Translate this page into:
HIV Testing, Household and Reproductive Health Decision-Making: The Role of Women Autonomy in a Nationally Representative Study in Cambodia

*Corresponding author: Wah Wah Myint, Center for Community Health and Aging, School of Public Health, Texas A&M University, 212 Adriance Lab Rd, College Station, TX, USA wah@tamu.edu
-
Received: ,
Accepted: ,
How to cite this article: Myint WW, Yusuf A, Nguyen A, Samman E. HIV testing, household and reproductive health decision-making: The role of women autonomy in a nationally representative study in Cambodia. Int J MCH AIDS. 2025;14:e001. doi: 10.25259/IJMA_36_2024
Abstract
Background and Objective
Women’s autonomy plays a critical role in decision-making of health service use. This study aims to evaluate the relationship between Human Immunodeficiency Virus (HIV) testing and decision-making autonomy among Cambodian women aged 15–49.
Methods
We used data from the 2021–2022 Cambodia Demographic and Health Survey (DHS) and our sample consisted of currently married/cohabiting women aged 15–49 (N = 13,755). The outcome variable was “ever been tested for HIV.” Covariates were household decision-making and reproductive health decision-making scores, socio-demographic characteristics (age, place of residency, education, wealth quintiles, and employment status), and HIV knowledge (HIV self-test kits, drugs to prevent HIV in babies during pregnancy, antiretroviral [ARV] drugs, and pre-exposure prophylaxis).
Results
Sixty-one percent of studied women reported ever being tested for HIV. The logistic regression results revealed that women with a higher household decision-making score (aOR = 2.09, p < 0.001), reproductive health decision-making score (aOR = 1.72, p < 0.001), from 25 to 29 age groups (aOR = 2.21, p < 0.001), with a higher education (aOR = 1.96, p = 0.001), from the richest groups (aOR = 1.73, p < 0.001), had knowledge of HIV test kits but never get tested (aOR = 1.38, p = 0.035), heard of drugs to avoid HIV transmission to babies during pregnancy (aOR = 1.21, p < 0.001), and heard of ARV drugs (aOR = 1.28, p < 0.001) were more likely to get tested for HIV than their counterparts. Women living in rural areas (aOR = 0.56, p < 0.001) and those who had discriminatory attitudes (aOR = 0.76, p = < 0.001) were less likely to get HIV tests than those in urban areas and those without discrimination.
Conclusion and Global Health Implications
Findings revealed that greater autonomy is important for health care use, particularly HIV testing for women in Cambodia.
Keywords
Cambodia
Decision-Making
HIV Testing
Personal Autonomy
Women’s Health
INTRODUCTION
Background of the Study
Human Immunodeficiency Virus (HIV)/Acquired Immuno-Deficiency Syndrome (AIDS) remains a global public health challenge. About 40 million people are living with HIV/AIDS (PLWHA) in 2023, of which 1.3 million are newly acquired cases.[1] Women and girls accounted for 73% (29 million) of the PLHIV and 44% (572,000) of all new HIV infections. [1] In response to the alarmingly high rates of HIV infections worldwide, the Joint United Nations Programme on HIV/AIDS (UNAIDS) set three 95 targets to end the AIDS epidemic by 2030. The three 95 targets aim to diagnose 95% of all HIV-positive individuals, provide antiretroviral (ARV) therapy for 95% of those diagnosed, and achieve viral suppression for 95% of those treated by 2030.[2] Among the world regions, Southeast Asia (SEA) is home to the second largest burden of HIV, with 6.5 million PLWHA and 300,000 new cases in 2022. [1] Among SEA countries, Cambodia is one of the many countries that has a considerable HIV prevalence and has many challenges despite tremendous efforts to meet the three 95 targets.
In 2022, an estimated 74,000 adults aged 15 and older in Cambodia were PLHIV, of which about 50% (36,000) were women.[1] Almost 500 new cases were seen among Cambodian women.[1] Many of these women contracted HIV from their spouses, who enjoyed condomless extramarital sexual intercourse with their wives.[3] Given that the majority of these women are of reproductive age, they could be the main drivers of pediatric HIV.[3] Therefore, early HIV testing is urgently needed as it is the gateway to early diagnosis and treatment, which leads to achieving undetectable and un-transmittable (U=U) viral loads.[4,5] Currently, 86% of PLHIV in Cambodia are aware of their HIV status.[6] However, in 2022, Cambodia’s National Demographic and Health Survey (DHS) reported that more than half (53%) of Cambodian women surveyed have never been tested for HIV.[7] It has been suggested that one of the reasons for not getting a test could be limited or lack of decision-making authority autonomy of the women.[8]
Women’s autonomy includes access to and control over resources, participation in household-level economic decisions, mobility, freedom from domestic violence, and freedom to act independently.[9] Although some studies in Sub-Saharan African countries[10,11,12] and Nepal[13] have evaluated the relationship between HIV testing and women’s autonomy, there is no literature on HIV testing and decision-making autonomy specific to Cambodia. Most of the available studies in SEA evaluated the influence of women’s household decision-making autonomy over maternal health and other reproductive outcomes; for example, some studies explored the relationship between women’s household decision-making autonomy and service utilization in Bangladesh,[14,15] Nepal,[16] Indonesia,[17] safer sex negotiation in Cambodia,[18] and use of contraception among Cambodian women.[19]
Objectives of the Study
This study aims to evaluate the relationship between HIV testing and Cambodian women’s household decision-making autonomy and reproductive health decision-making autonomy. The specific aims are as follows:
Specific aims
To describe the socio-demographic characteristics of married/cohabiting women in Cambodia.
