Translate this page into:
Correlates of Stillbirths at Nyeri Provincial General Hospital, Kenya, 2009-2013: A Retrospective Study
*Corresponding author email: jcheptum@yahoo.com
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Background:
Death of a baby in-utero is a very devastating event to the mother and the family. Most stillbirths occur during labor and birth with other deaths occurring during the antenatal period. Millions of families experience stillbirths, yet these deaths remain uncounted, and policies have not been clearly stipulated to address this issue. The aim of the study was to identify the possible causes of stillbirths as recorded in the medical records.
Methods:
A retrospective study looking at medical records of women who experienced stillbirths between 1st January 2009 and 31st December 2013 at Nyeri Provincial General Hospital, Kenya. The hospital records containing cases of stillbirths were retrieved and data abstraction forms were used to collect data and information.
Results:
Both fresh and macerated stillbirths were equally common. The stillbirth rate was 12.2 per 1,000 births. There was significant association between stillbirths and the clients who were referred and reason for referral, (p=0.029) and (p=0.005), respectively. The number of ANC visits during pregnancy was also significant (p=0.05). Mode of delivery and the reason for cesarean section were significantly associated with stillbirths, (p=0.003) and (p=0.032), respectively. The type of labor and delivery complications experienced was associated with stillbirths (p= 0.022).
Conclusion and Global Health Implications:
There were several factors associated with stillbirths thus efforts should be made to establish approaches aimed at prevention. Addressing the causes of stillbirths will contribute to reduction of perinatal mortality.
Keywords
Stillbirths
Medical Records
Labor
Delivery
Referral
Nyeri
Kenya
Background
The International Classification of Diseases, 10th revision (ICD-10) defines a fetal death as death prior to the complete expulsion or extraction from its mother of a product of conception, irrespective of the duration of pregnancy; the death is indicated by the fact that after such separation, the fetus does not breathe or show any other evidence of life, such as beating of the heart, pulsation of the umbilical cord, or definite movement of voluntary muscles without specification of the duration of pregnancy.[1] Maternal and newborn conditions account for a substantial part of the health gap between the developed and developing countries.[2] In developed countries, the stillbirth rate is around 6 per 1, 000 births; it is about 26 per 1, 000, in less-developed countries; and it is about 31 per 1, 000 births in the least developed countries.[3] Stillbirth may be suspected when the mother ceases to feel fetal movement and the Obstetrician is unable to hear fetal heart tones.
Across the globe, around 3 million babies are stillborn every year—more than 8,200 babies a day.[4] Almost half of all stillbirths, or 1.2 million, happen when the woman is in labor. In Africa, a woman has a higher chance, about 24 times more of getting a stillbirth as compared to a woman in a higher income country.[5] According to the World Health Organization (WHO) statistics, the estimated rate of stillbirths in Kenya is 22 per 1000 births.[6] In Uganda, the stillbirth rate is 25 per 1000 births, Ethiopia is also 25 per 1000 while in Nigeria, it is estimated at 42 per 1000.[6] These deaths are directly related to the lack of skilled care at this critical time for mothers and babies.[7] In developing countries, a third of stillbirths are almost always or often blamed on the woman or on evil spirits.[8] Millions of families experience stillbirth, yet these deaths remain uncounted, unsupported, and the solutions understudied.[4] Stillbirths are believed to contribute to the overwhelming majority of perinatal mortality in some developing countries.[9] The major causes of stillbirths include childbirth complications, maternal infections in pregnancy, maternal disorders e.g. hypertension and diabetes, fetal growth restriction and congenital abnormalities.[10]
The vast majority of stillbirths are preventable, and simple interventions could lead to healthy infants as a rich reward for the resources invested.[11] Stillbirths were not included in the Millennium Development Goals tracking and remain invisible in global policies with only about 2% of all stillbirths being counted through vital registration and global estimates based on household surveys or modeling.[4,12] Stillbirths have not been as well studied despite the fact that more than 3 million stillbirths occur annually.[13] The need for better data is a pressing issue in stillbirth prevention, where there is a significant gap in translating knowledge into proven strategies to reduce fetal mortality.[14] Knowing the causes of stillbirth is essential when designing interventions.[4] The stillbirth rate is a reflection of health status and policies, socioeconomic indicators related to health and access and adequacy of health care.[15]
Central province in Kenya is reported to have the lowest infant mortality rates; however, there are still cases of stillbirths reported despite accessibility to health facilities and health care. This study, therefore, sought to establish the possible causes of stillbirths in Nyeri Provincial General Hospital (PGH), Kenya, through review of medical records.
