Translate this page into:
Towards the Elimination of Pediatric HIV: Enhancing Maternal, Sexual, and Reproductive Health Services
✉Corresponding author e-mail: ahairston@pedaids.org
-
Received: ,
Accepted: ,
Abstract
Almost 10 years ago, the United Nations adopted a comprehensive, four-pronged approach for the prevention of mother-to-child transmission of HIV (PMTCT). Despite all four prongs being central to the elimination of pediatric HIV, and the health of the mother being critical to reaching this goal, PMTCT programs have historically focused more attention on preventing HIV transmission from mother to child (prong 3) than on preventing HIV in women of reproductive age (prong 1) and preventing unintended pregnancies in women living with HIV (prong 2). In this commentary, experts from the Elizabeth Glaser Pediatric AIDS Foundation (EGPAF) argue that within the context of efforts to eliminate pediatric HIV, there are many ways to keep women living with HIV alive and at the center of the response to the global epidemic. One of the ways to do this is to enhance maternal and sexual and reproductive health (SRH) services. Within the elimination agenda, integration and linkages between PMTCT and comprehensive SRH services can keep mothers alive and at the center of the response. The commentary highlights some of the foundation's global health work supporting, evaluating and enhancing maternal and SRH services provided to women living with HIV and proposes concrete actions for donors, researchers, policy makers and program implementers to further enhance maternal and SRH services within the context of PMTCT. If keeping women living with HIV is an integral component of the elimination of pediatric HIV agenda, maternal and SRH research, policies and programs need to be strengthened within the context of PMTCT. Donor funding and priorities for PMTCT also need to be more supportive of primary prevention of HIV infection among women of childbearing age and preventing unintended pregnancies among women living with HIV.
Keywords
HIV/AIDS
Elimination of pediatric HIV
PMTCT
Reproductive and sexual health
Maternal health
Introduction
In 2002, the United Nations (UN) adopted a four-pronged approach to the prevention of mother-to-child transmission of HIV (PMTCT). These four prongs represent the cornerstones of comprehensive PMTCT service delivery: primary prevention of HIV infection among women of childbearing age (prong 1), preventing unintended pregnancies among women living with HIV (prong 2), preventing HIV transmission from a woman living with HIV to her infant (prong 3), and treatment, care, and support to women living with HIV, their children, and families (prong 4)[1]. Despite all four prongs being central to the elimination of pediatric HIV, and the health of women being important to reaching this goal, PMTCT programs have historically focused more attention on identifying HIV infection among pregnant women to prevent HIV transmission from mother to child (prong 3) than on preventing HIV in women of reproductive age (prong 1) and preventing unintended pregnancies in women living with HIV (prong 2)[2-4]. Figure 1 shows estimates of new HIV infections among children in 25 countries from 2009 until 2015 based on scenarios in which different combinations of prongs l through 3 are used.[5] These estimates show a projected 79% reduction in new infections by 2015 using a combination of prongs 1,2, and 3 and limiting breastfeeding to 12 months, compared with a 60% reduction using prong 3 alone. The estimates shown in Figure 1 highlight how important prongs l and 2 are in reaching the elimination of pediatric HIV and the estimated impact of increasing antiretroviral coverage for women living with HIV.
