Translate this page into:
Assessing the Impact of an Intervention on Caregivers’ Awareness and Completion of Continuum of Care Among Pregnant Women

* Corresponding author: May Soe Aung, Department of Preventive and Social Medicine, University of Medicine (1) Yangon, 245, Myoma Kyaung Road, Lanmadaw Township, Yangon-11131, Myanmar. Tel: +959 5058827. maysoeag2010@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Aung MS, Soe MM, Win HH, Mya KS. Assessing the impact of an intervention on caregivers’ awareness and completion of continuum of care among pregnant women. Int J MCH AIDS. 2024;13:e024. doi: 10.25259/IJMA_22_2024
Abstract
Background and Objective
The continuum of care (CoC) is an important approach that should be prioritized for improving maternal health. The World Health Organization recommends working with individuals, families, and communities to ensure continuous care throughout pregnancy, childbirth, and the postpartum period. The purpose of this study was to assess the impact of an intervention on the awareness of the CoC among main caregivers and the completion of CoC among pregnant women.
Methods
During the COVID-19 pandemic, a community-based quasi-experimental study was conducted in two townships of the Yangon Region, including 200 pairs of pregnant women and their caregivers. The intervention focused on providing health education sessions and distributing pamphlets to caregivers in the intervention group. The study aimed to assess the awareness of main caregivers about CoC and completion of CoC among pregnant women. A key predictor variable for evaluating the outcome was receiving an intervention package by the main caregivers in the intervention. The analysis used logistic regression, including the propensity score model, and was conducted using STATA vs 15.1.
Results
The final analysis included 193 pairs. Most main caregivers were husbands: 47 were husbands in the intervention and 59 in the control group, while 24 mothers were included in both groups. The awareness of CoC for maternal health among main caregivers from the intervention group was 9.97 times higher than those from the control group (AOR = 9.97, 95% CI: 5.12 to 19.43, p < 0.001). The completion of CoC among women from the intervention group was 2.17 times higher than those from the controls (AOR = 2.17, 95% CI 1.08 to 4.37, p < 0.05). The awareness of main caregivers was found to be a significant predictor for completion of CoC.
Conclusion and Global Health Implications
Health education intervention for main caregivers could improve CoC completion among pregnant women. It provided baseline information for further interventions at the family level for improving CoC among pregnant women in the future.
Keywords
Caregivers
Continuum of Care
Health Education
Pregnant Women
INTRODUCTION
Background of the Study
Maternal health from pregnancy to the postnatal period is inseparable and the continuum of care (CoC) connects essential maternal health packages for building natural interactions.[1] In low- and middle-income countries (LMICs), the continuous uptake of antenatal care (ANC), skilled birth attendance, and postnatal care (PNC) is essential for better maternal health outcomes.[2] According to the World Health Organization (WHO), an operational CoC with accessible and quality care is essential before and during pregnancy, childbirth, and the postnatal period.[3] The WHO recommended the first ANC during the first 12 weeks’ gestation, followed by contacts at 20, 26, 30, 34, 36, 38, and 40 weeks’ gestation.[4] To improve the health of women and reduce maternal mortality, great attention by skilled attendants is required to recognize danger signs early and a timely referral to a well-equipped facility.[5] It is also important to receive PNC within the first 24 hours followed by check-ups on the second or third day and the seventh day to identify, monitor, and manage health problems during the postnatal period.[6]
In Myanmar, the maternal mortality ratio (MMR) was 250 per 100,000 in 2017 which was higher than in South East Asia region, and nearby countries.[7,8] Women who had at least four antenatal clinic visits accounted for only 59% by 2016.[9] The deliveries by skilled birth attendance were 60% and institutional delivery was 37% from 2015 to 2016.[10] Most women, especially from rural areas practiced inadequate PNC.[11] Maternal death was related to poor access, understanding, and using health information by women and their families.[12] There was evidence that the mother-in-law’s influence, guidance from relatives, and male engagement, are associated with the use of ANC and PNC.[11,13] A framework for developing interventions by the WHO emphasizes the role of men and other influential family members in promoting awareness at the individual, family, and community levels.[14] Based on the gaps between services and needs found by interventional research, further strategies and activities can be prioritized. To reach the MMR target by 2030, the WHO recommended CoC as an effective approach for Myanmar pregnant women.[15] Therefore, it is necessary to consider an appropriate way at the family level to increase the CoC for maternal health. According to Myanmar culture, the influence of family members is an important contributing factor to the continuous utilization of health care among pregnant women. Therefore, the intervention for raising family caregivers’ awareness of maternal health care is essential to enhance the completion of CoC among pregnant women.