Methods
This was a retrospective study seeking to review case medical records carried out at Nyeri Provincial General Hospital (PGH) currently referred as Nyeri County and Referral Hospital, Kenya. The research questions were: 1) what are the socio-demographic characteristics of women who experienced stillbirths; 2) what are the possible causes of stillbirths recorded; and finally, 3) which labor complications were associated with stillbirths? Medical records of postnatal women who had stillbirths between 1st January 2009 up to 31st December 2013 were retrieved. Data abstraction forms were used to collect data and information from the medical records. Data was collected on patients’ socio-demographic characteristics, recorded antenatal care services offered, maternal morbidities and stillbirths from the patient case notes. The outcome variable was the stillbirths versus the live births. Completed questionnaires were entered into Stata version 12.0 (College Station, TX). Data was analyzed using Stata version 12.0 and presented in forms of tables and figures. Descriptive statistics were done to describe the study population and percentages were reported. Bivariate analysis was done and the significance level was set at p < 0.05. Ethical review was obtained from Kenyatta University Ethical Review Committee (KUERC). A research permit was obtained from the National Council for Science, Technology and Innovation (NACOSTI) and from the hospital management team at Nyeri PGH. Care was taken to ensure that the medical records’ confidentiality was maintained throughout the study.
Results
The total number of deliveries that were recorded in the hospital during the study period were 22,919. A total of 280 maternal record files of women who had experienced both fresh and macerated stillbirths between 1st January 2009 to 31st December 2013 were retrieved. Thus, the stillbirth rate at the hospital was 12.2 per 1,000 births.
Socio-demographic data
Most of the women (80.3%) were aged between 20 – 34 years of age. Majority of them were multiparas (62.7%). On the level of education, most had primary (42.5%) and secondary school education (36.4%). Most of them were married (70.7%). On occupation, 45% of the women were unemployed and only 9.6% had a salaried job (Table 1). In logistic regression, there was no significance between the stillbirths and education level, marital status, occupation and existence of family illness (Table 2).
| Number | Percentage | |
|---|---|---|
| Age group (n=279) | ||
| 15-19 | 14 | 5.0 |
| 20-24 | 93 | 33.3 |
| 25-29 | 68 | 24.4 |
| 30-34 | 63 | 22.6 |
| 35-39 | 35 | 12.5 |
| 40-45 | 5 | 1.8 |
| 46-49 | 1 | 0.4 |
| Parity | ||
| Primigravida | 93 | 33.21 |
| Multipara | 176 | 62.86 |
| Grand multipara | 11 | 3.93 |
| Level of education | ||
| None | 3 | 1.07 |
| Primary | 119 | 42.50 |
| Secondary | 102 | 36.43 |
| Tertiary | 35 | 12.50 |
| Not indicated | 21 | 7.50 |
| Marital status | ||
| Married | 198 | 70.71 |
| Single | 73 | 26.07 |
| Divorced/separated | 2 | 0.71 |
| Not indicated | 7 | 2.50 |
| Occupation | ||
| Unemployed | 126 | 45.00 |
| Casual job | 25 | 8.93 |
| Self-employed | 81 | 28.93 |
| Salaried job | 27 | 9.64 |
| Not indicated | 21 | 7.50 |
| Odds ratio (OR) | z | P>z | [95% conf. interval] | |
|---|---|---|---|---|
| Age | 0.99 | −0.56 | 0.573 | 0.9483-1.029 |
| Education level | 1.10 | 0.78 | 0.433 | −0.1615-0.3773 |
| Marital status | 0.99 | 0.24 | 0.808 | −0.3452-0.4431 |
| Occupation | 0.89 | −1.12 | 0.261 | −0.2890-0.0784 |
| Family illness | 1.19 | 0.97 | 0.330 | −0.2252-0.6707 |
Antenatal care (ANC)
Majority of the women who had stillbirths had attended ANC and only 18% had not attended. On the place of ANC attendance, most of the women (68.2%) attended public facilities, 5.4% attended private facilities and others attended other facilities including TBAs. Missing data was 8.6%. Most of the women (76.8%) who had stillbirths did not have any complications during the pregnancy while 22.2% had complications which were pre-eclampsia (34.3%), diabetes mellitus (1.6%), hyperemesis gravidarum (15.6%) and other complications (48.4%). There was no significant association between having a stillbirth and ANC attendance or place that the client attended ANC, however, the number of ANC visits during pregnancy was significant, (p=0.05, 95% CI: -0.657 - 1.265) (Tabel 4).
