Translate this page into:
Access to and Utilization of Maternal and Child Healthcare Services During COVID-19 Pandemic in Rural Bangladesh

Corresponding author: Md. Matiur Rahman, TMSS, TMSS Foundation Office, Thengamara, Bogura, Bangladesh. Tel: +8801713377022 dr_matiur@yahoo.com
-
Received: ,
Accepted: ,
How to cite this article: Rahman MM, Bin Siddique MK, Rahman A, Islam R, Rahim MMU. Access to and Utilization of Maternal and Child Healthcare Services During COVID-19 Pandemic in Rural Bangladesh. Int J MCH AIDS. 2024;13:e018. doi: 10.25259/IJMA_612
Abstract
Background and Objective
Geographically remote areas in lower-middle-income countries like Bangladesh experienced significant Maternal and Child Health (MCH) care shortages during the COVID-19 pandemic. These shortages were exacerbated by preexisting inadequate public health infrastructure and using existing health resources for pandemic management. The objective of this study was to assess the status of access to and utilization of maternal and child healthcare services among rural people during the outbreak of COVID-19.
Methods
A community-based descriptive, exploratory, cross-sectional study was carried out from May to August 2020 among the rural people of the four districts of northern Bangladesh. A total of 639 women were included in the study with a sample random sampling technique, and multistage random sampling techniques were applied to select the study area. A pretested semi-structured questionnaire was used for data collection. SPSS Version 22 was used for the statistical analysis.
Results
The mean age of the respondents was 34.3 years with an SD ± 10 years. 37.7% of respondents belonged to the 21–30 year age group followed by the 31–40 years age group (34.9 %). Of the total 639 respondents, 59.5% were female. There were significant associations and moderate positive correlations between educational qualification, occupational status, and age group of the respondents (p=0.001). Most of the respondents (67.6%) indicated that they experienced health problems during COVID-19 with 70.6% of them specifically mentioning MCH-related problems. Out of them, only 33.1% mentioned they could access and utilize MCH services, whereas 66.9% of them could not access MCH Services. Major barriers to utilizing MCH services were the COVID-19 lockdown, lack of transport facilities, fear of being infected, shutdown of healthcare facilities, and unavailability of healthcare professionals. The differences in health facility usage before and during COVID-19 are statistically significant with p = < 0.001.
Conclusion and Global Health Implications
During the COVID-19 pandemic, access to and utilization of MCH services was significantly hampered, particularly in Bangladesh’s remote and rural regions during the strict lockdown times. The identified barriers were the COVID-19 lockdown, lack of transport facilities, fear of being infected, shutdown of healthcare facilities, and unavailability of healthcare professionals. Building strengthened health systems, capacity building of informal healthcare providers, backup plans, and alternate service delivery models are necessary to ensure access to maternity and child health.
Recommendations
For future pandemics and natural disaster situations, the ‘concerned officials should strategically have backup plans and alternative service delivery models to strengthen the health system. And, there should be collaborative efforts among the countries to support each other to address the crisis situations.
Keywords
COVID-19
Access and Utilization of MCH Service
Rural Communities
Bangladesh
Healthcare Access
Service Utilization
Healthcare Accessibility
INTRODUCTION
The World Health Organization (WHO) announced the COVID-19 pandemic as a global health crisis. Since then, more than 622 million people have been infected with the novel coronavirus and over 6.5 million have lost their lives, according to the latest data available as of 29 September 2022.[1] Maternal and child health (MCH) is one of the important components of essential healthcare service. As essential healthcare services were hampered due to COVID-19, the MCH services were also hampered, between March and May 2020, and there was a reduction in access and utilization of basic essential MCH services such as antenatal care, postnatal care family planning, and immunization due to the implementation of the lockdown which triggered fear of contracting COVID-19 and deterred people from accessing basic MCH care.[2] A 17–43% increase in maternal fatalities during the COVID–19 pandemic was predicted by retrospective case series model.[3] Bangladesh faced many challenges in containing the disease and ensuring the availability of MCH services. The country had to cope with limited resources, inadequate infrastructure, and social barriers that affected the health outcomes of mothers and children.[4] The authorities advised the public to avoid hospital visits in the initial phase of the outbreak unless they were critically necessary. This recommendation also applied to pregnant women, who faced additional risks of exposure and complications.[5] Continuous lockdown, fear of getting infected with COVID-19, and massive disruption in the provision of maternal health services (such as antenatal and postnatal care) negatively impacted the MCH services.[6,7] Also, the institutional delivery rate significantly decreased in Bangladesh.[8]
These disruptions pushed back many low- and middle-income countries’ (LMICs) endeavors to ensure safe institutional deliveries.[9] An additional 6,000 children could die worldwide every day from preventable causes over the next 6 months as the COVID-19 pandemic continues to weaken health systems and disrupt routine services.[10] In Bangladesh too, the uptake of critical health services for children under 5 years of age has significantly decreased due to the COVID-19 pandemic. The service utilization for children under 5 years of age in March 2020 was down 25% compared to March 2019.[10] The COVID-19 pandemic has not only ravaged the economic metrics in Bangladesh but has also led to indirect and long-term health adversities manifested as starvation, malnutrition, and MCH hazards. These are threatening to alter progress in the associated socioeconomic indicators.