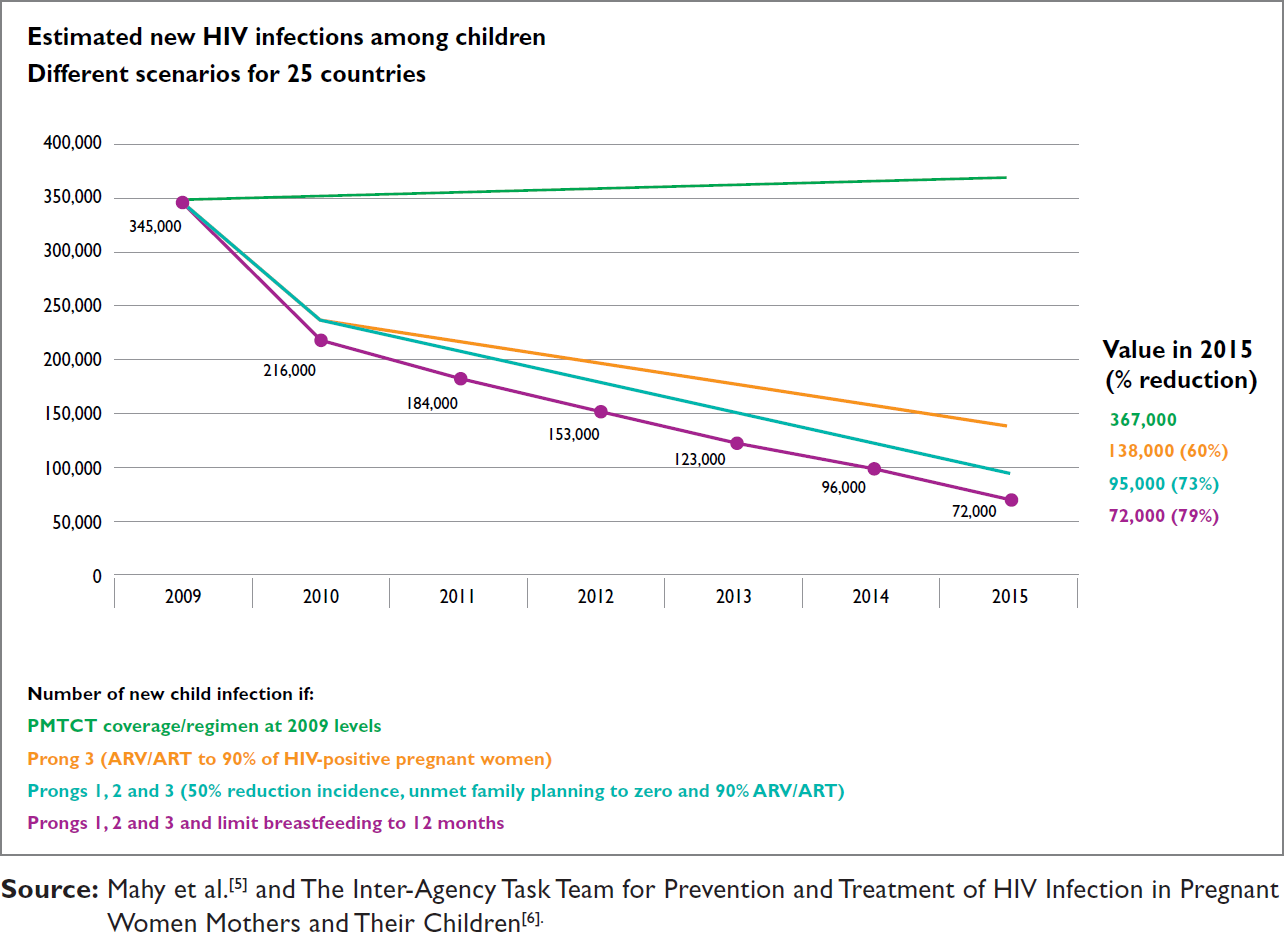
- New HIV Infections Among Children in 25 Countries 2009-2015 By PMTCT Prongs (5-6)
Global Plan Towards Eliminating New HIV Infections
There has been a concerted effort over the past few years to integrate and link (see Box 1 for definitions) maternal and child health (MCH) and sexual and reproductive health (SRH) services with PMTCT services to more comprehensively address all four prongs and increase the focus on women's health. At the UN Special Session on HIV in 2011 (UNGASS 2011), world leaders launched the Global Plan Towards the Elimination of New HIV Infections Among Children by 2015 and Keeping their Mothers Alive (the Global Plan), which outlines how countries can ultimately reach the goal of eliminating pediatric HIV[7]. The Global Plan not only recognizes the importance of maternal health in its title, but the first of the four overarching principles of the Global Plan is to keep women living with HIV at the center of the response. The Global Plan describes this as including but not limited to; mothers and children having access to optimal HIV prevention and treatment regimens based on the latest guidelines, women living with HIV having access to family planning services and commodities as well as the meaningful participation of women in developing and implementing programs to tackle the barriers to services and to work as partners in providing care and address HIV and gender-related discrimination that impedes service access and uptake as well as client retention. There are also defined targets of reducing maternal deaths by 50%, reducing HIV incidence in women aged 15-49 by 50%, and reducing unmet need for family planning among women living with HIV to zero[7]. The Preventing Unintended Pregnancies Strategic Framework has been developed by the Inter-Agency Task Team for Prevention and Treatment of HIV Infection in Pregnant Mothers and Their Children (IATT) in support of national efforts to translate the Global Plan into action[6]. Donors are also calling for HIV services to be inte-grated into SRH services, and encouraging HIV implementers to play active roles in evaluating, coordinating, and leveraging support for broader maternal health service delivery capacity[8]. This shift is applauded, but in order to keep mothers living with HIV at the center of the response, there needs to be an increased focus on maternal health and SRH within the context of PMTCT.
