Translate this page into:
Adapted Counseling Care Model for Management of Female Sexual Dysfunction Among Women Living With and Without HIV

*Corresponding author: Fatima M. Damagum, Department of Family Medicine, Aminu Kano Teaching Hospital, Kano, Nigeria drfatima0984@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Damagum FM, Ahmed ZD, Jalo RI, Salihu HM, Wester CW, Aliyu MH. Effectiveness of an adapted counseling care model for management of female sexual dysfunction among women living with and without HIV in Northern Nigeria. Int J MCH AIDS. 2024;13:e025. doi: 10.25259/IJMA_37_2024
Abstract
Background and Objective
Sexual health research among women living with human immunodeficiency virus (HIV) has focused mainly on sexual practices and risk behaviors, with little consideration for treating sexual dysfunction and improving sexual satisfaction. The aim of this pilot study was to assess the effectiveness of an adaptive counseling care model in the management of female sexual dysfunction (FSD) among women living with HIV and without HIV in northern Nigeria.
Methods
This was a prospective cohort study of 200 women with HIV and a matched comparison arm of 200 women without HIV. Sexual function was assessed using the Female Sexual Function Index (FSFI), with a score ≤ 26.55 indicating FSD. We counseled women with FSD using the Permission, Limited Information, Specific Suggestions, Intensive Therapy (PLISSIT) model and evaluated the effectiveness of the model by comparing mean differences in baseline and six weeks post-intervention FSFI scores.
Results
The overall prevalence of FSD was 96.8%, with no difference between HIV-positive and HIV-negative participants (p = 0.398). Based on the six domains of the FSFI, the most common reported dysfunctions were sexual pain (21.7%), sexual desire disorder (17.6%), orgasm disorder (17.6%), lubrication disorder (17.2%), sexual arousal (16.9%), and poor sexual satisfaction (9.0%). The overall mean FSFI score (±standard deviation, SD) for those with FSD, in both groups (n = 387) prior to the counseling intervention was 16.05±10.65 (HIV-positive: 18.58±8.46; HIV-negative: 13.98±10.85). At the end of the intervention, the overall mean FSFI score in both groups increased to 23.58±16.53 (HIV-positive: 21.37±11.24; HIV-negative: 16.72±13.81) (p < 0.05 in all cases).
Conclusion and Global Health Implications
FSD is very common among women in Northern Nigeria, irrespective of HIV status. An adapted counseling care model improved sexual function in both HIV-positive and HIV-negative women. The PLISSIT model can guide healthcare providers to initiate and navigate sexual health discussions with women in this setting.
Keywords
Female Sexual Dysfunction
HIV
Adaptive Counseling
Nigeria
INTRODUCTION
In the past decade, there has been increasing attention to the importance of addressing the concept of sexual health. Promoting sexual health can complement traditional public health efforts to improve mental health and quality of life.[1] Sexual health is an important component of overall health, but there are numerous barriers (professional, religious, cultural, and personal) that prevent women from receiving proper medical care and support for their sexual health needs.[2] Northern Nigeria is a highly conservative setting, and religious beliefs and cultural practices associated with the predominantly Muslim communities pose unique challenges to the identification and management of female sexual dysfunction (FSD). However, despite the enormous burden of FSD (prevalence of >80%)[3] in this population and the availability of effective treatment measures, FSD has been poorly researched.
The common denominator of all FSD is personal distress, which results in depression and anxiety, thereby affecting mental health and reducing the quality of life for the women affected.[4–8] For example, in a study on women with hypoactive sexual desire disorder (the most common FSD), respondents had low scores on validated measures of quality of life (SF-36 and SF-12 Health Surveys, and the EQ-5D)[9,10] that were comparable in magnitude to data reported among persons with lower back pain or diabetes mellitus.[9–13]
Of all people currently living with human immunodeficiency virus (HIV) globally, 9% of them reside in Nigeria.[14] Nigeria ranks fourth in the global burden of people living with HIV, with an estimated ~1.9 million people living with HIV and 51,000 AIDS-related deaths annually.[15–17] Research on the sexual health of women with HIV infection has generally focused on sexual practices and risk behaviors without giving sufficient consideration to sexual satisfaction and dysfunction. However, diminished sexual function among these women is associated with more severe HIV-related symptoms and a decrease in adherence to antiretroviral treatment.[18] There is also a dearth of data on this subject from Nigeria, despite an HIV prevalence of 1.4% among Nigerians aged 15–49 years.[19] In addition, there are currently no guidelines to manage sexual dysfunction in the HIV care setting in the country.
