings align with those from similar interventions in Sub-Saharan Africa,[20] but the recorded knowledge increase was higher than in previous similar interventions.[21] Moreover, while previous, robust studies mainly focus on objective skills and clinical outcomes,[22] the inclusion of participants’ and mentors’ evaluation in the qualitative analysis allows for a provider-centered adaptation of the intervention.
From the study, valuable lessons emerge to enhance similar training models in fragile and humanitarian settings, along with other contexts characterized by severely limited resources.
First, capitalizing on the established HMS-BABC module facilitated effective and prompt implementation allowing the training to adhere closely to evidence-informed practices and a more efficient replication. This enabled resources to be directed toward customization and contextualization, while still maintaining content validity and relevance.
Second, strategically selecting facilities from fragile settings and primarily focusing on midwives, and collaborating with professional associations, district leadership, and humanitarian response agencies yielded high rates of attendance. While acknowledging hierarchies-related dynamics, the presence of diverse professionals, including obstetricians, doctors, and clinical officers, optimized teamwork and communication as a major factor in timely and successful PPH management.[20,23,24]
Third, several improvement areas surfaced. The need to “unlearn” outdated practices, particularly in PPH management sequences, was observed and more time might have been dedicated to addressing it.[20,19] Clarity on the distinct role of HSC and oxytocin appeared insufficient at times, and continuous reinforcement of this message was recommended. Participants’ experienced difficulties in timely access to pre-learning materials due to logistical challenges and lack of adequate electronic devices and internet connection.
Fourth, efforts to maintain technical and facilitation integrity in training replication efforts cannot be overstated. The cumulative insights gleaned from this research with prior policy recommendations are combined in the Table 1.[25] The application of the specific steps could help countries and partners in planning and implementing PPH refresher course training that incorporates HSC and TXA while concurrently fostering capacity-building and empowerment of midwives.
| National Policy |
|
| Training |
|
| Health Facility Readiness |
Ensure a well-functioning supply chain to guarantee continuous availability of HSC, TXA, and other essential emergency obstetric care supplies in labor, delivery, and postpartum areas around the clock. Assemble PPH kits containing essential medications and materials for treatment. Procure essential materials, including blood-measurement drapes or jars for quantifying bleeding, a wall clock for documenting intervention timing, and a bell for summoning assistance during obstetric emergencies. Promote dialogue and action on maintaining the cold chain to ensure the availability of quality oxytocin for PPH treatment. |
HSC: Heat-stable carbetocin, TXA: Tranexamic acid, PPH: Postpartum hemorrhage.
Strengths and Limitations of the Study
The mixed-method approach was a strength, offering quantitative trends and operational insights from participants. OSCE checklists offer potential as quality assurance tools,[26] and they were used in our training, albeit not systematically. This and the non-measurement of knowledge retention downstream (e.g., at 6, 9, or 12 months) - due to limited resources - constitute study limitations. To enhance fidelity for easier training replication, several strategies could not be integrated into our methodology, and should be considered for future interventions. These include enhancing documentation, promptly analyzing training outcomes, and offering training to trainers, regular refreshers, and remote support to facilitators to enable them to address diverse learning needs and quality assurance mechanisms.[26]
Further research is needed to analyze the impact of CoP on peer support and mentoring in sustaining knowledge and skills, as well as PPH case discussion and management for continuous quality improvement. Interdisciplinary dynamics between doctors, midwives, and other cadres, and its influence on effective PPH management should also be further researched.
CONCLUSION AND GLOBAL HEALTH IMPLICATIONS
A refresher training strategy inclusive of HSC and TXA on PPH prevention and treatment indicated adequate implementation and positive influence on participants’ knowledge, skills, and confidence. The lessons learned can guide future training initiatives, helping improve maternal health outcomes in humanitarian contexts.
Key Messages
-
A comprehensive training strategy to integrate heat-stable carbetocin and tranexamic acid for postpartum hemorrhage prevention and treatment in humanitarian settings in South Sudan and Uganda, including self-learning, in-person workshops, and supportive supervision, increased knowledge and skills among health providers, empowering midwives as leaders.
-
Adaptation of existing modules from Breathing After Birth Complete, strategic facility and participants’ selection, and continuous skills drills were key success factors.
-
Lessons learned from this study emphasize the importance of unlearning outdated practices, clear communication among providers, support for self-paced learning, and documentation for continuous improvement.
Acknowledgments
We express our gratitude to all the participants who generously shared their time and insights for this study.
Compliance with Ethical Standards
Conflicts of Interest
The authors declare no competing interests.
Financial Disclosure
Nothing to declare.
Funding/Support
Ferring Pharmaceuticals generously provided funding and supplies for the study components with heat-stable carbetocin; the donor had no role in the design of the study and interpretation of the results. UNFPA Procurement Service Branch supported the implementation of the phase with tranexamic acid. The publication of this study was supported by funding from MSD, through its MSD for Mothers initiative, and is the sole responsibility of the authors. MSD for Mothers is an initiative of Merck & Co., Inc., Rahway, NJ, U.S.A.
Ethics Approval
Institutional Review Board was obtained in both countries as follows: Uganda National Council for Science and Technology (UNCST; HS2456ES) and the ethics committee in South Sudan (RERB NO: 32/21/07/2022 – MOH/RERB/29/2022).
Declaration of Patient Consent
Patient’s consent not required as there are no patients in this study.
Use of Artificial Intelligence (AI)-Assisted Technology for Manuscript Preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The opinions expressed are those of the authors and do not necessarily reflect the views of the funding agencies. UNFPA is solely interested in studying the implementation of HSC and TXA from a public health and emergency response standpoint. The aim is to potentially include the drugs in the complementary items offered through UNFPA Procurement and Supply for certain contexts. It is important to note that the factors motivating UNFPA to consider adding HSC and TXA to its catalog for specific situations might differ from the considerations of national health authorities.