According to WHO, Bangladesh has the second-lowest doctor-to-patient ratio in South Asia, with 5.26 per 10,000 inhabitants. Adding fuel to the fire, most hospitals suspended MCH services during the pandemic. Amid the lockdown, and fear of community transmission, private hospitals and clinics stopped providing any services to the public.[2] During COVID-19, 2.4 million expected births were estimated in Bangladesh, and pregnant mothers and babies born were threatened by disruptions in MCH services.[11]
Shortage of healthcare facilities, service providers, fear, and social factors such as transport, education, family, and stigma, there is limited MCH services access in Bangladesh.[12,13]
The COVID-19 pandemic has worsened the already precarious situation of rural women who need maternity healthcare services. Many of them face barriers such as distance, cost, and lack of quality care in their areas. The lockdowns and travel restrictions have made it even harder for them to access the essential services they need during pregnancy and childbirth.[14]
This study, therefore, assessed the status of access to and utilization of maternal and child healthcare services during COVID-19 among the rural people of Northern Bangladesh.
METHODS
Study Setting
There are two divisions and 16 administrative districts in northern Bangladesh. Of these 16 districts, the researcher considered four (or 25%) of them: Bogura, Gaibandha, Joypurhat, and Naogaon. These four districts are located in the northern divisions of Rajshahi and Rangpur. According to the Bangladesh Bureau of Statistics, there are 19,139,424 more females than men in these two divisions’ a combined population of 37,947,943 (BBS, 2022).
Study Design and Period
A community-based, exploratory, cross-sectional survey was undertaken to determine the status of access to and utilization of mother and child healthcare during COVID-19 in rural parts of Northern Bangladesh. The research was conducted during the first wave of the COVID-19 pandemic, when the country was under lockdown (May 2020 to August 2020).
Population and Recruitment Procedure
A face-to-face survey was used to interview a carefully selected sample of people. The study included Bangladeshi nationals aged 18 and above who were clients of the Thengamara Mohila Sabuj Sangha (TMSS) Healthcare Center, which provides essential healthcare services to the community. We confirmed their eligibility by asking about their birth year and national identity card possession, which is only available to Bangladeshis over 18. Participants who were physically or mentally ill or declined to take part in the study were excluded.
Sample Size Determination
During the COVID pandemic lockdown, we estimated that 50% (p=0.05) of the population had access to medical services, based on a representative sample of 384 with 95% confidence and 5% precision levels. Adjusting for the 1.5 design impact and the 20% nonresponse rate, the sample sizes were increased to 576 and 720, respectively. We selected 720 qualified participants from 4 districts (unequally distributed): Bogura (31.6%), Gaibandha (26.3%), Naogaon (24.5%), and Joypurhat (17.6%). Of these, 645 consented to participate, while 75 declined. After removing incomplete interviews, a total of 639 completed interviews were used for the study. The investigation utilized multistage sampling, with four randomly chosen districts, two upazilas from each district, and two union parishads from each upazila, resulting in data collection from 16 union parishads.
