Translate this page into:
Cervical Precancer Treatment Outcomes in Cameroon

Corresponding author: Joseph F. Nkfusai, Faculty of Health Sciences, University of Buea, P. O. Box 63 Buea, Cameroon. Tel: +237-677-698-459 Email: fonyuyj@yahoo.com
-
Received: ,
Accepted: ,
How to cite this article: Nkfusai JF, Manga SM, Nulah K, Ngalla C, Manjuh F, Nkfusai N, et al. Cervical Precancer Treatment Outcomes in Cameroon. Int J MCH AIDS. 2024;13:e020. doi: 10.25259/IJMA_8_2024
Abstract
Background and Objective
The ablative and excision treatment procedures are effective, accessible, and affordable in resource-constrained settings, but the rollout and posttreatment follow-up are not remarkable. The outcomes of treatment procedures among women treated for precancerous lesions of the cervix have not been adequately studied in Cameroon. This study assessed the outcome of ablative and excisional treatment procedures.
Methods
This was a cross-sectional study that assessed the clinical outcome of 170 women treated for cervical precancers using ablative and excisional procedures in 2019 and 2020. Demographic and clinical data (treatment and posttreatment follow-up) were abstracted from the program registry. The data was analyzed to assess the clinical outcomes of cervical precancer treatment. The association between each independent variable and the dependent variable was examined in a simple logistic regression. All variables with p < 0.2 in the bivariate logistic regression model were subjected to a multivariable logistic model to get rid of cofounders and obtained adjustable odds ratios. The data was summarized using odds ratios, with p-value < 0.05 considered significant. All statistical analyses were performed using STATA version 17.
Results
The cervical precancer treatment effectiveness of 93.55% was disaggregated into 94.37% and 88.23% for ablative and excisional procedures, respectively, with less severe adverse clinical effects. Despite the high awareness of women on the importance and timing of posttreatment follow-up, its uptake was 54.71%. Most of the women who got pregnant after the procedures delivered live and healthy babies. Women who were HIV positive were 89% (0.89 times) [aOR = 0.11, 95%CI (0.01 0.85), p = 0.034] less likely to have effective treatment for cervical precancer when compared to HIV-negative women. Those with low-grade lesions were eight times [aOR = 8.39, 95%CI (1.10 64.06), p = 0.04] more likely to have effective treatment for cervical precancer treatment compared to those with high-grade lesions.
Conclusion and Global Health Implications
Ablative and excisional treatment procedures for cervical precancer were effective with limited adverse effects in Cameroon. Women living with HIV and those with large lesions experienced lower treatment effectiveness. Most of the women who got pregnant after the procedures delivered live and healthy babies. Posttreatment follow-up which is highly recommended because of recurrent/persistent lesions was barely above average.
Keywords
Cervical Precancer
Clinical Outcome
Ablative and Excisional Procedures
Cameroon.
INTRODUCTION
Cervical cancer begins as a precancer lesion which can be detected during screening and effectively treated. Smaller precancers are treated by ablation using cryotherapy/thermal ablation (TA) while larger/more serious precancer lesions are treated by excision using large loop excision of the transformation zone (LLETZ).[1–4] Excisional procedures comprise surgical removal of precancerous cells or affected tissue from the cervix and include LLETZ and laser conization.[5] Ablative treatment procedures utilize extreme temperatures to destroy precancerous cells and include cryotherapy, CO2 laser ablation, and TA (e.g., diathermy, cold coagulation).[6–8] The World Health Organization (WHO) has recommended ablative and excision procedures for its “screen-and-treat” and “see, triage and treat” approaches to secondary CC prevention in low-and-middle income countries (LMICs). In the “screen-and-treat” approach for CC, the decision to treat is based on a positive primary screening test only, while the “see, triage, and treat” approach uses HPV DNA testing as a primary test, and those who test positive for high-risk HPV types are triaged with visual inspection with acetic acid (VIA).[4,9,10]
The ablative and excision treatment procedures are effective, available, convenient, and relatively affordable in resource-constrained settings but the rollout and posttreatment follow-up are not remarkable.[11–13] There is regional variation in the uptake of CC interventions for reasons which are societal, economic, and based on life style.[11,14] Barriers to low uptake of CC interventions in Cameroon include culture, religion, the psychological impact of embarrassment, the influence of husbands, cost, discomfort, and vulnerability.[15] The effects of ablative and excisional treatment among women treated for precancerous lesions of the cervix have not been adequately studied in Cameroon. This study is thus concerned with the clinical outcomes of ablative and excisional procedures for treating cervical precancers by the Cameroon Baptist Convention Health Services in Cameroon Women’s Health Program (CBCHS-WHP).
