Translate this page into:
Prevalence of Intestinal Parasitic Infections and their Association with Nutritional Status of Rural and Urban Pre-School Children in Benue State, Nigeria
Corresponding author email: organicjev@yahoo.com
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Background and Objectives:
Intestinal parasitic infections are highly prevalent in developing countries, contributing to high incidence of malnutrition and morbidity. This study aimed to find the prevalence of intestinal parasitic infections and their association with nutritional status of children in Benue State, Nigeria.
Methods:
A cross sectional study conducted from January-June 2016, among 418 school children under-5 years of age. Anthropometric data, height-for-age, weight-for-height, and weight-for-age Z-scores from each child and fecal samples were collected and screened for intestinal parasites using standard laboratory methods.
Results:
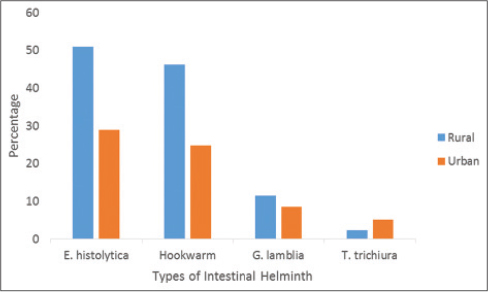
Among the intestinal parasitic infections detected, the prevalence of E. histolytica was higher (51.0% and 29.0%) than all other parasites encountered in rural and urban pupils (P<0.05). Other parasites were Hookworm (46.2% and 24.8%); G. lamblia (11.5% and 8.6%); and T. trichiura (2.4% and 5.2%). The prevalence of stunting (HAZ<-2), in rural and urban pupils were 43.8% and 32.9%; 64.4% and 39.0% rural and urban pupils were underweight (WAZ<-2), while 30.3% and 24.3% were wasted (WHZ<-2). Infected children had significantly (P<0.05) higher z-scores than the uninfected children.
Conclusion and Global Health Implications:
Benue State is among the Nigerian states with the highest burden of tropical diseases with a current plan of elimination implemented through mass drug administration. This study identify/evaluate some essential information that will support the planning and implementation of the State’s ongoing efforts.
Keywords
Intestinal Parasites
Nutritional Satus
Preschool Children
Rural-urban
Benue State-Nigeria
1. Introduction
Hundreds of thousands of avoidable deaths are caused each year by parasitic infections, particularly the intestinal helminthes, and these infectious diseases affect the nutritional status of most children under the age of five.[1] It has been estimated to affect about 3.5 billion people globally and caused morbidity in approximately 450 million people.[1] Developing countries are the most affected, majority being school children because of their typical hand-mouth activity, uncontrolled fecal activity and their immature immune systems. The climatic conditions in this part of the world favor the development and survival of these parasites, the high prevalence in a region results to infection and diseases that are the immediate causes of malnutrition and death in young children.[2] Records show that a global estimate of 162 million under-five years old children are documented to be stunted, 99 million underweight and 51 million wasted.[3] A silent emergency already exists in Nigeria, as the country has extremely poor nutritional indices: stunting 37%, underweight 29% and wasting 18%.[4]
Diarrhea is the second leading cause of death among children under five in Nigeria after malaria.[5] E. histolytica, G. lamblia, N. americanus, A. doudenale, hookworm, ascariasis and trichuriasis are the other common intestinal parasitic infections in Benue State, Nigeria.[6] The incidence of the disease varies greatly with seasons and a child’s age; the youngest children are most vulnerable, due to poor environmental sanitation and contamination of water.[7] Malnutrition and intestinal parasitic infections are common public health problems of children in Nigeria. These parasitic infections have detrimental impact on host nutritional status in several ways, they can depress appetite and food intake, compete for micronutrients, or blood loss resulting in the loss of iron, diarrhea, vomiting, dehydration, weight loss and growth retardation, fever, school attendance, physical activity and cognitive performance of school age children.[8-11] Thus, the objective of this study was to determine the prevalence of intestinal helminthic infections and assess the nutritional status of pre-school aged children in communities of Gboko Local Government Area of Benue State in Nigeria’s Middle Belt region.
