Translate this page into:
Improving HIV Prevention for Key Populations in Nigeria: Insights on Access, Barriers, Stigma, and Service Utilization

*Corresponding author: Olaniyi Felix Sanni, Research and Development, Heartland Alliance Limited GTE, Gwarinpa, FCT-900108, Abuja, Nigeria sfelix@heartlandalliancenigeria.org
-
Received: ,
Accepted: ,
How to cite this article: Emmanuel GO, Sanni OF, Roger A, Umoh P, Boniface OB, Paul A, Yahaya IM, Auwal AM. Improving HIV Prevention for Key Populations in Nigeria: Insights on Access, Barriers, Stigma, and Service Utilization. Int J MCH AIDS. 2025;14:e005. doi: 10.25259/IJMA_49_2024
Abstract
Background and Objective
Human immunodeficiency virus and acquired immunodeficiency syndrome (HIV/AIDS) remains a significant public health challenge globally, with key populations (KPs) such as female sex workers (FSWs), men who have sex with men (MSM), and people who inject drugs (PWIDs) being disproportionately affected. Despite the availability of various HIV prevention services, including pre-exposure prophylaxis (PrEP) and community-based antiretroviral therapy (ART), the willingness of KPs to access these services remains a critical concern. This study aims to assess the prevalence of HIV and the willingness to access HIV preventive services among KPs in three selected local government areas (LGAs) in Nigeria.
Methods
A cross-sectional study was conducted in 2023 across three LGAs, Gwale, Fagge, and Tarauni, in Kano State, Nigeria, using a snowball sampling technique. A total of 1,320 participants, recruited from brothels and nightclubs, were tested for HIV using self-test kits. Willingness to access HIV services was assessed using a structured questionnaire. Data were analyzed using descriptive statistics and binary logistic regression.
Results
The overall HIV prevalence among KPs was 10.8%. MSM and PWIDs exhibited higher HIV prevalence rates compared to FSWs. Willingness to access HIV preventive services was recorded at 57.7%, with significant influences from geographical location and sexual practices. Participants from Tarauni were more willing to access services, and those engaging in vaginal sex were more likely to seek preventive services. HIV self-testing had a high uptake of 95.9%, while PrEP uptake was 68.0%. Major barriers included stigma, lack of comprehensive services, and limited knowledge of service providers.
Conclusion and Global Health Implications
This study highlights the critical need for targeted interventions addressing the specific barriers faced by KPs in these regions. Enhancing service accessibility and addressing stigma is essential for reducing HIV transmission and achieving epidemic control in Nigeria by 2030.
Keywords
Health Services Accessibility
HIV Seroprevalence
Key Populations
Population Groups
Willingness to Access HIV Services
INTRODUCTION
Human immunodeficiency virus and acquired immunodeficiency syndrome (HIV/AIDS) continue to be a significant public health challenge worldwide, with approximately 39.9 million people globally reported living with HIV in 2023.[1] Despite substantial progress in prevention and treatment, certain groups remain disproportionately affected, contributing significantly to the persistence of the epidemic.[1] Among these groups, Key Populations (KPs), including people who inject drugs (PWIDs), men who have sex with men (MSMs), and female sex workers (FSWs), are particularly vulnerable due to a combination of behavior, structural, and societal factors of marginalization.[2,3] Globally, KPs and their sexual partners account for approximately 55% of new HIV infections in 2022.[2] and range between 40% and 50% in 2016.,[4] highlighting their critical role in the ongoing transmission of the virus.
The burden of HIV among KPs in Africa is notably high, with sub-Saharan Africa bearing the heaviest burden.[5] According to a 2016 World Health Organization (WHO) policy brief, the proportion of new infections in key populations is substantial. However, it varies greatly across the sub-Saharan African region, with an estimated 10% in Uganda, 30% in Burkina Faso, 34% in Kenya, 37% in Nigeria, 43% in Ghana, and 45% in Benin.[4] KPs in this region face even greater risks due to factors such as stigma, discrimination, and limited access to healthcare services. Studies have shown that HIV prevalence among KPs is significantly higher than in the general population, making them a focal point for intervention efforts.[6] For example, the prevalence of HIV among MSMs and FSWs in sub-Saharan Africa is higher than among the general adult population, underscoring the urgency of targeted prevention strategies.[7]
In Nigeria, the situation mirrors the broader African context, with KPs experiencing disproportionately high rates of HIV infection. Onovo et al.[8] reported that, despite making up only 2.3% of Nigeria’s adult population, KPs and their sexual partners account for an estimated 11.30% of new HIV infections.[8] The HIV epidemic in the country is heavily concentrated among these populations, who are often marginalized and underserved by the healthcare system. According to recent studies, the prevalence of HIV among KPs in Nigeria is significantly higher than in the general population, with FSWs and MSM being particularly affected.[9] This heightened vulnerability is exacerbated by factors such as poverty, social exclusion, and the criminalization of certain behaviors, which further hinder access to essential HIV prevention and treatment services.[9]
Despite the availability of various HIV prevention services, including pre-exposure prophylaxis (PrEP) and community-based antiretroviral therapy (ART), the willingness of KPs to access these services remains a critical concern. Several factors influence this willingness, including awareness, perceived stigma, and the quality of healthcare services provided.[10] A survey conducted in 2018 highlighted that high-risk drug users, such as PWIDs in Nigeria, faced frequent legal challenges, with an average of three arrests per person.[11] Access to oral PrEP in Nigeria remains limited, with only a small fraction of the population at risk of having initiated the treatment.[12] Furthermore, fewer than half of high-risk individuals, including PWIDs, are projected to have accessed HIV testing services (HTS), which is a critical step in linking individuals to ART and achieving viral suppression.[13]
Notwithstanding the preventive and treatment services available, their uptake among KPs is often limited due to stigma, criminalization, and other structural barriers.[14] As a result, there is a need to understand the specific factors that influence the willingness of KPs in Nigeria to access HIV preventive services. This study aims to examine the prevalence of HIV and the desire to access HIV preventive services among KPs in three selected Local Government Areas (LGAs) in Nigeria. By focusing on these specific communities, the study seeks to provide insights that could inform more effective and targeted intervention strategies, ultimately contributing to the reduction of HIV transmission among KPs and contributing to the broader goal of eliminating the HIV epidemic in Nigeria by 2030.