Objectives of the Study
This quasi-experimental study aimed to assess the impact of an intervention on the awareness of CoC among main caregivers and the completion of CoC among pregnant women.
Hypothesis
The intervention package for main caregivers improves CoC among pregnant women in rural areas of the Yangon Region.
METHODS
Study Period and Area
The study was conducted from February 2020 to June 2021 during the COVID-19 pandemic. Taik Kyi from the north district and Kyauktan from the south district of Yangon Region were selected as intervention and control townships, respectively. There were adequate rural settings and people with different ethnic and religious groups were residing in both townships. Taik Kyi Township has one township hospital, four station hospitals, and four rural health centers whereas Kyauktan Township has one township hospital, five station hospitals, and nine rural health centers.[16,17] According to the Yangon Regional Health Department, they were the third-highest MMR townships in their relevant districts in 2018. Moreover, in both townships, there were more than 3000 pregnant women, MMR was about 1 per 1000 live births and the rate of ANC for four or more times was less than 85%.
Study Population
Pregnant women aged 18 years and above with pregnancy of not later than 20 weeks’ gestation and their main caregiver of any sex with the age between 18 years and 65 years were included in the study. Family members who could make pregnancy-related important decisions and live together with pregnant women under the same shelter throughout pregnancy up to six weeks after delivery are eligible as main caregivers.
Sample Size Determination
The proportion of completed antenatal visits (0.59) reported in a nationally representative survey was used for the control group, and that for the intervention group was assumed as 0.9 in the sample size calculation.[10] Two population proportion formula was used with 95% CI, the power of 80%, and a design effect of 2 for cluster sampling.[18] The total required sample was 200 pairs of pregnant women and their main caregivers who were equally divided for each group.
Sampling Procedure
First, townships, village tracts, and rural health centers/sub-centers were purposely chosen according to geographical backgrounds and antenatal care coverage by keeping consideration of preventing contamination effect. Then, eight villages from the intervention township and nine villages from the control township were included in the study. Finally, eligible pregnant women and their main caregivers from each village were selected consecutively to reach the calculated sample size.
Intervention Package
The intervention package included a 30-minute health talk by trained midwives and the delivery of a pamphlet for main caregivers. The pamphlet was designed based on the findings that came out from the focus group discussion with local midwives, main caregivers, and pregnant women from the intervention areas. The pamphlet was prepared in the Myanmar language, including both text messages and pictorials. The prioritized messages included in the pamphlet were: (1) timing and frequency of antenatal and postnatal care, (2) institutional delivery, (3) skilled attendants, (4) danger signs, (5) information about two doses of tetanus toxoid, (6) the importance of blood pressure measurement and blood testing, (7) proper nutrition, (8) ways of healthy living, and (9) drugs necessary from pregnancy to the postpartum period. The pictorials used in the pamphlet were cited from the Myanmar Maternal and Child Health (MCH) handbook and self-developed under the guidance of the Maternal and Reproductive Health Division. Eight pictures, given in the pamphlet, showed examination by a skilled healthcare provider; receiving tetanus toxoid; taking blood pressure measurements; taking drugs during pregnancy; giving support by the caregiver for taking drugs; healthy foods; salty diets; and danger signs. The pamphlet included a log table to help main caregivers track the timing of ANC and PNC visits for pregnant women. The updated pamphlet was distributed to the caregivers responsible for the pregnant women and who attended the health education session [Supplementary file].