2. Methods
2.1. Study sites
The present research was a cross sectional study conducted from January-June 2016, among 418 school children under the age of five living in Gboko. The area covers a land mass of 2,264 square kilometers with a population of 361,325 people according to 2006 Nigeria census. On the geo-political map of Nigeria, the area is located between Latitude 630° and 810° north of the Equator and Longitudes 8° and 10° east of the Greenwich Meridian.
2.2. Subjects
A multistage sampling was used to select samples. The 17 council wards in Gboko Local Government Area (LGA) were clustered into districts. Five (5) council wards from the LGA were selected randomly. A list of certified primary schools was obtained from Benue State Ministry of Education, the schools in the randomly selected council ward (Gboko-north, Igorov, Mbadim, Ukpekper, Mbankur) were further clustered into urban and rural primary schools. These schools were further clustered into private and public schools in both urban and rural areas. In all, 4 schools were selected from a council ward (a private & a public school in both rural and urban areas of each council ward), making a total of 20 schools. Entirely, 422 pupils both boys and girls ranging from ages of 2-5 years were randomly selected. The actual size of those that participated in the research were 418 with 208 children from rural areas and 210 children from urban areas.
2.3. Ethical clearance
Before the commencement of the research, permission was obtained from the headmasters of all the schools including the pupil’s parents/guardian. The study protocol was approved by the Benue state Ministry of Health’s ethical committee with the reference number MED/156/VOL.1/56.
2.4. Anthropometric measurement
Anthropometric measurements such as height and weight were taken by a set of trained investigators following the internationally accepted standard techniques.[12] Height and weight measurements were recorded to the nearest 0.1cm and 0.5kg respectively. Weight-for-height (WHZ), which was used to identify wasting in children, was computed for all boys and girls of ages 2-5 years. Height-for-age (HAZ) and weight-for-age (WAZ) ratios were used to diagnose children with stunted and underweight growth (<-2SD) respectively.[3,13]
2.5. Parasitological examination
Stool samples were collected in labeled screw capped plastic containers for parasitological examination within one hour of collection. All stool samples were re-examined microscopically using the formal ether concentration technique which is considered to be the most-sensitive method for most intestinal helminthes.[14]
2.6. Data analysis
SPSS windows version 21.0 was used for data analysis. Anthropometry indices were computed using the calculator mode of anthropometry calculating software program Epi Info version 6. Wasting, stunting and underweight were defined as Z score values of less than -2SD (Standard Deviation). Descriptive and inferential statistical tests were performed. The significance of the differences in frequency distribution was tested by using chi-square analyses. P-values less than 0.05 were considered statistically significant.
3. Results
The result presented below is the data for 418 pupils (208 rural and 210 urban) who returned stool sample and their anthropometric data were obtained. There were 103 males and 105 females for rural areas and 106 males and 104 females for urban areas. The subjects were grouped between 2-5 years with a mean age of 4.22 ± 0.81 years. Table 1 summarizes the prevalence of intestinal parasite in the pupils. Prevalence of infection was significantly (P<0.05) higher among the rural pupils than among the urban pupils. Prevalence of E. histolytica was higher in both rural (51.0%) and urban areas (29.0%) than all other parasites encountered in the study areas (P<0.05). Other parasites found in both rural and urban areas were Hookworm (46.2% and 24.8%); G. lamblia (11.5% and 8.6%); and T. trichiura (2.4% and 5.2%). The subjects co-infected with mixed species of parasites were (63.5% and 40.0%) in rural and urban pupils respectively (Figure 1).