The CBCHS-WHP is a large faith-based comprehensive cervical cancer prevention program operating in Cameroon. From 2007 to 2022, CBCHS-WHP screened over 120,000 women for cervical cancer from across the national territory and treated over 5,000 of the women who tested positive for cervical precancer. Although beginning 2020, they commenced the use of Human Papillomavirus (HPV) testing as primary screening for women aged 30 years and older, the program has relied principally on visual inspection with acetic acid and Lugol’s iodine (VIA/VILI) enhanced by digital cervicography (DC). As recommended by WHO, cervical precancers are treated using cryotherapy or TA for smaller lesions and LLETZ for larger lesions.[16] The program has a coordination office and runs a database for enrolled women.
The clinical outcomes of ablative and excision cervical precancer treatment for selected women treated in 2019 and 2020 will provide evidence to support cervical intervention improvement as the program is incrementally being scaled up and replicated in LMICs.
METHODS
This was a cross-sectional study in which data on a sample population of 170 women treated for cervical precancers using ablative and excisional procedures in 2019 and 2020 were abstracted from the registry and used to assess clinical outcomes. The choice of 2019 and 2020 was to enable to have a reasonable sample size and to prevent recall bias. Demographic/clinical data collected on enrollment and treatment/posttreatment follow-up data from 2019 to 2023 and supplementary data collected using a structured questionnaire were considered in the study [Figure 1]. The records of the study participants were reviewed systematically from January 2019 to January 2023 to assess clinical outcomes. Cervical cancer posttreatment follow-up records had test results, treatment procedure, and posttreatment follow-up results.
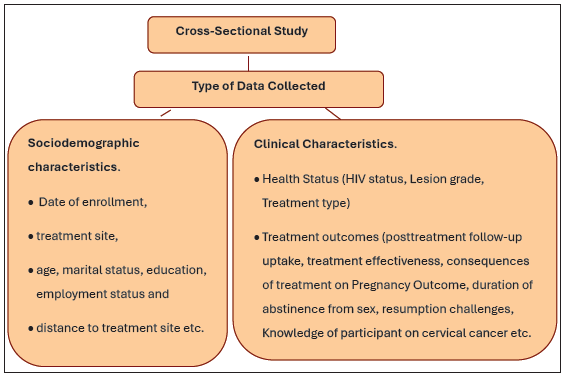
- Study Design.
Clinical outcomes comprised the effectiveness and medical effects of the treatment, including pain, and effects of treatment on reproductive health.
Sample Calculation and Sampling Techniques
The sample size of 170 was determined using the Lorenz formula for an infinite population with a known proportion of 9%. The 9% was the prevalence of precancer established from the screening of over 12,000 women for cervical cancer in Cameroon.[ 16] The women who were eligible for this study included those who received cervical precancer treatment in 2019/2020 and consented to participate in the study while those who were ill or not in a good mental state to provide answers to the questions were excluded from the study.
The sampling method was multistage. The choice of 2019 and 2020 for the study was convenient while systematic random sampling was used to select the sample of 170 participants from the 340 women treated in 2019/2020. Study serial numbers were allocated to the accessible population for two years to facilitate the sampling process. The selection intervals of 2 were determined and used to select the participants from the women treated in 2019 and 2020, respectively. Simple balloting was used to determine the start point, which was 1, meaning that we selected patients with serial numbers: 1, 3, 5, etc.
Measures
The independent variables classified into personal, health status and environmental were collected at enrollment. The personal variables were: age (<30, 30–49, and ≥50 years old); level of education [0–7 years (primary level), 8–4 years (secondary level), and ≥15 years (tertiary level)]; marital status (single: never married, divorced, and widowed; married); employment status (officially employed and self-employed: hairdressing, petit-trading, farming, etc.); health status variables or medical characteristics were the VIA/VILI lesion characteristics (low grade versus high grade) and HIV status (negative versus positive). The environmental variables were the region where treatment was done (the region where the women were treated: Center, Littoral, Northwest, South, Southwest, and West) and the time covered to access services (less than or equal to 30 minutes or greater than 30 minutes).