To evaluate the influence of household and reproductive health decision-making on HIV testing among married/cohabiting women in Cambodia.
To assess the relationship between HIV-related knowledge, including self-test kits and ARVs and HIV testing among married/cohabiting women in Cambodia.
METHODS
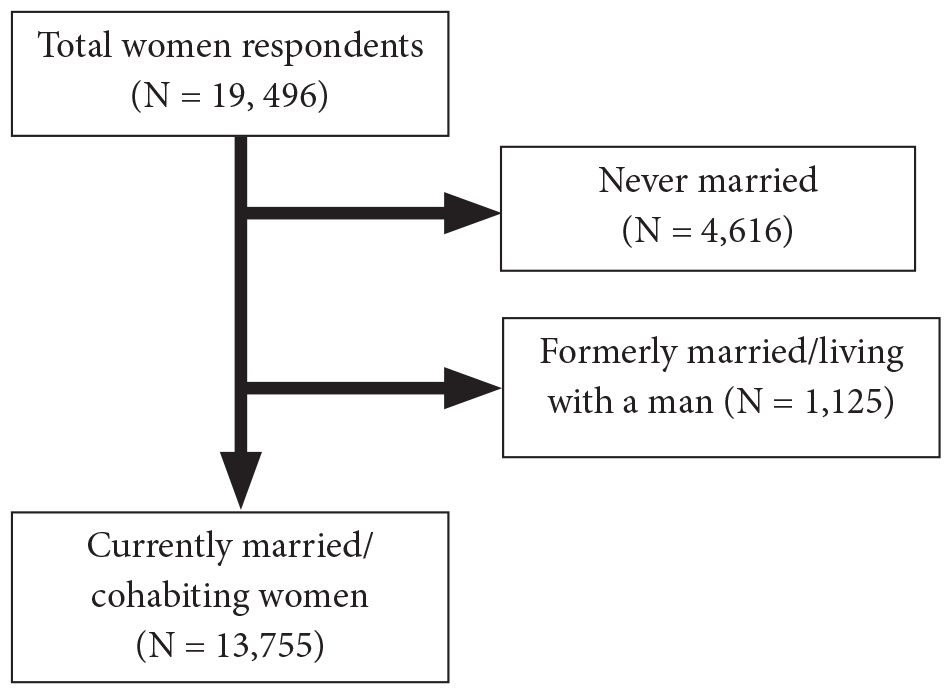
This study used the women’s data (Total N = 19,496) of Cambodia’s DHS (2021–2022). The main eligibility criteria were currently married/cohabiting, non-pregnant women. Of the total women survey, we excluded never married (N = 4,616) and formerly married (N = 1,125) women, leaving our final sample of currently married/cohabiting non-pregnant women to be 13,755 [Figure 1].[7] Cambodia’s DHS used a two-stage stratified random sampling methodology: the first stage being at the cluster level and the second stage at the household level.[7] Cambodia’s DHS received ethical approval from the Institutional Review Board (IRB) of Inner-City Fund (ICF) International.[20] This study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STOBE) guidelines for observational cross-sectional studies.
Study Variables
Outcome variable
The outcome variable was if the respondent has “ever been tested for HIV.” It is a dichotomous variable (No = 0, Yes = 1).
Covariates
Socio-demographic variables
The socio-demographic variables included age groups (15–18, 19–24, 25–29, 30–34, 35–39, 40–44, 45–49), place of residency (urban/rural), education level (no education, primary, secondary, and higher), wealth index (poorest, poorer, middle, richer, and richest), and employment status (no employment, worked in the last 12 months, currently working, have a job but on leave for the last 7 days). The wealth index is a composite measure that is calculated based on selected consumable households’ assets (e.g., electricity, television, radio, bicycles, housing construction materials, including roofing and flooring, drinking water, and sanitation facilities).[21]
HIV-related knowledge variables
This study used the screening question, “Have you heard about HIV or AIDS (No = 0, Yes = 1)". If the respondents reported yes, then the following HIV-related knowledge questions were asked: (a) knowledge about drugs to avoid HIV transmission to babies during pregnancy (No = 0, Yes = 1), (b) knowledge of and attitude towards pre-exposure prophylaxis (PrEP) for HIV prevention (haven’t heard, heard and approved to take it every day, heard but do not approve to take it every day, heard but not sure about approving it), (c) knowledge and use of HIV self-test kits (i.e., never heard, have tested, knows self-test kit but never got tested), and (d) heard of ARV drugs to treat HIV (No = 0, Yes = 1). We also included the discriminatory attitude of the respondents, which was created from two scenarios: (a) would buy vegetables from a vendor with HIV and (b) children with HIV should be allowed to attend school with children without HIV. These two scenarios are in line with the UNAIDS Global AIDS Monitoring (GAM) indicator 6.1 on discriminatory attitudes.[22] If a respondent answered no/don’t know/not sure/depends on either of the questions, it was recoded as zero. If the respondent answered yes to both questions, it was recoded as one.