Data Collection
The study used a pretested, semi-structured questionnaire for personal interviews with research participants, ensuring compliance with the Bangladeshi government and WHO COVID guidelines. The lead investigator and supervisors monitored data accuracy and consistency daily. The questionnaire had two parts: the first focused on sociodemographic factors such as age, gender, education, employment, residence, religion, marital status, household size, living arrangements, and income. The second part addressed access and utilization of MCH services during the COVID lockdown, including health issues, access to healthcare facilities, and reasons for low accessibility.
Data Quality Assurance
The research objectives guided the design of the data collection instruments, which were partly based on standard questionnaires to ensure data quality. Two experts in the field validated the questionnaire before the final version was administered to the respondents. The data collection and supervision team consisted of 13 registered nurses who received 3 days of training. A pretest was conducted with 10% of the sample in a rural area before the actual data collection. The principal investigator monitored the whole process closely. The interview was conducted in the native language for better comprehension.
Statistical Analysis
Data were entered, cleaned, and analyzed using SPSS version 22 software (IBM Corp. Released 2013. IBM SPSS Statistics for Windows, Version 22.0. Armonk, NY: IBM Corp.). Percentages, frequencies, charts, and cross-tabulations were used to describe the significant characteristics of respondents. Chi-Square and Pearson correlation (linear regression) analyses were done to observe any association and correlation among the variables.
Ethical Approval
The Ethical Review Committee (ERC) of the TMSS Medical College (TMC) in Bogura, Bangladesh, approved the research protocol, questionnaire, consent statement, and ways to get informed consent. The ERC reference number is 2020/01. At the beginning of the interview, written consent was taken from the respondents after conveying that complete confidentiality of personal data would be strictly maintained. Each person who took part in the study was also told why they were taking part and that they could choose not to and could leave the interview at any time before the survey. Face-to-face interviews were done while keeping a safe distance and taking safety precautions. There was first-aid care available in case of an emergency situation. Cramer’s V test builds upon the X2 test by quantifying the strength of the association between the two categorical variables. It provides a value between 0 and 1. Higher Cramer’s V values indicate a stronger association between the variables; 0.1 weak association, 0.3 moderate association, 0.5 strong association.
RESULTS
Sociodemographic Characteristics of the Participants
A comprehensive overview of the sociodemographic characteristics of the participants and their relationships with each other is provided in Table 1. The participants were 639 people from different age groups, genders, religions, marital statuses, educational qualifications, occupational statuses, family heads, family types, household sizes, and families having children under five years of age. The table also shows the results of the X2 test, Cramer’s V, and Pearson correlation (linear regression) for some of the characteristics. The Table 1 reveals some important findings, such as:
-
-
The majority of the participants were aged between 21 and 40 years (72.6%), female (59.5%), Muslim (92%), married (89.8%), and lived in nuclear families (80%).
-
-
The most common educational qualification was primary education (26.8%), followed by junior school certificate (21.4%) and secondary school certificate (17.7%). Only 14% of the participants had higher education (honors, master’s, and above).
-
-
The most common occupational status was a housewife (46.3%), followed by a service holder (21.4%) and business (11.9%). Only 0.8% of the participants were physicians/nurses/health workers.
-
-
The majority of the participants had male family heads (90%) and medium-sized families (4–6 members) (62%). Only 39% of the participants had a child under five years of age in their family.
-
-
Educational qualification had a significant association with occupational status (X2 = 13.762, df = 6, p = 0.032) and a moderate positive correlation with the age group of the respondents (Cramer’s V = 0.344).
-
-
Occupational status had a significant association with educational qualification (X2 = 22.763, df = 7, p = 0.002) and a moderate positive correlation with the age group of the respondents (Cramer’s V = 0.441).
