Translate this page into:
Integrating Prevention of Mother-to-Child Transmission of HIV Care into General Maternal Child Health Care in Western Kenya
*Corresponding author email: msuhl@iu.edu
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Background:
Health systems integration is becoming increasingly important as the global health community transitions from acute, disease-specific health programming to models of care built for chronic diseases, primarily designed to strengthen public-sector health systems. In many countries across sub-Saharan Africa, including Kenya, prevention of mother-to-child transmission of HIV (pMTCT) services are being integrated into the general maternal child health (MCH) clinics. The objective of this study was to evaluate the benefits and challenges for integration of care within a developing health system, through the lens of an evaluative framework.
Methods:
A framework adapted from the World Health Organization’s six critical health systems functions was used to evaluate the integration of pMTCT services with general MCH clinics in western Kenya. Perspectives were collected from key stakeholders, including pMTCT and MCH program leadership and local health providers. The benefits and challenges of integration across each of the health system functions were evaluated to better understand this approach.
Results:
Key informants in leadership positions and MCH staff shared similar perspectives regarding benefits and challenges of integration. Benefits of integration included convenience for families through streamlining of services and reduced HIV stigma. Concerns and challenges included confidentiality issues related to HIV status, particularly in the context of high-volume, crowded clinical spaces.
Conclusion and Global Health Implications:
The results from this study highlight areas that need to be addressed to maximize the effectiveness and clinical flow of the pMTCT-MCH integration model. The lessons learned from this integration may be applied to other settings in sub-Saharan Africa attempting to integrate HIV care into the broader public-sector health system.
Keywords
HIV prevention
Maternal-child health
Prevention of maternal-to-child transmission
Health services
Integration
Kenya
Sub-Saharan Africa
1. Introduction
As the global health community transitions from acute, disease-specific health programming to models of care built for chronic diseases, attention has been turned to approaches focused on health systems integration.1 Health system integration has been described as “the extent, pattern, and rate of adoption and eventual assimilation of health interventions into critical health system functions.”2,3 Historically, vertical health care programming and financing has been the primary focus, with specific health infrastructure developed for specific disease states, such as malaria or HIV/AIDS. This approach promotes rapid scale-up of care services, particularly in the face of epidemics, simplifies monitoring and evaluation processes, and streamlines financing mechanisms, especially in low- and middle-income countries where health care programming is so commonly externally funded.4,5 Those against this approach believe it creates unsustainable, disease-specific care silos that could decrease access, quality and equity, and render the health system less responsive to the needs of the population.6 They argue that instead, a horizontal, more integrated, approach should be employed to focus on broader public health goals and health systems strengthening.7 A novel, diagonal approach has been developed, where separate, vertical programs are integrated into a broader set of primary health care services, despite retaining some specialized staff, resources, and infrastructure to ensure continued effectiveness. In this model, the individual barriers of the disease-specific and systemic methods can be overcome and leveraged to reinforce the overall system.8 To better organize prioritization for health systems strengthening efforts, the World Health Organization (WHO) has organized health systems into six critical functions or building blocks: (1) leadership and governance, (2) financing, (3) information systems, (4) health care workforce, (5) medical products and technologies (i.e., diagnostics and therapeutics and their supply chains), and (6) service delivery.2 An adapted framework has been similarly proposed to analyze the integration of targeted health interventions into health systems.7 Although the aforementioned building blocks have been established, there is a paucity of literature detailing programmatic examples of how this framework is used within an existing healthcare system, specifically as it relates to the evaluation of health systems integration.
For HIV care, integration of prevention of mother-to-child transmission (pMTCT) of HIV into the antenatal and postnatal clinics is a natural fit. These antenatal and postnatal clinics provide services for all pregnant women and their infants and young children, collectively referred to as maternal-child health (MCH) clinics. MCH clinics provide counseling and prenatal testing to pregnant mothers, as well as diagnose and manage conditions and illnesses during pregnancy. MCH clinics also perform weight checks, nutritional monitoring, immunizations for infants and young children, and strive to offer integrated management of childhood illness. There are multiple studies with small data sets showing that pMTCT – MCH integration improves HIV management, including increased uptake of anti-retroviral therapy (ART) during pregnancy, and more time spent with providers.9 However, systematic reviews and meta-analyses on this topic suggest persistently elevated rates of maternal-to-child transmission of HIV after integration, which suggests poor uptake of integrated pMTCT services.10,11
Option B+, the lifelong provision of antiretroviral therapy (ART) to any pregnant woman regardless of CD4 count or clinical stage, has been implemented in Kenya and is now the standard of care. After initiation, a randomized-controlled trial was conducted in Kenya to evaluate the effect of pMTCT and MCH clinic integration on health services.12 This study was plagued by very high attrition rates and showed no improvement in maternal ART adherence or vertical transmission of HIV.12 Further data analysis showed that women and children in integrated programs had longer wait times and experienced inadequate staffing and clinical space for the number of patients provided care.13 Many unanswered questions remained regarding the outcomes of integrating pMTCT services into the broader MCH care program, and there was a need to better understand the nature and extent of integration across the different health system functions.