The dependent variable for this study was treatment effectiveness coded as effective (Yes) or ineffective (No). Effective referred to women treated for VIA/VILI positive lesions from January 2019 to December 2020 who had their lesions cleared off during posttreatment follow-up and ineffective referred to those who presented persistent lesions.
Statistical Analysis
The data collected for the study were aggregated and cleaned in Microsoft Excel and exported to STATA version 17[17] for statistical analysis.
The association between each independent variable and dependent variable was examined in a simple logistic regression. All variables with p<0.2 were entered in the multivariable model. A backward stepwise selection was done using p-value > 0.2 as the removal criterion.
A binary logistic regression model was used to model the log odds for treatment effectiveness reviewed during the study period for demographic and clinical characteristics of the women. First, simple logistic regression analysis with just one independent variable at a time was performed with treatment effectiveness during the period of the study as the dependent variable. Secondly, the variables in the simple logistic regression model with p < 0.2 were entered into a multivariate logistic model with treatment effectiveness as the dependent variable, and education, HIV status, and lesion grade as independent variables.
The data was summarized using odds ratios with p-value and 95% CI. All statistical analyses were performed using STATA version 17[17] and a p-value less than 0.05 was considered statistically significant.
RESULTS
The 170 study participants were unevenly distributed into the six study regions (Center, Littoral, North-West, Southwest, South, and West) of Cameroon. The mean age of the participants was 36.53 (SD:08.91 and Range:16–70) and the modal age group was 30–49 [70.73% (116/170)]. The participants attained at least primary education and most of them attained secondary education [54.12% (92/170)]. Most [68.24(116/170)] of the study participants were married and self-employed [72.35% (123/170)].
One hundred and forty-five (85%) of the participants knew their HIV status and 112 (65.88%) were HIV negative. Most [87.5 l (133/152)] of the women had low-grade cervical precancer lesions and were treated using ablative procedure [81.82% (108/132)] [Table 1].
| Variables | Frequency | Percent (%) | Cum. Percent (%) |
|---|---|---|---|
| Age (n=164) – [(Years). Mean=36.53, SD=08.91, Range=16–70] | |||
| 19–29 | 36 | 21.95 | 21.95 |
| 30–49 | 116 | 70.73 | 92.68 |
| 50 + | 12 | 7.32 | 100 |
| Education Level (n=170) | |||
| Primary | 44 | 25.88 | 25.88 |
| Secondary | 92 | 54.12 | 80 |
| Tertiary | 34 | 20 | 100 |
| Marital Status (n=170) | |||
| Married | 116 | 68.24 | 68.24 |
| Single | 54 | 31.76 | 100 |
| HIV Status (n=170) | |||
| Negative | 112 | 65.88 | 65.88 |
| Positive | 33 | 19.41 | 85.29 |
| Unknown | 25 | 14.71 | 100 |
| Grade (n=152) | |||
| High | 19 | 12.5 | 12.5 |
| Low | 133 | 87.5 | 100 |
| Treatment Mode (n=132) | |||
| Ablative | 108 | 81.82 | 81.82 |
| Excisional | 24 | 18.18 | 100 |
cum.: Cumulative
Clinical Outcomes of Ablative and Excisional Cervical Precancer Treatment
More than half [54.71% (93/170)] of the women who participated in the study returned for posttreatment follow-up and 93.55% (87/93) did not present with lesions. In terms of treatment procedures, 94.37% (67/71) of those who received ablative treatment had the lesion cleared while 88.23% (14/17) who received excisional treatment also had the lesion cleared.
Of the 31 women who had a pregnancy after cervical precancer treatment, 23 (74.19%) had live and healthy babies while 5 (16.13%) had miscarriage. There was one case (3.23%) each of loss of baby at birth and preterm delivery. In terms of treatment procedure, ablation had 21 (77.78%) live births, four (14%) loss of pregnancy, and one (3.70%) case of preterm delivery while excisional had two [50% (2/4)] live births, one [25% (1/4)] stillbirth, and one [25% (1/4)] loss of pregnancy [Table 2].