The Permission, Limited Information, Specific Suggestions, Intensive Therapy (PLISSIT) sexual counseling model is a simple and cost-effective intervention targeting women with sexual dysfunction that can be applied by physicians at the point of care.[20] PLISSIT offers a succinct method for introducing sex into a clinical conversation, narrowing the scope of a patient’s concern, and offering effective counseling and treatment. This model has reduced symptoms of sexual dysfunction and improved sexual satisfaction among women in a variety of settings.[20,21] However, the PLISSIT model has not been adapted for use in Nigeria or among women with HIV. The purpose of this pilot study was to determine the prevalence and patterns of FSD and assess whether the PLISSIT counseling model was effective in improving sexual function among a cohort of HIV-positive and HIV-negative women living in Nigeria.
METHODS
This was a prospective cohort study conducted at the general outpatient and HIV clinics of Aminu Kano Teaching Hospital (AKTH), Kano, Nigeria. AKTH is a 750-bed referral hospital serving a catchment population of more than 15 million people.[22]
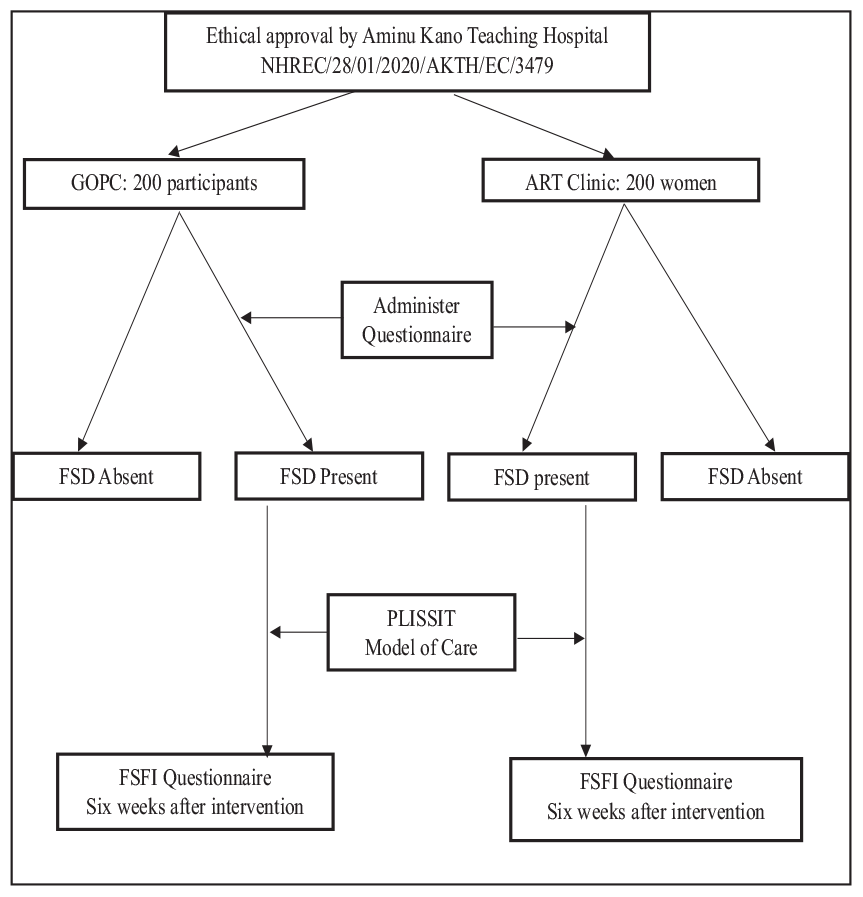
Female adults (aged 18–60 years) were recruited during their routine follow-up visits from June 2023 to August 2023. A total of 200 HIV-negative women were selected using a simple random sampling technique (balloting) from the general outpatient clinic, while another 200 HIV-positive women were similarly recruited from the HIV clinic. We excluded women with pregnancy, those with major psychiatric illnesses like major depression disorder, and those who reported no sexual activity in the past month by choice [Figure 1]. Written informed consent was obtained from all study participants. A table of random numbers was used to recruit the participants who met the inclusion criteria in both clinics.[23]
Prior to the commencement of the study, two female research assistants were trained on the use of the survey instrument, and ethical approval was obtained. We used a structured questionnaire and the Kobo Toolbox app for data collection.[24] The questionnaire had two parts: a demographics section and a Female Sexual Function Index (FSFI) section. The demographics section of the questionnaire captured personal information, including religion, marital status, parity, income, residence, and history of tobacco and alcohol use. There were also questions specific to FSD, specifically history of sexual trauma, sexual dysfunction in partners, and comorbidities among participants (i.e., hypertension, diabetes mellitus, sickle cell disease, asthma, and non-major psychiatric conditions). The FSFI contained 19 questions with five options that evaluated sexual desire, arousal, vaginal lubrication, orgasm, sexual satisfaction, and sexual pain.[25] The score of each domain was calculated by summing up the scores of each area, multiplied by the coefficient of each section. The coefficients are sexual desire (0.6), sexual arousal (0.3), vaginal lubrication (0.3), orgasm (0.4), sexual satisfaction (0.4), and sexual pain (0.4). The total FSFI score was obtained by summing the scores of all six domains. Scores range from 2 to 36. The higher the score, the better the sexual function. This tool has been used to validate data in Nigeria, a total FSFI score of =26.55 was used as a cutoff point to differentiate between women with sexual dysfunction and those without.[26,28] Scores below this threshold suggest the presence of sexual dysfunction in at least one domain.[27–29]
Participant recruitment was done concurrently in the HIV and outpatient clinics by trained research assistants who were fluent in the local Hausa language and conversant with the culture and customs of the area. The questionnaire was administered to participants in the local Hausa language in each clinic. Participants found to have FSD had individual counseling sessions based on the PLISSIT model. The number of counseling sessions for each individual was based on the participant’s type of sexual dysfunction.