More research is needed to examine real-world examples of how integration of health services is evaluated. The objective of this study was to evaluate the benefits and challenges of integration of pMTCT and HIV care within MCH clinics in western Kenya, using the WHO’s six health system building blocks as the analytical framework. Various aspects of integration across each of the health system functions were examined from the perspective of key stakeholders, including leadership and clinical staff, to better understand the challenges and benefits of this integrated system of health care delivery.
2. Methods
2.1. pMTCT – MCH Integration at AMPATH
The Academic Model Providing Access to Healthcare (AMPATH) is a partnership between Moi University, Moi Teaching and Referral Hospital, and a consortium of North American academic medical centers led by Indiana University. Their mission is to leverage the power of the tripartite academic mission – service, teaching and research – to develop leaders in health care and to support and improve the Ministry of Health (MOH) care system in western Kenya. The AMPATH HIV care program is an implementing partner funded by the President’s Emergency Plan for AIDS Relief (PEPFAR) through the United States Agency for International Development (USAID), supporting nearly 500 MOH facilities providing comprehensive HIV services for a catchment population of 8 million people in western Kenya.14-16 Historically, most pMTCT services in Kenya were delivered within the “vertical” HIV clinics within each MOH facility, separate from the general maternal-child health (MCH) care program. In some parts of the country, pMTCT services and general MCH care were provided together. However, in most larger volume clinics, there were separate rooms and staff, or even stand-alone pMTCT and HIV clinics, funded and delivered by larger vertical HIV care programs, that provided services distinct from the general MCH clinics. The Kenya MOH elimination of mother-to-child transmission of HIV (eMTCT) Strategic Framework 2012 – 2015 included integration of pMTCT services into MCH as part of its key strategic objectives.17 In late 2015, under direction from the Kenyan MOH, as well as USAID, the process of integrating AMPATH’s pMTCT services into the general MCH care system began. The goal of this integration process was to provide pMTCT care for all pregnant and breastfeeding women, including ART provision and disease monitoring, within the general MCH clinics. This would allow for all pregnant women and their infants to receive care together, in the same space, and with the same clinical staff, regardless of HIV status. When necessary, the integration process would also provide subsequent HIV-exposed infant testing, monitoring, and treatment within the MCH until the infant reached two years of age, when confirmatory HIV testing is performed. At this point, the mother would return to the AMPATH HIV clinic to continue her HIV care. The overarching goals of this integration process were to increase service efficiency and streamline the financing and delivery of HIV services into the MOH care system.17
After the Kenyan MOH’s mandate of pMTCT and MCH integration, a series of key stakeholder meetings were held between administrative and programmatic leadership and care providers within both the AMPATH HIV program and MOH MCH program, to plan the transition to integration. During this process, transfer procedures were developed, care guidelines were adapted, and trainings were planned to educate providers on how to deliver pMTCT and HIV care services within the MCH care system. During the initial stages of integration, a phased transition of services was initiated, to prevent overwhelming the current health care system. This transition allowed existing HIV-positive mothers and their exposed infants to be retained in the AMPATH HIV clinics, while only newly pregnant mothers with known HIV-infection or pregnant mothers with newly diagnosed HIV were transferred to the MCH for care. After the initial six-months of integration, all HIV-positive pregnant or breastfeeding women were transferred to the MCH for care. Since integration in 2015, there are approximately over 6,000 pregnant and breastfeeding mothers with known HIV infection who have been integrated from vertical AMPATH pMTCT services into general MOH MCH care across AMPATH’s catchment area in western Kenya.18
2.2. Evaluation Framework and Data Collection
Using the WHO’s health system building blocks framework for evaluating health systems integration, this evaluation study assessed the process of integration of pMTCT services into MCH care across the AMPATH program in western Kenya (Figure 1). During the roll-out of the integration process, a series of internal meetings among pMTCT and MCH program leadership were held to plan the integration of pMTCT and MCH services and discuss potential challenges that would need to be overcome. Following this, as integration began, a workplan was developed using the six WHO health system building blocks as a guide in order to address integration challenges across each of the health system functions and propose solutions to overcome them. Eighteen months after integration began, a meeting was held with seven key programmatic and clinical leaders in the pMTCT and MCH programs, to specifically discuss the nature and extent, as well as the benefits and challenges, of integration across each of the WHO’s six critical health system functions. Notes from these internal planning meetings, the integration workplan, and the post-integration follow-up meeting (known henceforth as Key Informant Sessions) were synthesized and organized into common themes using the WHO’s six health system building blocks as a guiding framework.
