Translate this page into:
Place of Residence and Inequities in Adverse Pregnancy and Birth Outcomes in India
∗Corresponding author email: deepa.dongarwar@bcm.edu
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Background and Objectives:
India, the second most populous country in the world, has two-thirds of its population living in rural areas. Rural women in developing countries like India have worse access to healthcare compared to their urban counterparts. We examined the association between place of residence and various pregnancy and birth outcomes among Indian women.
Methods:
We analyzed data from the 2015-2016 India Demographic and Health Survey (DHS). Socio-demographic and reproductive health-related information were obtained from Indian women of reproductive age. We calculated the prevalence of selected pregnancy and birth outcomes among the study participants. We conducted adjusted survey log binomial regression to determine the level of association between place of residence and various pregnancy and birth outcomes.
Results:
About 66.4% of the survey responders resided in villages. When adjusted for covariates, rural women had increased likelihood of experiencing miscarriage, stillbirth, early neonatal, late neonatal and infant mortality as compared to urban women. Urban women had 22% higher likelihood (PR = 1.22, 95% CI=1.10-1.35) of having an abortion as compared to rural dwellers.
Conclusion and Global Health Implications:
Despite India’s extensive efforts to improve maternal and reproductive health, wide geographical disparities exist between its urban and rural population. Interventions at various socio-ecologic and cultural levels, along with improved health literacy, access to improved health care and sanitation need attention when formulating and implementing policies and programs for equitable progress towards improved maternal and reproductive health.
Keywords
India
Maternal and reproductive health
Pregnancy outcomes
Birth outcomes
Miscarriage
Stillbirth
Neonatal mortality
Infant mortality
Abortion
Health equity
1. Introduction
1.1. Background of the Study
India, the home to more than a sixth of the world’s population, is one of the most culturally, religiously and ethnically diverse nations with two-thirds of the country’s population residing in villages.1 This number has decreased over the decades but still a vast majority continues to live in the rural areas. Despite progress in many fields, inequalities by socioeconomic status, geography and gender continue to persist. Inequities in health are not only the unequal but also the unfair distribution of healthcare due to unfair or inadequate social arrangements.2 Rural Indians lag behind due to many issues like inaccessibility to proper health centers, unavailability of modern technologies and amenities, coupled with poor sanitation.
Patriarchy continues to pull the reins of Indian society to this day. Girl-children are considered to be burdens and not treated the same way as boy-children. Girls, mainly in rural areas and from low socio-economic strata, are not considered to be the earning members of the family since they leave their parents’ homes after marriage, thus, they are relegated to the background when it comes to receiving formal education. When a girl is not educated, the entire family suffers; girls have high levels of fertility and mortality; they suffer from malnutrition and other related-health problems.3 Although outlawed for a long time ago, child marriage is still prevalent in many parts of rural India; it is estimated that 27% of 20–24year old females in India were married by age 18, and 7% were married by age 15.4 Although child marriage is a norm in several communities and many of the pregnancies from these marriages might be planned, teen pregnancies lead to multiple obstetric complications including preterm labor, low birth weight, pregnancy loss, infant mortality, pre-eclampsia, anemia and many others.5
1.2. Objectives of the Study
Although many studies have been conducted in the recent past to show the risks of adverse pregnancy outcomes among women in rural India,6,7 the existing literature on the impact of place of residence on various types of pregnancy and birth outcomes is very limited. We postulate that there is a varied effect of the place of residence on the different types of pregnancy and birth outcomes; and that overall, rural Indian women will have worse pregnancy and birth outcomes compared to their urban counterparts.
We hypothesize that there will be a contrast in the different types of pregnancy and birth outcomes like miscarriage, abortion, stillbirth, early-neonatal, late-neonatal, post-neonatal and infant mortality between rural and urban Indian women.
2. Methods
This was a cross-sectional study using the India Demographic and Health Survey (DHS) data for the year 2015-16. The DHS project is funded by the United States Agency for International Development (USAID) with contributions from other donors such as United Nations Children’s Fund (UNICEF), United Nations Population Fund (UNFPA), World Health Organization (WHO), and Joint United Nations Programme on HIV/AIDS (UNAIDS)8. The India DHS data was collected through National Family Health Survey which was presented to the survey takers in English and Hindi language. Translators were provided for those who did not understand or speak any of the two languages. The survey collects and disseminates information on characteristics of maternal health, children’s health, nutrition, family planning, and few diseases like malaria and HIV/AIDS. DHS selects nationally representative samples from different regions of the country.
