Translate this page into:
Comparative Study of the Prevalence of Type-2 Diabetes Mellitus in Various Demographic Regions of Andhra Pradesh, India: a Population based Study
*Corresponding author email: drgmani@gmail.com
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Background and Introduction:
Diabetes is increasing at alarming rate among Indians especially South Indians with prevalence of diabetes mellitus (PODM) varying in populations of different regions. This study assesses PODM in three geographical areas, namely: tribal, semi-urban, and urban, and to compare the diabetes risk in northern coastal districts of Andhra Pradesh state in India.
Methodology:
A random sampling method was followed to study the prevalence of diabetes in about 3,000 individuals of age group between 15-68 years, selecting 1,000 individuals from each area. As per 1988 World Health Organization criteria and norms, diabetes mellitus was diagnosed on the basis of 75-g oral glucose tolerance test (OGT). Statistical analyses were conducted using Microsoft Excel 2007.
Results:
The analysis of the study indicates that 35.5% individuals were identified to be diabetic, especially 7.8% from Tribal area, 12.5% from semi-urban and 15.1% from urban area.
Conclusion and Global Health Implications:
The study indicates that people in urban area were more prone to type-2 diabetes than those in Tribal and semi-urban area. New cases of diabetes were reported in tribal areas when compared to semi-urban and urban areas indicating that rural people were not spared from diabetes. The study also indicates that there is an increase in the prevalence of diabetes in tribal area of Andhra Pradesh State of India when compared to previous studies.
Keywords
Diabetes Mellitus (DM)
Prevalence of Diabetes Mellitus (PODM)
Oral Glucose Tolerance Test (OGT)
1. Background and Introduction
Now the time has come to allocate resources and permit national planning to quantify the prevalence of diabetes mellitus and the number of people affected by diabetes, now and in the future. Population growth, aging, urbanization, low physical activity and obesity are main causative factors of high prevalence of DM.[1] Diabetes mellitus (DM) is a chronic metabolic disorder in which the body does not produce or properly utilize insulin. Insulin is a hormone produced by the β-cells of the pancreas that is needed to absorb the glucose from the bloodstream into the cell which is utilized for the production of energy. The characteristic symptoms of diabetes are excessive urine production (polyuria), excessive thirst or increased fluid intake (polydipsia), excessive food intake (polyphagia), blurred vision, hypertension etc. These symptoms may not be observed if the blood sugar is mildly elevated.
The World Health Organization (WHO) stated that the incidence of DM appears to be increasing by about 6% per year and also predicted that the greatest number of diabetic individuals in the world by the year 2030 would be 9.40 million. Studies of industrial populations in India revealed that diabetes has become top most major problem in India and also worldwide and the deaths have increased by 35%.[2] The blue circle was recently adopted as the symbol for diabetes; much like the Red Ribbon is for AIDS.
India had 32 million diabetic patients in the year 2000 and this number would increase to 80 million by the year 2030.[1] International Diabetes Federation (IDF) also reported that the total number of diabetic subjects in India is 41 million in 2006 and that this would rise to 70 million by the year 2025.[3]
In a study from Cuttack, India showed that population based surveys carried out in the early 1970s in different Indian cities and nearby rural areas reported prevalence of diabetes ranging from 1.2% to 2.5%.[4] The first multi-center study in India was done by the Indian Council of Medical Research (ICMR) between 1972 and 1975. This study reported a prevalence of 3.0 % in urban areas and 1.3% in rural areas. The early signs of the looming diabetes epidemic were seen in Tenali, a semi-urban town in Andhra Pradesh which reported a high prevalence of 4.7%.[5] The first study in South India at Vellore in Tamil Nadu has shown that prevalence of diabetes is 2.5%.[6] A population based survey carried out in Chandigarh, Pondicherry and Varanasi towns reported the prevalence rates of 2.9%, 0.7% and 2.7% respectively.[7-9]