| Variables | Frequency | Percent (%) | Cum. Percent (%) |
|---|---|---|---|
| Posttreatment F/U (n=170) | |||
| No | 77 | 45.29 | 45.29 |
| Yes | 93 | 54.71 | 100 |
| Treatment Effectiveness (n=93) | |||
| Ineffective | 6 | 6.45 | 6.45 |
| Effective | 87 | 93.55 | 100,00 |
| Ablative (n=71) | |||
| Ineffective | 4 | 5.63 | 5.63 |
| Effective | 67 | 94.37 | 100,00 |
| Excision (n=17) | |||
| Ineffective | 2 | 11.77 | 12.77 |
| Effective | 15 | 88.23 | 100,00 |
| Posttreatment Pregnancy Outcome - (n=31) | |||
| Baby is alive | 23 | 74.19 | 74.19 |
| Lost baby at birth | 1 | 3.23 | 77.42 |
| Lost the pregnancy | 5 | 16.13 | 93.55 |
| Preterm delivery | 1 | 3.23 | 96.77 |
| Still pregnant | 1 | 3.23 | 100.00 |
| Posttreatment Pregnancy Outcome -Ablative (n=31) | |||
| Baby is alive | 21 | 77.78 | 77.78 |
| Lost baby at birth | 0 | 0.00 | 77.78 |
| Lost the pregnancy | 4 | 14.81 | 92.59 |
| Preterm delivery | 1 | 3.70 | 96.30 |
| Still pregnant | 1 | 3.70 | 100.00 |
| Posttreatment Pregnancy Outcome - Excisional (n=4) | |||
| Baby is alive | 2 | 50.00 | 50.00 |
| Lost baby at birth | 1 | 25.00 | 75 |
| Lost the pregnancy | 1 | 25.00 | 100,00 |
Cum: Cumulative, F/U: Follow-up.
Self-reported Clinical Outcomes of Ablative and Excisional Cervical Precancer Treatment
More than half [60.12% (101/168)] of the women who received precancer treatment did not indicate any inconvenience resulting from it. The inconveniences experienced by 67 (39.88%) women treated included pain (84.85%), bleeding (6.06%), stigma (4.55%), discharging (1.52%), miscarriage/abortion (1.52%), and stress/fear (1.52%).
Most of them abstained from sex for four or more weeks [91.67% (154/168)] and a large proportion of them eventually resumed sexual activities with no challenges [88.69% (149/168)]. On resumption of sexual activities, a few women faced challenges of pain [7.14% (12/168)] and bleeding [4.17% (7/168)].
The women who participated in the study were well informed [94.08% (159/169)] about the need to return for posttreatment follow-up and they got the information mostly from cervical cancer service providers [95.03% (153/161)] and from friends [3.11% (5/161)] and media [1.86 (3/161)]. Most of them indicated that they are supposed to return for posttreatment follow-up at one year [81.93% (136/166)] and a few indicated after six months [8.43% (14/166)]. Only a few women [9.64% (16/166)] did not know the follow-up time [Table 3].
| Variables | Frequency | Percent (%) | Cum. Percent (%) |
| Treatment Inconvenience (n=168) | |||
| No | 101 | 60.12 | 60.12 |
| Yes | 67 | 39.88 | 100 |
| Description of Treatment Inconveniences (n=66) | |||
| Pain | 56 | 84.85 | 84.85 |
| Bleeding | 4 | 6.06 | 90.91 |
| Discharging | 1 | 1.52 | 92.42 |
| Miscarriage/abortion | 1 | 1.52 | 93.94 |
| Stigma | 3 | 4.55 | 98.48 |
| Stress/fear | 1 | 1.52 | 100 |
| Duration of Abstinence from Sex (n=168) | |||
| ≤4 weeks | 14 | 8.33 | 8.33 |
| ≥4 weeks | 154 | 91.67 | 100 |
| Sexual Resumption Challenges (n=168) | |||
| None | 149 | 88.69 | 88.89 |
| Pain | 12 | 7.14 | 9583 |
| Bleeding | 7 | 4.17 | 100 |
| Posttreatment Pregnancy? (n=162) | |||
| NO | 119 | 73.46 | 73.46 |
| YES | 43 | 26.54 | 100 |
| Treatment Follow-Up Awareness (n=169) | |||
| NO | 10 | 5.92 | 5.92 |
| YES | 159 | 94.08 | 100 |
| Source of Posttreatment Follow-Up Awareness (n=161) | |||
| Health worker | 153 | 95.03 | 95.03 |
| Heard from friends | 5 | 3.11 | 98.14 |
| Heard from media | 3 | 1.86 | 100 |
| Timing of Posttreatment Follow-Up Awareness (n=166) | |||
| 1 year after treatment | 136 | 81.93 | 81.93 |
| 6 months after treatment | 14 | 8.43 | 90.36 |
| Do not know | 16 | 9.64 | 100.00 |
cum.: Cumulative
Association between Characteristics of Participants and Treatment Outcomes
Logistic regression test indicated that there was significant association between outcome of the treatment and clinical status (HIV status and grade of the lesion) of the woman. Women who were HIV positive were 89% or 0.89 times [aOR=0.11, 95% CI (0.01 0.85), p=0.034] less likely to have effective treatment for cervical precancer when compared to HIV-negative women. Those with low-grade lesions on the other hand were eight times [aOR=8.39, 95% CI (1.10 64.06), p=0.04] more likely to have effective treatment for cervical precancer compared to those with high-grade lesions [Table 4].