2.1. Study Variables
We utilized the women’s data file from the India DHS which includes survey responses from women of reproductive age (i.e. 15 – 49 years old). The women included in the survey were selected at random among all eligible candidates in the household. Complete anonymity was maintained by following measures like not recording the respondent’s name and recoding the respondent files with identification numbers. The survey was conducted in seclusion, or re-scheduled to accommodate the individuals, ensuring utmost privacy.
For our analysis, we restricted the data to women who had ever been pregnant which was not available in the data set as a direct variable. So we created a composite variable from the following 3 variables that were present in the dataset: (1) total children ever born; (2) currently pregnant; and (3) ever had a pregnancy termination. Women who responded “more than 0” to the first question or a “yes” to the second or third question were categorized as having experienced pregnancy.
Our exposure of interest was place of residence which was classified into urban and rural. Our outcomes of interest were six the following pregnancy and birth outcomes: (1) miscarriage; (2) abortion; (3) stillbirth; (4) early neonatal mortality; (5) late neonatal mortality; (6) post-neonatal mortality; and (7) infant mortality. The information on miscarriage, abortion and stillbirth was obtained from the dataset through one survey question which read – “Did any of the pregnancies end in miscarriage, abortion, or stillbirth?” The information on early, late, post neonatal and infant mortality was obtained from the variable “Age at death of the child” and this information was available for up to 20 children for each respondent. Early neonatal mortality was defined as the death of the child at age 0 – 7 days, late neonatal mortality at age 8 – 27 days, post-neonatal mortality at age 28 – 364 days and infant mortality at age 0 – 364 days. A woman might have experienced more than one of these outcomes and each experience was included in the analysis. The covariates included in the study were respondent’s education, wealth index, marital status and age at first birth.
2.2. Statistical Analysis
We conducted bivariate analysis using Pearson’s chi-squared test among rural and urban women based on socio-demographic characteristics like respondent’s age, education, literacy, occupation, their economic status described using wealth index, marital status, respondent’s age at first marriage, caste, their partner’s age and education. We also compared urban and rural women based on their pregnancy and birth characteristics like their age at first birth, number of children, place of delivery of the last 6 children, knowledge and use of contraception, and ever had single or multiple pregnancy terminations. For place of delivery, the information was available only for the last 6 pregnancies; and if any of the deliveries occurred at respondent’s, her parent’s or others’ home, they were classified as “Home”; if any of the 6 deliveries occurred in a public health center and none of them at home, they were categorized as “Public Health Center,” whereas if any of the deliveries occurred only in private health center and none at home or public health center, they were classified as “Private Health Center.” The reason to classify in the given fashion was that home, public and private health centers are considered to be in ascending order of ‘better access to health care’ in India.
We calculated the prevalence of miscarriage, abortion, stillbirth; early neonatal, late neonatal, post neonatal and infant mortality stratified by place of residence (i.e. rural and urban). Furthermore, we conducted adjusted survey log binomial regression to evaluate the association between place of residence and each of the outcome variables. The covariates that were loaded onto the adjusted models were education, wealth index, marital status and respondent’s age at first birth. All statistical analyses were conducted using R (version 3·5·2), RStudio (version 1.1.463) and all tests of hypotheses were two-tailed with the type-1 error rate set at 5%.
2.3. Ethical Approval
This study was performed using publicly available de-identified data and so it was approved as exempt by the Institutional Review Board (IRB) of Baylor College of Medicine.