METHODS
Design and Procedure
This cross-sectional study was conducted in 2023, involving data collection from KPs in nightclubs and brothels across three LGAs in Kano, Nigeria. These LGAs were specifically selected due to their high concentration of KPs. Participants underwent HIV testing using self-test kits, and those who tested positive were promptly linked to treatment services. To encourage the participation of participants in this sensitive study, the research team approached potential participants respectfully, explaining the study’s purpose and emphasizing confidentiality, privacy, and the importance of HIV awareness and treatment. They provided brief counseling in private spaces within the venues, ensuring participants felt comfortable and informed about the process, benefits, and voluntary nature of HIV self-testing. Sexually active participants in this study refer to an individual who has engaged in any form of sexual activity (vaginal, anal, or oral sex). Ethical considerations were thoroughly addressed, and support services were readily available for any follow-up needs. Additionally, the study assessed the willingness of KPs to access HIV services using a well-structured 17-item questionnaire. A willingness threshold was set at 75%.
Population and Sampling
This study was conducted in three LGAs: Gwale, Fagge, and Tarauni in Kano State, Northern Nigeria, with a population of Fagge (1,282,500), Gwale (588,500), and Tarauni (364,900).[15] In order to minimize potential selection bias, the study utilized snowball sampling to recruit participants, enhancing reach within the target population. However, FSWs unwilling to participate were excluded, and eligibility was restricted to those proficient in English or Pidgin. Individuals who could not communicate in either language were ineligible to participate. KPs aged 18 and above residing in the selected LGAs in Kano State were included in the study, while those below 18 years were excluded.
This study used a quantitative research approach to ensure comprehensive data collection and analysis. The snowball sampling technique was employed; the participants were recruited to participate in the survey from the brothels and clubs across the three LGAs in Kano State with referrals from initial participants. The initial participant selection was based on key informants familiar with the target locations within the three LGAs in Kano State. These informants identified individuals who frequented or worked in brothels and clubs, facilitating the recruitment of participants who met the study criteria.
The sample size for this study was calculated using a 5.8% prevalence of HIV among key populations in Kano State, according to Adeoye et al.[16] and a single proportion formula:
Where Z is the confidence level with Z-value for a 95% confidence level = 1.96.
Prevalence of HIV among KPs in Kano State, p = 5.8%, = 0.058 (Adeoye et al.[16]).
E is the margin of error, often set at 1.38% or 0.0138, to ensure a precise estimation of the HIV prevalence among key populations in Kano State while accounting for possible variations in the sample.
Adding 20% attrition, n = 1,100 + 220, = 1,320 (approximately).
To achieve maximum sample size, 20% attrition and 1.38% marginal error were used because of the anticipated decline to participate in the study by KPs due to stigmatization and unwillingness to disclose their status.
A proportionate allocation method was used to determine the minimum sample size from each LGA based on the population size of each LGA: Fagge (1,282,500), Gwale (588,500), and Tarauni (364,900). The estimated maximum sample sizes were Fagge (757), while the minimum estimated sample sizes for the remaining two LGAs were Gwale (347) and Tarauni (216). However, 1,320 valid data were collected across the three LGAs, representing 100% of the estimated minimum sample size. The sample size is justified due to the use of snowball sampling, which relies on participant referrals and can result in a broader reach, especially when recruiting hard-to-reach populations. This approach helps ensure the sample is sufficiently representative of the target population across three local government areas in Kano State, Nigeria.
Study Variables and Instruments
The survey employed a well-structured questionnaire comprising both open-ended and closed-ended questions to collect primary qualitative data from consenting KPs. The questionnaire was originally and specifically developed for this survey to address the unique focus areas of the research. This customization ensured relevance to the targeted KPs, facilitating the collection of specific primary qualitative data directly related to the study objectives. The questionnaire was divided into sections covering socio-demographics, willingness to access HIV services, HIV status, and the reasons for and against utilizing HIV services. Participants were provided with self-test kits to determine their HIV status. To address potential hesitancy in reporting HIV-positive results, participants were assured of confidentiality and provided with a supportive environment for disclosing their test results. Each participant self-reported their HIV status, with trained counselors available to offer guidance and support throughout the process, ensuring a non-judgmental atmosphere for full participation.
Data Analysis
The collected data were recorded, cleaned, and analyzed using Microsoft Excel and the Statistical Package for the Social Sciences (SPSS) for Windows, Version 28.0.[17] The data analysis included descriptive statistics, frequency distribution, and binary logistic regression, with the results presented in tables and figures for clear interpretation. Binary logistic regression was employed to assess the influence of socio-demographic variables on HIV prevalence and the willingness to access HIV services. Additionally, the reasons for and against HIV service uptake were illustrated using charts. The study adhered to the STrengthening the Reporting of OBservational studies in Epidemiology (STROBE) reporting of observational studies guidelines, as recommended by the Enhancing the QUAlity and Transparency Of health Research (EQUATOR) Network, to ensure transparent reporting of methods and findings.[18] Following these guidelines, data were systematically recorded, cleaned, and analyzed. This adherence enhances the reproducibility and reliability of the findings.
Informed consent was obtained from all participants, who were also informed of their right to withdraw from the study at any point without the need to provide any justification for their decision. Also, given the socially sensitive nature of the study, participants’ privacy and confidentiality were prioritized throughout the research process. All personal information and data collected were kept strictly confidential and securely stored, with access limited to authorized personnel only.
RESULTS
Socio-Demographic and Behavioral Characteristics of the Respondents
Table 1 highlights the socio-demographic and behavioral characteristics of KPs in Kano State. The sample includes 49.2% FSWs, 32.6% MSM, and 18.2% PWIDs. Most respondents are young, with 78.1% aged 18–34. Educational attainment varies, with 47.1% having secondary education, 25.7% tertiary education, and 16.8% having no formal education. The participants are evenly distributed across three local government areas: Gwale (37.9%), Fagge, and Tarauni (31.1% each). Drug abuse is common, with 58.4% reporting a history of abuse and 39.9% having injected drugs. Sexual behaviors reveal that 63.4% had multiple partners in the last three months, with vaginal sex being the most prevalent (66.7%), followed by anal (18.9%) and oral sex (12.9%). The age of first sexual debut is mostly between 14 and 17 years (37.0%). Motivations for sexual activity include fun/love/marriage (57.5%) and financial reasons (20.2%). Transactional sex is prevalent, with 29.4% paying for sex and 27.8% receiving gifts for sex. Condom use is inconsistent, with only 36.6% always using condoms in the last three months and 33.3% not using them during their last sexual encounter.