Women’s decision-making variables
The women’s decision-making variables were (a) respondents’ household decision-making authority and (b) respondents’ reproductive health decision-making authorities.[23] The household decision-making authority was created based on three scenarios: decision-making on (a) own health care, (b) large household purchases, and (c) visits to family or relatives. The original responses were decision-making (a) alone, (b) joint (herself and her partner), (c) by partner only, and (d) by others. We assigned a score of one to those who responded that the decision was made (a) alone or (b) joint and assigned zero for other responses. Similarly, the women’s reproductive health decision-making score was created based on two scenarios: whether the respondent has a say (a) to refuse sex and (b) to use a condom. We assigned one to those who reported yes to either one of these scenarios and zero to those who reported no to both scenarios.
Statistical Analysis
We performed descriptive statistics to describe the frequency and percentage included variables. We applied Pearson’s Chi-squared (X2) test of independence to observe the relationship between the outcome variable and covariates. We also assessed the correlation of two decision-making score variables to observe the strength and the direction between them by using Pearson’s correlation test. To predict the relationship between HIV testing and women’s autonomy, we conducted multivariable logistic regressions controlling other covariates that showed a significant relationship with the outcome variable (i.e., p-value < 0.05 in the bivariate analysis). We reported adjusted odds ratios (aOR) and 95% confidence intervals (CI) and applied a significant level of p-value < 0.05. Missing data were not included in the analyses. We also checked multicollinearity among independent variables using the “collin” command. All the analyses applied survey weights and used “svy” and “svyset” commands by using Stata 18.0.[24]
The ICF’s IRB approved the original study.[25]
RESULTS
Prevalence of Included Variables
Table 1 presents the prevalence of included variables. A higher percentage of HIV testing was observed in the women aged 35–39 group (22%), rural residents (56%), with primary education (45%), from the richest wealth quintile groups (22%), and with current employment (67%) compared to those who were aged 18–24, urban residents, from the lowest wealth quintile groups, and those who were not currently employed. About 88% reported having household decision-making autonomy in all scenarios, and 78% reported having decision-making autonomy on reproductive health-related issues. More than half (63%) reported ever being tested for HIV. Almost all (97%) had heard about HIV or AIDS. Of them, almost all (95%) had never heard about HIV self-test kits, 66% had heard about drugs to avoid HIV transmission to babies during pregnancy, and 70% had heard about ARV drugs to treat HIV. However, about 79% have never heard about PrEP, and about 26% of the studied women had a discriminatory attitude towards PLHIV.
| Socio-demographic characteristics (N = 13,755) | N | % |
| Age groups | ||
| 15–19 | 409 | 2.48 |
| 20–24 | 1,563 | 10.26 |
| 25–29 | 2,499 | 17.53 |
| 30–34 | 2,814 | 21.05 |
| 35–39 | 2,843 | 21.51 |
| 40–44 | 2,243 | 16.76 |
| 45–49 | 1,384 | 10.41 |
| Place of residency | ||
| Urban | 4,678 | 40.05 |
| Rural | 9,077 | 59.95 |
| Education level | ||
| No education | 2,345 | 14.03 |
| Primary | 6,314 | 45.06 |
| Secondary | 4,529 | 35.73 |