Some researchers have shown prevalence of 5.0% DM in Kudremukh, a semi-urban area in Karnataka. [10] The prevalence of known diabetes in Eluru, another town in west Godavari district of Andhra Pradesh was 1.5%.[11] The prevalence of type 2 diabetes had risen to 11.6% in the same urban area, that is Eluru, which had a prevalence of 8.2% five years before.[11, 12]
Differences in the prevalence of diabetes have been consistently reported from India in Urban and rural area. A recent study from rural Maharashtra showed a high prevalence of 9.3% DM.[13] The Prevalence of Diabetes in India Study carried out in 108 centers of India opines that 5.9% of urban population and 2.7% of rural population was affected by diabetes as per the WHO criteria.[14] According to the American Diabetic Association (ADA) criteria, the diabetic prevalence rates were 4.6% and 1.9% in urban and rural areas respectively.[15] It is quite evident from these studies that diabetes is becoming a major health problem in India. Diabetes cases are increasing day by day in rural as well as in tribal areas of Andhra Pradesh state also. The risk factors for DM include stress, environment, food habits, style of living, etc. vary in the three areas selected for the study. Apart from that the first author of this paper is from one of the study areas, that is Paderu tribal village and she could observe an increase of cases of DM in many tribal people who are going towards modernization and change of food habits when compared to earlier days. We could also observe the difference in some distinguishing characteristics like population, literacy and urbanicity of the three areas selected for the study. With the above supporting data we could draw some conclusions to our study (Table 1). Based on the above sociodemographic and socio economic data of rural people and their counterparts, a survey has been carried out to understand the prevalence of type-2 diabetes and to understand its spread, increase and causes in a tribal area (around Paderu village), urban area (Visakhapatnam city) in Visakhapatnam district and in a semi-urban area (i.e. Rajahmundry town) in East Godavari district of Andhra Pradesh state in India. This paper presents the results of the study.
| Region | Urbanicity (Rural/Urban/Semi urban) | Population | Literacy | ||||
|---|---|---|---|---|---|---|---|
| Total | Male | Female | Total | Male | Female | ||
| Paderu | Rural | 58,983 | 28902 | 30081 | 60.0 | 57.1 | 42.9 |
| Visakhapatnam city | Urban | 1,728,128 | 873,599 | 854,529 | 81.79 | 81.25 | 76.22 |
| Rajahmundry | Semi urban | 341,831 | 168,735 | 173,096 | 84.12 | 87.91 | 80.45 |
2. Methodology
2.1. Study area
To understand the prevalence of diabetes and its causes the present study was carried out in and around Paderu (PDR) village that comes under tribal area and in Visakhapatnam (VSKP) city coming under urban area and in Rajahmundry (RJY) town falling in Semi-urban area. The first two areas are located in Visakhapatnam district and the third one is located in East Godavari (EG) district of Andhra Pradesh. As per 2011 census based on population, Paderu area has total population of 58,983. Out of which 49% are male and 51% are female. Coming to the socio economic conditions like Education of Paderu area, illiterates are 41%, people having school education are 40.8% and higher education is about 14.1%. Overall literacy is 60%, in which males are dominant. Regarding population-level incomes, higher income groups earning more than 10,000/- rupees per month are less (29.5%) when compared to people earning more than 1000/-(39.7%) rupees and more than 5000/- (30.8%). Nearly 76% of males are employed when compared to females (57.8%) in this tribal area. The main occupation for these people is marketing of minor forest produce and to some extent Agriculture, fishing and hunting. Nowadays, some tribal people are also employed in government sectors. (Figure 1 and Table 2).