| Variable | Parameter (n = 1,320) | Frequency | Percentage (%) |
| KPs group | MSM | 430 | 32.6 |
| FSWs | 650 | 49.2 | |
| PWIDs | 240 | 18.2 | |
| Age (years) | 18–24 | 426 | 32.3 |
| 25–34 | 604 | 45.8 | |
| 35–45 | 210 | 15.9 | |
| Above 45 | 80 | 6.1 | |
| Education level | No formal education | 222 | 16.8 |
| Primary | 137 | 10.4 | |
| Secondary | 622 | 47.1 | |
| Tertiary | 339 | 25.7 | |
| Local government area | Fagge | 410 | 31.1 |
| Gwale | 500 | 37.9 | |
| Tarauni | 410 | 31.1 | |
| Drugs abuse | Never abused drugs | 549 | 41.6 |
| Ever abused drugs | 771 | 58.4 | |
| Drugs injection | Never injected drugs | 793 | 60.1 |
| Ever injected drugs | 527 | 39.9 | |
| Age of first sexual debut (years) | Below 13 | 305 | 23.1 |
| 14–17 | 489 | 37.0 | |
| 18 and above | 446 | 33.8 | |
| Reason for first sexual intercourse | Having fun/love/marriage | 759 | 57.5 |
| Peer pressure | 167 | 12.7 | |
| Rape/forced | 24 | 1.8 | |
| To obtain money | 267 | 20.2 | |
| Sexually active in the last three months | Not sexually active | 216 | 16.4 |
| Sexually active | 1,104 | 83.6 | |
| Sexual partners during the last three months | One | 267 | 20.2 |
| More than one | 837 | 63.4 | |
| Vaginal sex in the last three months | Not have vaginal sex | 224 | 17.0 |
| Have vaginal sex | 880 | 66.7 | |
| Anal sex in the last three months | Not have anal sex | 855 | 64.8 |
| Have anal sex | 249 | 18.9 | |
| Oral sex in the last three months | Not have oral sex | 934 | 70.8 |
| Have oral sex | 170 | 12.9 | |
| Transactional sex engaged in | No transactional sex | 183 | 13.9 |
| Paid for sex | 388 | 29.4 | |
| Paid & received | 166 | 12.6 | |
| Received gift for sex | 367 | 27.8 | |
| Condoms used in the last three months | Always | 483 | 36.6 |
| Irregularly | 621 | 47.0 | |
| Condoms used during the last sexual encounter | Not used condoms | 440 | 33.3 |
| Used condoms | 663 | 50.2 |
KPs: Key populations, FSWs: Female sex workers, MSM: Men who have sex with men, PWIDs: People who inject drugs.
Prevalence of HIV and the Associated Factors Among FSWs in Kano State
Table 2 presents HIV prevalence and associated factors among KPs in Kano State, revealing a 10.8% HIV positivity rate. FSWs had a significantly lower HIV prevalence compared to MSM (AOR: 0.346, p = 0.001). In contrast, PWIDs were at a higher risk of being HIV-positive than MSM (AOR: 2.827, p = 0.019). Interestingly, those who had ever injected drugs were less likely to be HIV-positive compared to those who had never injected (AOR: 0.253, p = 0.001). Engaging in vaginal or anal sex in the past three months significantly increased the likelihood of being HIV positive, with adjusted odds ratios of 5.270 (p < 0.001) and 2.213 (p = 0.030), respectively. Other factors such as age, education, location, drug abuse, sexual debut, sexual partner, oral sex, transactional sex, and condom use during the last sexual encounter or over the past three months did not show significant associations with HIV prevalence.
| Variable | Negative n (%) | Positive n (%) | COR (95% CI) | p-value | AOR (95% CI) | p-value |
| HIV test result | 1,178 (89.2) | 142 (10.8) | - | - | - | - |
| KPs group | ||||||
| MSM | 377 (87.7) | 53 (12.3) | Ref | - | - | - |
| FSWs | 595 (91.5) | 55 (8.5) | 0.658 [0.441–0.980] | 0.039* | 0.346 [0.184–0.650] | 0.001* |
| PWIDs | 206 (85.8) | 34 (14.2) | 1.174 [0.739–1.865] | 0.497 | 2.827 [1.183–6.757] | 0.019* |
| Age category (years) | ||||||
| 18–24 | 381 (89.4) | 45 (10.6) | Ref | - | - | - |
| 25–34 | 534 (88.4) | 70 (11.6) | 1.110 [0.746–1.651] | 0.607 | 1.319 [0.819–2.125] | 0.255 |
| 35–45 | 192 (91.4) | 18 (8.6) | 0.794 [0.447–1.408] | 0.430 | 0.834 [0.418–1.665] | 0.607 |
| Above 45 | 71 (88.8) | 9 (11.3) | 1.073 [0.502–2.293] | 0.855 | 1.259 [0.458–3.458] | 0.655 |
| Respondent education level | ||||||
| No formal education | 196 (88.3) | 26 (11.7) | 1.418 [0.811–2.479] | 0.221 | 1.534 [0.804–2.928] | 0.194 |
| Primary | 120 (87.6) | 17 (12.4) | 1.514 [0.803–2.857] | 0.200 | 1.196 [0.553–2.589] | 0.649 |
| Secondary | 552 (88.7) | 70 (11.3) | 1.356 [0.860–2.136] | 0.190 | 1.702 [0.982–2.950] | 0.058 |
| Tertiary | 310 (91.4) | 29 (8.6) | Ref | - | - | - |
| Local government area | ||||||
| Fagge | 364 (88.8) | 46 (11.2) | Ref | - | - | - |
| Gwale | 454 (90.8) | 46 (9.2) | 0.802 [0.521–1.234] | 0.315 | 0.922 [0.474–1.796] | 0.812 |
| Tarauni | 360 (87.8) | 50 (12.2) | 1.099 [0.718–1.683] | 0.664 | 0.915 [0.491–1.704] | 0.780 |
| Drug abuse | ||||||
| Never abused drugs | 481 (87.6) | 68 (12.4) | Ref | - | - | - |
| Ever abused drugs | 697 (90.4) | 74 (9.6) | 0.751 [0.530–1.065] | 0.108 | 0.832 [0.485–1.428] | 0.506 |
| Drugs injection | ||||||