All counseling sessions were performed by the research assistants (nurses), sexual health physician, and gynecologist (when needed). The PLISSIT counseling model was used in the following format:
The Permission component consisted of first obtaining permission from the patient to question them about their sexual dysfunction and showing openness to dialogue. The second step (Limited Information) was to provide information about the cause of sexual dysfunction, for example, lack of libido, pain, fatigue, vaginal dryness, anxiety, burden of HIV diagnosis, and so on. The third step (Specific Strategies) involved developing specific strategies for each problem. The last component (Intensive Therapy) involved implementing the treatment strategy previously discussed with the patient. Low sexual desire and anorgasmia were managed with medication, psychotherapy, and stress reduction. Sexual pain caused by vaginal dryness was managed with lubricating oils and intravaginal estrogen creams. Regarding pain and fatigue, it was recommended to practice different sexual positions, rest before intercourse, and use muscle relaxants or painkillers.
Subsequent counseling sessions were based on this format. The participants were offered medication and psychotherapy and referred to appropriate care, as indicated. Six weeks after the first counseling session, FSFI questionnaires were completed again by the participants. The patients continued to be seen after the study period.
Statistical Analysis
We computed the prevalence of FSD as the proportion of participants with FSD by HIV status. The statistical significance of the relationships between nominal and ordinal/categorical predictor variables was evaluated with the chi-square test of association. We used Student’s t-test or Wilcoxon rank-sum tests for comparisons of continuous variables. We used the mean FSFI scores for each of the six domains to compare the pattern of FSD by participant HIV status. The impact of the intervention on FSD was evaluated by subtracting mean FSFI scores before and after the intervention for each domain. All tests used a two-tail probability with p < 0.05 as statistically significant. The R statistical software (version 4.3.2) was used for all statistical analyses.[30]
Ethical Considerations
This study was approved by the ethics committee of Aminu Kano Teaching Hospital, reference number NHREC/28/01/2020/AKTH/EC/3479.
RESULTS
The overall prevalence of FSD among both groups was 96.8% (n = 387). The prevalence of FSD was 96.0% among women with HIV (n = 192) and 97.5% among women without HIV (n = 195). This difference was not statistically significant (p = 0.398). The majority of participants were between 25 and 44 years of age, married, of Hausa-Fulani ethnicity, and Muslim [Table 1]. The two groups were comparable in terms of demographic characteristics. History of hypertension, intimate partner violence, and male sexual dysfunction were more common among HIV-positive participants compared to participants without HIV [Table 1].