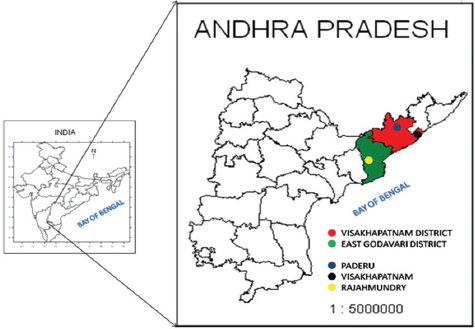
- Study area
| Indicator | Status | Percent |
|---|---|---|
| Education | Illiterate | 41 |
| Primary | 21.6 | |
| Secondary | 19.2 | |
| Above | 14.1 | |
| Income (in Rupees) | >1000/- | 39.7 |
| >5000/- | 30.8 | |
| >10000/- | 29.5 | |
| Occupation | Employed | |
| M | 75.5 | |
| F | 57.8 | |
| Unemployed | ||
| M | 13.3 | |
| F | 21.2 | |
2.2. Study instruments
A proforma was prepared to note the bio-data of sampled candidates i.e. Name, age, sex, onset age of the disease, height, weight, body mass index (BMI), waist to hip ratio (W/H), genetic background (GB) with regard to diabetes, blood sugar levels both fasting blood sugar (FBS) and post prandial (PP), employment status, distance and mode of travel for regular job purpose etc. If the person is already diabetic, his/her weight at the onset of disease and present weight are also noted. This proforma helped us a lot in getting important information regarding the prevalence of the disease, sex-wise, the onset of the age and also factors causing the disease etc. The present management practices like diet control, exercise, type of exercise and number of times per day, intake of sweets and beverages, etc. being adopted by each person suffering with the disease is also taken into consideration for drawing results.
This study was based mainly on personal interaction with every individual studied in order to fill up questionnaire that forms the main database for the study. From each area studied, a total of 1,000 subjects were selected for the study. The areas selected for the study have variations in population size. Paderu has a population of 58,983; Visakhapatnam city has a population of 1,728,128; and the Semi urban area Rajahmundry has a population of 341,831 (Table 1). The study population included all men and women aged 15-68 years. Random samples of the study subjects were drawn from each locality of the selected area proportional to their population sizes. The identification of the localities and households were done with the help of a field staff of primary health centers. The selection of the lane and first house within the locality was done by random selection by employing the procedure described in the cluster sampling technique used for evaluation of universal immunization coverage.[16] Starting from the first house onwards all the houses within the lane were covered continuously, keeping toward the left. This procedure was continued until the sample size for each locality was obtained.
After establishing a good rapport and getting their consent, complete details of person was recorded as per the proforma mentioned above through personal interviews. The proforma was designed in consultation with local endocrinology physicians. Ethical clearance for the study was obtained from the Institutional Ethical Committee of Andhra University prior to the initiation of the study.
In all the three study areas, the proforma of illiterate uneducated and old individuals was filled personally. The people were cooperative, gave all the required information with great enthusiasm and readily came forward to undergo the OGT test, an important parameter to know whether one is diabetic or not. Subjects were screened for both FBS and PP blood sugar using a glucometer. The glucometer which was used in our study is Accu-Chek Active of Germany Company. The diabetic screening test was first done in the early morning with the fasting sample, and then the subjects were given 75 gm of anhydrous glucose in 200 ml of water and exactly after 2 hours, the sample for pp screening was taken. Results were analyzed as per WHO criteria. The same procedure was followed for each individual studied in all the three areas.
3. Results
3.1. Prevalence of type-2 diabetes in Tribal area (Around Paderu Village)
A sample of 1000 candidates has been chosen for the study in Tribal area i.e. in Paderu division in Visakhapatnam district. These 1,000 candidates were spread over four mandals (mandals are administrative divisions or sub districts comprising several villages or village clusters in Visakhapatnam district viz., Araku (Station 1); Chintapalli (Station 2); Paderu (Station 3); and Pedabayalu (Station 4). In Station 1, out of 206 subjects studied, 20 were positive, of which 6 were old cases and 14 were new cases. Out of 194 subjects studied in Station 2, 14 were positive which include 5 old and 9 new cases. In Station 3, out of 343 subjects studied, 26 were positive, of which 7 old and 19 new cases. Out of 257 subjects studied in Station 4, 18 were positive, of which 5 old and 13 new cases. Out of these 1,000 candidates 23 were identified as old cases and other 55 were identified as new cases, thus making total positive cases as 78 (7.8%). Surprisingly, during the conversation with 55 new patients, it was understood that these candidates were unaware of the disease they are suffering. The results of the study in this area are shown in Table 3 and Figure 2.