| Higher | 567 | 5.18 |
| Household wealth quintile | ||
| Poorest | 3,723 | 18.76 |
| Poorer | 2,459 | 18.09 |
| Middle | 2,636 | 19.67 |
| Richer | 2,750 | 21.65 |
| Richest | 2,187 | 21.82 |
| Employment status | ||
| No employment | 2,996 | 21.34 |
| In the past year | 1,418 | 9.8 |
| Currently working | 9,082 | 67.02 |
| Have a job but on leave last 7 days | 259 | 1.83 |
| Household decision-making score | ||
| Score 0 | 659 | 4.51 |
| Score 1 | 342 | 2 |
| Score 2 | 901 | 5.74 |
| Score 3 | 11,853 | 87.76 |
| Decision-making score on reproductive health | ||
| Score 0 | 979 | 6.37 |
| Score 1 | 2,337 | 15.84 |
| Score 2 | 10,439 | 77.79 |
| Respondents had heard about HIV or AIDS | ||
| No | 533 | 2.95 |
| Yes | 13,222 | 97.05 |
| Ever been tested for HIV if heard about HIV or AIDS | ||
| No | 5,386 | 37.03 |
| Yes | 7,836 | 62.97 |
| HIV-related variables (N = 13,222) | ||
| Knowledge and use of HIV self-test kits | ||
| Never heard of HIV self-test kits | 12,647 | 95.19 |
| Have tested | 56 | 0.5 |
| Knows test kit but never get tested | 519 | 4.31 |
| Heard of drugs to avoid HIV transmission to babies during pregnancy | ||
| No | 5,070 | 34.39 |
| Yes | 8,152 | 65.61 |
| Heard of antiretroviral (ARV) drugs to treat HIV | ||
| No | 4,613 | 29.75 |
| Yes | 8,609 | 70.25 |
| Knowledge and attitude to pre-exposure prophylaxis (PrEP) to prevent getting HIV | ||
| Haven’t heard about PrEP | 10,872 | 79.13 |
| Heard and approved to take it every day | 2,014 | 18.44 |
| Heard but do not approve of taking it every day | 257 | 1.85 |
| Heard but not sure about approving it | 79 | 0.59 |
| Discriminatory attitude | ||
| No discrimination | 9,217 | 73.97 |
| Discrimination exists | 4,005 | 26.03 |
Note: HIV-related knowledge and discriminatory attitude questions are asked only if the respondents reported they heard about HIV or AIDS (N = 13,222).
Results from Bivariate Analyses
The results from Pearson’s X2 bivariate analyses [Table 2] demonstrated a significant relationship between HIV testing and socio-demographic variables (age groups, place of residency, education level, household wealth quintile, and employment status) and decision-making scores (household decision-making score and reproductive health decision-making scores) (all p < 0.001). Moreover, the results revealed a significant relationship between HIV testing and HIV knowledge variables: knowledge and use of HIV self-test kits (p = 0.001), heard of drugs to prevent HIV transmission to babies during pregnancy (p < 0.001), and had heard about ARV (p < 0.001), knowledge and attitude towards PrEP to prevent HIV prevention (p = 0.002), and discriminatory attitude (p < 0.001). The results from Pearson’s correlation test also revealed that the household decision-making score and the reproductive decision-making score are positively correlated (correlation coefficient [r] = 0.76, p < 0.001).
| No = 5,919 | Yes = 7,836 | N = 13,755 | |||
| N (%) | N (%) | N (%) | X2 | p-value | |
| Age groups | |||||
| 15–19 | 213 (3.08) | 196 (2.11) | 409 (2.48) | 1198.86 | <0.001 |
| 20–24 | 562 (8.91) | 1,001 (11.12) | 1,563 (10.26) | ||
| 25–29 | 712 (11.21) | 1,787 (21.55) | 2,499 (17.53) | ||
| 30–34 | 887 (14.87) | 1,927 (24.98) | 2,814 (21.05) | ||
| 35–39 | 1,201 (20.11) | 1,642 (22.4) | 2,843 (21.51) | ||
| 40–44 | 1,306 (22.94) | 937 (12.83) | 2,243 (16.76) | ||
| 45–49 | 1,038 (18.89) | 346 (5.01) | 1,384 (10.41) | ||
| Place of residency | |||||
| Urban | 1,439 (27.53) | 3,239 (48.02) | 4,678 (40.05) | 571.74 | <0.001 |