3. Results
3.1. Sociodemographic Characteristics Results
A total of 699,686 women 15- 49 years of age were surveyed in India for the DHS 2015-16. Of these, 70.63% (494,221) women had had a pregnancy experience and were included in our study. It was observed that 335,121 (66.4%) women lived in rural areas while 168,326 (33.6%) were urban dwellers. The socio-demographic characteristics of Indian women who had experienced pregnancy is displayed in Table 1. Rural women were twice as likely to be uneducated and illiterate when compared with urban women. As per wealth index, which is a composite measure of a household’s ownership of selected assets like television, materials used for construction of the respondent’s house, access to clean drinking water and sanitation etc., it was observed that rural women were more likely to be ‘poorest’/‘poorer’ compared to urban dwellers (52.7% vs. 9.4%). Around 30% of the women living in urban areas were forward class (those not belonging to Scheduled Caste, Schedule Tribe or Other Backward Classes) in comparison to 18.5% women in rural areas.
| Urban (169326, 33.6%) | Rural (335121, 66.4%) | p-value | |||
|---|---|---|---|---|---|
| n | % | n | % | ||
| Age Group | <0.0001 | ||||
| <20 years | 1991 | 1.2 | 8304 | 2.5 | |
| 21 - 29 years | 50576 | 29.9 | 117139 | 35.0 | |
| 30 - 39 years | 63530 | 37.5 | 115316 | 34.4 | |
| 40+ years | 53229 | 31.4 | 94362 | 28.2 | |
| Education | <0.0001 | ||||
| No education | 34169 | 20.2 | 141381 | 42.2 | |
| Primary | 20933 | 12.4 | 53312 | 15.9 | |
| Secondary | 83811 | 49.5 | 124701 | 37.2 | |
| Higher | 30413 | 18.0 | 15727 | 4.7 | |
| Literacy | <0.0001 | ||||
| Cannot read at all | 39503 | 23.3 | 155507 | 46.4 | |
| Able to read only parts of sentence | 9379 | 5.5 | 23411 | 7.0 | |
| Able to read whole sentence | 119266 | 70.4 | 152510 | 45.5 | |
| No card with required language | 350 | 0.2 | 760 | 0.2 | |
| Blind/visually impaired | 828 | 0.5 | 2933 | 0.9 | |
| Occupation | <0.0001 | ||||
| Not in work force/no occupation | 22461 | 13.3 | 36182 | 10.8 | |
| Professional/technical/managerial | 1283 | 0.8 | 939 | 0.3 | |
| Clerical | 179 | 0.1 | 151 | 0.0 | |
| Sales | 705 | 0.4 | 612 | 0.2 | |
| Agricultural | 1062 | 0.6 | 13507 | 4.0 | |
| Services/household and domestic | 1771 | 1.0 | 1546 | 0.5 | |
| Manual - skilled and unskilled | 2418 | 1.4 | 3272 | 1.0 | |
| Don’t know | 504 | 0.3 | 589 | 0.2 | |
| Missing | 138942 | 82.1 | 278323 | 83.1 | |
| Wealth Index | <0.0001 | ||||
| Poorest | 4757 | 2.8 | 87768 | 26.2 | |
| Poorer | 11259 | 6.6 | 88872 | 26.5% | |
| Middle | 26466 | 15.6 | 77731 | 23.2 | |
| Richer | 52379 | 30.9 | 53380 | 15.9 | |
| Richest | 74465 | 44.0 | 27370 | 8.2 | |
| Marital Status | <0.0001 | ||||
| Never in union [includes: married gauna not performed] | 203 | 0.1 | 407 | 0.1 | |
| Married | 159492 | 94.2 | 318319 | 95.0 | |
| Widowed | 7489 | 4.4 | 13134 | 3.9 | |
| Divorced | 586 | 0.3 | 761 | 0.2 | |
| No longer living together/separated | 1555 | 0.9 | 2500 | 0.7 | |
| Respondent’s age at first marriage | <0.0001 | ||||
| <10 years | 61 | 0.0 | 308 | 0.1 | |
| 10 - 14 years | 508 | 0.3 | 1572 | 0.5 | |
| 15 - 18 years | 1130 | 0.7 | 3298 | 1.0 | |
| 19 - 29 years | 509 | 0.3 | 1193 | 0.4 | |
| 30 - 30 years | 17 | 0.0 | 25 | 0.0 | |
| 40+ years | 5 | 0.0 | 27 | 0.0 | |
| Missing | 167096 | 98.7 | 328697 | 98.1 | |
| Caste | <0.0001 | ||||
| Scheduled Caste | 29115 | 17.2 | 73655 | 22.0 | |
| Scheduled Tribe | 6773 | 4.0 | 39749 | 11.9 | |
| Other Backward Classes | 73911 | 43.7 | 145526 | 43.4 | |
| None of them | 50768 | 30.0 | 62070 | 18.5 | |