| Parasites | Rural children No (%) infected n=208 | Urban children No (%) infected n=210 | Total No (%) children infected n=418 |
|---|---|---|---|
| E. histolytica | 106 (51.0) | 61 (29.0) | 167 (40) |
| Hookworm | 96 (46.2) | 52 (24.8) | 148 (35.4) |
| G. lamblia | 24 (11.5) | 18 (8.6) | 42 (10.0) |
| T. trichiura | 5 (2.4) | 11 (5.2) | 16 (3.8) |
| Mixed infection | 132 (63.5) | 84 (40.0) | 216 (51.7) |
- Prevalence of intestinal parasites among children in rural and urban communities
There were significant relationships between intestinal parasitic infection and school types as well as the community (Table 2). Male and female pupils were equally likely to get a parasitic infection. The public school pupils were more infected with the parasites than the private school pupils (66.4% and 36.2%) and the pupils from the rural settings were more infected than those from the urban settings (63.5% and 39.5%).
| Variables | Helminthic Infection (%) Yes No |
Chi-square | p-value | |
|---|---|---|---|---|
| Gender | ||||
| Male (209 | 114 (54.5) | 95 (45.5) | 1.62 | P>0.05 |
| Female (209) | 101 (48.3) | 108 (51.7) | ||
| Community | ||||
| Rural (208) | 132 (63.5) | 76 (36.5) | 23.96 | P<0.05 |
| Urban (210) | 83 (39.5) | 127 (60.5) | ||
| School type | ||||
| Public (211) | 140 (66.4 | 71 (33.6) | 37.94 | P<0.05 |
| Private (207 | 75 (36.2) | 132 (63.8) | ||
P<0.05 Statistically Significant
Table 3 shows associations between the various risk factors and intestinal parasitic infections among the school pupils. Among all the potential risk factors explored, pupils from rural communities had the highest level of some risk factors that could easily result to infection. A total of 64.4% use well as their source of drinking water as against 29.0% in urban, 41.8% pupils in rural settings use pit latrine whereas only 14.3% in urban uses pit latrine, 38.0% pupil live in a house with sand as their type of floor as against 0.0% in urban areas and more importantly only 13.0% of the pupils in the rural area had been de-wormed in the 6 months preceding the study, 42.8% were not, while the remaining 44.2% had never been de-wormed. But in urban setting, 44.8% had been dewormed, 30.0% had not, and only 25.2% were never dewormed. The habit of washing hands after toilet use posed a problem in both rural and urban settings, 15.4% in rural settings still wash their hands while only 26.7% in urban settings do wash their hands after toilet use.
| Variables | Rural n=208 | % | Urban n=210 | % |
|---|---|---|---|---|
| Drink water source | ||||
| Tap | 74 | 35.6 | 149 | 71.0 |
| Well | 134 | 64.4 | 61 | 29.0 |
| Type of toilet facility | ||||
| Water closet | 69 | 33.2 | 164 | 78.1 |
| Pit latrine | 87 | 41.8 | 30 | 14.3 |
| Bush | 52 | 25.0 | 16 | 7.6 |
| Type of floor | ||||
| Tiles | 26 | 12.5 | 105 | 50.0 |
| Carpet | 40 | 19.2 | 26 | 12.4 |
| Cement | 63 | 30.3 | 79 | 37.6 |
| Sand | 79 | 38.0 | 0 | 0.0 |
| De-worm last 6 months | ||||
| Yes | 27 | 13.0 | 94 | 44.8 |
| No | 89 | 42.8 | 63 | 30.0 |
| Never | 92 | 44.2 | 53 | 25.2 |
| Wash hands after toilet use | ||||
| Yes | 32 | 15.4 | 56 | 26.7 |
| No | 176 | 84.6 | 154 | 73.3 |
The overall prevalence of nutritional indicators below -2SD is presented in Table 4, the prevalance of stunting in rural and urban pupils were 43.8% and 32.9%; 64.4% and 39.0% rural and urban pupils were underweight while 30.3% and 24.3% were wasted. Rural children were significantly (P<0.05) more malnourished than urban children. Only E. histolytica, Hookworm and G. lamblia were significantly (P<0.05) associated with low height-for-age (stunting), weight-for-height (wasting) and weight-for-age (underweight).