| Never injected drugs | 696 (87.8) | 97 (12.2) | Ref | - | - | - |
| Ever injected drugs | 482 (91.5) | 45 (8.5) | 0.670 [0.462–0.972] | 0.035* | 0.253 [0.112–0.570] | 0.001* |
| Age of first sexual debut | ||||||
| Below 13 years | 266 (87.2) | 39 (12.8) | 0.829 [0.534–1.288] | 0.405 | 0.838 [0.485–1.447] | 0.525 |
| 14–17 years | 436 (89.2) | 53 (10.8) | 0.765 [0.485–1.208] | 0.250 | 0.682 [0.367–1.269] | 0.227 |
| 18 years and above | 401 (89.9) | 45 (10.1) | Ref | - | - | - |
| Reason for first sexual intercourse | ||||||
| Having fun/love/marriage | 675 (88.9) | 84 (11.1) | Ref | - | - | - |
| Peer pressure | 152 (91.0) | 15 (9.0) | 0.793 [0.445–1.412] | 0.431 | 0.888 [0.450–1.752] | 0.733 |
| Rape/forced | 22 (91.7) | 2 (8.3) | 0.731 [0.169–3.162] | 0.674 | 1.092 [0.236–5.052] | 0.911 |
| To obtain money | 232 (86.9) | 35 (13.1) | 1.212 [0.795–1.848] | 0.371 | 1.065 [0.610–1.860] | 0.825 |
| Sexual partners during the last three months | ||||||
| One | 245 (91.8) | 22 (8.2) | Ref | - | - | - |
| More than one | 744 (88.9) | 93 (11.1) | 1.392 [0.856–2.265] | 0.183 | 1.807 [0.971–3.365] | 0.062 |
| Vaginal sex in the last three months | ||||||
| Not have vaginal sex | 204 (91.1) | 20 (8.9) | Ref | - | - | - |
| Have vaginal sex | 785 (89.2) | 95 (10.8) | 1.234 [0.744–2.048] | 0.415 | 5.270 [2.305–12.052] | <0.001* |
| Anal sex in the last three months | ||||||
| Not have anal sex | 772 (90.3) | 83 (9.7) | Ref | - | - | - |
| Have anal sex | 217 (87.1) | 32 (12.9) | 1.372 [0.888–2.119] | 0.154 | 2.213 [1.079–4.539] | 0.030* |
| Oral sex in the last three months | ||||||
| Not have oral sex | 833 (89.2) | 101 (10.8) | Ref | - | - | - |
| Have oral sex | 156 (91.8) | 14 (8.2) | 0.740 [0.413–1.328] | 0.313 | 0.758 [0.401–1.432] | 0.393 |
| Transactional sex engaged in | ||||||
| No transactional sex | 162 (88.5) | 21 (11.5) | Ref | - | - | - |
| Paid for sex | 343 (88.4) | 45 (11.6) | 1.012 [0.584–1.755] | 0.966 | 0.922 [0.470–1.809] | 0.814 |
| Paid & received | 149 (89.8) | 17 (10.2) | 0.880 [0.447–1.732] | 0.712 | 0.610 [0.261–1.423] | 0.253 |
| Received gift for sex | 335 (91.3) | 32 (8.7) | 0.737 [0.412–1.318] | 0.303 | 0.558 [0.263–1.186] | 0.129 |
| Condoms used in the last three months | ||||||
| Always | 442 (91.5) | 41 (8.5) | Ref | - | - | - |
| Irregularly | 547 (88.1) | 74 (11.9) | 1.458 [0.976–2.179] | 0.066 | 1.066 [0.621–1.831] | 0.816 |
| Condoms used during the last sexual encounter | ||||||
| Not used condoms | 385 (87.5) | 55 (12.5) | 1.462 [0.991–2.158] | 0.055 | 1.336 [0.799–2.235] | 0.269 |
| Used condoms | 604 (91.1) | 59 (8.9) | Ref | - | - | - |
Source: Field Survey Conducted in Kano State Crude Odds Ratio (COR), Adjusted Odds Ratio (AOR).
*Significant at p < 0.05. KPs: Key populations, FSWs: Female sex workers, MSM: Men who have sex with men, PWIDs: People who inject drugs, LGAs: Local government areas, CI: Confidence interval, Ref: Reference.
Factors Associated With Willingness to Access HIV Service Among KPs
Table 3 highlights key factors influencing the willingness of KPs in Kano State to access HIV preventive services, with an overall willingness rate of 57.7%. FSWs were initially more willing to access these services than MSM (COR: 2.136, p < 0.001), but this significance disappeared after adjusting for other variables (AOR: 1.075, p = 0.756). Education level had mixed effects; both secondary and tertiary education were linked to lower willingness compared to those with no formal education in the crude analysis, but these associations were not significant after adjustment. Geographical location played an important role in willingness, with respondents from Tarauni being much more willing to access services than those from Fagge (AOR: 26.404, p < 0.001). Those from Gwale showed less willingness in the crude analysis (COR: 0.752, p = 0.034), but this reversed in the adjusted model (AOR: 1.729, p = 0.013). Drug use history showed a positive association with willingness in the crude analysis but lost significance after adjustment. Sexual practices were strong predictors; individuals who engaged in vaginal sex in the last three months were significantly more likely to seek HIV services (AOR: 4.344, p < 0.001), while those who engaged in anal sex were less likely to be willing (AOR: 0.413, p = 0.002). Engagement in transactional sex initially appeared to increase willingness, but this was not significant after adjustment. Condom use during the last sexual encounter was associated with a higher desire to access services (AOR: 1.660, p = 0.012).
| Variable | Not Willing n (%) | Willing n (%) | COR (95% CI) | p-value | AOR (95% CI) | p-value |
| Willing to take HIV services | 559 (42.3) | 761 (57.7) | - | - | - | - |
| KPs group | ||||||