| Don’t know | 1454 | 0.9 | 2106 | 0.6 | |
| Missing | 7306 | 4.3 | 12014 | 3.6 | |
| Partner’s age | <0.0001 | ||||
| <20 years | 32 | 0.0 | 140 | 0.0 | |
| 20 - 29 years | 4097 | 2.4 | 10774 | 3.2 | |
| 30 - 39 years | 10136 | 6.0 | 19242 | 5.7 | |
| 40 - 49 years | 9576 | 5.7 | 16148 | 4.8 | |
| 50+ years | 4733 | 2.8 | 7565 | 2.3 | |
| Missing | 140753 | 83.1 | 281252 | 83.9 | |
| Partner’s Education | <0.0001 | ||||
| No education | 3727 | 2.2 | 13500 | 4.0 | |
| Primary | 3651 | 2.2 | 9597 | 2.9 | |
| Secondary | 16268 | 9.6 | 28486 | 8.5 | |
| Higher | 6671 | 3.9 | 5012 | 1.5 | |
| Don’t know | 53 | 0.0 | 155 | 0.0 | |
| Missing | 138955 | 82.1 | 278371 | 83.1 | |
We compared pregnancy characteristics among rural and urban Indian women (Table 2). We found that close to a half of the rural women (46.1%) had childhood birth experiences in comparison to 37% in urban areas. Almost a quarter of rural women and 14% of urban women had 4 or more children. With respect to place of delivery, rural mothers had a higher prevalence of delivering the child at home or in a public health center, whereas the frequency of delivery in private health care settings was greater among urban women. Urban women had a higher prevalence of experiencing at least one and multiple pregnancy terminations. The knowledge and usage of contraception was also higher among urban residents as compared to their rural counterparts.
| Urban (169326, 33.6%) | Rural (335121, 66.4%) | p-value | |||
|---|---|---|---|---|---|
| n | % | n | % | ||
| Respondent’s age at first birth | <0.0001 | ||||
| 10 - 14 years | 5244 | 3.1 | 13260 | 4.0 | |
| 15 - 19 years | 57406 | 33.9 | 141234 | 42.1 | |
| 20 - 29 years | 95663 | 56.5 | 163203 | 48.7 | |
| 30 - 39 years | 4718 | 2.8 | 5090 | 1.5 | |
| >= 40 years | 126 | 0.1 | 176 | 0.1 | |
| Missing | 6169 | 3.6 | 12158 | 3.6 | |
| Number of children | <0.0001 | ||||
| None | 6032 | 3.6 | 11806 | 3.5 | |
| 1 - 3 children | 139473 | 82.4 | 241684 | 72.1 | |
| 4 - 6 children | 21702 | 12.8 | 71896 | 21.5 | |
| 7 -9 children | 1965 | 1.2 | 9020 | 2.7 | |
| 10 or more children | 154 | 0.1 | 715 | 0.2 | |
| Place of delivery | <0.0001 | ||||
| Home | 4533 | 2.7 | 25456 | 7.6 | |
| Public health center | 24821 | 14.7 | 72857 | 21.7 | |
| Private health center | 25406 | 15.0 | 31136 | 9.3 | |
| Missing | 114566 | 67.7 | 205671 | 61.4 | |
| Knowledge of contraception | <0.0001 | ||||
| Knows no method | 684 | 0.4 | 3872 | 1.2 | |
| Knows only folkloric /traditional method | 43 | 0.0 | 244 | 0.1 | |
| Knows modern method | 168598 | 99.6 | 331004 | 98.8 | |
| Ever used contraception | <0.0001 | ||||
| No | 46965 | 27.7 | 115080 | 34.3 | |
| Yes | 122360 | 72.3 | 220041 | 65.7 | |
| Ever had a pregnancy termination | <0.0001 | ||||
| Yes | 31606 | 18.7 | 52213 | 15.6 | |
| No | 137719 | 81.3 | 282907 | 84.4 | |
| Have had multiple pregnancy terminations | <0.0001 | ||||
| Yes | 675 | 0.4 | 1124 | 0.3 | |
| No | 10092 | 6.0 | 18840 | 5.6 | |
| Missing | 158558 | 93.6 | 315156 | 94.0 | |
3.2. Dependent or Outcome Results
Figure 1 presents the prevalence of various pregnancy and birth outcomes among rural and urban women. Abortion was the only pregnancy outcome which had significantly lower prevalence among rural women in comparison to urban women. The frequency of early neonatal mortality was more 70% greater among rural compared to urban women (7.2% versus 4.2%). The frequency of stillbirth was 50% greater while late neonatal mortality rate was double among rural as compared to urban inhabitants. Also, infant mortality was found to be significantly higher among rural mothers.