| Characteristic |
HIV-negative, N = 200 n (%) |
HIV-positive, N = 200 n (%) |
p-value |
| Age group, n (%) | 0.001* | ||
| 18–24 years | 15 (7.5%) | 36 (18.0%) | |
| 25–34 years | 57 (28.5%) | 55 (27.5%) | |
| 35–44 years | 82 (41.0%) | 52 (26.0%) | |
| 45–55 years | 42 (21.0%) | 47 (23.5%) | |
| >55 years | 4 (2.0%) | 10 (5.0%) | |
| Monthly income (NGN), n (%) | 0.020* | ||
| 0–29,000 | 188 (94.0%) | 176 (88.0%) | |
| 30,000–59,000 | 11 (5.5%) | 15 (7.5%) | |
| 60,000 and above | 1 (0.5%) | 9 (4.5%) | |
| Tribe, n (%) | 0.9 | ||
| Hausa-Fulani | 177 (88.5%) | 179 (89.5%) | |
| Yoruba | 4 (2.0%) | 5 (2.5%) | |
| Igbo | 2 (1.0%) | 1 (0.5%) | |
| Other | 17 (8.5%) | 15 (7.5%) | |
| Religion, n (%) | >0.9 | ||
| Islam | 190 (95.0%) | 191 (95.5%) | |
| Christianity | 8 (4.0%) | 7 (3.5%) | |
| Other | 2 (1.0%) | 2 (1.0%) | |
| Marital status | <0.001* | ||
| Single | 10 (5.0%) | 2 (1.0%) | |
| Divorced | 36 (18.0%) | 2 (1.0%) | |
| Married | 118 (59.0%) | 183 (91.5%) | |
| Widowed | 36 (18.0%) | 13 (6.5%) | |
| Parity, n (%) | <0.001* | ||
| Nulliparous | 26 (13.0%) | 39 (19.5%) | |
| Multiparous (2–5 children) | 117 (58.5%) | 78 (39.0%) | |
| Grand multiparous (>5 children) | 57 (28.5%) | 83 (41.5%) | |
| Medical comorbidities | |||
| Hypertension | 0.002* | ||
| No | 165 (82.5%) | 138 (69.0%) | |
| Yes | 35 (17.5%) | 62 (31.0%) | |
| Diabetes mellitus | 0.073 | ||
| No | 191 (95.5%) | 182 (91.0%) | |
| Yes | 9 (4.5%) | 18 (9.0%) | |
| Asthma | 0.812 | ||
| No | 194 (97.0%) | 193 (96.5%) | |
| Yes | 6 (3.0%) | 7 (3.5%) | |
| Sickle cell disease | >0.9 | ||
| No | 200 (100%) | 199 (99.5%) | |
| Yes | 0 (0%) | 1 (0.5%) | |
| Other comorbidities | 0.286 | ||
| No | 142 (71.0%) | 130 (65.0%) | |
| Yes | 58 (29.0%) | 70 (35.0%) | |
| None, n (%) | <0.001* | ||
| No | 82 (41.0%) | 117 (58.5%) | |
| Yes | 118 (59.0%) | 83 (41.5%) | |
| Education, n (%) | 0.137 | ||
| Primary | 52 (26.0%) | 41 (20.5%) | |
| Secondary | 84 (42.0%) | 87 (43.5%) | |
| Tertiary | 39 (19.5%) | 55 (27.5%) | |
| Others | 25 (12.5%) | 17 (8.5%) | |
| Residence, n (%) | 0.364 | ||
| Rural | 10 (5.0%) | 15 (7.5%) | |
| Urban | 190 (95.0%) | 185 (92.5%) | |
| Employment, n (%) | 0.911 | ||
| Employed | 17 (8.5%) | 18 (9.0%) | |
| Unemployed | 183 (91.5%) | 182 (91.0%) | |
| Alcohol use | 0.429 | ||
| No | 1 (0.5%) | 4 (2.0%) | |
| Yes | 199 (99.5%) | 196 (98.0%) | |
| Past sexual trauma | 0.761 | ||
| Yes | 2 (1.0%) | 4 (2.0%) | |
| No | 198 (99.0%) | 196 (98.0%) | |
| Partner’s sexual dysfunction | <0.001* | ||
| Absent | 191 (95.5%) | 171 (85.5%) | |
| Present | 9 (4.5%) | 29 (14.5%) | |
| Intimate partner violence | <0.001* | ||
| Absent | 183 (91.5%) | 148 (74.0%) | |
| Present | 17 (8.5%) | 52 (26.0%) | |
*Significant associations where p<0.05, n: Sample size, N: Total population, NGN: Naira.
The pattern of FSD based on the six domains of the FSFI was similar in both groups, as shown in Table 2. In both groups, the most common complaint was pain (92.3%), followed by disorders of sexual desire (85.3%), orgasmic disorders (85.0%), arousal disorders (72.8%), poor lubrication (67.8%), and low sexual satisfaction (48%).
| Pattern of sexual dysfunction | All participants n, % | HIV-positive | HIV-negative | ||
|
Dysfunction present n (%) |
Dysfunction absent n (%) |
Dysfunction present n (%) |
Dysfunction absent n (%) |
||
| Arousal | 291 (72.8%) | 147 (73.5%) | 53 (26.5%) | 144 (72.0%) | 56 (28.0%) |
| Desire | 341 (85.3%) | 172 (86.0%) | 73 (36.5.0%) | 169 (84.5%) | 31 (15.5%) |
| Lubrication | 271 (67.8%) | 127 (63.5%) | 53 (26.5%) | 144 (72.0%) | 56 (28.0%) |
| Orgasm | 340 (85.0%) | 167 (83.3%) | 33 (16.5%) | 173 (88.5%) | 27 (13.5%) |
| Satisfaction | 192 (48.0%) | 88 (44.0%) | 112 (56.0%) | 104 (52.0%) | 96 (48.0%) |
| Pain | 369 (92.3%) | 184 (92.0%) | 16 (8.0%) | 185 (92.5%) | 15 (7.5%) |
FSD: Female sexual dysfunction.