| Box 1. Defining “Linkage” and “Integration” in the Context of MCH and HIV |
| While there are currently no globally accepted standard definitions of these terms, the following working definitions are used in this commentary: |
| Linkages: Strategies that link different kinds of MCH and HIV policies, programs, or services. This can include instituting or strengthening referral systems from one service to another to ensure that services delivered by separate providers at different times are provided within a comprehensive, well-coordinated system. |
| Integration: Strategies that join together different kinds of MCH and HIV policies, programs, or services to ensure provision of comprehensive services. These can include cross-training health providers to offer multiple services in one location or supporting multiple providers to offer different services in one location. |
In this commentary we recognize that, within the context of efforts to eliminate pediatric HIV, there are many ways to keep women living with HIV alive and at the center of the response and argue that one of the ways to do this is to enhance maternal and sexual and reproductive health (SRH) services. We describe that, within the elimination agenda, integration and linkages between PMTCT and comprehensive SRH services can keep mothers alive (as shown in Figure 2 below) and at the center of the response. We also highlight some of the work that the Elizabeth Glaser Pediatric AIDS Foundation (EGPAF) is supporting and evaluating to enhance maternal and SRH services provided to women living with HIV. We conclude by proposing concrete actions for donors, researchers, policy makers and program implementers to further enhance maternal and SRH services within the context of PMTCT.
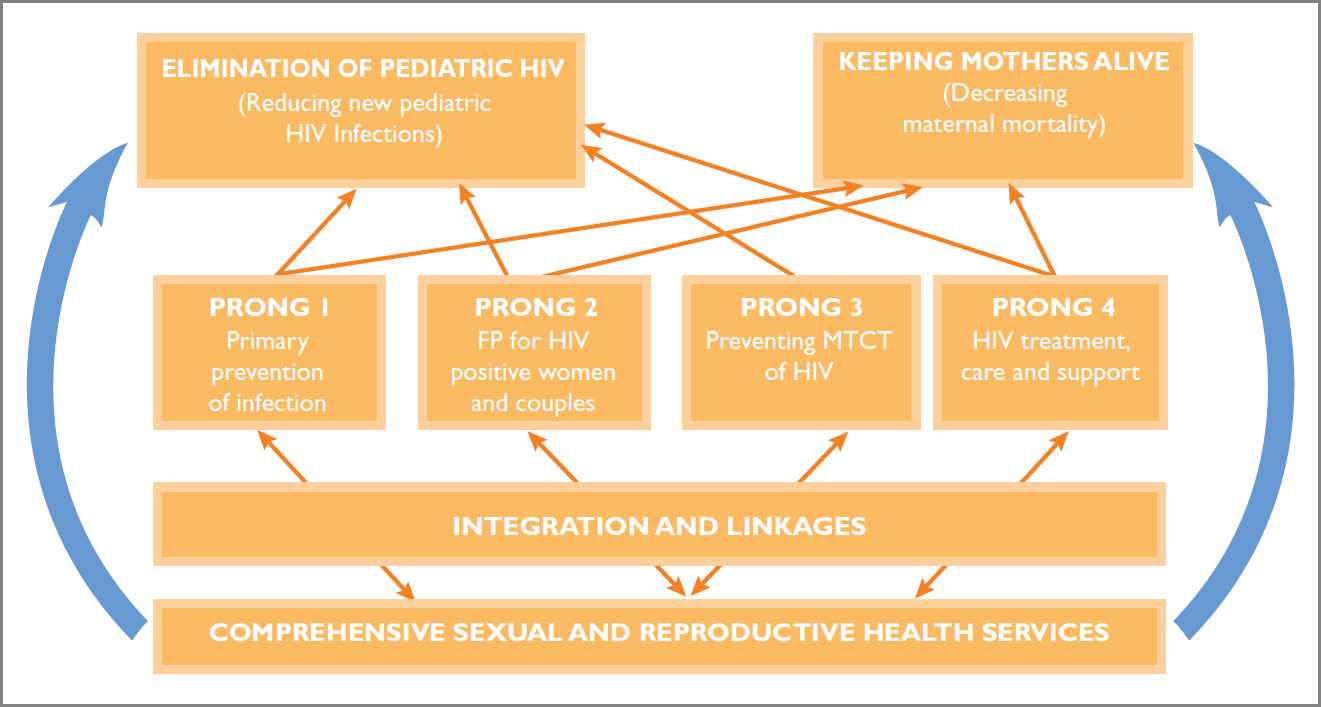
- PMTCT Prongs and Integration and Linkages to SRH Services' Contribution to the Elimination of Pediatric HIV and Keeping Mothers Alive
Background
Maternal Health Must be the Center of Eliminating Pediatric HIV