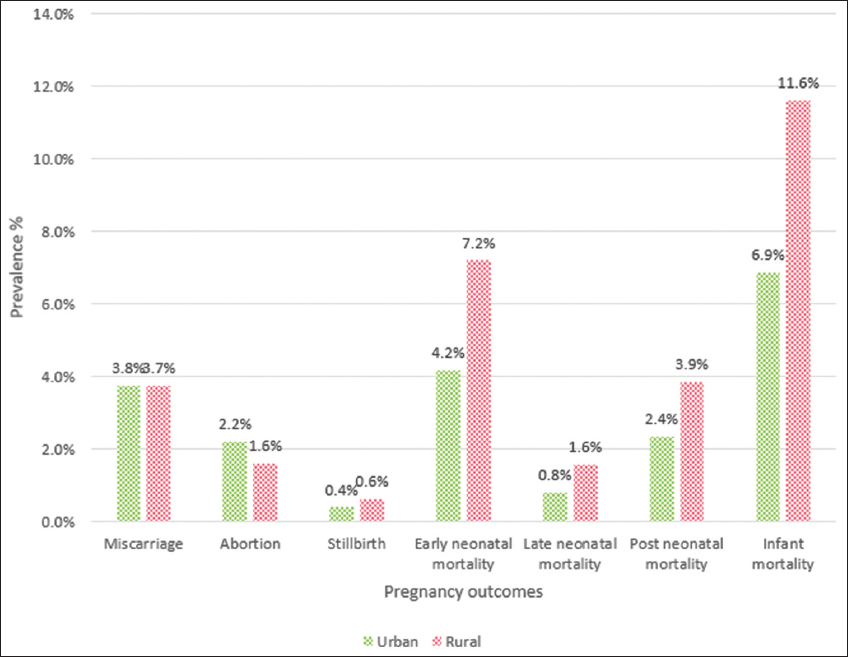
- Prevalence of various pregnancy and birth outcomes among urban and rural Indian women
Table 3 summarized the results of the adjusted estimates for the association between place of residence and various pregnancy and birth outcomes. With the exception of abortion, where rurality was a protective factor; and post-neonatal mortality which had similar risk, all other pregnancy and birth outcomes were worse among rural women as compared to their urban counterparts after adjusting for covariates. Rural women were 12% more likely (PR: 1.12, 95% CI: 1.02-1.23) to experience a miscarriage when compared with urban women. They also had 1.21 and 1.19 times increased likelihood of having a stillbirth and late neonatal mortality respectively in comparison to the urban residents. Additionally, the chances of experiencing infant mortality was 7% higher (PR: 1.07, 95% CI: 1.02-1.12) among rural dwellers.