| Variables | Rural | Urban | ||||
|---|---|---|---|---|---|---|
| HFA | WFA | WFH | HFA | WFA | WFH | |
| Stunting | Underweight | Wasting | Stunting | Underweight | Wasting | |
| No. examined | 208 | 208 | 208 | 210 | 210 | 210 |
| No.below -2SD | 91 | 134 | 63 | 69 | 82 | 51 |
| % below -2SD | 43.8% | 64.4% | 30.3% | 32.9% | 39.0% | 24.3% |
| Mean Z-score | −1.869 | −2.06 | −1.72 | −1.69 | −1.81 | −1.65 |
| SD | 0.64 | 0.73 | 0.75 | 0.68 | 0.78 | 0.71 |
| Sex | ||||||
| No.(%) of boys Below -2SD | 50 (48.5) | 74 (71.8) | 36 (35.0) | 40 (37.7) | 44 (41.5) | 23 (21.7) |
| No. (%) of girls Below -2SD | 41 (39.0) | 60 (57.1) | 27 (25.7) | 29 (27.9) | 38 (36.5) | 28 (26.9) |
4. Discussion
Generally intestinal parasitic infection are dangerous disease causing agents among school children ultimately resulting to malnutrition.[2] The prevalence of intestinal parasitic infection in this study (63.5%) in rural and (40.0%) in urban is lower (80.9% rural and 51.4% urban) than what was found by Opara et al in Eastern Nigeria,[2] and also the 75.7% found by Wosu et al in South Eastern Nigeria,[15] but higher than the 30.6% as reported by Adekunle et al, 45.5% that was reported by Emeka,[16] and the 52.0% reported by Adefioye et al.[17] These results evidently showed a high level of intestinal parasitic infection especially among the rural dwellers. Such prevalence has been attributed to ignorance, poverty, poor environmental and personal hygiene, shortages of clean potable water and indiscriminate defecation as most vegetable farmers use excreta as manure which is a veritable source of infection since children and their mothers often go to the farm to tender to the vegetables.[18] Despite all these factors, the relatively high prevalence connotes continuous infection, re-infection and transmission of intestinal parasites. The commonest was the co-infection of E. histolytica, hookworm and G. lamblia. No individual had up to four parasites.
This present study recorded a high degree of malnutrition among the children investigated for intestinal parasitic infections. 64.4% of pupils in rural areas were found to be underweight whereas 39.0% in urban were underweight. This rate is similar to what was reported by Goon et al,[19] he reported 43% to be underweight in Benue State and Emeka[18] who reported 57.9%. Higher rates of underweight were however reported by Adekunle et al,[20] in rural and semi-urban communities of Osun State who reported 70.0% and 54.7% in the year 2015. These findings agree with the publication of other researchers.[8, 10] The high rate (>=30%) of stunting and underweight recorded in this study was due to high prevalence of E. histolytica, hookworm, G. lamblia and T. Trichiura. It has been documented by Crompton and Neisheimthat growth and development during childhood could be diminished by ascariasis, trichiuriasis and hookworm infection.[21]
Intestinal parasitic infections can cause vomiting, diarrhea, anorexia, abdominal pain and nausea that may result in reduced food intake, thereby further reducing nutrient availability hence contributing to undernutrition[22] therefore the government and other Non-governmental organizations (NGOs) involved in development should introduce adequate strategies to crisscross on personal and environmental hygiene, especially for the rural dwellers. There is also need for regular deworming of school-age children, especially those living in the rural communities. They should also design relevant policies or review existing ones in order to savage the situation because a greater proportion of the population still live in rural communities.[23]
5. Conclusions and Global Health Implications
The prevalence of intestinal helminthic infection in this study was high and was significantly associated with the nutritional status of the respondents. It was such that children with intestinal parasitic infections were more malnourished when compared with those with no infection. There is need for regular de-worming of preschool-age children, especially those living in the rural communities. Reducing the prevalence of parasitic infections in school children, may be of tremendous benefit on child growth, development and educational outcome.