| Characteristics | Frequency | Percent | X2 Test | Cramer’s V | Pearson Correlation |
|---|---|---|---|---|---|
| Age Group of the Respondents | |||||
| <21 | 46 | 7.2 | - | - | 0.004 p = 0.458 |
| 21–30 | 241 | 37.7 | |||
| 31–40 | 223 | 34.9 | |||
| 41–50 | 95 | 14.9 | |||
| 51–60 | 24 | 3.8 | |||
| >60 | 10 | 1.6 | |||
| Gender of the Respondents | |||||
| Male | 259 | 40.5 | - | - | 0.008 p = 0.419 |
| Female | 380 | 49.5 | |||
| Religious Status of the Respondents | |||||
| Muslim | 588 | 92.0 | - | - | 0.011 p = 0.390 |
| Hindu and Others | 51 | 8.0 | |||
| Marital Status of the Respondents | |||||
| Single | 48 | 7.5 | - | - | 0.004 p= 0.457 |
| Married | 574 | 89.8 | |||
| Divorced | 3 | .5 | |||
| Widowed | 11 | 1.7 | |||
| Separated | 3 | .5 | |||
| Educational Qualification of the Respondents | |||||
| Illiterate | 62 | 9.7 |
X2 = 13.762 df = 6 p = 0.032 |
0.344 | 0.089 p = 0.012 |
| Primary | 171 | 26.8 | |||
| Junior School Certificate | 137 | 21.4 | |||
| Secondary School Certificate | 113 | 17.7 | |||
| Higher Secondary Certificate | 67 | 10.5 | |||
| Honors | 60 | 9.4 | |||
| Masters and above | 29 | 4.6 | |||
| Occupational Status of the Respondents | |||||
| Service Holder | 137 | 21.4 |
X2 = 22.763 df = 7 p = 0.002 |
0.441 | - |
| Physician/Nurse/Health Worker | 5 | 0.8 | |||
| Business | 76 | 11.9 | |||
| Farming | 43 | 6.7 | |||
| Day Labor | 20 | 3.1 | |||
| Unemployed | 15 | 2.3 | |||
| Housewife | 296 | 46.3 | |||
| Student | 33 | 5.2 | |||
| Others | 14 | 2.2 | |||
| Family Head | |||||
| Male | 575 | 90 | - | - | - |
| Female | 64 | 10 | |||
| Family Type | |||||
| Nuclear Family | 511 | 80 | - | - | - |
| Joint Family | 128 | 20 | |||
| Household Size | |||||
| Small Family (1–3 Members) | 196 | 30.7 | - | - | - |
| Medium Family (4–6 Members) | 396 | 62 | |||
| Large Family (≥7 Members) | 47 | 7.4 | |||
| Family Having Child Under Five Years of Age | |||||
| Yes | 248 | 39 | - | - | - |
| No | 391 | 61 | |||
df: Degree of freedom
Type of Health Problems Experienced During COVID-19
The majority (67.6%) of respondents reported experiencing health issues during COVID-19, with 70.6% of them specifically mentioning MCH-related problems. They also indicated the need to visit a health facility for MCH services during the pandemic [Table 2].
| Characteristics | Frequency | Percent |
|---|---|---|
| Status of experiencing health problems during the COVID period (n = 639) | ||
| Yes | 432 | 67.6% |
| No | 207 | 32.4% |
| Status of experiencing maternal and child health problems during the COVID period (n = 432) | ||
| Yes | 305 | 70.6% |
| No | 127 | 29.4% |
| Types of maternal and child health–related issues or problems* (n = 305) | ||
| ANC services | 142 | 46.6% |
| PNC services | 103 | 33.7% |
| Childhood immunization | 87 | 28.5 % |
| Delivery services | 45 | 17.8% |
| Treatment of childhood illness | 117 | 38.4% |
| Family planning | 109 | 35.7% |
| Postabortion care | 12 | 03.9% |
| Neonatal care | 36 | 11.8% |
| Others | 71 | 23.3% |
| Access to MCH facilities during COVID-19 (n = 305) | ||
| Access to MCH facilities | 101 | 33.1% |
| Could not access MCH facilities | 204 | 66.9% |
Nearly half (46.6%) of the respondents required ANC services, followed by 33.7% needing PNC and 17.8% seeking delivery services. In addition, 35.7% visited health facilities for family planning–related services. Children’s immunization was needed by 28.5% of respondents, while childhood illness and neonatal care were reported by 38% and 11% of respondents, respectively. Postabortion care was required by 4% of respondents [Table 2].
Status of Access to and Utilization of MCH Service
The majority of respondents (27.4%) reported being unable to access MCH services due to the COVID lockdown, followed by 24% citing lack of transportation and 18% expressing fear of contracting COVID-19 [Figure 1].