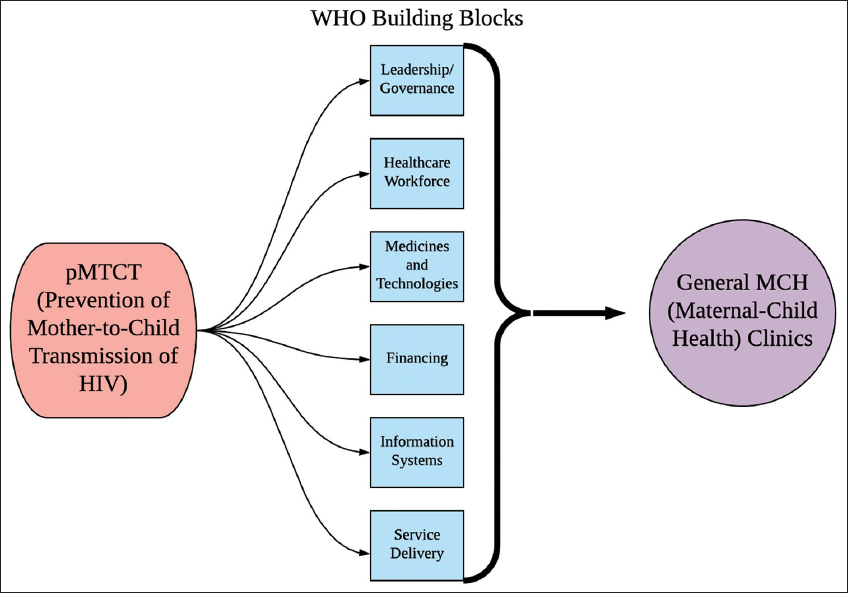
- The World Health Organization Health Systems Framework Adapted to pMTCT – MCH Integration
In November 2016, approximately six months following integration, a structured survey of clinical providers in six MCH clinics across western Kenya was conducted to assess provider perspectives on integration. The clinics were chosen by convenience sampling, as these are high-volume sites within the AMPATH catchment area where integration was known to have occurred. A broad range of provider cadres and roles within the MCH were included, although all had to have at least one year of experience working in the MCH prior to integration.
Survey questions were aimed at identifying provider perceptions on specific aspects of pMTCT-MCH integration, such as the degree to which it may be beneficial, whether the prior model of care was preferred, and the biggest benefits and challenges of integration. Providers were allowed to indicate more than one benefit and challenge.
2.3. Data Analysis and Ethical Approvals
Survey results were analyzed with Microsoft Excel using descriptive statistics. For the structured survey of MCH providers, written informed consent was received prior to participation and ethical approval was obtained from the Institutional Research and Ethics Committee of Moi Teaching and Referral Hospital and Moi University College of Health Sciences in Eldoret, Kenya, as well as the Institutional Review Board of Indiana University School of Medicine. IRB approval was not obtained for the key stakeholder meetings, as these were conducted as part of the clinical care program and no personally identifiable information was discussed. These discussions were summarized and key themes were extracted.