| Rural | 4,480 (72.47) | 4,597 (51.98) | 9,077 (59.95) | ||
| Education level | |||||
| No education | 1,544 (21.31) | 801 (9.4) | 2,345 (14.03) | 815.94 | <0.001 |
| Primary | 2,921 (51.05) | 3,393 (41.25) | 6,314 (45.06) | ||
| Secondary | 1,360 (25.55) | 3,169 (42.21) | 4,529 (35.73) | ||
| Higher | 94 (2.09) | 473 (7.14) | 567 (5.18) | ||
| Household wealth quintile | |||||
| Poorest | 2,094 (25.08) | 1,629 (14.74) | 3,723 (18.76) | 644.76 | <0.001 |
| Poorer | 1,136 (21.42) | 1,323 (15.97) | 2,459 (18.09) | ||
| Middle | 1,148 (22.09) | 1,488 (18.14) | 2,636 (19.67) | ||
| Richer | 978 (18.89) | 1,772 (23.4) | 2,750 (21.65) | ||
| Richest | 563 (12.51) | 1,624 (27.75) | 2,187 (21.82) | ||
| Employment status | |||||
| No employment | 1,269 (22.67) | 1,727 (20.5) | 2,996 (21.34) | 29.06 | <0.001 |
| In the past year | 633 (10.26) | 785 (9.51) | 1418 (9.8) | ||
| Currently working | 3,942 (65.86) | 5,140 (67.77) | 9,082 (67.02) | ||
| Have a job but on leave last 7 days | 75 (1.21) | 184 (2.22) | 259 (1.83) | ||
| Household decision-making score | |||||
| Score 0 | 335 (6.16) | 324 (3.46) | 659 (4.51) | 66.34 | <0.001 |
| Score 1 | 148 (2.15) | 194 (1.9) | 342 (2) | ||
| Score 2 | 413 (4.86) | 488 (6.29) | 901 (5.74) | ||
| Score 3 | 5,023 (86.83) | 6,830 (88.35) | 11,853 (87.76) | ||
| Decision-making score on reproductive health issues | |||||
| Score 0 | 643 (9.84) | 336 (4.17) | 979 (6.37) | 214.93 | <0.001 |
| Score 1 | 1,124 (17.66) | 1,213 (14.68) | 2,337 (15.84) | ||
| Score 2 | 4,152 (72.5) | 6,287 (81.15) | 10,439 (77.79) | ||
| HIV related variables | N = 5,386 | N = 7,836 | N = 13,222 | ||
| Knowledge and use of HIV self-test kits | |||||
| Never heard of HIV self-test kits | 5,229 (35.93) | 7,418 (59.26) | 12,647 (95.19) | 57.89 | <0.001 |
| Have tested | 14 (0.1) | 42 (0.39) | 56 (0.5) | ||
| Knows test kit but never get tested | 143 (1) | 376 (3.32) | 519 (4.31) | ||
| Heard of drugs to avoid HIV transmission to babies during pregnancy | |||||
| No | 2499 (14.82) | 2,571 (19.56) | 5,070 (24.67) | 109.86 | <0.001 |
| Yes | 2,887 (22.21) | 5,265 (43.41) | 8,152 (65.61) | ||
| Heard of antiretroviral(ARV) drugs to treat HIV | |||||
| No | 2,249 (13.06) | 2,364 (16.69) | 4,613 (29.75) | 112.82 | <0.001 |
| Yes | 3,137 (23.97) | 5,472 (46.28) | 8,609 (70.25) | ||
| Knowledge and attitude to pre-exposure prophylaxis (PrEP) to prevent getting HIV | |||||
| Haven’t heard about PrEP | 4,522 (29.94) | 6,350 (49.19) | 10,872 (79.13) | 26.26 | 0.002 |
| Heard and approved to take it every day | 712 (6.06) | 1,302 (12.38) | 2,014 (18.44) | ||
| Heard but do not approve of taking it every day | 114 (0.76) | 143 (1.09) | 257 (1.85) | ||
| Heard but not sure about approving it | 38 (0.28) | 41 (0.31) | 79 (0.59) | ||
| Discriminatory attitude | |||||
| No discrimination | 3,275 (66.43) | 5,942 (78.41) | 9,217 (73.97) | 229.67 | <0.001 |
| Discrimination exists | 2,111 (33.57) | 1,894 (21.59) | 4,005 (26.03) |
Note: HIV-related knowledge and discriminatory attitude questions are asked only if the respondents reported they heard about HIV or AIDS (N = 13,222).
Multivariable Logistic Regression Results
Socio-demographic characteristics
The results from the multivariable logistics regressions are presented in Table 3. The findings revealed that women aged 25–29 were more than twice as likely to get an HIV test (aOR = 2.21, 95% CI = 1.59, 3.07) than those who were aged 15–18. Additionally, women in rural Cambodia were less likely to get tested for HIV than those in urban areas (aOR = 0.59, 95% CI = 0.48–0.64).