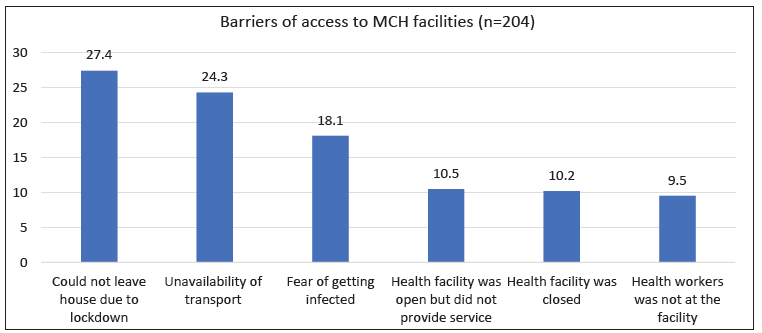
- Barriers of access to maternal and child health (MCH) facilities during COVID-19 (n = 305; Yes = 101; No = 204).
Ten percent of the population reported that the healthcare facility was closed, while a similar number of respondents (10%) stated that facilities were open but did not provide services. In addition, almost the same number of respondents mentioned that service providers were not available at the facility to provide MCH-related services [Table 2].
Before COVID-19, the majority of respondents (72% and 85.3%) had access to community clinics and government hospitals for MCH services, but during COVID-19, this decreased to 36% and 46%, respectively [Figure 2]. Conversely, more than half of the respondents visited informal healthcare providers for MCH services. The differences in health facility usage before and during COVID-19 are statistically significant with p = <0.001.
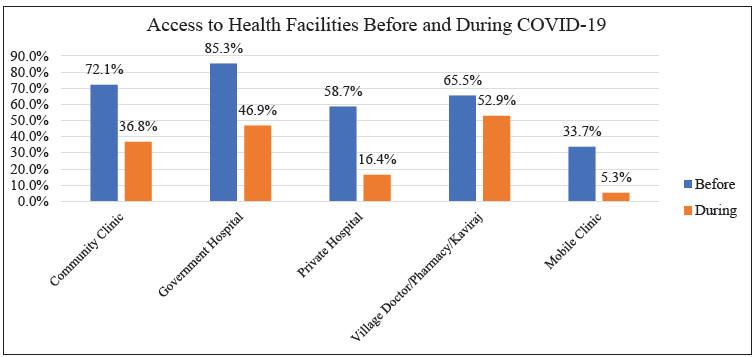
- Comparison of access to health facilities before and after the onset of COVID-19.
DISCUSSION
This study investigated the accessibility and utilization of maternal and child healthcare services among rural populations during the COVID-19 pandemic. It revealed that 67.6% of respondents encountered issues accessing health services, with 70.6% lacking access to MCH services. Factors such as inequity, education, occupation of the mother and her partner, household income, adherence to COVID-19 preventive measures, and pre-COVID maternity service use were all linked to a reduced likelihood of utilizing maternal health services during the COVID-19 restrictions.