Promoting maternal health among women living with HIV is central to keeping HIV-positive mothers living with HIV alive and at the center of the agenda to eliminate pediatric HIV. Just 58 countries contribute to 91% of the global burden of maternal mortality; 38 of these countries are in Africa[9] and 17 of these countries are among the 22 focus countries identified in the Global Plan as having the highest estimated numbers of pregnant women living with HIV[7]. In fact, the vast majority of HIV-associated maternal deaths (86%-92%) occur in sub-Saharan Africa and more recent assessments of trends in maternal mortality indicate that HIV has become a leading cause of death during pregnancy and the postpartum period in countries with a high HIV prevalence[10]. The association between skilled attendance at birth and reduced maternal mortality, coupled with strategies a skilled birth attendant (SBA) can use to reduce both the incidence and severity of complications during labor and delivery constitute sufficient grounds to recommend that an SBA be present for every birth[11]. However, many births in resource-limited settings, including settings with a high burden of HIV, are not attended by an SBA. It is estimated that there will be between 130 and 180 million non-SBA births in South Asia and sub-Saharan Africa between 201 1 and 2015, and that 90% of these will occur in rural areas[12].
Family planning addresses needs of women within the context of PMTCT because it allows women and men to attain their desired number of children and determine the spacing of pregnancies[13]. Although many HIV-positive women and couples wish to manage their reproductive options, evidence suggests that unmet need for family planning may be higher among HIV-positive women than the general population[14]. Studies in Cote d'Ivoire, Rwanda, South Africa, and Uganda have found levels of unintended pregnancies among HIV-positive women ranging from 51% to 91%.[15-18]. Halperin and colleagues conducted an analysis of data from the 2008 UNAIDS report on the AIDS epidemic that suggests family planning is cost-effective for HIV prevention as well as for preventing pregnancies among women living with HIV[2]. The direct health benefits of meeting the need for both family planning and maternal and newborn health services (i.e., a continuum of care to help couples plan their pregnancies and provide timely antenatal, delivery, and postpartum services, including urgent care for complications that arise among women and newborns) would lead to health system improvements that could provide lifesaving care to women and their newborns while at the same time strengthening services for other urgent medical needs[19].