The average FSFI score among both groups prior to intervention was 16.05±10.65 (HIV positive: 18.58±8.46, HIV negative:13.98±10.85). The mean score of sexual function after the intervention increased to 23.58±16.53 (HIV positive: 21.37±11.24, HIV negative: 16.72±13.81). This change was statistically significant (p < 0.001).
DISCUSSION
FSD negatively affects the quality of life and physical well-being of women.[31] Studies on female sexual function are important, as they lead to improved awareness, and enable the institution of superior preventive measures and treatment modalities for FSD.[31,32] Studies of FSD among women living with HIV have focused mainly on sexual behavior. This study examined the prevalence of FSD in two groups of women—those living with HIV and those without HIV and assessed the effectiveness of an adaptive counseling care model in the management of FSD among women living with HIV in northern Nigeria.
The overall prevalence of FSD in both groups was found to be 96.8%, with no statistically significant difference by HIV status. This prevalence is much higher than reports from other settings, including Enugu, Southern Nigeria (53.5%),[32] Egypt (50.4%),[27] Iran (31.5%),[33] Saudi Arabia (60%),[34] Jordan (64%),[35] Cameroon (42%),[36] and the United States (43%).[37] A meta-analysis also found a lower prevalence of 40.9%.[38] A possible reason for this disparity in findings from our study could lie in the conservative nature of northern Nigeria, where open discussions about sexual problems and sex education are deemed taboo.[39,40] This cultural context may lead to less awareness of FSD as a problem, resulting in a reluctance to seek assistance. Not surprisingly, another study in the same environment revealed a much closer high prevalence of 86%,[3] reinforcing the influence of cultural factors on the recognition and reporting of sexual health issues in the region.
Based on the six domains of the FSFI, we found that the most common sexual dysfunctions were sexual pain (92%), sexual desire disorder (85.3%), and orgasm disorder (85%). A meta-analysis published in 2018 provided a broader perspective on the prevalence of sexual dysfunction across domains.[38] The estimates indicated a wide range of prevalence in each domain of sexual dysfunction: hypoactive desire disorder 28.2% [6%–70%]; sexual aversion disorder, [5%–24%] sexual arousal disorder 22.6% [1%–60%]; lubrication difficulties 20.6% [1%–53%]; female orgasmic disorder 25.7% [8%–72%]; and pain 20.8% [1%–72%].[38] While we did not examine the frequency of sexual activity, other studies that identified pain as their primary domain of FSD suggested less frequent exposure to sexual activity to be likely responsible. This explanation is supported by other studies that included women who had undergone circumcision, where pain also emerged as the predominant domain for sexual dysfunction.[39,40] These findings underscore the multifaceted nature of sexual dysfunction and its varied prevalence across different domains.
The PLISSIT sexual counseling model is a simple and cost-effective intervention targeting women with sexual dysfunction and can be implemented by physicians at the point of care.[41] Several studies have demonstrated the model’s effectiveness in alleviating symptoms of sexual dysfunction and improving sexual satisfaction among women in diverse settings.[42,43] However, despite its proven efficacy, the PLISSIT model has not been adapted for use among women with HIV in predominantly conservative northern Nigeria. The introduction and customization of the PLISSIT model could potentially fill this void, offering a tailored and culturally sensitive approach to sexual counseling for women living with HIV in Northern Nigeria.