Referral
The women who were referred were 58.2% while 41.8% were not referred from a health facility. Most of the women (92.1%) were admitted into the hospital before delivery while 7.9% were admitted after delivery. The women were referred from the health centers and dispensaries (22.9%), self- referral from home (22.9%), the private hospitals (4.3%) and other places/locations (7.9%). The commonest reason for referral was reduced or no fetal movement (29.5%) and other reasons (22.9%) (Table 3). On regression analysis, there was significant association between the clients who were referred and reason for referral, (p=0.029, 95% CI -1.789, - 0.10) and (p=0.005, 95% CI: 0.309 - -0.05) respectively.
| Variable | Frequency (n) | Percentage |
|---|---|---|
| Referral (n=280) | ||
| Yes | 163 | 58.21 |
| No | 117 | 41.79 |
| Reason for referral (n=163) | ||
| Fetal distress | 18 | 11.04 |
| Malpresentation | 16 | 9.81 |
| Reduced/no fetal movements | 48 | 29.45 |
| Prolonged labor | 12 | 7.36 |
| APH | 16 | 9.81 |
| PET | 14 | 8.59 |
| Others | 37 | 22.7 |
| Not indicated | 2 | 1.2 |
| Odds ratio (OR) | z | P>|z| | [95% conf. interval] | |
|---|---|---|---|---|
| Referral | −0.87 | −2.18 | 0.029 | −1.789-0.0947 |
| Place of referral | −0.06 | −0.46 | 0.648 | −0.2241-0.1394 |
| Reason for referral | −0.14 | −2.80 | 0.005 | −0.3087- −0.0542 |
| ANC attendance | 0.28 | 0.62 | 0.535 | −0.6572-1.265 |
| Visits | 0.16 | 1.92 | 0.023 | 0212-0.2931 |
| Place of ANC attended | −0.06 | −0.26 | 0.791 | −0.231-0.1762 |
| ANC complication | 1.54 | 0.52 | 0.024 | −0.417-0.7202 |
| Type of complication | 0.4 | 2.19 | 0.029 | 0.0422-0.7706 |
Delivery
Most of the women (92.5%) delivered in hospital: 1.8% in the health centers and dispensaries, 4.3% delivered at home, while 1.4% in other places. Gestation at birth was above 36 weeks gestation for 34.6% of the women and for 33.2% of the women gestation was between 33-36 weeks (Table 5). Most of the women (80.7%) had vaginal delivery and 19.3% had caesarean section (C/S). Cephalic presentation was common for both those that had vaginal delivery or C/S. Those that weighed below 2500 g were 56.4%, 29.6% weighing between 2500 – 3500 g and 11.1% weighed over 3500 g at birth. Those who were not weighed were 2.86%. The reasons for C/S included obstructed labor, fetal distress, malpresentation, maternal conditions, fetal abnormalities, and others. On regression analysis, there was significant association between the stillbirths and the reason for cesarean section and the mode of delivery, (p=0.032, 95% CI: 0.012 - 0.272) and (p=0.003, 95% CI: 0.163 - 0.817) respectively (Table 6). There was no association with the gestation at delivery or the presentation at birth. Birth weight was significantly associated with stillbirths, (p=0.037, 95% CI: 1.019 - 1.877). The labor and delivery complications experienced among the women were obstructed labor (6%), eclampsia (8%), fetal distress (21%), postpartum hemorrhage (PPH) (24%), retained placenta (9%) and other complications accounted for 32% (Figure 1). There was significant association between the stillbirths and the type of labor and delivery complications experienced, (p= 0.022, 95% CI: -0.384 - -0.03) (Table 3).