Linking Reproductive Age Women to Sexual and Reproductive Health Services in Developing Countries
Linking HIV-positive women of reproductive age in resource-limited settings and their partners to SRH services is not only an important part of keeping mothers at the center of the agenda to eliminate pediatric HIV, but is also key to ensuring that women remain alive and healthy. A systematic review conducted by WHO and several other agencies in 2009 found that bi-directional linkages between SRH-and HIV-related policies and programs can lead to better access among people living with HIV to SRH services that are tailored to their needs, reduction of HIV-related stigma and discrimination, and enhanced program effectiveness and efficiency[20]. SRH linkages that are particularly relevant to the health needs of women within the context of PMTCT include linkages to syphilis and cervical cancer screening. In addition to the morbidity and mortality associated with syphilis and congenital syphilis, co-infection of syphilis and HIV among pregnant women is a significant risk factor for vertical HIV transmission[4,7]. It should also be noted that 83% of new cases of cervical cancer and 85% of deaths from the disease occur in resource-limited settings[21]. A study in Kenya found that young women with cervical cancer were more often HIV infected than women with fibroids of the same age group[22].
EGPAF'S Commitment to Maternal and Sexual and Reproductive Health
A variety of organizations and institutions have committed to, and are engaged in addressing maternal health and SRH within the context of PMTCT. It should however be noted that one of the key challenges related to increasing focus on maternal health and comprehensive SRH services within the elimination of pediatric HIV agenda is that implementing partners working in these different areas may have difficulty integrating their programs because US-funded reproductive health and HIV projects and programs are often separated, with programs using very different results and reporting mechanisms.
EGPAF seeks to prevent pediatric HIV infection and to eliminate pediatric HIV through research, advocacy, and prevention and treatment programs. As such, EGPAF is committed to promoting integration and linkage of SRH and HIV services in all the countries that it supports (see Figure 3 below), and to promoting these approaches through its close partnerships with ministries of health and a variety of national and international public health organizations and institutions. EGPAF:
Favors policies that affirm that all women and men, regardless of HIV status, have the right to determine the number and spacing of their children;
Favors increasing access to prevention, screening, and treatment of sexually transmitted infections (STIs) as part of a comprehensive package of reproductive health services;
Favors increasing access to high-quality, safe, and appropriate obstetric care and services to improve maternal and child health and survival; and
Favors increasing the availability of high-quality, safe, and comprehensive care for all women accessing services, and places a special emphasis on ensuring that women living with HIV receive the antenatal care (ANC) and HIV services they need for their own health and the health of their children.

- Countries where EGPAF Works in Sub-Saharan Africa
A variety of country-specific efforts point to EGPAF's growing involvement in this important area. EGPAF, with support from PEPFAR (The US President's Emergency Plan for AIDS Relief) and various other donors, works in a variety of countries to support increased facility-based deliveries assisted by Skilled Birth Attendants (SBAs), earlier and more frequent antenatal care visits, primary prevention of HIV among pregnant women, provision of family planning (FP) at all points across the continuum of care, and provision of HIV care and treatment (including long-term antiretroviral therapy) for HIV-positive women. Some specific examples of how EGPAF links women to maternal health and SRH services are highlighted below.
In close collaboration with ministries of health in Tanzania, Cameroon and Lesotho, EGPAF is supporting the scale-up of cervical cancer screening and the roll-out of the human papillomavirus (HPV) vaccine though funding from USAID (in Tanzania and Lesotho) and CDC (in Cameroon). In Lesotho, EGPAF is working with the Ministry of Health and Social Welfare (MOHSW) to establish a center of excellence for women living with HIV at the Senkatana Center in Maseru. The center offers screening for cervical cancer alongside HIV care and treatment services. EGPAF will be training health care workers and students in the screening and prevention of cervical cancer. EGPAF and other partners have also worked with the MOHSW in developing national HPV guidelines to support the national roll-out of the vaccine.