In our study, the overall mean FSFI score for participants with FSD in both groups was initially 15.67. Following a six-week counseling intervention using the PLISSIT model, there was a statistically significant increase in the overall mean FSFI score to 23.58 [Table 3]. This finding is consistent with Abelhakm et al., who found statistically significant differences in mean scores on the Arizona Sexual Experiences Scale before and after implementing the PLISSIT model program.[41] Other studies that used the Arizona Sexual Experience Scale reported similar effectiveness of the PLISSIT model.[42–44] Torkzahrani et al. also demonstrated a statistically significant decrease in sexual problems among lactating women after using the PLISSIT model,[45] as did other studies that revealed post-intervention improvement in all the dimensions of sexual function[36–38] and in the sexual quality of life.[46–48]
| All participants | HIV-positive | HIV-negative | |||||||
| Sexual function | Before intervention | After intervention | p-value | Before intervention | After intervention | p-value | Before intervention | After intervention | p-value |
| Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | ||||
| Arousal | 2.49 (1.90) | 3.17 (0.82) | 0.016* | 3.28 (1.82) | 3.51 (2.01) | 0.002* | 2.13 (1.82) | 2.73 (0.86) | 0.014* |
| Desire | 2.82 (1.46) | 3.62 (0.62) | 0.001* | 2.99 (1.45) | 3.39 (1.42) | 0.012* | 2.66 (1.45) | 2.91 (1.44) | 0.015* |
| Lubrication | 2.70 (2.02) | 3.43 (0.72) | 0.003* | 3.22 (1.74) | 3.65 (0.63) | 0.003* | 2.31 (2.18) | 2.89 (0.92) | 0.002* |
| Orgasm | 2.77 (2.07) | 2.89 (0.71) | 0.067 | 3.35 (1.79) | 3.52 (0.67) | 0.052 | 2.31 (2.18) | 2.74 (0.76) | 0.015* |
| Satisfaction | 2.04 (1.37) | 5.23 (0.61) | 0.004* | 1.74 (1.53) | 2.61 (0.63) | 0.001* | 1.16 (1.44) | 1.79 (0.43) | 0.002* |
| Pain | 3.41 (2.64) | 5.24 (0.90) | 0.001* | 4.00 (2.33) | 4.69 (2.62) | 0.001* | 2.96 (2.81) | 3.66 (2.51) | 0.012* |
| Total | 16.05 (10.65) | 23.58(16.53) | <0.001 | 18.58 (8.46) | 21.37 (11.24) | <0.001 | 13.98 (10.85) | 16.72(13.81) | <0.001 |
*Statistically significant association. FSFI: Female sexual function index, SD: Standard deviation.
Our findings suggest that the PLISSIT model can be a practical guide for healthcare providers to initiate and navigate sexual health discussions. Sung et al.’s work further supports this notion, emphasizing the model’s utility in offering a structured approach for healthcare professionals to introduce sexual health topics, provide counseling, and implement interventions.[48] The PLISSIT model not only addresses the specific sexual health needs of women in Northern Nigeria but could also serve as a versatile tool for healthcare providers in fostering open and effective communication about sexual health.
Limitations
This study relies on interviewer-based data, which can be influenced by participants’ willingness to disclose sensitive information about sexual dysfunction, potentially leading to underreporting or overreporting. Furthermore, there may be other factors influencing the prevalence of FSD and the effectiveness of the PLISSIT model that were not controlled for, such as other contraceptive use, ART, and hormonal imbalance.
CONCLUSION AND GLOBAL HEALTH IMPLICATIONS
This study reveals that FSD is very common and often underreported among women visiting outpatient clinics. Through patient education, participants gain awareness that FSD is a common issue among women, which can reduce feelings of isolation and stigma. Incorporating the PLISSIT model into routine care by healthcare practitioners can provide a structured approach to addressing FSD, leading to better patient outcomes. Policymakers should prioritize the development of guidelines and policies that include routine screening and management of FSD in women with HIV. Additionally, allocating resources to train healthcare providers in the PLISSIT model and other effective interventions can improve care quality. Further research should be supported to explore the long-term benefits of the PLISSIT model and other interventions for FSD in diverse populations of women with and without HIV.
Key Messages
The study reveals a strikingly high prevalence of female sexual dysfunction (FSD) among women with and without human immunodeficiency virus (HIV), highlighting a critical and often overlooked health issue in this population.
Implementing the Permission, Limited Information, Specific Suggestions, Intensive Therapy (PLISST) model of care can significantly improve symptoms of female sexual dysfunction, suggesting that it is a valuable and effective management strategy for women with and without human immunodeficiency virus.
Training healthcare providers on the Permission, Limited Information, Specific Suggestions, Intensive Therapy (PLISST) model and other effective interventions for female sexual dysfunction is essential to enhance care delivery and patient outcomes.
Acknowledgments
We wish to acknowledge the bravery of our participants, who shared their intimate challenges with us. This study would not be possible without them.
COMPLIANCE WITH ETHICAL STANDARDS
Conflicts of Interest
Dr. Hamisu Salihu is on the editorial board of Int J MCH AIDS.
Financial Disclosure
This research was supported by the National Institutes of Health (NIH). The content is solely the responsibility of the authors and does not necessarily represent the official view of the NIH, the Department of Health and Human Services or the United States government.