| Outcome: Ever been tested for HIV (N = 13,222) | aOR (95% CI) |
| Household decision-making (self or joint with the respondent partner) | |
| Score 0 = No decision-making at all | Ref |
| Score 1 | 1.88 (1.37, 2.59)*** |
| Score 2 | 2.09 (1.51, 2.92)*** |
| Score 3 | 1.74 (1.37, 2.21)*** |
| Reproductive health decision-making | |
| Score 0 = No decision-making at all | Ref |
| Score 1 | 1.72 (1.36, 2.18)*** |
| Score 2 | 1.72 (1.39, 2.13)*** |
| Age groups | |
| 15–19 | Ref |
| 20–24 | 1.76 (1.27, 2.46)*** |
| 25–29 | 2.21 (1.59, 3.07)*** |
| 30–34 | 1.91 (1.38, 2.64)*** |
| 35–39 | 1.34 (0.98, 1.85) |
| 40–44 | 0.69 (0.49, 0.95)* |
| 45–49 | 0.32 (0.22, 0.45)*** |
| Place of residency | |
| Urban | Ref |
| Rural | 0.56 (0.48, 0.64)*** |
| Education level | |
| No education | Ref |
| Primary | 1.31 (1.14, 1.53)*** |
| Secondary | 1.74 (1.49, 2.05)*** |
| Higher | 1.96 (1.35, 2.69)*** |
| Household wealth quintiles | |
| Poorest | Ref |
| Poorer | 1.07 (0.92, 1.25) |
| Middle | 1.05 (0.89, 1.25) |
| Richer | 1.23 (1.03, 1.47)* |
| Richest | 1.73 (1.37, 2.19)*** |
| Employment status | |
| No | Ref |
| Yes, in the past year | 1.02 (0.86, 1.22) |
| Currently working | 0.86 (0.76, 0.98)* |
| Have a job, but on leave last 7 days | 1.63 (1.103, 2.41)* |
| Knowledge and use of HIV self-test kits | |
| Never heard of HIV test kits | Ref |
| Has tested with HIV test kits | 1.48 (0.56, 3.87) |
| Knows test kits but never tested with them | 1.38 (1.02, 1.85)* |
| Heard of drugs to avoid HIV transmission to babies during pregnancy | |
| No | Ref |
| Yes | 1.21 (1.08, 1.37)*** |
| Heard of ARVs to treat HIV | |
| No | Ref |
| Yes | 1.28 (1.14, 1.44)*** |
| Knowledge and attitude to pre-exposure prophylaxis (PrEP) to prevent HIV | |
| Haven’t heard about it | Ref |
| Heard and approved to take it every day | 1.03 (0.86, 1.23) |
| Heard, but don’t approve of taking it every day | 1.03 (0.76, 1.403) |
| Heard, but not sure about approving its use | 0.87 (0.55, 1.36) |
| Discriminatory attitude | |
| No discrimination | Ref |
| Discriminatory attitude exists | 0.76 (0.67, 0.85)*** |
| _cons | 0.358 (0.22, 0.58)*** |
Note: *denotes p-value < 0.05;
***denotes p-value < 0.001. CI: Confidence interval, aOR: Adjusted odds ratio.
Some of the education and wealth quintiles also illustrated a significant relationship. The results revealed that the women with higher education were more likely to get HIV tests (aOR = 1.96, 95% CI = 1.35, 2.69) compared to those without formal education. Similarly, significant positive relationships between HIV test and the women from the two wealth quintile groups were observed: women from the richer (aOR = 1.42, 95% CI = 1.08, 1.86) and the richest groups (aOR = 2.24, 95% CI = 1.54, 3.26). Interestingly, the women in current employment were less likely to get tested for HIV (aOR = 0.86, 95% CI = 0.76, 0.98) than those who were unemployed.
Main variable (dependent or outcome) results
Women’s decision-making score ranges from zero to three. Women who reported at least one household decision-making score (aOR = 1.88, 95% CI = 1.371, 2.59) and reproductive health decision-making score (aOR = 1.76, 95% CI = 1.36, 2.18) were more likely to get tested for HIV compared to those without.
HIV-related variable(s) (covariates) results
Women having knowledge of HIV self-test kits but never being tested for HIV (aOR = 1.38, 95% CI = 1.02, 1.85), those who heard about the drugs to avoid HIV transmission to babies during pregnancy (aOR = 1.21, 95% CI = 1.08, 1.37), and those who heard about ARVs (aOR = 1.28, 95% CI = 1.14, 1.44) were more likely to get tested for HIV than those who did not have such knowledge. Conversely, women who had a discriminatory attitude towards people with HIV/AIDS were less likely to get tested for HIV than those who did not (aOR = 0.76, 95% CI = 0.67, 0.85).
Multicollinearity Results
The results from multicollinearity analysis among covariates showed that the multicollinearity in this model may not be an issue (conditional number without intercept = 3.245).
DISCUSSION
The present study aimed to evaluate the relationship between HIV testing and decision-making autonomy among married/cohabiting Cambodian women. As consistent with the findings from a previous study, this study found that Cambodian women with any household decision-making autonomy were more likely to get tested for HIV than their counterparts, highlighting that women’s decision-making plays an important role in health service utilization.[10]
Our findings on the significant relationship between HIV testing and those who had reproductive health decision-making is a novel finding. Although a study in Cambodia by Ung et al. (2014) reported that refusal of sexual activity and autonomy have a positive relationship, their study did not research HIV testing. [18] Another prior qualitative study conducted by Webber and colleagues in Cambodia reported that using condoms in the marital relationship could raise distrust issues from their husbands, and thus the women did not ask for it, jeopardizing women’s health as they can contract sexually transmitted diseases.[26] Moreover, our findings on the positive correlation between household decision-making and reproductive health decision-making suggested that one decision-making autonomy could influence the other; this is consistent with the finding from another study in Cambodia that revealed that the women who had full decision-making power were more likely to refuse sex.[18] Similarly, Seidu and colleagues found that women with medium and high levels of household decision-making authority were more likely to have safer sex practices than those who did not, which supported the present study’s findings.[10]
Our finding that, when compared to women aged from 15-19 women aged 25–34 were more likely to get HIV tests and those aged 45–49 were less likely to get tested for HIV may need to explore cultural-specific reasons in the Cambodian context. However, our findings were inconsistent with the findings from a study in Kenya in which the women aged 20–29 were more likely to get HIV tests and those from age groups 30–49 were less likely to get HIV tests.[5] Both studies suggest that older age groups were less likely to get an HIV test; perhaps the women in the 45–49 age group may have considered no or low HIV risk, which requires further studies. In view of this finding, it might be beneficial to evaluate a trend of HIV testing prevalence among women aged 45–49 or research the potential reasons. Also, the finding that rural women residents were less likely to get tested for HIV when compared to their urban counterparts is consistent with the findings from a previous multicounty study,[27] and highlights the need for urgent research specifically on the awareness, availability, and accessibility of HIV testing services in rural areas.