Special Collection
This article is published as part of the special collection on prevention and treatment of postpartum hemorrhage in high-burden low- and middle-income countries: building cross-national evidence through implementation research.
REFERENCES
- Trends in maternal mortality 2000 to 2020: Estimates by WHO, UNICEF, UNFPA, World Bank Group and UNDESA/Population Division. 2023. [Accessed 2023 Nov 14]. Available from:https://www.who.int/reproductivehealth/publications/maternal-mortality-2000-2017/en/
- Maternal mortality evidence brief. :1-4.
- Global causes of maternal death: A WHO systematic analysis. Lancet Glob Health.. 2014;2(6):323-3. doi:10.1016/S2214-109X(14)70227-X
- [Google Scholar]
- Minimum initial service package (MISP) for sexual and reproductive health in disasters. J Evid Based Med.. 2014;7(4):245-8. doi:10.1111/jebm.12130
- [CrossRef] [PubMed] [Google Scholar]
- Central Emergency and Response Fund Life-Saving Criteria. 2020. p. :1-20.
- The Sphere Handbook: Humanitarian charter and minimum standards in humanitarian response (4th ed). 2018.
- Joint statement of recommendation for the use of uterotonics for the prevention of postpartum haemorrhage. Published online 2021. [Accessed 2023 Nov 14]. Available from: https://www.figo.org/joint-statement-recommandation-uterotonics-prevention-pph
- Prevention and treatment of postpartum hemorrhage in low-resource settings- FIGO safe motherhood and newborn health (SMNH) committee. Int J Gynecol Obstet.. 2012;117(2):108-18. doi:10.1016/j.ijgo.2012.03.001
- [Google Scholar]
- World Health Organization model list of essential medicines. Ment Holist Heal Some Int Perspect.. 2019;21:119-34.
- [Google Scholar]
- Tranexamic acid for postpartum hemorrhage treatment in low-resource settings: A rapid scoping review. Int J Environ Res Public Health.. 2022;19(12):7385.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Climate action during the pandemic: Annual Results Report 2020. Published 2021 Mar [Accessed 2023 Nov 14]. Available from: https://www.greenclimate.fund/document/annual-results-report-2020
- 2023 Global Report on Internal Displacement (GRID). Published 2023 May 11 [accessed 2023 Nov 14]. Available from: https://www.internal-displacement.org/publications/2023-global-report-on-internal-displacement-grid/
- Trends in inequality in maternal and child health and health care in Uganda: Analysis of the Uganda demographic and health surveys. BMC Health Serv Res.. 2022;22(1):1-12. doi:10.1186/s12913-022-08630-x
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- The State of the World’s Midwifery 2021. Fast Facts; 2021. p. :1.
- Low dose, high frequency: a learning approach to improve health workforce competence, confidence, and performance. Jhpiego. 2014:1-4. [Accessed 2023 Nov 14]. Available from: http://www.healthynewbornnetwork.org/resource/low-dose-high-frequency-a-learning-approach-to-improve-health-workforce-competence-confidence-and-performance/
- Enhancing the effectiveness of flipped classroom in health science education: A state-of-the-art review. BMC Med Educ.. 2022;22(1):1-15. doi:10.1186/s12909-021-03052-5
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- The strengthening the reporting of observational studies in epidemiology (STROBE) statement: Guidelines for reporting observational studies. Bull World Health Organ.. 2007;85(11):867-72. doi:10.2471/BLT.07.045120
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Consolidated criteria for reporting qualitative research (COREQ): A 32-item checklist for interviews and focus groups. Int J Qual Heal Care.. 2007;19(6):349-57. doi:10.1093/intqhc/mzm042
- [CrossRef] [Google Scholar]
- “No patient should die of PPH just for the lack of training!” Experiences from multi-professional simulation training on postpartum hemorrhage in northern Tanzania: A qualitative study. BMC Med Educ.. 2017;17(1):1-12. doi:10.1186/s12909-017-0957-5
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Helping mothers survive bleeding after birth: Retention of knowledge, skills, and confidence nine months after obstetric simulation-based training. BMC Pregnancy Childbirth.. 2015;15(1):1-7. doi:10.1186/s12884-015-0612-2
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Peer-assisted learning after onsite, low-dose, high-frequency training and practice on simulators to prevent and treat postpartum hemorrhage and neonatal asphyxia: A pragmatic trial in 12 districts in Uganda. PLoS One.. 2018;13(12):1-17. doi:10.1371/journal.pone.0207909
- [CrossRef] [Google Scholar]
- Changing the landscape of obstetric resident education in low- and middle-income countries using simulation-based training. Int J Gynecol Obstet.. 2021;154(1):72-8. doi:10.1002/ijgo.13526
- [Google Scholar]
- A relational approach to improving interprofessional teamwork in post-partum haemorrhage (PPH) BMC Health Serv Res.. 2022;22(1):1-13. doi:10.1186/s12913-022-08463-8
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- How to use heat- stable carbetocin and tranexamic acid for the prevention and treatment of postpartum haemorrhage in low- resource settings. BMJ Glob Health.. 2022;7(4):e008913. doi:10.1136/bmjgh-2022-008913
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Developing institutional capacity for reproductive health in humanitarian settings: A descriptive study. PLoS One.. 2015;10(9):1-18. doi:10.1371/journal.pone.0137412
- [CrossRef] [Google Scholar]
- Interventions to improve trainers’ learning and behaviors for educating health care professionals using train-the-trainer method: A systematic review and meta-analysis. J Contin Educ Health Prof.. 2021;41(3):202-9.
- [CrossRef] [PubMed] [Google Scholar]