With support from the World Health Organization (WHO) Special Program for Research and Training in Tropical Diseases' Sexually Transmitted Disease Diagnostic Initiative and the London School of Hygiene and Tropical Medicine, EGPAF conducted a study in 2009/2010 that found that introducing rapid syphilis testing for pregnant women at antenatal clinics (ANC) sites offering PMTCT services in Zambia and Uganda is feasible, accepted by health-care providers, and cost effective. The findings of the study have informed guideline development, training of health care workers, and the roll-out of these services in both Zambia and Uganda. [23-24]
EGPAF's Integration of HIV and MCH Services in Developing Countries
EGPAF has a number of on-going studies exploring integration of HIV and MCH services. In Tanzania, the United Nation's Population Fund (UNFPA) has supported EGPAF to implement and evaluate an FP/HIV integration model in Tanzania's Shinyanga Region. The study looks at the co-location of FP (i.e., screening, counseling, and commodities) and HIV care and treatment services at local Care and Treatment Centers (CTC). In Kenya, the Gates Foundation supported EGPAF to conduct an observational prospective cohort study that compared infant follow-up results, when services for HIV-exposed children were provided within Maternal and Child Health (MCH) clinics or in specialized HIV Comprehensive Care Clinics (CCC), in two District hospitals in Kenya.[25] HIV services integrated in MCH in one district hospital led to better follow-up of HIV-exposed infants than in a similar hospital with services provided separately in a CCC.
Increasing Focus on Maternal And Sexual Reproductive Health Within the Pediatric HIV Elimination Agenda
Those involved with HIV, MCH, and SRH program implementation at a variety of levels can take concrete actions to enhance maternal and SRH in the context of PMTCT. Recommendations for various stakeholders positioned to lead these efforts are as follows:
Donors
Increase funding for development, evaluation and scale-up of program models aimed at linkage and integration of FP, SRH, MCH, and HIV services.
Ensure that funding for PMTCT programs supports comprehensive health services for pregnant women and linkages to SRH, FP and MCH services.
Researchers
Evaluate the effectiveness, efficiency, and impact of integrated programs[4].
Adopt the recommendations contained in Pregnancy Intentions of HIV-Positive Women:
Forwarding the Research Agenda-a report issued by the Harvard School of Public Health Program on International Health and Human Rights following a March 2010 conference and symposium-with a specific focus on the following recommendations[26]:
○ Conduct additional studies to assess HIV-positive women's contraceptive needs, including identifying barriers to acquiring and using various forms of contraception to ensure availability and acceptability
○ Conduct studies comparing the appropriateness and effectiveness of various service delivery models, including those that integrate HIV care with SRH services.
Policy Makers
Ensure that strategies and activities addressing the first two prongs of PMTCT are included (with appropriate resource allocations) in the development and implementation of national plans and strategies for the elimination of pediatric HIV.
Ensure that ministries of health, donors, and implementing partners support and adopt the Preventing Unintended Pregnancies Strategic Framework that supports the Global Plan[27].
Program Implementers
-
Incorporate evidence-informed approaches to maternal and SRH service linkages within PMTCT programs. A review of the evidence by Gay and colleagues found that successful and promising interventions to improve the SRH and rights of women living with HIV include:
○ providing contraceptives and family planning counseling as part of HIV services;
○ ensuring early postpartum visits provide family planning and HIV information and services;
○ providing youth-friendly services;
○ providing information and skills building support to reduce unprotected sex;
○ supporting disclosure to increase safer sexual behavior;
○ integrating cervical cancer screening and treatment into HIV care;
○ promoting condom use for dual protection against pregnancy and HIV to make condoms more acceptable; and
○ providing antiretrovirals and counseling to increase HIV prevention behavior[28].