All messages in the pamphlet were explained in the health talk session after routine antenatal care procedures of pregnant women. Health education for main caregivers was provided individually due to the different days and timing of antenatal visits for pregnant women. The education included explaining the importance of main caregivers supporting regular ANC, safe delivery, and PNC of pregnant women. They were also encouraged to share suggestions and information received from health talks and pamphlets with pregnant women. For pregnant women requiring extreme attention, main caregivers were requested to record the timing of ANC and PNC in the log table. After the health talk session, the pamphlet was given to the main caregivers to take home. At the end of the session, the main caregivers were urged to use the pamphlet throughout the antenatal period up to the postnatal period to provide advice and care to pregnant women. In the control group, the timing and procedures of participants’ recruitment, and baseline data collection were similar to that of the intervention group. Apart from not providing a health education package for the main caregivers, all eligible pregnant women received routine ANC and follow-up care from locally assigned midwives. Awareness of the CoC among main caregivers and completion of CoC among pregnant women in both intervention and control groups were assessed after a 2-week postpartum period of participating women as the outcomes of the study.
Statistical Analysis
STATA version 15.1 (StataCorp. 2017. Stata Statistical Software: Release 15.1. College Station, TX: StataCorp LLC.) was used for data analysis. Awareness of CoC was categorized into two groups (<6 points and ≥6 points) including timing and frequency of ANC and PNC; skilled birth attendance; institutional delivery; and danger signs. The completion of CoC was defined as fulfillment in eight antenatal visits; birth by a skilled attendant; and PNC within 24 hours after birth followed by two additional checks. The chi-square test was used to identify differences in outcome between intervention and comparison groups with p-value <0.05 as statistical significance. Multivariable binary logistic regression analysis by different models was applied to find the effect of intervention. Being a quasi-experimental design, a propensity score was generated to create valid and counterfactual comparison groups.[19] After the collinearity check, the main caregiver’s age, sex, education, marital status, source of health information, pregnant women’s age, education, gravida, and number of family members were included in the propensity score model. The regression model with the smallest Akaike Information Criterion (AIC) value was used as the final fitted model. The effects of the intervention were presented using an adjusted odds ratio (AOR) with a 95% confidence interval (CI).
Ethical Approval
This study was approved for ethical consideration by the Institutional Review Board (IRB) of the University of Public Health, Yangon, Myanmar. Before the interview, the researcher discussed the study objectives. Participation was voluntary and assured to maintain confidentiality. A unique identification code was used to guarantee anonymity. Similar informed consent form was used for both the intervention and control groups. All participants have given informed consent to participate in the study.
RESULTS
Sociodemographic Characteristics
Approximately 50% of the main caregivers were husbands, the majority were dependents, and more than 20% of both groups worked in agriculture and animal husbandry. Regarding marital status, 82.3% in the intervention group and 90.7% in the control group were married. In both groups, the highest proportion of pregnant women were aged less than 35 years, very few were illiterates, and half of them were working women. Although multiparous women were found more in both groups, the majority had less than three children. The main source of health information for both caregivers and pregnant women was mass media and healthcare providers [Table 1].