| Variables | Treatment Outcome | COR (95%CI) | p-value | aOR (95%CI) | p-value | |
|---|---|---|---|---|---|---|
| Ineffective | Effective | |||||
| Age (n=91) – [(Years). Mean=36.53, SD=08.91, Range=16–70] | ||||||
| 16–29 | 0 (0.00) | 18 (20.93) | 1 | |||
| 30–49 | 4 (80.00) | 60 (69.767) | 1.88 (0.19 18.93) | 0.594 | ||
| ≥50 | 1 (20.00) | 8 (9.30) | 1 | |||
| Education Level (n=93) | ||||||
| Primary | 4 (66.67) | 22 (25.29) | 1 | |||
| Secondary | 2 (33.33) | 47 (54.02) | 4.27 (0.73 25.12) | 0.108 | 1.75 (0.2 13.4) | 0.59 |
| Tertiary | 0 (0.00) | 18 (20.69) | ||||
| Occupation (n=93) | ||||||
| Unemployed | 0 (0.00) | 22 (25.29) | ||||
| Employed | 6 (100.00) | 65 (74.71) | ||||
| Marital Status (n=93) | ||||||
| Married | 4 (66.67) | 61 (70.11) | 1 | |||
| Single | 2 (33.33) | 26 (29.89) | 0.85 (0.15 4.95) | 0.859 | ||
| HIV Status (n=93) | ||||||
| Negative | 2 (33.33) | 70 (80.46) | 1 | |||
| Positive | 4 (66.67) | 14 (16.09) | 0.1 (0.02 0.60) | 0.012 | 0.11 (0.01 0.85) | 0.034 |
| Unknown | 0 (0.00) | 3 (3.45) | ||||
| Grade (n=88) | ||||||
| High Grade | 3 (50.00) | 8 (9.20) | 1 | |||
| Low Grade | 3 (50.00) | 79 (90.80) | 9.88 (1.70 57.27) | 0.011 | 8.39 (1.10 64.06) | 0.04 |
| Treatment Mode (n=88) | ||||||
| Ablative | 4 (66.67) | 67 (81.71) | 1 | |||
| Excisional | 2 (33.33) | 15 (18.29) | 0.45 (0.07 2.68) | 0.378 | ||
| Access to Clinic Time (n=91) | ||||||
| ≤30 Minutes | 2 (40) | 38 (44.19) | 1 | |||
| ≥30 Minutes | 3 (60) | 48 (55.81) | 0.84 (0.13 5.30) | 0.855 | ||
COR: Crude odds ratio, AOR: Adjusted odds ratio, CI: Confidence interval. Statistically significant p<0.05 in bold.
