Translate this page into:
Feasibility, Acceptability, and Appropriate Use of Novel and Lesser-Used Medicines for Prevention and Treatment of Postpartum Hemorrhage: Evidence from Implementation Research

* Corresponding author: Sara Rushwan, Concept Foundation, Avenue de Sécheron, Geneva, Switzerland. Tel: +41 22 734 2560 s.rushwan@conceptfoundation.org
-
Received: ,
Accepted: ,
How to cite this article: Rushwan S, Tufa T, Gülmezoglu M. Feasibility, acceptability, and appropriate use of novel and lesser-used medicines for prevention and treatment of postpartum hemorrhage: Evidence from implementation research. Int J MCH AIDS. 2024;13:S4-8. doi: 10.25259/IJMA_17_2023
Abstract
Maternal mortality remains one of the primary global health challenges of the 21st century, despite major medical advances in the field. Although solutions are available, inequities determine where mothers die, with the majority of maternal deaths occurring in low- and middle-income countries (LMICs). More than one-third of maternal deaths are related to obstetric hemorrhage and most commonly postpartum hemorrhage (PPH). Effective, quality-assured uterotonics significantly reduce PPH-related morbidity and mortality. Updated World Health Organization (WHO) recommendations on uterotonics used for PPH prevention include the addition of heat-stable carbetocin (HSC) to the suite of prophylactic uterotonic agents as well as the use of tranexamic acid (TXA) for PPH treatment. Both medicines are promising interventions in obstetric care. However, the introduction of these medicines faces numerous challenges to end-user access, such as decentralized procurement, time-consuming policy updates, market access barriers, lack of demand for quality-assured products, and inadequate systematic training and information provision, impeding access in many LMICs. Assessing the feasibility and acceptability of implementing these medicines in different resource settings can help bridge the gap between research and development to policy and practice, in an effort to reduce the significant health inequities facing women accessing the public health sector for quality care during labor and delivery. In this Special Collection, we explore the findings from mixed-methods implementation research studies in nine LMICs which support the acceptability and feasibility of HSC and TXA administration by healthcare providers, generating evidence to help inform the introduction and scale-up of these new and lesser-utilized PPH medicines.
Keywords
Postpartum Hemorrhage
Heat-Stable Carbetocin
Tranexamic Acid
Low-and-Middle Income Countries
Implementation Research
INTRODUCTION
Despite progress, maternal mortality rates remain at unacceptably high levels, raising the alarm for not being able to reach the Sustainable Development Goal (SDG) 3 maternal mortality target by 2030.[1] To accelerate progress, addressing the direct causes of maternal mortality and morbidity remains a priority, especially postpartum hemorrhage (PPH) which continues to be the leading direct cause of maternal death. The SDG 3.1 target is to achieve a global maternal mortality ratio (MMR) of less than 70 maternal deaths per 100,000 live births by 2030; however, the reduction in MMR has stagnated in most regions between 2016 and 2020.[2] This necessitates an understanding of in-country realities, identifying key priorities for research, advocacy, and implementation and translating what good looks like into action.
PPH is defined as maternal blood loss of 500 ml or more after birth and results in approximately 70,000 maternal deaths annually.[3] Consequently, immediate administration of uterotonics by healthcare providers post-delivery is crucial and to have emergency care available during and after birth if required. The urgency to address stagnant PPH figures and global efforts to increase the investment in essential medicines has allowed for evidence generation on the effectiveness of heat-stable carbetocin (HSC), a long-acting oxytocin analog, for PPH prevention,[4,5] and tranexamic acid (TXA), an antifibrinolytic, for PPH treatment,[6] with the added advantage of not requiring a cold chain to maintain quality. This is important in settings where the cold chain is at risk of being compromised. Nonetheless, barriers to accessing quality PPH care in low- and middle-income countries (LMICs) hinder these medicines’ potential to reduce maternal deaths, rendering their translation into health policies and clinical practice challenging. Important steps for achieving access include the revision and update of national policies surrounding key priority maternal and newborn health recommendations, and catalyzing political will to operationalize an accelerated pathway to access these interventions for populations with the greatest need. Policy change shortens the interval in getting World Health Organization (WHO) PPH recommendations adopted within countries, and implementation research studies facilitate strategies for national-level adaptation of recommendations into clinical practice.