3. RESULTS
3.1. Themes Emerging from the Key Informant Sessions
The perspectives of key pMTCT and MCH leadership on the benefits and challenges of pMTCT – MCH integration across each of the six critical health system functions are summarized in Table 1. Leadership perceived key benefits of integration to include: strengthening of the MCH health system by increasing national recognition and resources; the ability to qualify for performance-based incentives; convenience for families to have all care under one roof; and reducing stigma for HIV-positive patients receiving antenatal care at the HIV clinics. The key informant sessions revealed major challenges including longer wait times, lack of common communication channels and accountability, and logistical issues including location of ART storage and dispensing. There were also concerns that there would be accidental disclosure of a mother’s HIV status to other patients within the clinic. Task-shifting also seemed to be a significant area of focus, as the staff at the MCH clinics were asked to perform at a much higher level than previously. Nurses were requesting and dispensing ART from the pharmacy and performing blood draws on HIV-exposed infants. Mentor mothers, trained lay-persons analogous to peer navigators, stepped up to obtain vital signs and perform routine record keeping and encounter documentation. While additional training was needed for the staff to perform these tasks, it did enable clinical staff to work at the top of their abilities.
| (1) Leadership and Governance | Benefits: • Increased opportunity for further collaboration in an already collaborative environment between the Kenyan MOH and AMPATH • Alignment with national MOH priorities |
| Challenges: • Push for rapid integration without laying adequate groundwork and lack of preparation • Lack of common or standardized communication channels between AMPATH and MCH • Separate leadership and governance structures between AMPATH and MCH leading to unclear reporting structure, lack of accountability, and different priorities, planning, budgeting, and performance evaluations between the two programs |
|
| (2) Health Workforce | Benefits: • Task-shifting to work at highest functional level and take on new roles MCH nurses appreciated the recognition that they were capable of taking on new roles and building their program |
| Challenges • High turnover rate and rotation of MCH staff • Need for extra training for MCH staff given new roles providing pMTCT and HIV care • Negative attitudes related to the perception that pMTCT and HIV care was specialized and was not in the purview of the MCH |
|
| (3) Medical Products and Technologies (i.e., Diagnostics and Therapeutics) | Benefits: • The ability of the MCH to procure anti-retroviral therapy directly, rather than going through the AMPATH pharmacy |
| Challenges: • Anti-retroviral drug storage is challenging for MCH due to space, security, and refrigeration issues • Specialized HIV testing is not conducted in the traditional MCH lab, requiring the referral of mothers and infants back to the AMPATH lab • Lab results not getting returned in time or lost |
|
| (4) Financing | Benefits: • Opportunity to implement performance-based incentives into MCH clinics, which had historically been practiced at AMPATH • Ability to leverage multiple resources for training and capacity building |
| Challenges: • Differences in user fees between AMPATH, which was mostly free care, and the MCH, which charged various user fees, and lack of a clear plan to harmonize these fee structures • Different funding streams for pMTCT and MCH care, leading to further accountability issues |
|
| (5) Information Systems | Benefits: • None noted |
| Challenges: • Increased requirements for clinical documentation and programmatic monitoring and evaluation needed for pMTCT compared to general MCH care • AMPATH pMTCT and the MCH use separate information systems; the AMPATH system is electronic and the MCH system is paper-based • Separate information systems and the transfer process created issues related to missing data and accountability for data collection • When a mother transferred from the AMPATH pMTCT program to the MCH this created a gap in record keeping, due to the different clinical information systems, limiting the longitudinal clinical tracking abilities, as well as hampering research, monitoring, and evaluation efforts |
|
| (6) Service Delivery | Benefits: • Opportunity to have all care under one roof and streamlining services • Normalizing HIV care with non-HIV care and reducing stigma • Future opportunities for integrated service delivery after integration of pMTCT and MCH |
| Challenges: • Rapidly changing HIV guidelines leading to staff confusion and need for continual training and mentorship • New workflow with HIV+/pMTCT patients integrated into general MCH care • Longer queues and clinic crowding • HIV+ mothers not being used to the new location at the MCH leading to confusion and lack of comfort • Lack of adequate sensitization and counseling of pMTCT mothers ahead of time because integration happened quickly • Lack of continuous longitudinal care from MCH to HIV follow-up care after pregnancy and for infants after age 2 • Disjointed care for pregnant mothers with older children receiving HIV care at AMPATH • Accidental disclosure and stigma against HIV+ patients • Loss of additional ancillary and supportive services for HIV+ mothers, such as nutrition, psychosocial support, and poverty-reduction efforts, that were part of AMPATH’s care program but not traditional components of the MCH clinic • Concern for increased loss-to-follow-up due to mothers “falling through the cracks” during integration transfer process, and lack of adequate number outreach workers / mentor mothers at MCH |
3.2. Clinical Provider Survey
Of the clinical providers surveyed, 76% (n=25) believed that pMTCT-MCH integration was beneficial for the mothers and their babies. Nearly all (n=32) reported that they would not want to return to the previous model of care, and only one reported that they had no preference. The most commonly reported benefit seen with integration was the reduction of HIV-related stigma (41.7%, n=20). Thirty-three clinical MCH staff were surveyed from six different high-volume clinics throughout western Kenya. Most were nurses who had been working in MCH for more than 3 years, and almost all participants were female (Table 2).