In this study, MCH services encompass ANC, PNC, immunization, delivery, child illness, family planning, and abortion services. The findings of this study align with those of similar studies conducted in comparable contexts.[13] During COVID-19, the majority of these services were declined in India[15] and Pakistan.[16] The same patterns of disruption and reduction in the use of MCH services were observed in other countries, such as Haiti, Lesotho, Liberia, Malawi, Mexico, and Sierra Leone. These countries experienced challenges on both the supply side (e.g., availability of health workers, commodities, and facilities) and the demand side (e.g., accessibility, affordability, and acceptability of services) of the health system.[17] Access to MCH services is hindered by several factors during the COVID-19 lockdown. These include limited transport options, infection risk, unavailability of health facilities, and scarcity of health professionals. A similar situation was reported in a rural Nigerian study.[13,18,19] The utilization of MCH service was impeded by several factors, according to another study. These factors included fear of infection, lack of transportation, and financial constraints.[20]
The COVID-19 pandemic had a negative impact on the availability and use of maternal and child healthcare services, according to this study. The accessibility rate of community clinics dropped from 72.13% before the pandemic to 36.84% during the pandemic. Government hospitals also saw a decline from 85.30% to 46.90%, while private hospitals or clinics faced a similar challenge. These findings suggest reduced access to and utilization of essential healthcare services for mothers and children during the COVID-19 crisis. Many people prefer to consult local and informal health providers, such as village doctors and Kabiraj (informal healthcare provider), instead of formal ones. They are afraid of being exposed to COVID-19 if they visit official facilities,[21] unavailability of doctors and private and public transport, and decreased family income were other factors, were supported by another study.[11,22] Similarly, countries like India (20.1 million), China (13.5 million), Nigeria (6.4 million), Pakistan (5 million), and Indonesia (4 million) witnessed low birth rate during the pandemic and most of these countries had high neonatal mortality rates even before the pandemic and may see these levels increase with COVID-19 conditions.[23]
The COVID-19 pandemic significantly disrupted access to MCH services. This study investigated the challenges and barriers to accessing these services, including emergency care. It also emphasized the importance of preparedness, collaboration between the government and private sector, and global partnerships in addressing the impact of the COVID-19 pandemic and future pandemics. Previous research has consistently shown that maternal and partner education positively influences the uptake of health services.[24,25] In a similar vein, financially independent mothers and spouses are less likely to face barriers to service access.[24,25] Mothers from higher-income homes, who are more likely to be able to afford transportation and medical expenses, are similarly affected.[25]
The utilization of maternal health services during any upcoming pandemic could be improved by empowering mothers, raising awareness about COVID-19 prevention, 13 and strengthening the health system. Informal healthcare service providers should also provide training in fundamental infection prevention and control with referral connections to medical facilities. 25
Strengths and Limitations of the Study
It is important to note that this is a rapid study conducted during the COVID-19 lockdown. Data were collected by trained healthcare professionals of TMSS. Further mixed-method studies will be needed to explore the in-depth situations and challenges in access to and utilization of maternal child healthcare services.
CONCLUSION AND GLOBAL HEALTH IMPLICATIONS
During the COVID-19 pandemic, there were MCH care shortages in geographically isolated areas of lower-middle-income nations like Bangladesh. In northern Bangladesh, MCH service utilization decreased during COVID-19. Major barriers to utilizing MCH services were the COVID-19 lockdown, lack of transport facilities, fear of being infected, shutdown of healthcare facilities, and unavailability of healthcare professionals. Building strengthened health systems, capacity building of rural informal healthcare providers, backup plans, and alternate service delivery models is necessary to ensure access to maternity and child health without restriction services for upcoming pandemics. Moreover, all the countries should work collaboratively to address future crisis situations, as the world is now considered as a global village.
Key Messages
-
o
During COVID-19, access to and utilization of maternal and child healthcare services was hindered due to structural barriers, lack of experience, and lack of preparedness in the health system.
-
o
Global partnership, government–private sector collaboration, emergency management, and early preparedness are essential to address COVID-19 like a large-scale pandemic.
-
o
Capacity-building of informal healthcare providers for providing emergency service and referrals.
Acknowledgments
The authors would like to thank all the staff of TMSS for their support in conducting this study. The authors would like to acknowledge Prof. Dr. Hosne Ara Begum, PhD, Prof. Dr. Moudud Hossain Alamgir Pavel, and other colleagues at the Health Sector, TMSS for their advisory support. The authors are grateful to all the participants who provided valuable data for this study.
COMPLIANCE WITH ETHICAL STANDARDS
Conflicts of Interest
The authors declare no competing interests.
Financial Disclosure
Nothing to declare.
Funding/Support
There was no funding for this study.
Ethics Approval
This study was approved by the Institutional Ethical Review Committee of the TMSS Medical College, Bogura, Bangladesh number (2020/01).
Declaration of Patient Consent
Patient’s consent is not required as there are no patients in this study.
Use of Artificial Intelligence (AI)-Assisted Technology for Manuscript Preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
None.