| Characteristics | Caregivers | Pregnant women | ||||||
|---|---|---|---|---|---|---|---|---|
|
Intervention (N = 96) |
Control (N = 97) |
Intervention (N = 96) |
Control (N = 97) |
|||||
| n | % | n | % | n | % | n | % | |
| Relationship with the pregnant woman | ||||||||
| Husband | 47 | 48.9 | 59 | 60.8 | ||||
| Mother | 24 | 25.0 | 24 | 24.8 | ||||
| Mother-in-law | 9 | 9.4 | 7 | 7.2 | ||||
| Sister | 6 | 6.3 | 2 | 2.1 | ||||
| Sister-in-law | 5 | 5.2 | 3 | 3.1 | ||||
| Daughter | 1 | 1.0 | 1 | 1.0 | ||||
| Friend | 2 | 2.1 | 0 | - | ||||
| Father/Brother/Other relatives | 2 | 2.1 | 1 | 0.1 | ||||
| Sex | ||||||||
| Male | 48 | 50.0 | 59 | 60.8 | ||||
| Female | 48 | 50.0 | 38 | 39.2 | ||||
| Age (years) | ||||||||
| 20 and less | 4 | 4.2 | 4 | 4.1 | ||||
| 21 to 40 | 45 | 46.9 | 60 | 61.9 | ||||
| 41 to 50 | 25 | 26.0 | 15 | 15.5 | ||||
| 51 to 60 | 18 | 18.8 | 14 | 14.4 | ||||
| >60 | 4 | 4.2 | 4 | 4.1 | ||||
| Mean ± SD | 40.2 ± 12.0 | 38.0 ± 12.1 | ||||||
| Age (years) | ||||||||
| 25 and less | 32 | 33.3 | 29 | 29.9 | ||||
| 26 to 35 | 51 | 53.2 | 47 | 48.5 | ||||
| 36 to 45 | 13 | 13.5 | 21 | 21.7 | ||||
| Mean ± SD | 28.5 ± 6.0 | 29.0 ± 6.1 | ||||||
| Level of education | ||||||||
| Illiterate | 3 | 3.1 | 2 | 2.1 | ||||
| Read and write | 5 | 5.2 | 7 | 7.2 | 1 | 1.0 | 3 | 3.1 |
| Grade1 to 4 | 40 | 41.7 | 50 | 51.6 | 35 | 36.5 | 40 | 41.2 |
| Grade 5 to 8 | 28 | 29.2 | 25 | 25.8 | 26 | 27.1 | 32 | 32.9 |
| Grade 9 to 10 | 17 | 17.7 | 7 | 7.2 | 22 | 22.9 | 12 | 12.4 |
| University and above | 6 | 6.3 | 8 | 8.3 | 9 | 9.4 | 8 | 8.3 |
| Occupation | ||||||||
| Dependent/Not working¶ | 23 | 23.9 | 27 | 28.1 | 43 | 44.8 | 46 | 47.4 |
| Employee/Working¶ | 7 | 7.3 | 10 | 10.5 | 53 | 55.2 | 51 | 52.6 |
| Laborer | 17 | 17.7 | 20 | 20.8 | ||||
| Self-employed | 14 | 14.6 | 4 | 4.2 | ||||
| Seller | 7 | 7.3 | 10 | 10.4 | ||||
| Farmer/Agriculturing/Animal husbandry | 22 | 22.9 | 20 | 20.8 | ||||
| Others | 6 | 6.3 | 5 | 5.2 | ||||
| Marital status | ||||||||
| Never married | 5 | 5.2 | 3 | 3.1 | 1 | 1.0 | 0 | - |
| Married | 79 | 82.3 | 88 | 90.7 | 94 | 98.0 | 97 | 100 |
| Divorced/Separated/Widowed | 12 | 12.5 | 6 | 6.2 | 1 | 1.0 | 0 | - |
| Gravida | ||||||||
| Primary | 45 | 46.9 | 38 | 39.2 | ||||
| Multipara | 51 | 53.1 | 59 | 60.8 | ||||
| Number of living children | ||||||||
| None | 48 | 50.0 | 40 | 41.2 | ||||
| ≤3 | 46 | 47.9 | 52 | 53.6 | ||||
| >3 | 2 | 2.1 | 5 | 5.2 | ||||
| Family member | ||||||||
| <5 | 63 | 65.6 | 72 | 74.2 | ||||
| ≥5 | 33 | 34.4 | 25 | 25.8 | ||||
| Monthly household family income (Myanmar Kyats, MMK) | ||||||||