| MSM | 226 (52.6) | 204 (47.4) | Ref | - | - | - |
| FSWs | 222 (34.2) | 428 (65.8) | 2.136 [1.665–2.740] | <0.001* | 1.075 [0.682–1.692] | 0.756 |
| PWIDs | 111 (46.3) | 129 (53.8) | 1.287 [0.938-1.767] | 0.118 | 0.647 [0.366–1.143] | 0.134 |
| Age category (years) | ||||||
| 18–24 | 184 (43.2) | 242 (56.8) | Ref | - | - | - |
| 25–34 | 248 (41.1) | 356 (58.9) | 1.091 [0.849–1.403] | 0.495 | 1.147 [0.804–1.638] | 0.449 |
| 35–45 | 88 (41.9) | 122 (58.1) | 1.054 [0.754–1.473] | 0.758 | 1.003 [0.629–1.601] | 0.989 |
| Above 45 | 39 (48.8) | 41 (51.2) | 0.799 [0.495–1.290] | 0.359 | 1.524 [0.774–2.997] | 0.223 |
| Respondent Education Level | ||||||
| No formal education | 76 (34.2) | 146 (65.8) | Ref | - | - | - |
| Primary | 46 (33.6) | 91 (66.4) | 1.030 [0.657–1.615] | 0.898 | 1.362 [0.748–2.480] | 0.312 |
| Secondary | 289 (46.5) | 333 (53.5) | 0.600 [0.436–0.825] | 0.002* | 1.063 [0.684–1.652] | 0.786 |
| Tertiary | 148 (43.7) | 191 (56.3) | 0.672 [0.473–0.954] | 0.026* | 1.037 [0.637–1.690] | 0.883 |
| Local government area | ||||||
| Fagge | 214 (52.2) | 196 (47.8) | Ref | - | - | - |
| Gwale | 296 (59.2) | 204 (40.8) | 0.752 [0.578–0.979] | 0.034* | 1.729 [1.120–2.670] | 0.013* |
| Tarauni | 49 (12.0) | 361 (88.0) | 8.044 [5.636–11.481] | <0.001* | 26.404 [14.987–46.518] | <0.001* |
| Drug abuse | ||||||
| Never abused drugs | 266 (48.5) | 283 (51.5) | Ref | - | - | - |
| Ever abused drugs | 293 (38.0) | 478 (62.0) | 1.533 [1.228–1.914] | <0.001* | 1.096 [0.729–1.646] | 0.660 |
| Drugs injection | ||||||
| Never injected drugs | 361 (45.5) | 432 (54.5) | Ref | - | - | - |
| Ever injected drugs | 198 (37.6) | 329 (62.4) | 1.389 [1.109–1.739] | 0.004* | 1.363 [0.867–2.144] | 0.180 |
| Age of first sexual debut | ||||||
| Below 13 years | 113 (37.0) | 192 (63.0) | Ref | - | - | - |
| 14–17 years | 203 (41.5) | 286 (58.5) | 0.829 [0.618–1.112] | 0.212 | 1.140 [0.745–1.745] | 0.546 |
| 18 years and above | 195 (43.7) | 251 (56.3) | 0.758 [0.562–1.021] | 0.068 | 1.058 [0.672–1.664] | 0.808 |
| Reason for first sexual intercourse | ||||||
| Having fun/love/marriage | 318 (41.9) | 441 (58.1) | Ref | - | - | - |
| Peer pressure | 76 (45.5) | 91 (54.5) | 0.863 [0.616–1.209] | 0.393 | 1.627 [1.046–2.531] | 0.031* |
| Rape/forced | 11 (45.8) | 13 (54.2) | 0.852 [0.377–1.927] | 0.701 | 0.769 [0.275–2.150] | 0.617 |
| To obtain money | 92 (34.5) | 175 (65.5) | 1.372 [1.026–1.834] | 0.033* | 0.880 [0.576–1.343] | 0.554 |
| Sexual partners during the last three months | ||||||
| One | 96 (36.0) | 171 (64.0) | Ref | - | - | - |
| More than one | 332 (39.7) | 505 (60.3) | 0.854 [0.642–1.136] | 0.279 | 0.972 [0.640–1.475] | 0.893 |
| Vaginal sex in the last three months | ||||||
| Not have vaginal sex | 161 (71.9) | 63 (28.1) | Ref | - | - | - |
| Have vaginal sex | 267 (30.3) | 613 (69.7) | 5.867 [4.240–8.119] | <0.001* | 4.344 [2.227–8.474] | <0.001* |
| Anal sex in the last three months | ||||||
| Not have anal sex | 262 (30.6) | 593 (69.4) | Ref | - | - | - |
| Have anal sex | 166 (66.7) | 83 (33.3) | 0.221 [0.164–0.298] | <0.001* | 0.413 [0.233–0.732] | 0.002* |
| Oral sex in the last three months | ||||||
| Not have oral sex | 338 (36.2) | 596 (63.8) | Ref | - | - | - |
| Have oral sex | 90 (52.9) | 80 (47.1) | 0.504 [0.363–0.701] | <0.001* | 0.841 [0.541–1.307] | 0.441 |
| Transactional sex engaged in | ||||||
| No transactional sex | 82 (44.8) | 101 (55.2) | Ref | - | - | - |
| Paid for sex | 124 (32.0) | 264 (68.0) | 1.729 [1.205–2.480] | 0.003* | 0.843 [0.529–1.343] | 0.472 |
| Paid & received | 89 (53.6) | 77 (46.4) | 0.702 [0.461–1.071] | 0.101 | 0.687 [0.375–1.259] | 0.224 |
| Received gift for sex | 133 (36.2) | 234 (63.8) | 1.428 [0.996–2.049] | 0.053 | 0.710 [0.420–1.200] | 0.201 |
| Condoms used in the last three months | ||||||
| Always | 167 (34.6) | 316 (65.4) | 0.729 [0.570–0.932] | 0.012* | 0.910 [0.620–1.335] | 0.631 |
| Irregularly | 261 (42.0) | 360 (58.0) | Ref | - | - | - |
| Condoms used during the last sexual encounter | ||||||
| Not used condoms | 195 (44.3) | 245 (55.7) | Ref | - | - | - |
| Used condoms | 233 (35.1) | 430 (64.9) | 1.469 [1.148–1.880] | 0.002* | 1.660 [1.116–2.470] | 0.012* |
Source: Field Survey Conducted in Nigeria Crude Odds Ratio (COR), Adjusted Odds Ratio (AOR).
*Significant at p < 0.05. KPs: Key populations, FSWs: Female sex workers, MSM: Men who have sex with men, PWIDs: People who inject drugs, CI: Confidence interval, Ref: Reference.
HIV Services Uptake Among KPs
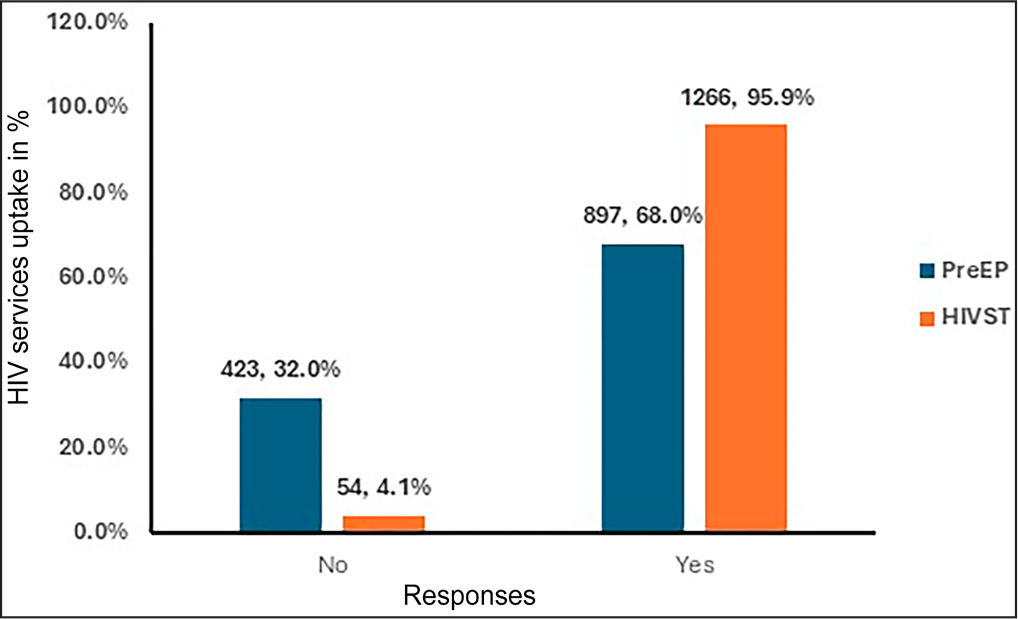
Figure 1 presents the uptake of two key HIV services among KPs. A substantial majority of KPs, 95.9%, reported using HIV self-testing (HIVST), while the uptake of PrEP was 68.0%.