DISCUSSION
Clinical Outcomes of Ablative and Excisional Cervical Precancer Treatment
Cervical precancer posttreatment follow-up uptake was slightly above average. This was similar to the findings of Manga et al., in which 55.2% of the women returned for at least one posttreatment follow-up during a period of five years.[18] Most (93.55%) of the women who return for posttreatment follow-up did not present with lesions which falls within the range of 77%–97% for ablative and excisional cervical precancer treatment reported by Martin-Hirsch et al. in the Cochrane Database Systematic Review in 2020.[19,20]
A substantial proportion of the women who got pregnant after the treatment delivered live and healthy babies. Few women experienced loss of pregnancy, loss of baby at birth, and preterm delivery. Other adverse effects experienced after the treatment procedures included pain, bleeding, stigma, and fear/stress. These findings were consistent with those of Santesso et al., in a systematic and meta-analysis of the benefits and harms of ablative and excisional cervical precancer treatment conducted in 2016 where recurrence was 5.3%, 12 months after cryotherapy or loop electrosurgical excision procedure (LEEP). They were equally similar to the findings of Castle et al., on the treatment of cervical intraepithelial lesions conducted in 2017 in which cryotherapy and thermal coagulation successfully eradicated 75–85% of high-grade cervical lesions with minor adverse effects.[11,12]
Most of the women who underwent ablative and excisional treatment procedures abstained from sex for four or more weeks and had no major challenges upon resumption. The challenges faced by a few women on the resumption of sexual activities comprised pain and bleeding. This is similar to the findings of Pinder et al. in 2020 where few participants complained of moderate to severe pain after ablative and excisional procedures.[21]
Women who were HIV positive were less likely to have an effective treatment for cervical precancer when compared to HIV-negative women. Those with low-grade lesions were more likely to have effective treatment for cervical precancer treatment compared to those with high-grade lesions. This agreed with the study by Oga et al., on recurrence of cervical intraepithelial lesions after ablative treatment in HIV-positive and HIV-negative women in Nigeria in 2016 where recurrence of lesions was higher in HIV-positive women compared to HIV-negative women.[3]
The women who participated in the study were well informed about the need to return for posttreatment follow-up and they got the information mostly from cervical cancer service providers and then from friends and media. Most of them indicated that they were supposed to return for posttreatment follow-up at one year and a few indicated after six months. A few women did not remember the follow-up appointment time. Follow-up at one year was appropriate for women who were HIV-negative and those who did not experience any inconvenience from the intervention procedure. The fact that most of the information on posttreatment follow-up was obtained from the service providers indicates that service providers disseminate appropriate information on this special aspect of cervical cancer care. The low cervical precancer posttreatment follow-up cannot therefore be attributed to a knowledge gap but patient-related factors. This matched with the findings of Nkfusai et al. on the assessment of knowledge and risk of cervical cancer among women in the Buea Health District in Cameroon in 2019 which indicated that women were informed about cervical cancer.[22,23]
Limitations
Our study had some limitations which included dependence on data collected by the service providers on the enrollment of the women for treatment to a greater extent and missing data on clients. We did not have enough time and other resources to recollect missing data from the client’s individual records (consultation card).
CONCLUSION AND GLOBAL HEALTH IMPLICATIONS
The combined clinical effectiveness of ablative and excisional procedures was 93.55% and this was disaggregated to 94.37% and 88.23% for ablative and excisional procedures, respectively, with no severe adverse clinical effects. Posttreatment follow-up remained only slightly above average (54.71%) despite the high awareness on its need and timing. Most of the women who got pregnant after the procedures delivered live and healthy babies. These procedures are thus safe, convenient, and effective. Women who were HIV-positive were less likely to have effective treatment for cervical precancer compared to HIV-negative women. Those with low-grade lesions were more likely to have effective treatment for cervical precancer treatment compared to those with high-grade lesions.
Key Messages
-
Ablative and excisional procedures boast a 93.55% overall effectiveness, with minimal adverse effects, underscoring their safety and effectiveness in treating cervical precancer.
-
Cervical precancer posttreatment follow-up remained low (54.71%) despite the high (81.93%) awareness on the importance of posttreatment follow-up among women, thus continuum of care for cervical precancers needs to be strategized.
-
Women who got pregnant after undergoing cervical precancer treatment delivered live and healthy babies, affirming the safety and effectiveness of ablative and excisional procedures.
Acknowledgments
The authors are grateful to all who took part in this study.
COMPLIANCE WITH ETHICAL STANDARDS
Conflicts of Interest
The authors declare that they have no conflict of interest.
Financial Disclosure
None.
Funding/Support
None.
Ethics Approval
Ethical approvals were obtained from the Institutional Review Board of the Faculty of Health Sciences, University of Buea (Number 1791-04) and from the Cameroon Baptist Convention Health Services Institutional Review Board, Cameroon (Approval Number IRB2022-45).