PATHWAY TO PRODUCT INTRODUCTION AND ACCESS
Challenges
National policy change is essential, but, on its own insufficient in the provision of access to life-saving medicines and technologies. The global maternal health community should consider health system factors such as human resources, commodity management capacity, and knowledge of individual medicines that influence a healthcare provider’s ability to use essential commodities safely and sustainably. Introducing these medicines requires a pathway that ensures long-term sustainability, which brings to light challenges related to accessibility, affordability, efficacy, and safety, as well as regulatory and policy barriers that impact their availability and use.
Collaborative Efforts
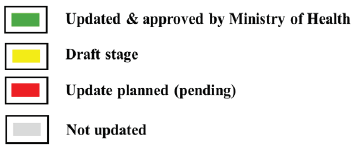
A 2019–2022 collaboration between Concept Foundation, WACI Health, the International Federation of Gynecology and Obstetrics, and the International Confederation of Midwives (as well as key regional and national stakeholders) was aimed at accelerating access to HSC and TXA in 15 sub-Saharan African countries (see Table 1 for country status at project end). The project shed light on some of the key barriers associated with implementing new recommendations for PPH prevention and management. These include a disconnect between global recommendations and national adoption, time-consuming in-country processes to update policies and clinical protocols, and limited cross-talk between key sectors.[7] Our learnings include the need for (1) a coordinated guideline development and dissemination strategy, (2) a supported health system to ensure the availability of these essential medicines, (3) comprehensive training of skilled healthcare providers according to evidence-based recommendations, (4) intersectoral collaboration and harmonization, and (5) evidence generation on the feasibility, acceptability, and appropriate use to support the successful implementation of the updated guidelines.
| Country* | National guideline status | National EML status |
|---|---|---|
| 1. Burkina Faso | ||
| 2. DRC | ||
| 3. Ethiopia | ||
| 4. Ghana | ||
| 5. Liberia | ||
| 6. Rwanda | ||
| 7. Senegal | ||
| 8. South Sudan | ||
| 9. Sierra Leone | ||
| 10. Ivory Coast | ||
| 11. Uganda |
Special Collection Research Findings
When assessing the efficacy and safety of HSC and TXA for the prevention and management of PPH, it is vital to consider the practicality of utilizing these drugs in diverse country settings. This involves evaluating their acceptability, ease of administration by healthcare providers, and other pertinent factors within the health systems of each country. By considering these components, informed decisions can be made about the appropriateness of these drugs for various contexts, ultimately contributing to improved prevention and management of PPH.
This Special Collection contains implementation research studies conducted in nine LMICs, which assessed the integration challenges and opportunities for HSC and TXA in routine care within the public health sector, and safe and appropriate use by healthcare providers.
Rushwan et al. conducted implementation pilots in selected facilities in Burkina Faso, Ethiopia, Ghana, Sierra Leone, and Uganda to assess the safe and appropriate use of HSC and TXA.[8] Alwadhi et al. conducted a secondary analysis of HSC introduction into 15 facilities in the state of Madhya Pradesh in India.[9] The Smiles for Mothers program yielded two studies that used mixed-methods research to assess HSC introduction in 39 facilities from ten counties in Kenya (Ruto et al.) and 18 facilities across three states in Nigeria (Amode et al.).[10,11] The United Nations Population Fund (UNFPA) Humanitarian Response Division conducted quantitative analyses of HSC and TXA introduction into humanitarian settings in six facilities in South Sudan and Uganda.[12,13] The UNFPA team also conducted qualitative research to gain insight into healthcare providers’ perspectives on using HSC and TXA,[14] and Rosmini et al. evaluated the integration of HSC and TXA within the PPH training strategy adopted in South Sudan and Uganda in the context of empowering midwives in humanitarian settings.[15] The findings overall conclude that it is feasible and acceptable to introduce HSC and TXA into public health systems of all the research study countries with high provider acceptance, with the need for health system adaptations to optimize introduction and scale-up. The outcomes of these research studies generate evidence that can be used to inform the development of an implementation strategy for nationwide adoption of quality-assured HSC and TXA use, which will support country-level funding opportunities and assist Ministries of Health in their introduction, scalability, and sustainability efforts. Gülmezoglu, et al. make the case for an end-to-end approach to planning and execution for timely and coordinated end-user access to essential maternal health medicines, applying this lens to HSC and TXA’s access pathways.[16]