| 1st Quartile (≤150,000) | 31 | 32.3 | 23 | 23.7 | ||||
| 2nd Quartile (1,500,001 to 200,000) | 25 | 26.0 | 21 | 21.7 | ||||
| 3rd Quartile (200,001 to 300,000) | 27 | 28.1 | 25 | 25.8 | ||||
| 4th Quartile (>300,000) | 13 | 13.5 | 28 | 28.9 | ||||
| Source of health information* | ||||||||
| Mass media | 85 | 88.5 | 89 | 91.8 | 91 | 94.8 | 95 | 97.9 |
| Healthcare providers | 79 | 82.3 | 85 | 87.6 | 90 | 93.8 | 89 | 91.8 |
| Others | 3 | 3.1 | 9 | 9.3 | 5 | 5.4 | 19 | 19.6 |
Awareness of Main Caregivers on the Continuum of Maternal Healthcare after Intervention
The intervention group showed significantly higher awareness of the importance of first antenatal (AN) visit than the control group: 62.5% versus 13.4%. About eight or more times as many participants in the intervention group (76.0%) were significantly more aware than in the control group (32.0%) of ANC. All main caregivers from both groups were aware of the role of a skilled attendant during childbirth. More than twice of the participants from the intervention group (95.8%) were aware of the timing to take postnatal care within 24 hours after birth compared to the control group (43.3%) (p < 0.001). Two-thirds of the intervention group were aware of the mandatory three or more additional checks after the first PNC while only about half of the controls were aware of it (p < 0.001). Nearly 20% of participants in the control group were not aware of any pregnancy danger signs, which was significantly higher than the intervention group.
Continuum of Care among Pregnant Women from the Antenatal to the Postnatal Period
According to Figure 1, the completion of the CoC for maternal health was significantly higher in the intervention group than in the controls (p < 0.001).
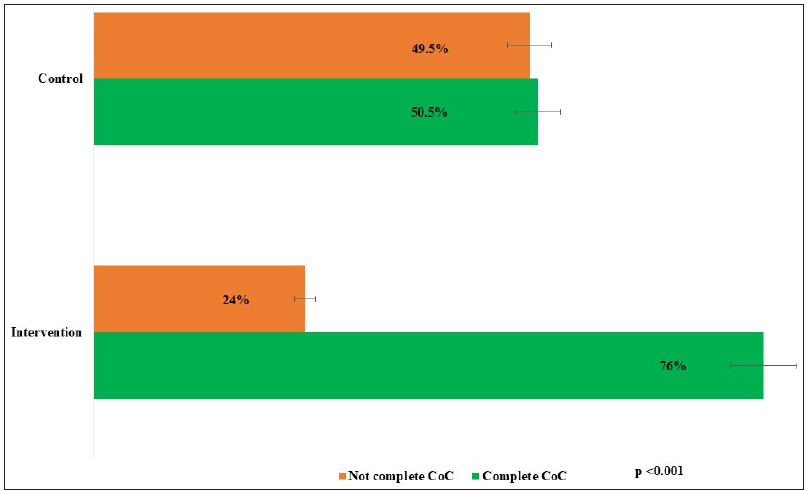
- Completion of continuum of care (CoC) among pregnant women. P-value: Points out the significant higher proportion of the CoC in the intervention group than the control group.
Comparison of Study Outcomes between Intervention and Control Groups
It is indicated in the Table 2 that the main caregivers in the intervention group were more aware of the CoC for maternal health compared to those in the control group. The akaike information criterion (AIC) value 1 was lower than that of Model 2 and nested in Model 2. According to this, Model 1 was chosen as a more fitted model and it revealed that awareness of CoC for maternal health among main caregivers from the intervention group was 9.97 times higher than those from the control group.