| Gestation at delivery (n=280) | Frequency | Percentage | ||
|---|---|---|---|---|
| Below 24 weeks | 8 | 2.86 | ||
| 24-28 weeks | 29 | 10.36 | ||
| 29-32 weeks | 52 | 18.57 | ||
| 33-36 weeks | 93 | 33.21 | ||
| Above 36 weeks | 97 | 34.64 | ||
| Not indicated | 1 | 0.36 | ||
| Mode of delivery (n=226) | ||||
| Presentation | Vaginal | Percentage | Cesarean section | Percentage |
|---|---|---|---|---|
| Cephalic | 175 | 77.43 | 31 | 57.41 |
| Breech | 47 | 20.79 | 20 | 30.04 |
| Others | 4 | 1.76 | 3 | 5.56 |
| Below 2500 g | 144 | 63.71 | 14 | 25.92 |
| 2500 g-3500 g | 54 | 23.89 | 29 | 53.7 |
| Above 3500 g | 21 | 9.29 | 10 | 18.51 |
| Not weighed | 7 | 3.1 | 1 | 1.85 |
| Variable | Odds ratio (OR) | z | P>|z| | [95% conf. interval] |
|---|---|---|---|---|
| Reason for cesarean section | 0.76 | 2.14 | 0.032 | 0.0118-0.2717 |
| Place of delivery | 0.23 | 1.04 | 0.299 | −0.2078-0.6759 |
| Gestation | 1.02 | 0.48 | 0.632 | −0.1690-0.2786 |
| Presentation | 1.4 | 1.57 | 0.117 | −0.1008-0.9018 |
| Delivery mode | 3.03 | 2.93 | 0.003 | 0.1625-0.8168 |
| Labor complication | 0.23 | −2.29 | 0.022 | −0.3836- −0.0298 |
| Birth weight | 1.38 | 2.09 | 0.037 | 1.019-1.877 |
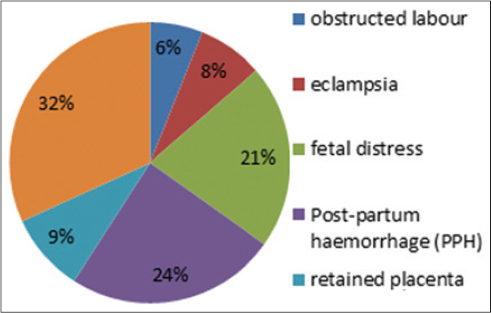
- Labor and Delivery Complications
Type of stillbirth
Fresh and macerated stillbirths were equally common, 50.5% and 49.5%. Most of the stillbirths (83.6%) did not have any congenital abnormality (Table 7). The presence or the type of congenital abnormality was not significantly associated with stillbirths (Table 8).
| Variable | Frequency | Percentage |
|---|---|---|
| Type of still birth (n=280) | ||
| Macerated Stillbirth (MSB) | 141 | 50.36 |
| Fresh Stillbirth (FSB) | 138 | 49.29 |
| Twins with FSB and MSB | 1 | 0.36 |
| Congenital abnormality (n=280) | ||
| Yes | 46 | 16.43 |
| No | 234 | 83.57 |
| Type of abnormality (n=43) | ||
| Hydrocephalus | 5 | 11.6 |
| Anencephaly | 9 | 20.9 |
| Abdominal abnormalities | 3 | 7 |
| Others | 22 | 51.2 |
| Multiple abnormalities | 4 | 9.3 |
| Odds ratio | z | P>|z| | [95% conf. interval] | |
|---|---|---|---|---|
| Congenital abnormality | 0.64 | −0.73 | 0.468 | 0.18872.1503 |
| Type of abnormality | 1.04 | 0.28 | 0.776 | 0.79031.3706 |
Limitation: This was a retrospective study and some information in the files were missing and thus was a limitation for this study.