| Area of study | Stn1 (Araku) | Stn2 (Chintapalli) | Stn3 (Paderu) | Stn4 (Pedabayalu) | Total |
|---|---|---|---|---|---|
| Total case studies | 206 | 194 | 343 | 257 | 1000 |
| Old cases | 06 | 05 | 07 | 05 | 23 |
| New cases | 14 | 09 | 19 | 13 | 55 |
| Total positive cases | 20 | 14 | 26 | 18 | 78 |
| Prevalence (%) | 9.7 | 7.2 | 7.6 | 7.0 | 7.8 |
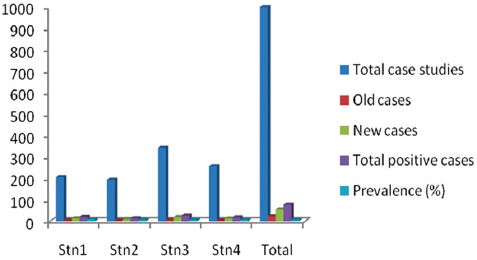
- Prevalence of type-2 diabetes in Tribal area, Paderu division
3.2. Prevalence of type-2 diabetes in semi-urban area (Rajahmundry town)
The total number of subjects taken in Rajahmundry town was spread into three localities viz. Jaya Krishnapuram (JKP), Veerabhadrapuram (VBP) and Devichowk (DC). Out of total 422 subjects studied in Jaya Krishnapuram area 54 were positive of which 39 were old cases and 15 were new cases. Out of total 316 subjects studied in Veerabhadrapuram area 43 were positive which include 35 old and 8 new cases Out of the total 242 cases studied in Devichowk, 31 were positive, with 22 old and 9 new cases. Interestingly all these three areas have more or less equal prevalence as shown in the Table 4 and Figure 3.
| Area of study | JayaKrishnapuram (JKP) | Veerabhadrapuram (VBP) | Devichowk (DC) | Total |
|---|---|---|---|---|
| Total case studies | 442 | 316 | 242 | 1000 |
| Old cases | 39 | 35 | 22 | 96 |
| New cases | 15 | 08 | 09 | 32 |
| Total positive cases | 54 | 43 | 31 | 128 |
| Prevalence (%) | 12.22 | 13.61 | 12.81 | 12.81 |
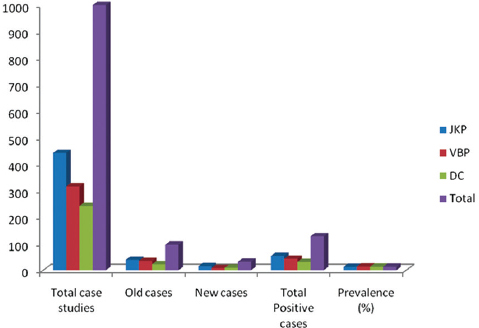
- Prevalence of type-2 diabetes in semi-urban area, Rajahmundry
3.3. Prevalence of type-2 diabetes in urban area (Visakhapatnam City)
Three localities viz., Gopalapatnam (GPTM), Saligramapuram (SGRP) and Maharanipeta (MRP) were selected for the present study in this city. These areas were selected such that each area was separated from the others by a considerable distance i.e. about 5-6 km. A total of 1000 subjects were studied with 226 in Gopalapatnam, 326 in Saligramapuram and 448 in Maharanipeta. Of these 226 cases studied in Gopalapatnam 13.7% were affected by diabetes while 17.4% of 326 in Gopalapatnam and 14% of 448 in Maharanipeta were affected by DM respectively. Thus, the total prevalence of DM in this urban Visakhapatnam is 15.1%. Out of these three localities, SGRP showed highest prevalence of DM. The results of the study in Visakhapatnam are shown in Table 5 and Figure 4.