Funding/Support
This work is supported by the Fogarty International Center (FIC) and the National Institute on Alcohol Abuse and Alcoholism (NIAAA) of the U.S. National Institutes of Health (NIH) award number 1D43TW011544. The findings and conclusions are those of the authors and do not necessarily represent the official position of the FIC, NIAAA, NIH, the Department of Health and Human Services, or the government of the United States of America.
Ethics Approval
The research/study was approved by the Institutional Review Board at Aminu Kano Teaching Hospital, number NHREC/28/01/2020/AKTH/EC/3479, dated January 27, 2023.
Declaration of Participant Consent
Informed consent was obtained in a written form from all study participants.
Use of Artificial Intelligence (AI)-Assisted Technology for Manuscript Preparation
The authors confirm that there was no use of AI-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
This research was supported by the National Institutes of Health (NIH) under award number [1D43TW011544] The content of this article is solely the responsibility of the authors and does not necessarily represent the official view of the NIH, nor does it constitute a product endorsement by the NIH.
REFERENCES
- Prevalence of female sexual dysfunction symptoms and its relationship to quality of life: A Japanese female cohort study. Urology.. 2005;65:143-8.
- [CrossRef] [PubMed] [Google Scholar]
- Female sexual health: Barriers to optimal outcomes and a roadmap for improved patient–clinician communications.J Women’s Health.. 2019;28((4)):432-43.
- [CrossRef] [PubMed] [PubMed Central]
- Female sexual dysfunction among women attending the family planning clinic at Aminu Kano Teaching Hospital: A cross-sectional survey. Niger J Basic Clin Sci.. 2019;16:32-7.
- [CrossRef] [Google Scholar]
- Why is impaired sexual function distressing to women? The primacy of pleasure in female sexual dysfunction. J Sex Med.. 2015;12((3)):728-37.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Female sexual dysfunction: Prevalence and risk factors. J Clin Diagn Res.. 2013;7:2877-80.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Incidence of sexual dysfunction: A prospective survey in Ghanaian females. Reprod Biol Endocrinol.. 2010;8:106.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Sexual dysfunction in women: An overview of risk factors and prevalence in Indian women. J South Asian Feder Obst Gynae.. 2012;4:134-6.
- [Google Scholar]
- Prevalence of sexual dysfunction in women: Results of a survey study of 329 women in an outpatient gynecological clinic. J Sex Marital Ther.. 1993;19:171-88.
- [CrossRef] [PubMed] [Google Scholar]
- EQ-5D and the EuroQol group: Past, present and future. Appl Health Econ Health Policy.. 2017;15:127-37.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Comparing the reliability and validity of the SF-36 and SF-12 in measuring quality of life among adolescents in China: A large sample cross-sectional study. Health Qual Life Outcomes.. 2020;18((1)):360.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Hypoactive sexual desire disorder in postmenopausal women: Quality of life and health burden. Value Health.. 2009;12:763-72.
- [CrossRef] [PubMed] [Google Scholar]
- Correlates of sexual activity and satisfaction in midlife and older women. Ann Fam Med.. 2015;13:336-42.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Female sexual dysfunction (FSD): Prevalence and impact on quality of life (QoL). Maturitas.. 2016;94:87-91.
- [CrossRef] [PubMed] [Google Scholar]
- HIV AIDS Epidemic Control Report Q2 June 2023. Available from: https://www.phis3project.org.ng/phis3-resources/hiv-aids-epidemic-control-report-june-2023/
- [Google Scholar]
- Nigeria HIV/AIDS Indicator and Impact Survey (NAIIS) 2018: Technical Report. Abuja, Nigeria. Oct [cited 2022 Aug 24]. Available from: https://www.ciheb.org/media/som/microsites/ciheb/documents/NAIIS-Report-2018.pdf
- [Google Scholar]
- Number of Deaths Due to Aids in Nigeria as of 2021 (in 1,000s). Statista, Statista Inc.. [cited 2022 Aug 24]. Available from: https://www.statista.com/statistics/1262130/deaths-due-to-aids-in-nigeria/?
- [Google Scholar]
- Sexual health for people living with HIV. Reproductive Health Matt.. 2007;15((29)):67-92.
- [CrossRef] [PubMed] [Google Scholar]
- Sexual dysfunction and its determinants among women infected with HIV. Int J Gynecol Obstetr.. 2017;137((3)):301-8.
- [CrossRef] [PubMed] [Google Scholar]
- Sexual counseling with the PLISSIT model: A systematic review. J Sex Mar Ther.. 2022;48((3)):309-18.