Discussion
From the study findings, there were factors associated with stillbirths which have policy and practice implications for maternal and child health in the region and the country.
Demographic factors
Most of the women who had stillbirths were aged between 25-34 years old. This is the peak of the women’s reproductive age. The majority of women experiencing stillbirths in this age could be attributed to the fact that most births are occurring during this period. The findings are similar to those from a study in China which found out that most stillbirths occurred between 21-35 years of age.[16] A Nigerian study concluded that teenage pregnancy had more adverse outcomes compared to other age groups.[17] Most of the women were multiparas, having had between 1-4 pregnancies. Nyeri has a low fertility rate according to the Kenya Demographic and Health Survey (KDHS) statistics.[18] Majority of the women who had stillbirths had primary level and secondary level of education. This could be attributed to the proximity and accessibility of schools which could increase the level of education in the County. This could also be attributed to economic empowerment in the region.
Antenatal care
Majority of the women attended ANC, mostly in the public health facilities. This could be attributed to the accessibility of the public health facilities and the cost of treatment as compared to private institutions where the cost can be higher. However, the number of visits attended was not indicated in most of the in-patient’s records. The number of ANC visits attended was significantly associated with stillbirths (p=0.051). Focused ANC aims at comprehensive care during each visit. A woman who attends fewer visits may not benefit from all services that were provided and this may lead to failure to detect complications that may arise during pregnancy. Similar observations were made from a retrospective hospital study in India.[19] Most of the women never had complications during pregnancy. The common complications experienced pre-eclampsia, gestational diabetes and other complications such as hemorrhage. Complications during pregnancy have been associated with stillbirths. The findings support findings from a hospital based retrospective study carried out at Pravara rural hospital in India which indicated that pregnancy-induced hypertension was the commonest cause of stillbirths. [19]
Referral
Among the women who experienced stillbirths, 58.2% of them were referred from another health facility; however, 41.8% were self-referrals from home. This may be attributed to knowledge of danger signs during pregnancy, labor and delivery. Significant association was found between referral and the reason for referral, p=0.03 and p=0.01 respectively. Some complications which may arise during pregnancy, labor and delivery such as fetal distress, reduced fetal movements or malpresentations indicate a compromise in the fetal life in utero. This increases the risk of stillbirths especially if the woman is unable to access care immediately. A study in Nigeria found that late referral was a contributor to delivery of stillbirths.[20]
Delivery
Most of the women delivered in hospital above 36 weeks gestation and others between 33-36 weeks. A study assessing the risk of stillbirths and gestational age had similar findings indicating that the risk of stillbirths increased with gestational age.[21] However, the findings of this study differed with findings from a review of stillbirths and early neonatal deaths in six developing countries, namely, Argentina, Egypt, India, Peru, South Africa and Vietnam which found that prematurity was the commonest cause.[14] Vaginal delivery was the commonest mode of delivery. For those that had cesarean section (C/S), the reasons for C/S included obstructed labor, fetal distress, and others. The reason for C/S and the baby’s birth weight were significantly associated with stillbirths. A study in Ghana found that the highest risk for stillbirths was during labor and delivery.[22] Both fresh and macerated stillbirths were commonly experienced unlike a study in Nigeria which found that macerated stillbirths were common. [20] Most of them did not have a congenital abnormality.
Conclusion and Global Health Implications
Stillbirths are caused by multiple factors ranging from antenatal, referral and delivery factors. More efforts should be focused on minimizing stillbirths by designing preventive strategies at antenatal care and delivery. The health facility staff from peripheral facilities should be empowered on how to handle complications in order to minimize stillbirths arising from referrals.