Declaration of Patient Consent
Patient’s consent not required as there are no patients in this study.
Use of Artificial Intelligence (AI)-Assisted Technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
None.
REFERENCES
- Web Annex A. Syntheses of evidence; 2021. [Accessed 2024 Feb 04]. Available from: https://apps.who.int/iris/bitstream/handle/10665/342366/9789240030886-eng.pdf.
- Global strategy to accelerate the elimination of cervical cancer as a public health problem and its associated goals and targets for the period 2020 – 2030. Vol 2
- Recurrence of cervical intraepithelial lesions after thermo-coagulation in HIV-positive and HIV-negative Nigerian women. BMC Womens Health. 2016;16:25.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- National guideline clearinghouse | WHO guidelines for screening and treatment of precancerous lesions for cervical cancer prevention (2nd ed). World Health Organization; 2021. [Accessed 2024 Feb 04]. Available from: http://www.guideline.gov/content.aspx?f=rss&id=49521&osrc=12
- Efficacy of loop electrosurgical excision procedure with cold coagulation for treating cervical intraepithelial neoplasia: A two center cohort study. Obstet Gynecol Sci. 2017;60(2):200-6.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- WHO technical guidance and specifications of medical devices for screening and treatment of precancerous lesions in the prevention of cervical cancer.
- Interpretation of “WHO guideline for screening and treatment of cervical pre-cancer lesions for cervical cancer prevention, 2nd ed.”. Zhonghua Yi Xue Za Zhi. 2021;101(34):2653-7. Chinese. doi:10.3760/cma.j.cn112137-20210719-01609
- [CrossRef] [PubMed] [Google Scholar]
- WHO Guidelines for the use of thermal ablation for cervical pre-cancer lesions.
- Implementing a fee-for-service cervical cancer screening and treatment program in Cameroon: Challenges and opportunities. Oncologist. 2017;22(7):850-9.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Implementation strategies to improve cervical cancer prevention in sub-Saharan Africa: A systematic review. Implement Sci. 2018;13(1):1-18.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Treatment of cervical intraepithelial lesions. Int J Gynaecol Obstet. 2017;138:20-5.
- [CrossRef] [PubMed] [Google Scholar]
- Systematic reviews and meta-analyses of benefits and harms of cryotherapy, LEEP, and cold knife conization to treat cervical intraepithelial neoplasia. Int J Gynaecol Obstet. 2016;132(3):266-71.
- [CrossRef] [PubMed] [Google Scholar]
- Feasibility of thermocoagulation in a screen-and-treat approach for the treatment of cervical precancerous lesions in sub-Saharan Africa. BioMed Central Womens Health. 2017;17(1):2.
- [CrossRef] [Google Scholar]
- Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394-424.
- [CrossRef] [PubMed] [Google Scholar]
- Challenges and opportunities associated with cervical cancer screening programs in a low income, high HIV prevalence context. BioMed Central Womens Health. 2021;21(1):1-14.
- [CrossRef] [Google Scholar]
- Prevalence, predictors, and same day treatment of positive VIA enhanced by digital cervicography and histopathology results in a cervical cancer prevention program in Cameroon. PLoS One. 2016;11(6)
- [CrossRef] [Google Scholar]
- Stata Functions Reference Manual.
- Factors associated with adherence to post-treatment follow-up among a cohort of women with acetic acid/Lugol’s iodine positive lesions of the cervix in Cameroon: A retrospective cohort study. Gynecol Oncol Rep. 2023;49:101269.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Ablative therapies for cervical intraepithelial neoplasia in low-resource settings: Findings and key questions. J Glob Oncol. 2018;4:1-10.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Europe PMC funders group surgery for cervical intraepithelial neoplasia. Cochrane Database Syst Rev. 2015;2015(9):CD008478.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Thermal ablation versus cryotherapy or loop excision to treat women positive for cervical precancer on visual inspection with acetic acid test: pilot phase of a randomised controlled trial. Lancet Oncol. 2020;21(1):175-84.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Prevalence of precancerous cervical lesions in women attending Mezam Polyclinic Bamenda, Cameroon. Pan Afr Med J. 2019;32:174.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Assessment of the current state of knowledge and risk factors of cervical cancer among women in the Buea Health District, Cameroon. Pan Afr Med J. 2019;33:1-9.
- [CrossRef] [Google Scholar]