| Predictor variables | Awareness of CoC for maternal health¶ | |
|---|---|---|
| Model 1 | Model 2* | |
| ORCrude [95% CI] | AOR [95% CI] | |
| Control group | 1 | 1 |
| Intervention group | 9.97 [5.12,19.43]a | 9.28 [4.59,18.78]a |
| Model summary | ||
| Constant | 0.2a | 0.18a |
| Likelihood ratio Chi-square | 53.82a | 56.75a |
| Pseudo R 2 | 0.20 | 0.21 |
| AIC value | 215.86 | 220.93 |
| LR Chi-square for testing: Model 1 nested in Model 2 2.29, p = 0.57. | ||
In Table 3, all three logistic regression models revealed that pregnant women in the intervention group were more likely to complete a CoC for maternal health than pregnant women from the control group. Model 2 had the lowest AIC value, nested in Model 3 (p = 0.19), and therefore, Model 2 was chosen as the best-fitted model. The completion of CoC among women from the intervention group was 2.17 times higher than those from the controls and it was also found that the awareness of main caregivers was also a significant predictor of the outcome. The results showed that there was a better impact of the intervention on the completion of CoC among pregnant women.
| Predictor variables | Completion of CoC for maternal health | ||
|---|---|---|---|
| Model 1 | Model 2† | Model 3* | |
| ORCrude [95% CI] | AOR [95% CI] | AOR [95% CI] | |
| Control | 1 | 1 | 1 |
| Intervention | 3.11 [1.68,5.75]a | 2.17 [1.08,4.37]b | 2.20 [1.05,4.64]b |
| Awareness on CoC | |||
| Less than facts | 1 | 1 | |
| Six and above | 2.13 [1.04,4.35]b | 2.10 [1.01,4.38]b | |
| Model summary | |||
| Constant | 1.02 | 0.88 | 0.80 |
| Likelihood ratio Chi-square | 13.74a | 18.04a | 24.09a |
| Pseudo R 2 | 0.05 | 0.07 | 0.09 |
| AIC value | 244.18 | 241.88 | 243.83 |
| LR Chi-square for testing: Model 2 nested in Model 3 | 6.05, p = 0.19 | ||
DISCUSSION
Effect of Intervention
Health education is an important tool to improve health-oriented attitudes in a given society.[20] The intervention through health talks reinforced with wall-mounted posters and handbills in Nigeria reported improved knowledge about danger signs and utilization of health facility delivery services among pregnant women.[21] A study on CoC in Ghana reported that exposure to media influenced CoC for maternal health.[22] In the current interventional study, a pamphlet containing pictures and texts for the main caregivers could be more effective in helping them remember the health-related messages. This would allow caregivers to learn at any time, during the COVID-19 pandemic, and advise pregnant women about the right maternal health services.
After the intervention, more main caregivers from the intervention group were aware of ANC than the control group. This finding pointed out that although the main caregivers were not the primary users of MCH services, they were interested in receiving adequate antenatal care for their pregnant women. Therefore, health education for caregivers of pregnant women was an alternative way to improve the awareness of maternal health care within the community in addition to routine services for pregnant women. This is similar to the study among postnatal mothers after the Structured Teaching Program in India, where there was an improvement in postnatal care knowledge.[23] In the current study, the main caregivers from the intervention group were more aware of postnatal care than the control. These findings proved that although the target audience was not similar, community awareness could be improved by interventions including a health educational approach. Moreover, there was a significantly higher awareness of danger signs in the intervention group than in the control group. This was consistent with community-based intervention including health education in rural Tanzania; and the intervention by provision of birth and emergency preparedness card plans and counseling by healthcare providers in rural Bangladesh.[24,25] These highlighted the role of health education interventions to improve caregivers’ awareness of important pregnancy-related danger signs for preventing complications in pregnant women. The difference in the overall awareness level of the CoC between the two groups highlighted the effectiveness of health education intervention for raising awareness of main caregivers for participation from the antenatal to postnatal period of pregnant women. This was similar to the findings of the family-oriented antenatal group educational program in rural Tanzania.[26]
The current study showed higher CoC among women from both intervention areas (76%) and control areas (50.5%) compared to the study with secondary analysis of the nationwide survey during 2015–2016 where the prevalence of CoC among 15–49 years Myanmar mothers was 42.5% with CoC definition as the presence of four times and above antenatal care, delivery with skilled birth attendance, and postnatal care within first 48 hours.[27] To ensure quality care and desired outcomes for maternal health improvement, it was suggested that more health education activities and a wide range of strategies were needed.[28] The effect of an intervention that included counseling of families by frontline health workers and the use of a printed deck of cards for improving Reproductive, Maternal, Newborn, and Child Health (RMNCH) CoC coverage was found in an Indian study.[29] Comparably, CoC completion in the current study was found among two-thirds of women from the intervention group but only half of the participants completed CoC in the control group. These findings pointed out the effect of the health education intervention on the completion of CoC among pregnant women.