RECOMMENDATIONS BASED ON STUDIES’ FINDINGS
Our recommendations based on the collective evidence generated in this Special Collection are to foster an enabling environment for the scale-up of HSC and TXA as new and lesser-used commodities. First, investment in health system strengthening demands multi-sectoral, concerted efforts for capacity building, centralized procurement, and improving the supply chain. This includes (but is not limited to) stakeholders such as policymakers, donors, procurement agencies, professional associations, non-governmental organizations, and civil society organizations. Second, healthcare providers are necessary to building resilient health systems, and empowering midwives, given their vital frontline contributions, should be incorporated into PPH training and supportive supervision. Third, a paradigm shift, on the perceived low return on investment in maternal health medicines, is needed to address structural maternal health market barriers and align with global efforts to reduce maternal mortality. There can be limited awareness and/or acceptance of this bottleneck at the ministry level as well as limited knowledge of new maternal and newborn health interventions that are particularly suited to LMIC realities. We believe targeted, multi-level demand generation can greatly amplify advocacy activities for policy change and beyond.
CONCLUSION AND GLOBAL HEALTH IMPLICATIONS
Lessons learned from all studies in this Special Collection include the need for a holistic and streamlined approach to PPH training that adheres to evidence-informed practices, engaging key stakeholders, and improving health information systems to support an enabling environment for the safe introduction of essential maternal health interventions into clinical practice. Additionally, there is a pressing need to enhance the data recording quality and ensure that key data is consistently captured in routine health records. This limitation can be addressed through regular supportive supervision and continuous monitoring and evaluation in the implementation of HSC and TXA to ensure ongoing effectiveness and safety. A larger sample size across all studies would also help improve the generalizability of the results.
Overall, the studies collectively indicate that the safe introduction and use of HSC and TXA in primary, secondary, and tertiary facilities is feasible and favorable to healthcare providers. Our goal is that this Special Collection underscores the safety, feasibility, and acceptability of introducing quality-assured HSC and TXA and also the importance of appropriate training and implementation research to meaningfully advance the field by building the evidence base for scale-up across various LMIC contexts. The global health implications are defining steps needed to introduce essential PPH medicines safely and effectively into the public health system of LMICs and the importance of implementation research to support safe and appropriate introduction into clinical practice. The potential impact is generating evidence to inform future national policy decisions that enhance PPH quality of care, ultimately improving maternal health outcomes and advancing the SDGs.
Key Messages
-
Heat-stable carbetocin (HSC) and tranexamic acid (TXA) are World Health Organization recommended medicines that have the potential to address gaps in postpartum hemorrhage (PPH) care in cold chain-challenged settings.
-
Implementation research in varied high-burden settings allows an understanding of the factors that contribute to the successful implementation and integration of recommended interventions into overall PPH care.
-
The research outcomes from this Special Collection generate evidence of the benefits and potential challenges related to the introduction of HSC and TXA into postpartum care in public facilities of low-and middle-income countries.
Acknowledgments
We would like to thank all country partners, principal investigators, research teams, and global organizations for their efforts in leading and executing these implementation research studies.
COMPLIANCE WITH ETHICAL STANDARDS
Conflicts of Interest
Concept Foundation assists the innovator of heat-stable carbetocin in registering the medicine in low- and middle-income countries. Concept Foundation works with one tranexamic acid innovator to develop products that are easier to use at peripheral levels of healthcare.
Financial Disclosure
Nothing to declare.
Funding/Support
The publication of this Special Collection was supported by funding from Merck Sharp & Dohme (MSD) through its MSD for Mothers initiative and is the sole responsibility of the authors. MSD for Mothers is an initiative of Merck & Co., Inc., Rahway, NJ, USA.
Ethics Approval
Not applicable.
Declaration of Patient Consent
Not applicable.