Reasons for Accessing HIV Services Among KPs
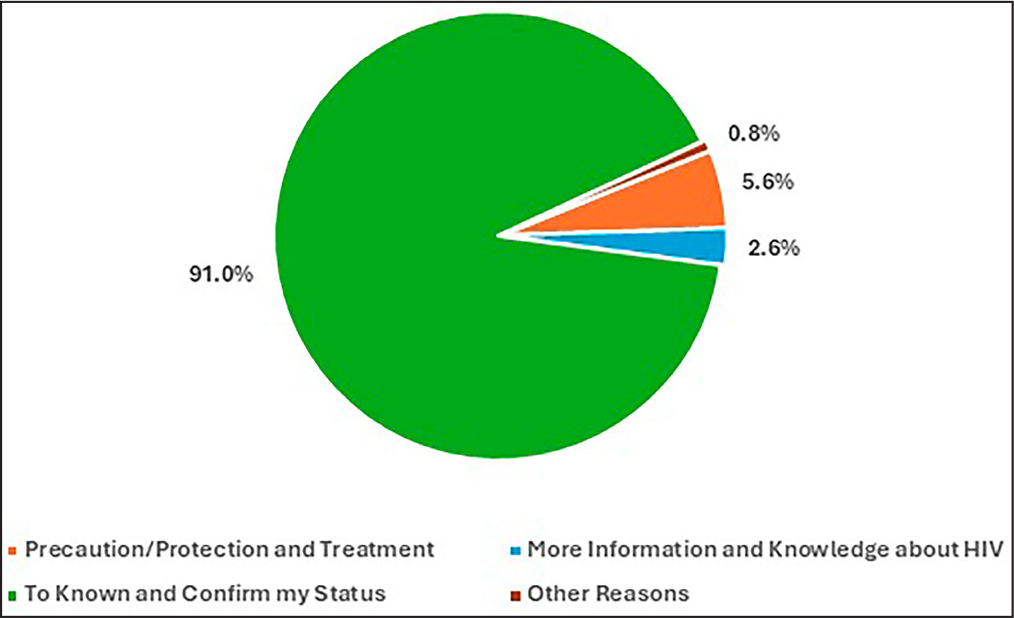
Figure 2 outlines the primary reasons KPs access HIV services. The overwhelming majority, 91.0%, cited the desire to “know and confirm my status” as their main motivation. A smaller portion, 5.6%, accessed services for precaution, protection, and treatment. Only 2.6% sought HIV services to gain more information and knowledge about HIV. A very small fraction, 0.8%, accessed services for other reasons.
Obstacles to Accessing HIV Services Among KPs
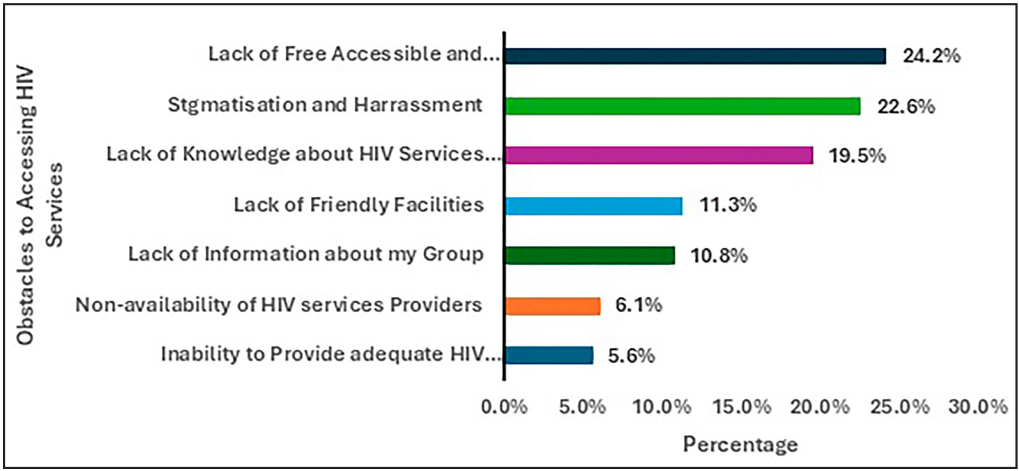
Figure 3 shows the key obstacles faced by KPs in accessing HIV services. The most significant barrier, cited by 24.2%, is the lack of free, accessible, and comprehensive HIV services. The issue of stigmatization and harassment was reported by 22.6% as the obstacle to accessing the services. Lack of knowledge about HIV service providers is another significant obstacle, with 19.5% reporting this as a barrier. Lack of friendly facilities was identified by 11.3%, and 10.8% cited a lack of information about my group as a barrier to accessing HIV services among the KPs. Smaller percentages of respondents reported the non-availability of HIV service providers (6.1%) and inability to provide adequate HIV counseling services (5.6%) as barriers.
DISCUSSION
The study found that FSWs made up the largest proportion of respondents (49.2%), followed by MSM at 32.6% and PWIDs at 18.2%. This distribution is consistent with national data highlighting FSWs and MSM as key populations in Nigeria. The majority of respondents were young (78.1% aged 18–34), emphasizing the heightened vulnerability of youth in the HIV epidemic, a trend seen in other studies. Educational levels varied, with nearly half of the participants having secondary education while some lacked formal education. This variation aligns with other research showing that educational background influences engagement with HIV services. The study also reported a high prevalence of drug abuse (58.4%) and injection drug use (39.9%), reinforcing the strong link between substance use and HIV risk behaviors.
Sexual behaviors indicated high-risk practices, including multiple sexual partners (63.4%) and inconsistent condom use (36.6% always using condoms). These findings are consistent with studies highlighting risky sexual behaviors as major drivers of HIV transmission among KPs.[19,20]. The early age of sexual debut (37.0% between 14 and 17 years) and the prevalence of transactional sex further emphasize the structural and economic vulnerabilities faced by KPs, aligning with observations by Durosinmi-Etti et al.[21] and Sanni et al.[10] The overall HIV prevalence among KPs in Kano State was 10.8%, with significant variations across groups. FSWs exhibited a lower prevalence compared to MSM, while PWIDs had a higher prevalence than MSM. These findings partially align with the National HIV/AIDS & STIs Control Programme.[22] However, the lower prevalence among FSWs contrasts with some studies that indicate FSWs often bear a high HIV burden due to their high-risk behaviors and exposure.[16,23] This discrepancy may be attributed to effective targeted interventions for FSWs in Kano State, as suggested by Onovo et al.,[24] who highlighted the success of community-based ART clinics.