Our findings regarding women with some education levels and women in the wealthier groups were consistent with previous findings.[27,28] The current study’s finding that women with some education levels were more likely to get tested for HIV than those who had no formal education also highlighted a need to review the current HIV testing strategies to reach women with no formal education. Also, the findings that women from wealthier groups were more likely to get tested for HIV are interesting, especially if the HIV testing services were free then there should not be a problem for women in the poorest group to access them. However, further studies are required to understand this discrepancy. Future research could explore obstacles for women in the poorest and less educated groups to address ending HIV/AIDS and health inequity gaps. Furthermore, women who had current employment were less likely to get HIV testing, demonstrating that the women in employment may have obstacles finding time to go for an HIV test or may even be avoiding regular/routine HIV testing centers. This finding requires future studies.
Our findings on the significant relationship between HIV testing and HIV-related knowledge such as knowledge and use of HIV self-test kits, hearing of drugs to avoid HIV transmission to babies during pregnancy, and hearing of ARVs to treat HIV were novel findings. Although Cambodia’s Ministry of Health’s National Center for HIV/AIDS implemented HIV self-testing among high-risk populations such as transgender women, people who inject drugs, and people involved in prostitution, it would be beneficial if it were expanded to the general women population.[6] Moreover, the finding that those who had discriminatory attitudes were less likely to get tested for HIV than those who did not also suggest that activities that aim at reducing discrimination could improve the HIV testing situation. Although it is not exactly the same, this finding aligns with a previous study in which the women who never got tested for HIV exhibited a more discriminatory attitude towards people with HIV.[29]
Data Availability
The data for this study was publicly available at https://dhsprogram.com/data/ upon free registration.
Strengths and Limitations of the Study
The strength of this study was the use of the most recent and nationally representative dataset of Cambodia, the inclusion of the important decision-making variables, and HIV-related knowledge such as HIV self-test kits and ARVs. However, this study has some limitations. First, there could be a socially desirable bias as we used the self-reported data. Second, caution must be taken when interpreting the causal relationship as we used cross-sectional data. Third, the HIV-related knowledge questions such as HIV transmission and misconceptions were not included in our study as it only asked for women aged 24 and above, which is not the focus of this study.
CONCLUSION AND GLOBAL HEALTH IMPLICATIONS
To end the HIV epidemic, it is critical that everyone must have access to information and services related to HIV knowledge, testing, and anti-retroviral drugs. The country’s current strategies and programs should be reviewed to ensure that women, especially those who are poorer and less educated, have access to HIV-related information and services and be able to make decisions about their own health. The findings from this study clearly demonstrated that women still need to have control over the important decisions that impact them such as the use of available HIV preventive services.
Key Messages
1. In Cambodia, women with decision-making autonomy have more likelihood of getting a human immunodeficiency virus test than those who do not have one. 2. Cambodian women who had awareness of human immunodeficiency virus self-test kits, although they had never been tested before, were more likely to get tested than those who were not. 3. Women with knowledge related to antiretroviral drugs or drugs to prevent human immunodeficiency virus transmission to babies during pregnancy were more likely to get tested for human immunodeficiency virus than those who did not have such knowledge.
Acknowledgments
The authors want to thank the Demographic and Health Survey Program for their publicly available data.
COMPLIANCE WITH ETHICAL STANDARDS
Conflicts of Interest: The authors declare no competing interests. Financial Disclosure: Nothing to declare. Funding/Support: There was no funding for this study. Ethics Approval: For this study, we used de-identified secondary data, which are available in the public domain, and therefore the ethical review was not required. Declaration of Patient Consent: Patient’s consent not required as there are no patients in this study. Use of Artificial Intelligence (AI)-Assisted Technology for Manuscript Preparation: The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI. Disclaimer: None.