| Area of study | Gopalapatnam (GPTM) | Saligramapuram (SGRP) | Maharanipeta (MRP) | Total |
|---|---|---|---|---|
| Total case studies | 226 | 326 | 448 | 1000 |
| Old cases | 18 | 40 | 51 | 109 |
| New cases | 13 | 17 | 12 | 42 |
| Total positive cases | 31 | 57 | 63 | 151 |
| Prevalence (%) | 13.7 | 17.4 | 14 | 15.1 |
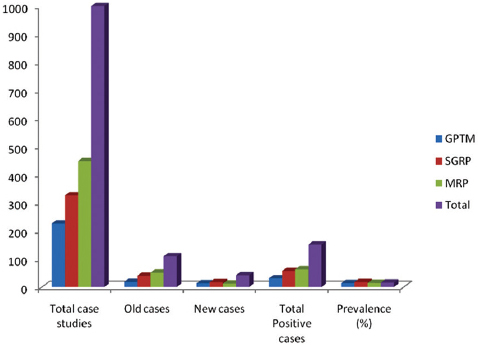
- Prevalence of type-2 diabetes in urban area (i.e., Visakhapatnam city)
3.4. Comparison of tribal, semi-urban and urban areas
The three areas selected under the study are different in socio-economic status and also life-style. The study included 1000 cases in each area. The prevalence of DM is higher in urban area (15.1%) when compared to semi-urban area (12.6%) and tribal area (7.8%) The analysis of the present study indicates that the DM is increasing with faster rate (5.5%) in tribal than in the other two areas where the rates of increase are 4.2% in urban and 5.0% in the semi-urban areas as evident from the new cases identified in each area. There is striking difference between the three areas with percentage ranging from 4.6% between tribal and semi-urban, 8.3% between tribal and urban and 2.5% between semi-urban and urban as shown in Table 6 and Figure 5. The Flow chart describing the study design and results in the three study areas is shown in Figure 6.
| Area of study | Tribal area | Semi-urban area | Urban area |
|---|---|---|---|
| Total case studies | 1000 | 1000 | 1000 |
| Old cases | 23 | 30 | 109 |
| New cases | 55 | 96 | 42 |
| Total positive cases | 78 | 126 | 151 |
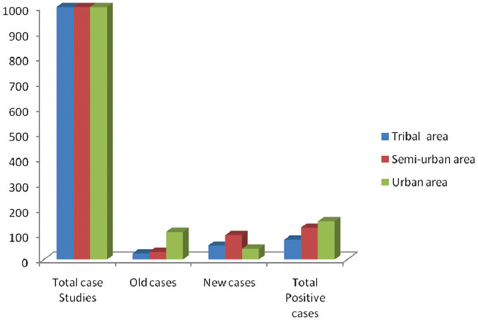
- Prevalence of type-2 diabetes in tribal, semi-urban, & urban areas of Andhra Pradesh
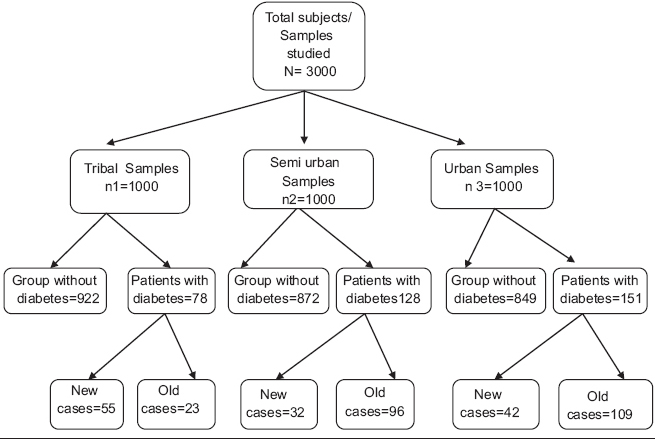
- Flow chart showing the study design and results in three areas of study
4. Discussion
In the present survey, the prevalence of diabetes and its increase in three demographical areas i.e., tribal, semi-urban and urban in north coastal Andhra Pradesh state of India were studied. Results of the above study indicate the highest prevalence of DM in urban area (15.1%), followed by semi urban (12.8%) and tribal areas (7.8%). The prevalence of the DM in urban area is nearly two times greater than that in the tribal area. The difference in prevalence from area to area may be due to the prevailing environmental conditions in the area, diet practices followed in that area, life style, awareness of the disease, socioeconomic status etc. There may be many other factors like obesity, genetic background, stress etc. for the cause of this disease. Visakhapatnam, an industrial city, is stamped as one of the pollutant cities in the country. Air and water pollution affect mankind thereby weakening the health status.