Through the development of robust indicators, rigorously monitor and evaluate integrated programs during all phases of implementation to improve current and future programs.
Ensure that key reproductive and maternal services (such as voluntary family planning, including preconception planning; prevention and management of gender-based violence; and STI management) are integrated with HIV services at the national, sub-national, and facility level to the largest extent possible.
Conclusions
The launch of the Global Plan and renewed momentum around eliminating pediatric HIV is a unique opportunity to ensure that women remain healthy and alive within efforts to eliminate pediatric HIV. This will require that PMTCT research, policies, and programs are linked with SRH and maternal health. To realize the full impact of such changes, implementing partners must work together to explore and make use of synergies between HIV and SRH programs to address the and eventually realize the goal of eliminating diverse health needs of women and their partners pediatric HIV.
The positions summarized in this commentary were developed by members of the Foundation's technical advisory group on MCH/ HIV linkages and integration (the M-TAG), which was made up of Foundation country and global staff. These positions are intended to guide a consistent Foundation-wide approach and framework for addressing this issue and do not supersede the national policies and guidelines of the countries in which the Foundation works.
References
- Guidance on global scale-up of the prevention of mother to child transmission of HIV: Towards universal access for women, infants, and young children and eliminating HIV and AIDS among children. 2007.
- [Google Scholar]
- Benefits and costs of expanding access to family planning programs to women living with HIV. AIDS. 2009;23(Suppl 1):S123-30.
- [CrossRef] [PubMed] [Google Scholar]
- The contribution of family planning towards the prevention of vertical HIV transmission in Uganda. PLoS One. 2009;4(11):e7691.
- [CrossRef] [PubMed] [Google Scholar]
- Reproductive choices for women with HIV. Bulletin of the World Health Organization. 2009;87(11):833-839.
- [CrossRef] [PubMed] [Google Scholar]
- What will it take to achieve virtual elimination of mother-to-child transmission of HIV? An assessment of current progress and future needs. Sexually Transmitted Infection. 2010;86(Suppl 2):ii48-55.
- [CrossRef] [PubMed] [Google Scholar]
- The Inter-Agency Task Team for Prevention and Treatemtnt of HIV Infection in Pregnant Women Mothers and Their Children. 2011. Preventing HIV and Unintended Pregnancies: Strategic Framework 2011-2015. Available from: http://www.unfpa.org/webdav/site/global/shared/documents/publications/2012/PreventingHIVUnintendedPregnanciesSF2011_2015.pdf
- [Google Scholar]
- Global Plan Towards Elimination of New HIV Infections Among Children by 2015 and Keeping Mothers Alive; 2011 [cited 2011 June] Available from: http://www.unaids.org/en/media/unaids/contentassets/documents/unaidspublication/2011/20110609_JC2137 Global-Plan-Elimination-HIV-Children_en.pdf
- [Google Scholar]
- Technical Considerations Provided by PEPFAR Technical Working Groups for the FY 2010 Country Operational Plan. 2009. Available from: http://www.pepfar.gov/documents/organization/169737.pdf
- [Google Scholar]
- The State of the World's Midwifery 2011; May 14,2012. Available from: http://www.unfpa.org/sowmy/resources/docs/mainreport/en_SOWMR Full.pdf
- [Google Scholar]
- Understanding Methods for Estimating HIV- Associated Maternal Mortality. Journal of Pregnancy. 2012;2012:958262.
- [CrossRef] [PubMed] [Google Scholar]
- Improving Birth Outcomes: Meeting the Challenge in the Developing World. In: Committee on Improving Birth Outcomes. Washington DC: National Academies Press; 2003.
- [Google Scholar]
- How many births in sub-Saharan Africa and South Asia will not be attended by a skilled birth attendant between 2011 and 2015? BMC Pregnancy and Childbirth. 2012;12:4-12.