Interestingly, respondents who had ever injected drugs were less likely to be HIV-positive. This counterintuitive finding contrasts with the well-established association between injection drug use and higher HIV risk.[16] Possible explanations include effective harm reduction programs or selection bias within the study sample, warranting further investigation.
Engagement in vaginal and anal sex significantly increased the likelihood of HIV positivity, underscoring the critical role of unprotected sexual activities in HIV transmission. These results are consistent with global and regional studies emphasizing the high transmission risk associated with these sexual practices, as reported by WHO[25] and Sanni et al.[10]
The study found that 57.7% of KPs were willing to access HIV preventive services. While FSWs initially appeared more willing than MSM in the crude analysis, this significance did not hold after adjustment. This nuanced finding aligns with Adepoju et al.,[26] who emphasized the complexity of factors influencing willingness to access services beyond demographic categories.
Education levels initially showed that secondary and tertiary education were associated with less willingness to access services, a finding that dissipated after adjustment. This contrasts with Durosinmi-Etti et al.,[21] who found that higher education often correlates with greater health service uptake due to increased awareness and health literacy. The discrepancy may reflect specific contextual factors in Kano State, such as differing perceptions of HIV services among educated individuals.
Geographical location emerged as a strong determinant, with respondents from Tarauni significantly more willing to access services compared to those from Fagge and those from Gwale showing increased willingness after adjustment. This finding is supported by Lo et al.[27] (2021), who emphasized the importance of accurate hotspot mapping and tailored interventions based on geographical nuances.
Sexual practices significantly influence willingness to access services. Individuals engaging in vaginal sex were more likely to seek HIV services, while those engaging in anal sex were less willing. This aligns with Bakare,[19] who identified specific sexual behaviors as critical factors in service uptake. The positive association with condom use further underscores the role of preventive behaviors in enhancing service willingness, consistent with global prevention strategies.[25]
The uptake of HIVST was remarkably high at 95.9%, while PrEP uptake stood at 68.0%. The high HIVST uptake mirrors findings by Shitu et al.,[28] who reported increased accessibility and acceptability of self-testing methods among KPs. The substantial PrEP uptake is encouraging and aligns with studies advocating for expanded PrEP availability to high-risk groups.[7,25] However, the overall PrEP uptake remains relatively low compared to HIVST, highlighting the need for continued efforts to promote PrEP awareness and accessibility, as suggested by Sanni et al.[10] primary motivation for accessing HIV services was the desire to “know and confirm my status” (91.0%), which aligns with global trends emphasizing the importance of HIV status awareness in prevention and treatment.[1] A smaller proportion accessed services for precaution, protection, and treatment, reflecting the varied motivations among KPs. This finding supports the recommendations by Durosinmi-Etti et al.[21] for tailored communication strategies that address diverse motivations for service uptake.
The study identified key barriers to accessing HIV services, with the most significant being the lack of free, accessible, and comprehensive services (24.2%), followed by stigmatization and harassment (22.6%). These challenges align with previous research by Emmanuel et al.[29] and Bakare,[19] which also cited stigma and service accessibility as major obstacles for KPs.
In light of the identified barriers to accessing HIV services, such as the lack of free, accessible, and comprehensive options as well as stigmatization and harassment, digital health technologies and social media can play a crucial role in health promotion and expanding access to these services. Digital platforms allow for anonymous and widespread dissemination of health information, which can help reduce stigma by normalizing HIV education and engagement. Social media, in particular, is evolving as a significant tool in health communication, contributing to improved quality of life across diverse populations globally[30] and among specific groups, such as older adults.[31] These platforms can help bridge gaps in access by offering supportive networks and accessible information, making health promotion more inclusive, and reducing barriers faced by marginalized groups. Additionally, the lack of knowledge about HIV service providers (19.5%) and unfriendly facilities (11.3%) further supports findings from earlier studies that emphasize the need for more inclusive and informed service delivery models.[24]
Limitations of the Study
The study’s reliance on self-reported data for sensitive topics such as drug use, sexual behavior, and condom use introduces potential bias. Participants may have underreported or overreported their behaviors due to social desirability or recall bias, which could affect the accuracy of the findings. Additionally, while the study primarily focused on HIV prevalence, it did not explore other sexually transmitted infections (STIs) or broader health issues among (KPs). Including these factors would have provided a more comprehensive understanding of the health challenges faced by KPs. Furthermore, the pervasive stigma and discrimination experienced by KPs may have influenced their willingness to participate and their honesty in reporting behaviors, potentially skewing the results and impacting the effectiveness of future interventions. The study’s generalizability is limited due to the purposeful selection of study sites and the use of snowball sampling, which may not represent the broader KPs. This sampling method introduces potential biases in participant selection, limiting the applicability of the findings to other settings or groups outside those specifically targeted in the study. Also, the findings may not fully reflect the diverse experiences and health challenges of KPs worldwide.
Strengths of the Study
The study achieved its targeted sample size (1,320 participants), ensuring robust statistical power for analysis.
A well-structured, specifically developed questionnaire allowed the collection of focused and relevant data on willingness to access HIV services.
Providing free self-testing kits and immediate treatment referrals addressed both health and ethical concerns, benefiting participants directly.
Advanced statistical methods enhanced the reliability of findings by accounting for socio-demographic influences on HIV prevalence and service willingness.
Adherence to STROBE guidelines and obtaining ethical approval ensured transparent reporting and ethical integrity throughout the study.
CONCLUSION AND GLOBAL HEALTH IMPLICATIONS
This study offers important insights into the socio-demographic and behavioral traits, HIV prevalence, and factors affecting the willingness to access HIV services among KPs in Kano State, Nigeria. It reveals higher HIV prevalence among MSM and PWIDs compared to FSWs and highlights the influence of sexual practices, drug use, and location on HIV risk and service access. The prevalence of risky behaviors like multiple partners and inconsistent condom use underscores the need for targeted prevention efforts. FSWs are more likely to be willing to access HIV services compared to MSM. While HIV self-testing and PrEP uptake are promising, gaps remain in their effectiveness. Barriers such as stigma, limited access, and insufficient knowledge about services hinder effective HIV service uptake, pointing to the need for more inclusive and comprehensive service delivery models tailored to the specific challenges of KPs in Kano State. Enhancing service accessibility and addressing stigma is essential for reducing HIV transmission and achieving the epidemic control goal in Nigeria by 2030.