References
- COVID-19 coronavirus pandemic. Published 2023 Apr 15. [Accessed 2023 Apr 15]. Available from: https://www.worldometers.info/coronavirus/
- The effect of COVID-19 on maternal newborn and child health (MNCH) services in Bangladesh, Nigeria and South Africa: Call for a contextualised pandemic response in LMICs. Int J Equity Health. 2021;20(1):77.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Maternal death due to COVID-19. Am J Obstet Gynecol. 2020;223(1):109.e1-109.e16.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Where do women birth during a pandemic? changing perspectives on safe motherhood during the COVID-19 pandemic. Journal of Global Health Science. 2020;2(1)
- [CrossRef] [Google Scholar]
- It’s the Destination and the journey—a mapping of the challenges in transport and referral for maternal and newborn health in pandemics and beyond. Front Public Health. 2021;9:612409.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Effective interventions to ensure MCH (Maternal and Child Health) services during pandemic related health emergencies (Zika, Ebola, and COVID-19): A systematic review. PLoS One. 2022;17(5):e0268106.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Fear of rise in maternal mortality looms large _ undefined. The business standard. published online 2020. [Accessed April 17, 2023]. Available from: https://www.tbsnews.net/bangladesh/health/fear-rise-maternal-mortality-looms-large-154096
- Effects of COVID-19 on maternal institutional delivery: Fear of a rise in maternal mortality. J Glob Health. 2021;11:1-3.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- As COVID-19 devastates already fragile health systems, over 6,000 additional children under five could die a day, without urgent action. [Accessed 2023 Apr 15]. Available from: https://www.unicef.org/press-releases/covid-19-devastates-already-fragile-health-systems-over-6000-additional-children
- Pregnant Mothers and Babies Born during COVID-19 Pandemic Threatened by Strained Health Systems and Disruptions in Services. [Accessed 2023 Apr 15]. Available from: https://www.unicef.org/bangladesh/en/press-releases/pregnant-mothers-and-babies-born-during-covid-19-pandemic-threatened-strained-health.
- Diabetes knowledge and utilization of healthcare services among patients with type 2 diabetes mellitus in Dhaka, Bangladesh. BMC Health Serv Res. 2017;17(1):586.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- ‘We delivered at home out of fear’: Maternity care in rural Nigeria during the COVID-19 pandemic. Int J MCH AIDS. 2023;12(1):e632.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Access to maternal health services during COVID-19. Europasian J Med Sci. 2020;2:46-50.
- [CrossRef] [Google Scholar]
- Accessing antenatal care (ANC) services during the COVID-19 first wave: Insights into decision-making in rural India. Rep Health. 2022;19(1):158.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Indirect effects of COVID-19 pandemic on reproductive, maternal, newborn and child health services in Pakistan. East Mediterr Health J. 2022;28(4):258-65.
- [CrossRef] [PubMed] [Google Scholar]
- Disruptions in maternal health service use during the COVID-19 pandemic in 2020: experiences from 37 health facilities in low-income and middle-income countries. BMJ Glob Health. 2022;7(1):e007247.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Challenges in access and satisfaction with reproductive, maternal, newborn and child health services in Nigeria during the COVID-19 pandemic: A cross-sectional survey. PLoS One. 2021;16(5):e0251382.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Effect of COVID-19 pandemic on provision of sexual and reproductive health services in primary health facilities in Nigeria: A cross-sectional study. Reprod Health. 2021;18(1):166.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Barriers and facilitators of access to maternal, newborn and child health services during the first wave of COVID-19 pandemic in Nigeria: Findings from a qualitative study. BMC Health Serv Res. 2022;22(1):611.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Knowledge, attitude, practice, and fear of covid-19: An online-based cross-cultural study. Int J Ment Health Addiction. 2023;21:1025-40.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Doctors at private hospitals left vulnerable. The Daily Star. [Last Update 2020 Apr 29; cited 2023 Apr 15]. Available from: https://www.thedailystar.net/editorial/news/doctors-private-hospitals-left-vulnerable-1897657
- The changing aspects of motherhood in face of the COVID-19 pandemic in low- and middle-income countries. Matern Child Health J. 2021;25(1):15-21.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Antenatal care services utilization during COVID-19 second wave attack in pasuruan, indonesia. J Med Life. 2022;15(1):7-14.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Adapting antenatal care in a rural LMIC during COVID‐19: A low literacy checklist to mitigate risk for community health workers. Int J Gynaecol Obstet. 2020;151(2):289-291.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Household socioeconomic status and antenatal care utilization among women in the reproductive-age. Front Public Health. 2021;9:724337.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]