| Miscarriage | Abortion | Stillbirth | Early neonatal mortality | Late neonatal mortality | Post neonatal mortality | Infant mortality | |
|---|---|---|---|---|---|---|---|
| Residence | |||||||
| Urban | Reference | Reference | Reference | Reference | Reference | Reference | Reference |
| Rural | 1.12 (1.02-1.23) | 0.82 (0.74-0.91) | 1.21 (1.03-1.43) | 1.09 (1.03-1.16) | 1.19 (1.08-1.31) | 0.97 (0.90-1.04) | 1.07 (1.02-1.12) |
| Education | |||||||
| None | Reference | Reference | Reference | Reference | Reference | Reference | Reference |
| Primary | 1.02 (0.91-1.14) | 1.07 (0.95-1.22) | 0.86 (0.73-1.01) | 0.89 (0.84-0.93) | 0.84 (0.76-0.94) | 0.74 (0.69-0.79) | 0.82 (0.78-0.86) |
| Secondary | 1.01 (0.93-1.11) | 1.23 (1.11-1.37) | 0.61 (0.53-0.70) | 0.64 (0.6-0.67) | 0.51 (0.46-0.56) | 0.46 (0.43-0.5) | 0.53 (0.51-0.56) |
| Higher | 1.05 (0.91-1.23) | 1.28 (1.09-1.51) | 0.48 (0.35-0.65) | 0.42 (0.37-0.47) | 0.32 (0.24-0.43) | 0.25 (0.21-0.29) | 0.31 (0.28-0.35) |
| Wealth Index | |||||||
| Richest | Reference | Reference | Reference | Reference | Reference | Reference | Reference |
| Poorest | 1.20 (1.04-1.39) | 0.57 (0.49-0.67) | 2.14 (1.65-2.78) | 1.87 (1.71-2.04) | 1.74 (1.47-2.05) | 1.76 (1.57-1.97) | 1.75 (1.62-1.88) |
| Poorer | 1.12 (0.98-1.29) | 0.75 (0.64-0.87) | 1.66 (1.28-2.14) | 1.65 (1.51-1.80) | 1.39 (1.18-1.63) | 1.54 (1.37-1.72) | 1.53 (1.42-1.64) |
| Middle | 0.99 (0.87-1.13) | 0.93 (0.81-1.07) | 1.4 (1.09-1.81) | 1.41 (1.29-1.55) | 1.31 (1.11-1.55) | 1.35 (1.19-1.52) | 1.33 (1.23-1.43) |
| Richer | 0.94 (0.82-1.07) | 1.03 (0.9-1.17) | 1.23 (0.94-1.60) | 1.16 (1.06-1.26) | 1.09 (0.92-1.30) | 1.19 (1.06-1.33) | 1.14 (1.06-1.23) |
| Marital Status | |||||||
| Married | Reference | Reference | Reference | Reference | Reference | Reference | Reference |
| Never in union [includes: married gauna not performed] | 2.64 (1.61-3.17) | 0.05 (0.02-0.09) | 4.53 (1.38-14.82) | 1.87 (1.03-3.40) | 12.64 (6.61-24.17) | 0.80 (0.39-1.67) | 2.32 (1.19-4.52) |
| Widowed | 1.26 (1.12-2.31) | 0.06 (0.03-0.15) | 6.67 (1.7-26.16) | 1.89 (1.03-3.44) | 8.26 (3.72-18.31) | 0.92 (0.44-1.92) | 2.38 (1.21-4.66) |
| Divorced | 3.66 (2.16-5.28) | 0.06 (0.02-0.16) | 4.75 (1.01-22.36) | 1.83 (0.93-3.62) | 10.66 (4.16-27.28) | 1.10 (0.45-2.66) | 1.32 (0.61-2.86) |
| No longer living together/separated | 3.59 (2.42-5.56) | 0.07 (0.03-0.17) | 3.12 (0.76-12.80) | 1.79 (0.95-3.37) | 9.99 (4.42-22.56) | 0.71 (0.32-1.56) | 1.67 (0.83-3.35) |
| Respondent’s age at first birth | |||||||
| 20 - 24 years | Reference | Reference | Reference | Reference | Reference | Reference | Reference |
| 10 - 14 years | 0.59 (0.42-0.85) | 1.77 (1.22-2.56) | 1.08 (0.65-1.8) | 1.60 (1.47-1.74) | 1.36 (1.15-1.62) | 1.56 (1.39-1.75) | 1.74 (1.62-1.87) |
| 15 - 19 years | 0.83 (0.76-0.90) | 1.34 (1.23-1.47) | 0.82 (0.72-0.94) | 1.24 (1.19-1.29) | 1.24 (1.14-1.34) | 1.28 (1.21-1.34) | 1.35 (1.31-1.40) |
| 25 - 29 years | 1.09 (0.95-1.25) | 0.82 (0.7-0.96) | 1.29 (1.01-1.66) | 0.97 (0.9-1.05) | 0.86 (0.74-1.01) | 0.90 (0.79-1.02) | 0.85 (0.79-0.92) |
| 30 - 34 years | 0.94 (0.72-1.23) | 0.86 (0.64-1.15) | 1.67 (1.11-2.52) | 0.98 (0.84-1.15) | 1.02 (0.74-1.39) | 0.80 (0.64-1.02) | 0.71 (0.61-0.83) |
| 35 - 39 years | 1.03 (0.57-1.85) | 0.81 (0.42-1.56) | 1.55 (0.64-3.77) | 0.66 (0.44-0.99) | 1.66 (0.8-3.46) | 0.68 (0.32-1.47) | 0.36 (0.23-0.57) |
| >= 40 years | 1.57 (0.22-11.28) | 0.79 (0.11-5.78) | 1.20 (1.02-1.41) | 1.10 (0.5-2.39) | 1.01 (0.32-3.22) | 1.55 (0.51-4.71) | 1.11 (0.49-2.55) |
3.3. Covariates
It was worth noting that increased educational qualification resulted in increased likelihood of abortion among Indian women. Also, women belonging to the two lowest economic quintiles were less likely to have an abortion. The opposite was true for the other outcome variables, namely, poorer and poorest women had increased likelihood of experiencing stillbirth, miscarriage, and infant mortality. There was a negative dose-response relationship between level of education attained and stillbirth, neonatal and infant mortality. Also, with increased economic potential, there seemed to be a statistically significant decrease in the likelihood of having stillbirth, early neonatal, late neonatal, post neonatal and infant mortality.
4. Discussion
4.1. Discussion