The 15% prevalence of DM in Visakhapatnam city found in this study is higher than that found earlier in several other cities in India viz.7.5% in Mumbai, 13.5% in Chennai, 12.4% in Bangalore, 11.7% in Kolkata, and 11.6% in New Delhi.[17] However, it is less than the prevalence in Hyderabad (16.6%) which was the capital city of Telangana state.[17] This indicates that the urban population in Andra Pradesh is more prone to DM than those in other cities in India. Interestingly, the prevalence of diabetes also varies considerably in different parts of rural India as observed in several studies.[18-20] Various studies have revealed that the prevalence of DM was at lower level in rural Punjab, in rural Kerala, in Mysore and in rural Nagpur when compared to our findings in the present study viz 7.8%.[21-23] The studies of Chennai Urban Rural Epidemiology Study (CURES) group have shown a prevalence of 15.5% in Chennai.[24] Similar studies carried out in Kerala, indicated a prevalence of 6.0% in urban area and 2.8% in tribal area as was observed in the present study. [25]
Number of people with diabetes in India is currently around 40.9 million and is expected to rise to 69.9 million by 2025 unless immediate preventive measures are taken.[26] Self-care behaviors like healthy eating, being physically active, monitoring of blood sugar, compliance with medications, good problem-solving skills, healthy coping skills and risk-reduction behaviors are essential for patients with diabetes along with good glycemic control.[27]
5. Conclusions and Global Health Implications
There is a vast variation in the prevalence of DM among urban, semi urban, and tribal areas as evident from the current study and other studies in various parts of India. In the present study we observed that DM cases are increasing in India day by day in urban and semi-urban areas but the increase is drastic in the tribal area. Studies from various parts of the world revealed that there was an association between illiteracy and DM,[28-32] which was also observed in the case of tribal areas in the present study.
There is an urgent need to arrange several awareness programs in different parts of the country particularly in tribal areas about symptoms of DM, factors causing it, medication, complications and its preventions etc. Imparting knowledge among the tribal about DM is highly essential at this juncture. The Government and non-government organizations should take leading steps in this regard. Taking the help from the students starting from school-aged children, press and media and health workers for this purpose may yield better results in controlling the spread of this dangerous disease in India.
Acknowledgment
The authors are grateful to Dr. K. V. Subrahmanyam, and Dr. Hemalatha from Visakhapatanam, Dr. N. B. Prasad, Rajahmundry and Dr. Krishna Rao from Paderu for their valuable assistance during the field work.
Conflict of Interest: None declared
Ethical Consideration:: This study was approved by the Institutional ethical committee of Andhra University, Visakhapatnam in 2008.
References
- Global prevalence of diabetes: Estimates for the year 2000 and projections for 2030. Diabetes Care. 2004;27:1047-53.
- [Google Scholar]
- on behalf of the Sentinel Surveillance System for Indian Industrial Populations Study Group. Methods for establishing a surveillance system for cardiovascular diseases in Indian industrial populations. Bulletin of the World Health Organization. 2006;84:461-9.
- [Google Scholar]
- Diabetes and impaired glucose tolerance. In: Diabetes Atlas. Belgium: International Diabetes Federation; 2006. p. :15-103.
- [Google Scholar]
- Survey for detection of glycosuria, hyperglycaemia and diabetes mellitus in urban and rural areas of Cuttack district. Journal of the Association of Physicians India. 1971;19:681.
- [Google Scholar]
- Diabetes Research Foundation Chennai, Development and Updation of the Diabetes Atlas of India. 2010
- [Google Scholar]
- A Study in retrospect of hospitalized patients of diabetes mellitus in South India. Journal of the Association of Physicians India. 1964;12:255.