- [CrossRef] [PubMed] [Google Scholar]
- Family planning: fact sheet. 2011. Geneva: World Health Organization; [May 14,2012]. Available from: http://www.who.int/mediacentre/factsheets/fs351/en/index.html
- [Google Scholar]
- Reaching the underserved: family planning for women with HIV. Studies in Family Planning. 2010;41(2):125-128.
- [CrossRef] [PubMed] [Google Scholar]
- Pregnancy, pregnancy desires, and contraceptive use among HIV-infected women: Findings from a survey of women enrolled in PMTCT in Rwanda. In: Third Annual Pediatric Conference on the Infected and Affected by HIV and AIDS. 2007.
- [Google Scholar]
- Ditrame Study Group. Contraceptive use, protected sexual intercourse and incidence of pregnancies among African HIV- infected women. DITRAME ANRS 049 Project, Abidjan 1995-2000. International Journal of STD and AIDS. 2002;13(7):462-8.
- [CrossRef] [PubMed] [Google Scholar]
- Reproductive intentions and outcomes among women on antiretroviral therapy in rural Uganda: a prospective cohort study. PLoS One. 2009;4(1):e4149. Epub2009 Jan 8
- [CrossRef] [PubMed] [Google Scholar]
- Depression among pregnant rural South African women undergoing HIV testing. Journal of the American Medical Association. 2006;295(12):1376-1378.
- [CrossRef] [PubMed] [Google Scholar]
- Adding It Up: The Costs and Benefits of Investing in Family Planning and Maternal and Newborn Health. 2009
- [Google Scholar]
- Sexual & Reproductive Health and HIV Linkages: Evidence Review and Recommendations. 2009. Available from: http://www.unaids.org/en/media/unaids/contentassets/dataimport/pub/agenda/2009/2009 linkages evidence review en.pdf
- [Google Scholar]
- Cervical cancer: the Sub-Saharan African perspective. Reproductive Health Matters. 2008;16(32):41-49.
- [CrossRef] [PubMed] [Google Scholar]
- Impact of HIV infection on invasive cervical cancer in Kenyan women. AIDS. 2003 Sep. 5;17(13):1963-1968.
- [CrossRef] [PubMed] [Google Scholar]
- Introduction of Rapid Syphilis Testing within Prevention of Mother-to-Child Transmission of HIV Programs in Uganda and Zambia: A field acceptability and feasibility study. 6th IAS Conference on HIV Pathogenesis, Treatment and Prevention. 2011.
- [Google Scholar]
- Introduction of Rapid Syphilis Testing within Prevention of Mother-to-Child Transmission of HIV Programs in Uganda and Zambia: A field acceptability and feasibility study. Journal of Acquired Immune Deficiency Syndrome 2012 Jul 19 [Epub ahead of print]
- [CrossRef] [PubMed] [Google Scholar]
- Provision of Services and Care for HIV- Exposed Infants: A Comparison of Maternal and Child Health Clinic and HIV Comprehensive Care Clinic Models. Journal of Acquired Immune Deficiency Syndrome, 2012 Sep. 1;61(1):83-89.
- [CrossRef] [PubMed] [Google Scholar]
- The Pregnancy Intentions of HIV-Positive Women: Forwarding the Research Agenda - Conference Report. In: Pregnancy Intentions of HIV-Positive Women. 17-19,2010
- [Google Scholar]
- Preventing HIV and unintended pregnancies: strategic framework 2011-2015. 2011. Available from: http://www.ippf.org/NR/rdonlyres/9C6DE8AA-ICI6-48FB-B212-A64FE3A0F2BF/5932/PreventingHIVandun intendedpregnanciesstrategicfram.pdf
- [Google Scholar]
- What works to meet the sexual and reproductive health needs of women living with HIV/AIDS. Journal of the International AIDS Society. 2011;14:56.
- [CrossRef] [PubMed] [Google Scholar]