Use of Artificial Intelligence (AI)-Assisted Technology for Manuscript Preparation
The authors confirm that there was no use of AI-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
None.
Special Collection
This article is published as part of the special collection on prevention and treatment of postpartum hemorrhage in high-burden low- and middle-income countries: building cross-national evidence through implementation research.
REFERENCES
- A roadmap to combat postpartum haemorrhage between 2023 and 2030. Geneva: World Health Organization; 2023. [Accessed 2024 Apr 8]. Available from: https://www.who.int/publications/i/item/9789240081802
- Trends in maternal mortality from 2000 to 2020: Estimates by WHO, UNICEF, UNFPA, World Bank Group and UNDESA/Population Division. Geneva: World Health Organization; 2023. [Accessed 2024 April 29]. https://www.who.int/publications/i/item/9789240068759
- Global causes of maternal death: A WHO systematic analysis. Lancet Glob Health.. 2014;2(6):e323-33.
- [CrossRef] [PubMed] [Google Scholar]
- Heat-stable carbetocin versus oxytocin to prevent hemorrhage after vaginal birth. N Engl J Med.. 2018;379(8):743-52. doi: 10.1056/nejmoa1805489
- [CrossRef] [PubMed] [Google Scholar]
- Uterotonic agents for preventing postpartum haemorrhage: A network meta-analysis. Cochrane Database Syst Rev.. 2018;4(4):CD011689.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Effect of early tranexamic acid administration on mortality, hysterectomy, and other morbidities in women with post-partum haemorrhage (WOMAN): An international, randomised, double-blind, placebo-controlled trial. Lancet.. 2017;389(10084):2105-16. doi:10.1016/S0140-6736 (17)30638-4
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Challenges in updating national guidelines and essential medicines lists in Sub-Saharan African countries to include WHO-recommended postpartum hemorrhage medicines. Int J Gynaecol Obstet.. 2022;158 (Suppl 1):11-13.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Integrating heat-stable carbetocin and tranexamic acid for postpartum hemorrhage prevention and management in sub-Saharan Africa: A five-country pilot implementation study. Int J MCH AIDS.. 2024;13 doi:10.25259/IJMA_34_2024
- [Google Scholar]
- Introduction of heat-stable carbetocin through a public-private partnership model in India: A retrospective study to determine feasibility and its optimal use in public health settings. Int J MCH AIDS.. 2024;13 doi:10.25259/IJMA_11_2023
- [Google Scholar]
- Introduction of heat-stable carbetocin for postpartum hemorrhage prevention in public sector hospitals in Kenya: Provider experience and policy insights. Int J MCH AIDS.. 2024;13 doi: 10.25259/IJMA_4_2024
- [Google Scholar]
- An implementation research study on uterotonics use patterns and heat-stable carbetocin acceptability and safety for prevention of postpartum hemorrhage in Nigeria. Int J MCH AIDS.. 2024;13 doi: 10.25259/IJMA_1_2024
- [Google Scholar]
- Postpartum hemorrhage in humanitarian settings: Heat-stable carbetocin and tranexamic acid implementation study in South Sudan. Int J MCH AIDS.. 2024;13 doi: 10.25259/IJMA_8_2023
- [Google Scholar]
- Postpartum hemorrhage in humanitarian settings: Heat-stable carbetocin and tranexamic acid implementation study in Uganda. Int J MCH AIDS.. 2024;13 doi: 10.25259/IJMA_9_2023
- [Google Scholar]
- Postpartum hemorrhage in humanitarian settings: Implementation insights from using heat-stable carbetocin and tranexamic acid. Int J MCH AIDS.. 2024;13 doi: 10.25259/IJMA_7_2023
- [Google Scholar]
- Empowering midwives in humanitarian settings: Integrating heat-stable carbetocin and tranexamic acid into postpartum hemorrhage training. Int J MCH AIDS.. 2024;13 doi: 10.25259/IJMA_10_2023
- [Google Scholar]
- A tale of two medicines: The need for ownership, end-to-end planning and execution for development and introduction of maternal health medicines. Int J MCH AIDS.. 2024;13 doi: 10.25259/IJMA_21_2024
- [Google Scholar]