- [Google Scholar]
- Prevalence of postprandial glycosuria in an urban community. Journal of the Association of Physicians India. 1966;14:519.
- [Google Scholar]
- Survey of diabetes mellitus in Pondicherry. In Diabetes in the Tropics. Diabetic Association of India, Bombay 1966:33.
- [Google Scholar]
- Epidemiological study of diabetes in the town of Varanasi. In Diabetes in the town of varanasi, In Diabetes in the Tropics. Diabetic Association of India, Bombay 1966:76.
- [Google Scholar]
- High prevalence of diabetes in an urban population in South India. British Medical Journal. 1988;297:587-590.
- [Google Scholar]
- The Eluru Survey: Prevalence of known diabetes in a rural Indian population. Diabetes Research and Clinical Practice. 1989;7:29.
- [Google Scholar]
- Rising prevalence of NIDDM in urban population of India. Diabetologia. 1997;40:232-237.
- [Google Scholar]
- To identify the risk factors for high prevalence of diabetes and impaired glucose tolerance in Indian rural population. International Journal of Diabetes in Developing Countries. 2006;26:19-23.
- [Google Scholar]
- Prevalence of diabetes in India Study, Study of diabetes. Diabetes Research and Clinical Practice. 2004;66:309-315.
- [Google Scholar]
- Diabetes mellitus in Dombivli--an urban population study. Journal of Association of Physicians India. 2001;49:713-16.
- [Google Scholar]
- Expanded program on immunization World Health Organization. Available from: http://www.whqlibdoc.who.int/hq/1991/WHO_EPI_MLM_91.1.pdf
- High prevalence of diabetes and impaired glucose tolerance in India: National Urban Diabetes Survey. Diabetologia. 2001;44:1094-101.
- [Google Scholar]
- Diabetes, Park’s textbook of preventive and social medicine 2000:292-5.
- Impaired glucose tolerance and diabetes mellitus in a rural population in South India. Diabetes Research and Clinical Practice. 1994;24:47-53.
- [Google Scholar]
- A study of prevalence of diabetes mellitus in working women of banking sector, Thesis Submitted to Nagpur University for M.D.(PSM) 1998
- [Google Scholar]
- High prevalence of multiple coronary risk factors in Punjabi Bhatia community. Indian Heart Journal. 2004;56:646-52.
- [Google Scholar]
- Prevalence of diabetes in a rural area of central India. International Journal of Diabetes in Developing Countries. 2007;27:8-10.
- [Google Scholar]
- Prevalence of known and undetected diabetes and associated risk factors in central Kerala--ADEPS. Diabetes Research and Clinical Practice. 2006;74(3):289-94.
- [Google Scholar]
- Secular trends in the prevalence of diabetes and impaired glucose tolerance in urban South India-the Chennai Urban Rural Epidemiology Study (CURES-17) Diabetologia. 2006;49:1175-1178.
- [Google Scholar]
- High prevalence of type 2 diabetes in an urban settlement in Kerala, India. Ethnic Health. 1999;4:231-9.
- [Google Scholar]
- Diabetes in 2007- What are the promises and challenges? Indian Journal of Medical Research 125; March 2007
- [Google Scholar]
- Role of self-care in management of diabetes mellitus. Journal of Diabetes and Metabolic Disorders. 2013;12:14.
- [Google Scholar]
- Lack of health insurance and decline in overall health in late middle age. New England Journal of Medicine. 2001;345:1106-12.
- [Google Scholar]
- Diabetes and urbanization in the Omani population: an analysis of national survey data. Population Health Metrics. 2006;4:5.
- [Google Scholar]
- Prevalence of diabetes, impaired fasting glucose and insulin resistance syndrome in an urban Indian population. Diabetes Research and Clinical Practice. 2003;61(1):69-76.
- [Google Scholar]
- Relationship of literacy and heart failure in adults with diabetes. BMC Health Service Research. 2007;7:98.
- [Google Scholar]
- Association between socio-demographic factors and diabetes mellitus in the north of Iran: A population based study. International Journal of Diabetes Mellitus 2 2010:154-157.
- [Google Scholar]