| Variable | N (%) |
|---|---|
| Clinic | |
| Eldoret | 7 (21) |
| Turbo | 5 (15) |
| Mosoriot | 6 (18) |
| Busia | 4 (12) |
| Webuye | 4 (12) |
| Kitale | 7 (21) |
| Clinical Role | |
| Nurse | 17 (52) |
| Nutritionist | 6 (18) |
| PMTCT Staff | 5 (15)* |
| Mentor Mother | 5 (15) |
| Clinical officer | 1 (3) |
| Counsellor | 1 (3) |
| Records Administrator | 1 (3) |
| Gender | |
| Female | 32 (96) |
| Age (in years) | |
| 25 – 34 | 6 (18) |
| 30 – 34 | 18 (55) |
| 35 – 39 | 3 (9) |
| > 40 | 6 (18) |
| Years of experience in MCH | |
| <1 | 4 (12) |
| 1-3 | 21 (63) |
| >3 | 8 (25) |
Other common responses were related to the convenience of more comprehensive care (Table 3). The biggest challenge perceived by the clinical providers was the higher patient volume (38.8%, n=19), with lack of space in the clinic being the second most common response (26.5%, n=13). Of note, three of the clinical providers reported that lack of privacy and confidentiality for HIV-infected patients was a big challenge with integration. While responses regarding the biggest benefits of integration were similar across clinic sites, a few of the biggest challenges appeared to affect certain clinics more than others. In 5 of the 6 clinics, providers indicated that high patient volume or lack of space was the biggest challenge they faced with integration.
| Question: | Response | N (%)* |
|---|---|---|
| What is the biggest benefit seen with integration?a | Less HIV stigma | 20 (41.7) |
| More streamlined and efficient services | 8 (16.7) | |
| Comprehensive care | 7 (14.6) | |
| Less frequent clinic visits for HIV infected mothers | 6 (12.5) | |
| Higher quality services | 6 (12.5) | |
| Cost-effective care | 1 (2.1) | |
| What is the biggest challenge seen with integration?b | Higher patient volume | 19 (38.8) |
| Lack of space in clinic | 13 (26.5) | |
| Lack of pMTCT training | 5 (10.2) | |
| Increased data entry requirements | 5 (10.2) | |
| Lack of privacy/confidentiality | 3 (6.1) | |
| Missing information on HIV-infected patients | 1 (2.0) | |
| Issues with the lab for HIV-infected and exposed families | 1 (2.0) | |
| Issues with additional supplies being in stock | 1 (2.0) | |
| Concern regarding new requirement for payment for services | 1 (2.0) |
4. Discussion
Key informants in leadership positions and MCH staff working within the clinic shared many of the same perspectives regarding benefits and challenges of integration. Key benefits of integration included convenience for families through streamlining of services, and reduced HIV stigma. Developing the new skills required of MCH nurses to deliver pMTCT and HIV care was initially a challenge, however, with additional training and mentorship, this was eventually thought to be beneficial. This additional skill-set built capacity and increased the recognition of the MCH workforce as they took on their new roles. However, other concerns remained regarding confidentiality issues related to HIV status, particularly in the context of high-volume, and crowded clinical spaces. Related to this, the key challenges perceived by both leadership and providers were increased patient volume without increased clinical staff or space. AMPATH and MCH leadership also identified multiple challenges related to the use of different information systems for clinical care, as well as monitoring and evaluation, which also speaks to the challenges related to separate governance and financing of both programs.