REFERENCES
- World AIDS day 2023: Fact sheet;. [cited 2024 May 23]. Available from: https://www.unaids.org/sites/default/files/media_asset/UNAIDS_FactSheet_en.pdf
- [Google Scholar]
- 2025 AIDS targets: UNAIDS;. [cited 2024 May 23]. Available from: https://www.unaids.org/sites/default/files/2025-AIDS-Targets_en.pdf
- [Google Scholar]
- Sociocultural influences on the transmission of HIV from husbands to wives in Cambodia: The male point of view. Am J Mens Health.. 2017;11((4)):845-54.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- HIV undetectable=untransmittable (U=U), or treatment as prevention;. [cited 2024 May 23]. Available from: https://www.niaid.nih.gov/diseases-conditions/treatment-prevention
- [Google Scholar]
- Trends and correlates of HIV testing amongst women: Lessons learnt from Kenya. Afr J Prim Health Care Fam Med.. 2013;5((1)):547.
- [CrossRef] [PubMed Central] [Google Scholar]
- Cambodia: Report prepared by the joint UN team on AIDS. Progress towards the fast-track targets Online: UNAIDS Aisa and Pacific;. [cited 2024 May 23]. Available from: https://open.unaids.org/sites/default/files/documents/Cambodia_Country%20Report_2020_formatted_EN_1.pdf
- [Google Scholar]
- Cambodia demographic and health survey 2021–22 final report. Phnom Penh, Cambodia, and Rockville, Maryland, USA: NIS, MoH, and ICF;
- [Google Scholar]
- Association between women’s household decision-making autonomy and health insurance enrollment in sub-saharan Africa. BMC Public Health.. 2023;23((1)):610.
- [CrossRef] [Google Scholar]
- Dimensions of women’s autonomy and the influence on maternal health care utilization in a north Indian city. Demography.. 2001;38:67-78.
- [CrossRef] [PubMed] [Google Scholar]
- Women’s healthcare decision-making capacity and HIV testing in sub-Saharan Africa: A multi-country analysis of demographic and health surveys. BMC Public Health.. 2020;20((1)):1592.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Women’s empowerment and HIV testing uptake: A meta-analysis of demographic and health surveys from 33 sub-Saharan African countries. Int J MCH AIDS.. 2020;9((3)):274-286.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Exploring women’s decision-making power and HIV/AIDS prevention practices in South Africa. Int J Environ Res Public Health.. 2022;19((24)):16626.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Empowerment as a predictor of HIV testing among married women in Nepal. J Assoc Nurses AIDS Care.. 2019;30((5)):563-74.
- [CrossRef] [PubMed] [Google Scholar]
- Effects of women’s autonomy on maternal healthcare utilization in Bangladesh: Evidence from a national survey. Sex Reprod Healthc.. 2017;14:40-7.
- [CrossRef] [PubMed] [Google Scholar]
- Women’s decision-making autonomy and utilisation of maternal healthcare services: Results from the Bangladesh demographic and health survey. BMJ Open.. 2017;7((9)):e017142.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Effect of women’s autonomy on maternal health service utilization in Nepal: A cross sectional study. BMC Women’s Health.. 2016;16:1-7.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Women’s decision-making autonomy in the household and the use of maternal health services: An Indonesian case study. Midwifery.. 2020;90:102816.
- [CrossRef] [PubMed] [Google Scholar]
- Negotiation for safer sex among married women in Cambodia: The role of women’s autonomy. J Biosoc Sci.. 2014;46((1)):90-106.
- [CrossRef] [PubMed] [Google Scholar]
- Factors influencing unintended pregnancies amongst adolescent girls and young women in Cambodia. Int J Environ Res Public Health.. 2019;16((20)):4006.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- DHS methodology;. n.d.[cited 2024 May 23]. Available from: https://dhsprogram.com/Methodology/Survey-Types/DHS-Methodology.cfm
- [Google Scholar]
- Global AIDS monitoring 2018: Indicators for monitoring the 2016 United Nations Political Declaration on Ending AIDS;.
- [Google Scholar]
- Understanding women’s empowerment: A comparative analysis of demographic and health surveys (DHS) data. DHS Comparative Reports No. 20. 2008
- [Google Scholar]
- Protecting the privacy of DHS survey respondents;. n.d.[cited 2024 May 23]. Available from: https://dhsprogram.com/Methodology/Protecting-the-Privacy-of-DHS-Survey-Respondents.cfm
- [Google Scholar]
- Knowledge and views regarding condom use among female garment factory workers in Cambodia. Southeast Asian J Trop Med Public Health.. 2010;41:685-95.
- [PubMed] [Google Scholar]
- Determinants of HIV testing uptake among women (aged 15–49 years) in the Philippines, Myanmar, and Cambodia. Int J MCH AIDS.. 2021;10((2)):221-30.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Age-related differences in socio-demographic and behavioral determinants of HIV testing and counseling in HPTN 043/NIMH project. AIDS Behav.. 2018;22((2)):569-79.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Factors associated with discriminatory attitudes towards people living with HIV among adult population in Ethiopia: Analysis on Ethiopian demographic and health survey. SAHARA-J.. 2020;17((1)):38-44.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]