Key Messages
1. The overall HIV prevalence among key populations in this study was 10.8%. Men who have sex with men (MSM) and people who inject drugs (PWIDs) showed higher HIV prevalence rates compared to female sex workers (FSWs). 2. Willingness to access HIV preventive services was recorded at 57.7%, influenced by geographical location and sexual practices. Participants from Tarauni were more willing to access services, and those engaging in vaginal sex were more likely to seek preventive services. 3. HIV self-testing had a high uptake of 95.9%, whereas pre-exposure prophylaxis (PrEP) uptake stood at 68.0%. 4. Major barriers included stigma, lack of comprehensive services, and limited knowledge among service providers. Targeted interventions that address these barriers are crucial for improving service uptake and reducing HIV transmission. Enhancing accessibility and tackling stigma are key strategies for achieving epidemic control in Nigeria by 2030.
Acknowledgments
None.
COMPLIANCE WITH ETHICAL STANDARDS
Conflicts of Interest: There was no conflict of interest among the authors. Financial Disclosure: USAID/PEPFAR. Funding/Support: There was no funding for this study. Ethics Approval: The research/study approved by the Institutional Review Board at Kano State Ministry of Health, number NHREC/17/03/2018, dated 17/04/2023. Declaration of Patient Consent: Patient’s consent is not required as there are no patients in this study. Use of Artificial Intelligence (AI)-Assisted Technology for Manuscript Preparation: The authors confirm that there was no use of Artificial Intelligence (AI)-Assisted Technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI. Disclaimer: None.
REFERENCES
- New HIV infections data among key populations: Proportions in 2010 and 2022;. :1-14.
- [Google Scholar]
- Stigma, HIV risk, and access to HIV prevention and treatment services among men who have sex with men (MSM) in the United States: A Scoping Review. AIDS Behav.. 2021;25((11)):3574-3604. [Last accessed 24 Aug 2024]
- [Google Scholar]
- HIV Prevention, Diagnosis, Treatment, and Care for Key Populations 2016 Update. 2018 IEEE Sensors Appl Symp SAS 2018 Proc 2016..
- [Google Scholar]
- Key populations are the future of the African HIV/AIDS pandemic. J Int AIDS Soc.. 2021;24((S3)):e25750.
- [Google Scholar]
- Acceptability and perceptions of HIV oral self-testing across settings: A comparative qualitative study among Dominican and Tanzanian female sex workers. Glob Public Health.. 2022;17((6)):870-84.
- [Google Scholar]
- Awareness of and willingness to use pre-exposure prophylaxis (PrEP) among people who inject drugs and men who have sex with men in India: Results from a multi-city cross-sectional survey. PLoS One.. 2021;16((2)):e0247352.
- [Google Scholar]
- Estimation of HIV prevalence and burden in Nigeria: A Bayesian predictive modelling study. eClinicalMedicine.. 2023;62:102098.
- [Google Scholar]
- Satisfaction with the use of public health and peer-led facilities for HIV prevention services by key populations in Nigeria. BMC Health Serv Res.. 2019;19((1)):856.
- [Google Scholar]
- Pre-exposure prophylaxis and HIV prevention among key populations in Nigeria. Int J MCH AIDS.. 2024;13:e013.
- [Google Scholar]
- Extra-legal policing strategies and HIV risk environment: Accounts of people who inject drugs in Nigeria. Drugs Educ Prev Policy.. 2020;27((4)):312-9.
- [Google Scholar]
- Barriers to accessing antiretroviral treatment among key populations in southwest Nigeria. Cureus.. 2024;16((4)):e59312.
- [Google Scholar]
- Individual and partnership characteristics associated with consistent condom use in a cohort of cisgender men who have sex with men and transgender women in Nigeria. BMC Public Health.. 2021;21((1)):1277.
- [Google Scholar]
- Kano (State, Nigeria) – Population statistics, charts, map and location [Internet]. [cited 2024 Sept 24]. Available from: https://citypopulation.de/en/nigeria/admin/NGA020__kano/
- [Google Scholar]
- Correlates of HIV prevalence among key population in Nigeria. J AIDS HIV Res.. 2021;13((2)):22-7.
- [Google Scholar]
- What is SPSS (Statistical IBM Corp. IBM SPSS Statistics for Windows, Version 28.0. 2021
- [Google Scholar]
- The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for Reporting Observational Studies [Internet];. 2023. [cited]. Available from: https://www.equator-network.org/reporting-guidelines/strobe/
- [Google Scholar]
- Key Population, HIV and human rights in Nigeria: Country context analysis. SSRN Electronic Journal. 2023
- [Google Scholar]
- Correlates of HIV prevalence among key population in Nigeria. J AIDS HIV Res.. 2021;13((2)):22-7.
- [Google Scholar]
- Communication needs for improved uptake of PrEP and HIVST services among key populations in Nigeria: A mixed-method study. AIDS Res Ther.. 2021;18((1)):88.
- [Google Scholar]
- Integrated Biological and Behavioural Surveillance Survey. Nigeria: Federal Ministry of Health;
- [Google Scholar]
- Are quantity surveyors competent to value for civil engineering works? Evaluating QSs’ competencies and militating factors Timothy. J Educ Pract.. 2016;7((16)):9-18.
- [Google Scholar]
- One-stop shop: A community-based antiretroviral therapy (ART) clinic model to improve human immunodeficiency virus (HIV) prevention and treatment cascade for key populations in Nigeria. Open Forum Infect Dis.. 2016;3((suppl_1)):483.
- [Google Scholar]
- Guideline on When to Start Antiretroviral Therapy and on Pre-Exposure Prophylaxis for HIV. :1-76. WHO;
- [Google Scholar]
- Regarding “willingness to pay for HIV prevention commodities among key population groups in Nigeria.”. Glob Health Sci Pract.. 2023;11((1)):e2200445.
- [Google Scholar]
- Key population hotspots in Nigeria for targeted HIV program planning: Mapping, validation, and reconciliation. JMIR Public Health Surveill.. 2021;7((2)):e25623.
- [Google Scholar]
- Breaking barriers: Differential service deliveries for key population community HIV/AIDS services action and response in northern Nigeria. Research Square. 2023 Dec 13:1-12.
- [CrossRef] [Google Scholar]
- Community perspectives on barriers and challenges to HIV pre-exposure prophylaxis access by men who have sex with men and female sex workers access in Nigeria. BMC Public Health.. 2020;20((1)):69.
- [Google Scholar]
- The evolving role of social media in enhancing quality of life: A global perspective across 10 countries. Arch Public Heal.. 2024;82((1)):28.
- [Google Scholar]
- Trends in health communication: Social media needs and quality of life among older adults in Malaysia. Healthcare (Basel).. 2023;11((10)):1455.
- [Google Scholar]