This study shows that there are statistically significant differences between women who lived in villages versus those who lived in urban areas when it comes to various socio-demographic and pregnancy-related markers. Rural inhabitants were observed to have worse access to education and infrastructural amenities which were utilized in creating the wealth index variable in the data set. Villages also had a higher proportion (77.3%) of socially disadvantaged women (scheduled caste, scheduled tribe and other backward classes) compared to cities and towns (64.8%). Around 7% of the rural dwellers’ partners had less than secondary education; which was considerably higher when compared to partners of urban residents (4.4%). Women in rural areas seemed to be giving birth at a younger age and had more children as compared to urban residents.
Our study confirmed what other studies have shown; that rural women had a higher prevalence of delivering a child at home or in a public health center than at a private institution9. Culturally, Indian women go to their parents’ house to have their delivery and to get postnatal care. The only option typically available to a huge number of rural and underprivileged women is home birth or delivery in government hospitals due to constraints of cost and access. Many of the home birth attendants are unskilled and uneducated; while the condition of government hospitals is equally grim where sometimes, two women and their newborns have to share the same bed.9 Even though medical advancement, state initiatives and awareness about cesarean births have resulted in about 90% of child births to be conducted in medical institutions,10 most of these births still occur in extremely unsanitary government hospitals, which explains the high maternal mortality ratio (174 per 100,000 births)11 in India.
We also observed that rural women had diminished prevalence of knowledge and usage of contraception in contrast to urban women. India is a country where it is a social norm to have a child early in the marriage, and contraception is less likely if a male child has not been born, and contraception is the sole responsibility of women. Generally, women fear using OCP (oral contraceptive pills) and IUD (intrauterine device); and have negative attitudes towards condoms. Among rural and tribal women, female sterilization is often the preferred means of contraception12. India has 31 million women (the highest among developing countries) with an “unmet need” for contraception.13
Our results showed that rural women had lesser likelihood of having an abortion whereas they had increased probabilities of experiencing other adverse pregnancy and birth outcomes like miscarriage, stillbirth and infant mortality. This could be attributed to lesser awareness and diminished access to quality health care. A huge percentage of information (about 94%) was missing in the variables pertaining to pregnancy terminations. The reason for this could be the social stigma attached to pregnancy loss; or to the fact that women continue to have or are forced to have abortions based on prenatal gender determination, although it remains a criminal offence in India. Another reason for such a high non-response rate could be the taboo associated with unwanted pregnancies caused by premarital sexual relationships, rape or even failure of contraception. Termination of pregnancy is permitted in India for a broad range of conditions up to 20 weeks of gestation but rural women think that seeking an abortion is a crime and become vulnerable to unsafe and illegal methods of pregnancy terminations, causing further complications like incomplete abortion, infection and so on.14
4.2. Limitations
As with any other survey-based research projects, ours has a few limitations like recall bias, inability to establish causal inferences and social likeability bias. There are various strengths to our study. DHS surveys are widely used throughout the world and the data collection process is considered highly meticulous and reliable. Moreover, the survey sample is representative of the population distribution of the country. To our knowledge, this is the first study that considers various types of pregnancy and birth outcomes and their association with place of residence. Therefore, our study can guide the development and implementation of targeted interventions among the various levels of heterogeneous social groups.