Strengths and Limitations of the Study
This is the first intervention study at the family level for the CoC among pregnant women in Myanmar. This intervention was needed for primary caregivers of pregnant women who played an essential role in supporting and decision-making for the continuum of maternal health care. This intervention applied the role of midwives who were the most dependable medical professionals in rural areas of Myanmar. In the data management stage of the study, the propensity score was used to adjust the confounding effect of background characteristics. Because of an interventional study conducted in the Yangon region only, a limitation in generalizability was an area for improvement. The preformed knowledge of maternal health care among pregnant women and the alertness of midwives to alarm the main caregivers before assessment of the outcomes were the possible contamination factors for the effectiveness of the intervention. The changes in healthcare accessibility or caregiver availability can contribute to potential biases introduced by the COVID-19 pandemic.
CONCLUSION AND GLOBAL HEALTH IMPLICATIONS
There were different methods in raising awareness of main caregivers and CoC among pregnant women. Therefore, the intervention composed of face-to-face health education sessions and delivery of educational pamphlets with key messages and pictorials was an effective strategy. This was also useful in maintaining maternal healthcare services utilization during the COVID-19 pandemic. It provided baseline information for further interventions at the family level to improve CoC among pregnant women in the future.
Key Messages
-
1.
Health talks with visual aids are effective in improving the awareness of caregivers on the continuum of care (CoC) for maternal health.
-
2.
Local basic health staff are key persons in implementing health promotion interventions to improve awareness and good practices of maternal health care.
-
3.
Health education intervention for family caregivers can affect the completion of CoC among pregnant women during the COVID-19 pandemic.
Acknowledgments
We are deeply indebted to midwives, pregnant women, and caregivers who actively participated in this study.
COMPLIANCE WITH ETHICAL STANDARDS
Conflicts of Interest
The authors declare no competing interests.
Financial Disclosure
Nothing to declare.
Funding/Support
This study is funded by MOH IR Grant, Myanmar.
Ethics Approval
The research/study approved by the Institutional Review Board at the University of Public Health, Yangon, Myanmar, number UPH-IRB (2020/PhD/1), dated 24 January 2020.
Declaration of Patient Consent
The authors certify that they have obtained all appropriate patient consent.
Use of Artificial Intelligence (AI)-Assisted Technology for Manuscript Preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
None.
REFERENCES
- The maternal, newborn, and child health continuum of care. Opportunities for Africa’s newborns. Practical data, policy and programmatic support for newborn care in Africa. Partnership for maternal, newborn and child health. Geneva: World Health Organization; 2006. p. :23-36.
- Effective linkages of continuum of care for improving neonatal, perinatal, and maternal mortality: A systematic review and meta-analysis. PLoS One.. 2015;10(9):e0139288.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Antenatal care. Opportunities for Africa’s newborns: Practical data, policy and programmatic support for newborn care in Africa. Partnership for maternal, newborn and child health. Geneva: World Health Organization; 2006. p. :55-62.
- Leveraging Antenatal Care to Increase Uptake of Postpartum Family Planning. A Key Time for Counseling. Maternal and Child Health Program, United States Agency for International Development. [accessed 2019 Aug 10]. Available from: http://www.mcsprogram.org/.
- Skilled attendants for pregnancy, childbirth and postnatal care. Br Med Bull.. 2003;67:39-57.