Compliance with Ethical Standards
Acknowledgements
We express our sincere appreciation to the head-teachers, parents, pupils, for their approval and cooperation throughout the duration of the study.
References
- Informal consultation on intestinal helminthes infection. Geneva, Switzerland: WHO; 2000. p. :16-18.
- The Impact of Intestinal Parasitic Infections on the Nutritional Status of Rural and Urban School-Aged Children in Nigeria. International Journal of MCH and AIDS. 2012;1(1):73-82.
- [Google Scholar]
- The Use and Interpretation of Anthropometry. Report of a WHO Expert Committee. Geneva, Switzerland: World Health Organization; 2012. p. :2-5.
- Country Progress Report – Nigeria 2013:56.
- 2009a. UNICEF/WHO State of the World Children 2008-Child Survival. :89-93. Available in http://www.unicef/who
- Relationship of intestinal parasitic infections and malnutrition among school children in Makurdi, Benue State, Nigeria. The Internet Journal of Epidemiology. 2013;7(1):20-24.
- [Google Scholar]
- Malnutrition and parasitic helminth infections. Journal of Parasitology. 2000;12(1):573-595.
- [Google Scholar]
- Linear Growth Retardation in Zanzibari School Children. American Society for Nutritional Sciences. 1997;12(7):10-19.
- [Google Scholar]
- The Effect of Intervention Methods on Nutritional Status and Cognitive Function of Primary SchoolChildren Infected with Ascarislumbricoides. American Journal of Tropical Medicine and Hygiene. 2014;5(9):791-795.
- [Google Scholar]
- Compliance and Absenteeism in Schoolchildren: Implications for Helminth control. Transaction of the Royal Society of Tropical Medicine and Hygiene.2015. ;8(7):148-152.
- [Google Scholar]
- The Use and Interpretation of Anthropometry. Report of a WHO Expert Committee. Geneva, Switzerland: World Health Organization; 2012. p. :72-77.
- Anthropometric indicators measurement guide. Washington D.C: Food and Nutrition Technical Assistance (FANTA) Project; 2003. p. :67-99.
- Basic Laboratory Methods in Medical Parasitology. Geneva, Switzerland: World Health Organization; 1991. p. :45-69.
- The Prevalence of Intestinal Parasitic Infections among School Children in a Tropical Rainforest, Community of Southern Nigeria. Journal of Animal Science advances.2014. ;4(8):1004-1008.
- [Google Scholar]
- Prevalence of Intestinal Helminthic Infection among School Children in Ruraland Semi Urban communities in Nigeria. Journal of Dental and Medical Sciences. 2015;6(5):23-29.
- [Google Scholar]
- Intestinal Helminthiasis among School Children in IlieOsun State, Sierra Leone Journal of Biomedical Research. . 2011;3(1):36-42.
- [Google Scholar]
- Intestinal Parasites among School Children in Soba and Igabi Local Government Area of Kaduna State, Nigeria. Nigerian Journal of Parasitology. 2013;1(3):39-42.
- [Google Scholar]
- Anthropometrically Determined Nutritional Status of Urban Primary School children in Makurdi, Nigeria. Benue State Ministry of Public Health. 2011;11(1):769.
- [Google Scholar]
- Intestinal Parasites and Nutritional Status of Nigerian Children. African Journal of Biomedical Research. 2015;4(5):115-119.
- [Google Scholar]
- Nutritional Impact of Intestinal Helminthiasis during the Human Life Cycle. Annual Review of Nutrition. 2002;2(2):55-59.
- [Google Scholar]
- Study on Prevalence and Nutritional Effect of Helminthic Infection in Rural Children in Nigeria. Journal of Nigerian Medical Practitioners. 2008;54(1):16-20.
- [Google Scholar]
- Legal Notice on Publication of 2006 Census Final Results. Vol 96. 2009. p. :B1-42.