5. Conclusion and Global Health Implications
This study highlights the strong association that exists between place of residence and various pregnancy and birth outcomes. Although India has made extensive efforts to increase access to reproductive health care, and in some regions a lot of progress has been achieved, the progress made has been uneven and inequitable; consequently, many marginalized women still lack quality access to maternal and reproductive health care, especially in rural areas. More work in the areas of gender equality, education, infrastructure and reproductive health care needs to be done to bridge the wide gap between rural and metropolitan India. It is key to note that economic status, gender, social status and geography are all closely interrelated in influencing use of and access to maternal and reproductive health care15. Appropriate attention should be given on how these social determinants interplay when designing policies and programs to reach equitable progress toward improved maternal and reproductive health.
Conflicts of Interest: The authors declare that they have no conflict of interest.
Funding/Support: None.
Ethics Approval: The study was performed on de-identified secondary data. IRB approval from Baylor College of Medicine obtained.
References
- Levelling up (Part1):A Discussion on Concepts and Principles for Tackling Social Inequities in Health. http://who.int/social_determinants/resources/leveling_up_part1.pdf
- Low female literacy rate in India - Factors and Impact on Society |My India. https://www.mapsofindia.com/my-india/society/low-female-literacy-rate-and-its-impact-on-our-society
- Risk of Adverse Pregnancy Outcomes among Women Practicing Poor Sanitation in Rural India:A Population-Based Prospective Cohort Study. PLOS Medicine. 2015;12(7) doi:10.1371/journal.pmed.1001851
- [Google Scholar]
- Influence of Sexual and Reproductive Health Literacy on Single and Recurrent Adolescent Pregnancy in Latin America. J ournal of Pediatric and Adolescent Gynecology 2019 doi:10.1016/j.jpag.2019.06.003
- [Google Scholar]
- Impact of social capital, harassment of women and girls, and water and sanitation access on premature birth and low infant birth weight in India. Plos One. 2018;13(10) doi:10.1371/journal.pone.0205345
- [Google Scholar]
- International Institute for Population Sciences (IIPS). http://iipsindia.ac.in/
- India:DHS 2015-16 - Final Report (English). https://dhsprogram.com/publications/publication-FR339-DHS-Final-Reports.cfm Published December 1 2017
- Population Reference Bureau. https://www.prb.org/maternalcareinindiarevealsga psbetweenurbanandruralrichandpoor/
- WHO UNICEF UNFPA World Bank Group and UNPD Maternal Mortality Estimation Inter-Agency Group. http://www.who.int/gho/maternal_health/countries/ind.pdf
- Barriers to use Contraceptive Methods among Rural Young Married Couples in Maharashtra, India:Qualitative Findings. Asian Journal of Research in Social Sciences and Humanities. 2015;5(6):18. doi:10.5958/2249-7315.2015.00132.x
- [Google Scholar]
- Multicountry analysis of pregnancy termination and intimate partner violence in Latin America using Demographic and Health Survey data. International Journal of Gynecology &Obstetrics. 2019;146(3):296-301. doi:10.1002/ijgo.12876
- [Google Scholar]
- Inequity in India:the case of maternal and reproductive health. Global Health Action. 2013;6(1):19145. doi:10.3402/gha.v6i0.19145