- [CrossRef] [PubMed] [Google Scholar]
- A study on postnatal care and its correlates among recently delivered women visiting to BRD medical college Gorakhpur. Int J Community Med Public Health.. 2017;4:1548-51.
- [CrossRef] [Google Scholar]
- United Nations Children’s Fund: Monitoring the situation of children and women, Maternal mortality. [Accessed 2019 Nov 10] Available from: https://data.unicef.org/topic/maternal-health/maternal-mortality/.
- Trends in maternal mortality 2000 to 2017: Estimates by WHO, UNICEF, UNFPA, World Bank Group and the United Nations Population Division: Executive summary. World Health Organization; 2019.
- National Guidelines for Antenatal Care for Service Providers. Nay Pyi Taw, Myanmar: Maternal and Reproductive Health Division; 2018.
- Myanmar Demographic and Health Survey 2015-16. 2017.
- Utilization of full postnatal care services among rural Myanmar women and its determinants: A cross-sectional study. F1000Res.. 2018;7:1167.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Review/Assessment of Implementation of Child Death Surveillance and Response (CDSR) in Myanmar. The Republic of the Union of Myanmar Ministry of Health and Sports, Department of Public Health, Child Health Division; 2018.
- Determinants of non-adherence to antenatal care among pregnant women. IOSR-JNHS.. 2018;17:15-24.
- [Google Scholar]
- Working with individuals, families and communities to improve maternal and newborn health: A toolkit for implementation. World Health Organization; 2017.
- Remarkable progress, new horizons and renewed commitment, ending preventable maternal, newborn and child deaths in South-East Asia region. [Last accessed on 2019 Oct 8]. Available from: https://apps.searo.who.int/RMNCAH-2019/Myanmar
- MIMU Township Profile. Kyauktan_2019_MMR. [Last accessed on 2019 Oct 15]. Available from: https://themimu.info/township-profiles
- MIMU Township Profile. Taikkyi_2019_MMR. [Last accessed on 2019 Oct 15]. Available from: https://themimu.info/township-profiles
- Fundamentals of biostatistics. Belmont, CA: Thomson-Brooks/Cole; 2006.
- Evaluating clinical and public health interventions: A practical guide to study design and statistics. Cambridge, England: Cambridge University Press; 2010.
- Health education as an important tool in the healthcare system. Polish J Public Health.. 2014;124:145-7.
- [Google Scholar]
- Effect of health education intervention on knowledge and utilization of health facility delivery services by pregnant women in Sokoto State, Nigeria. Int J Contemp Med Res.. 2018;5:F4-F9.
- [CrossRef] [Google Scholar]
- Utilization, predictors and gaps in the continuum of care for maternal and newborn health in Ghana. Int J MCH AIDS.. 2021;10(1):98-108.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Effectiveness of structured teaching programme on knowledge about postnatal care among mothers. Int J Res Med Sci.. 2017;5:4993-7.
- [CrossRef] [Google Scholar]
- Community health workers can improve male involvement in maternal health: Evidence from rural Tanzania. Global Health Action.. 2016;9:30064.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Capacities of women and men to improve maternal and newborn health: Effect of a community-based intervention package in rural Bangladesh. J Global Health.. 2019;9(1):010413.
- [CrossRef] [Google Scholar]
- Evaluation of a family-oriented antenatal group educational program in rural Tanzania: A pre-test/post-test study. Reprod Health.. 2018;15(1):117.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Continuum of care of mothers and immunization status of their children: A secondary analysis of 2015–2016 Myanmar demographic and health survey. Public Health Pract.. 2022;4:100335.
- [Google Scholar]
- Health education strategies targeting maternal and child health: A scoping review of educational methodologies. Medicine.. 2019;98(26):e16174.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Making the continuum of care work for mothers and infants: Does gender equity matter? Findings from a quasi-experimental study in Bihar, India. PLoS One.. 2017;12(2):e0171002.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]