- [CrossRef] [PubMed] [Google Scholar]
- The effect of sexual counseling based on PLISSIT model on improving the sexual function of married women with systemic lupus erythematosus: A randomized controlled trial. Sex Disability.. 2023;41((2)):451-66.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Outcomes and barriers to cervical cancer screening among human immunodeficiency virus-positive women attending aminu kano teaching Hospital, Kano State, Nigeria. Dutse Journ Pur and Appl Sci.. 2023;9((4b)):1-10.
- [CrossRef] [Google Scholar]
- New method of data collection using the kobo toolbox. J Positive Sch Psychol. 2022:1527-35.
- [Google Scholar]
- The Female Sexual Function Index (FSFI)—a systematic review of measurement properties. J Sex Med.. 2019;16((5)):640-60.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence of sexual dysfunction among females in a university community in Enugu, Nigeria. Niger J Clin Pract.. 2014;17:791-6.
- [CrossRef] [PubMed] [Google Scholar]
- Sexual dysfunction among women in a Nigerian gynecological outpatients unit. Trop J Obstetr Gynaecol.. 2019;36((1)):61-6.
- [Google Scholar]
- Scoring and interpretation of the FSFI: What can be learned from 20 years of use? J Sex Med.. 2020;17((1)):17-25.
- [CrossRef] [PubMed] [Google Scholar]
- Data analysis with R statistical software. A guidebook for scientists. 2013 Eco-explore;
- [Google Scholar]
- The prevalence of sexual dysfunctions and sexually related distress in young women: A cross-sectional survey. Fertility Sterility.. 2020;113((2)):426-34.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence of female sexual dysfunction among five hundred women at the childbearing period in upper Egypt: A cross sectional study. IJMA.. 2022;4((6)):2456-62.
- [CrossRef] [Google Scholar]
- Female sexual dysfunction in a population-based study in Iran: Prevalence and associated risk factors. Int J Impot Res.. 2006;18((4)):382-95.
- [CrossRef] [Google Scholar]
- Prevalence and predictive factors of female sexual dysfunction in a sample of Saudi women. Sex Med.. 2021;9((1)):100277.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Prevalence and associated risk factors of female sexual dysfunction among Jordanian women. J Family Med Prim Care.. 2018;7((6)):1488-92.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Prevalence and associated factors of female sexual dysfunction among sexually active students of the University of Buea. Sex Med.. 2021;9((5)):100402.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Predictors of female sexual dysfunction: A systematic review and qualitative analysis through gender inequality paradigms. BMC Womens Health.. 2018;18:108.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Prevalence of sexual dysfunction among reproductive-age women in Iran: A systematic review and meta-analysis. J Midwifery Reprod Health.. 2018;6((3)):1296-304.
- [Google Scholar]
- Sexual dysfunction and infertility amongst spouses in Adamawa state, Nigeria. Am J Health Res.. 2021;9:1-8.
- [Google Scholar]
- Female sexual dysfunction: Prevalence and risk factors. J Clin Diagn Res.. 2013;7:2877-80.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Effect of PLISSIT model sexual counseling program on sexual quality of life for postpartum women. Am J of Nursing Sci.. 2018;7((2)):63-72.
- [CrossRef] [Google Scholar]
- Effect of PLISSIT model sexual health enhancement program for women with gynecologic cancer and their husbands. J Korean Acad Nurs.. 2013;43((5)):681-9.
- [CrossRef] [PubMed] [Google Scholar]
- Effectiveness of application of PLISSIT counseling model on sexuality for breast cancer’s women undergoing treatment, Egypt. Am J Nurs Sci.. 2015;4((4)):218-30.
- [Google Scholar]
- The prevalence of female sexual dysfunction among migraine patients. Iran J Neurol.. 2015;14((1)):8-11.
- [PubMed] [PubMed Central] [Google Scholar]
- The effectiveness of consultation based on PLISSIT Model on sexual function of lactating women, Iran. J Urmia Nurs Midwifery Fac.. 2016;14((7)):639-46.
- [Google Scholar]
- Effects of sexual rehabilitation using the PLISSIT model on quality of sexual life and sexual functioning in post-mastectomy breast cancer survivors. Asian Pacific J Cancer Prev.. 2016;17((11)):4849.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Female sexual dysfunction and the placebo effect: A meta-analysis. Obstetr Gynecol.. 2018;132((2)):453-8.
- [CrossRef] [PubMed] [Google Scholar]
- Sexual health care for women with dyspareunia, Taiwan, Taiwanese. J Obstetr Gynaecol.. 2011;50:268-74.
- [CrossRef] [PubMed] [Google Scholar]