Acknowledgement:
We acknowledge the management of Nyeri PGH for allowing this study to be carried out in the facility. Specifically, we appreciate Matron Waikwa for her entire support during the study. Special mention goes to Wambui for her immense support in retrieving files in the maternity records office. Special thanks goes to Godwin Rutto and Henry Rotich for assisting during the data collection process. We acknowledge Dedan Kimathi University of Technology (DeKUT) for the financial support that saw the success of this study. We wish to thank everybody who in one way or the other contributed to the success of this study.
Conflict of Interest: The authors declare no conflict of interest.
References
- International Classification of Diseases and Related Health Problems Vol 2. (10th Revision). Geneva: World Health Organization; 1993.
- National Roadmap for accelerating the attainment of MDGs related to maternal and newborn health in Kenya, Ministry of Health, Central Bureau of Statistics, Macro International. 2010.
- WHO Neonatal and Perinatal Mortality – Country, Regional and Global Estimates. 2006.
- Stillbirths: Where? When? Why? How to make the data count? Lancet. 2011;23(377)(9775):1448-63.
- [Google Scholar]
- Partnership for Maternal Child health (PMNCH) fact sheet: Stillbirths. http://www.who.int/pmnch/media/press_materials/fs/201106_stillbirths/en
- 2009. WHO Country stillbirth rates per 1000 total births for. http://www.who.int/pmnch/media/news/2011/stillbirths_countryrates.pdf
- 2009. WHO National, regional, and world wide estimates of stillbirth rates in 2009 with trends since 1995, policy brief WHO/RHR/11.03. http://www.who.int/reproductivehealth/topics/maternal_perinatal/stillbirth/who_rhr_11-3.pdf?ua=1
- Ethiopian Journal of Reproductive Health. 2008;2(1)
- WHO Stillbirths. at http://www.who.int/maternal_child_adolescent/epidemiology/stillbirth/en
- BMC Pregnancy Childbirth. 2009;9(6)
- the GAPPS Review Group, Global report on preterm birth and stillbirth (1 of 7): definitions, description of the burden and opportunities to improve data. BMC Pregnancy and Childbirth 2010(1):S1.
- [Google Scholar]
- Preventing those so-called stillbirths, Bulletin of the World Health. Organization. 2008;86(4):241-320.
- [Google Scholar]
- Causes of stillbirths and early neonatal deaths: data from 7993 pregnancies in six developing countries. Bulletin of the World Health Organization. 2006;84:699-705.
- [Google Scholar]
- Evaluation of clinicosocial factor associated with antepartum and intrapartum stillbirth in Kathmandu medical college teaching hospital Journal of South Asian Federation of Obstetrics and Gynecology, January-April. 2009;1(1):14-18.
- Poor knowledge on causes and prevention of stillbirths among health care providers: An implication for regular in-service training in developing countries. Journal of Chinese Clinical Medicine. 2010;51:221-225.
- [Google Scholar]
- Socio-demographic determinants of teenage pregnancy in the Niger Delta of Nigeria. Open Journal of Obstetrics and Gynecology. 2012;2:239-243.
- [Google Scholar]
- Kenya National Bureau of Statistics (KNBS) and ICF Macro. Calverton, Maryland: KNBS and ICF Macro. Nairobi, Kenya; 2010.
- A review of socio demographic factors and obstetric causes of stillbirths at Tertiary care hospital. IOSR Journal of Pharmacy. 2012;2(3):475-478.
- [Google Scholar]
- Risk of Stillbirth and Infant Death Stratified by Gestational Age. Obstetrics and Gynecology. 2012;120(1):76-82.
- [Google Scholar]
- Aetiology of stillbirths and neonatal deaths in rural Ghana: implications for health programming in developing countries. Paediatric Perinatal Epidemiology. 2008;22(5):430-7.
- [Google Scholar]
- Stillbirth Rate in a Teaching Hospital in SouthEastern Nigeria: A Silent Tragedy. Annals of Medical and Health Sciences Research. 2012;2(2)
- [Google Scholar]