Integration of care is often perceived as an organizing method for both economic benefits and service delivery, to provide comprehensive care that is easily accessible by all those who need it.19 However, when health care integration is formally evaluated, the purpose, nature, and extent of the integration is often found to be highly heterogeneous20 and interventions are rarely completely integrated into all health system functions.7 By evaluating the integration of pMTCT and HIV care within MCH at AMPATH through the WHO framework, we were able to identify strengths and challenges related to integration of care that can be utilized for policy making within the healthcare system and beyond.
Initially, a pMTCT – MCH technical working group was formed to create a shared leadership structure, guiding the implementation of solutions in response to each of the challenges encountered across each of the health system functions. From this working group, several innovations were implemented within the pMTCT-MCH clinic to strengthen the integration process. One specific solution was to expand the role of mentor mothers. These individuals are hired from within the community which they live, and are often HIV-positive. Their life experiences enable them to provide social support for families affected by HIV. After integration, mentor mothers expanded their role to be trained to help overburdened MCH nurses obtain patient vitals and perform clinical record keeping. Additionally, they helped guide pregnant mothers through the transfer process, mitigating potential loss-to-follow-up. In resource-limited settings with limited clinical staff, having fully cohesive staff performing at the top level of their ability maximizes a health care systems’ ability to provide care for its patients. Additional ongoing innovative work is being done to harmonize the two information systems to minimize data gaps, ensure uninterrupted care, and meet monitoring and evaluation requirement of both programs.
The results from this study highlight some areas that need to be addressed to maximize the effectiveness and clinical flow of the pMTCT-MCH integration model. While some challenges, such as inadequate clinical staff and space, may require large systematic changes in infrastructure and resources, utilizing substantial time to organize and finance, other areas of concern could be addressed immediately. For example, both key informants and clinical providers noted that HIV-positive patients risked a breach of confidentiality when accessing pMTCT care due to limited clinical space. This environment sets the stage for accidental disclosure and increased stigma for HIV-positive patients receiving care. Clinical space reorganization and patient flow redesign may offer practical solutions for maintaining confidentially without increasing the size of the clinical space. Additional solutions to overcome this challenge include the implementation of protocols, reinforced by further staff training, promoting confidential discussions regarding HIV status within crowded clinical spaces, thus avoiding inadvertent disclosure. Other areas of focus for clinical improvement include streamlining the system for ART administration for patients and increased training and mentorship of clinical staff for their additional responsibilities.
Our paper is limited by reporting the perspectives of program leadership and clinical providers alone. Future studies should also incorporate the voices of pregnant mothers themselves. Future research should also look at the impact that pMTCT-MCH integration has on patient outcomes, such as vertical transmission of HIV, maternal and infant mortality, and the growth and development of HIV-exposed infants. Evaluation of this policy change is critical to ensure that clinical practice is having the anticipated outcome of improving the health and health care of HIV-positive women and their young children.
5. Conclusion and Global Health Implications
We performed a health system evaluation of a policy change involving the integration of pMTCT care into the MCH clinics in western Kenya. The perspectives from key informants and clinical providers identified major benefits of integration as convenience and reduced HIV stigma, while also noting challenges, such as increase patient volume, longer wait times, inadequate staffing and clinical space, risk for inadvertent HIV disclosure, and disparate information systems. Further work needs to be done to address the challenges related to integration to ensure that this practice change does not negatively impact care for pregnant HIV-positive mothers and their infants. The lessons learned from this integration may be applied to other settings in sub-Saharan Africa attempting to integrate HIV care into the broader MOH health care system.
Acknowledgements:
None
Compliance With Ethical Standards
Conflicts of Interest: The authors have no conflicts of interest relevant to this article to disclose.
Funding/Support: The study was unfunded.
Ethics Approval: Ethical approval was obtained from the Institutional Research and Ethics Committee of Moi Teaching and Referral Hospital and Moi University College of Health Sciences in Eldoret, Kenya, as well as the Institutional Review Board of Indiana University School of Medicine.
Disclaimer: None.
References
- World Health Organization. In: When do vertical (stand alone) programmes have a place in health systems?. Geneva, Switzerland: World Health Organization; 2008.
- [Google Scholar]
- Everybody's business--strengthening health systems to improve health outcomes:WHO's framework for action. Geneva, Switzerland: World Health Organization; 2007.
- The World health report 2000:health systems:improving performance. Geneva, Switzerland: World Health Organization; 2000.
- An assessment of interactions between global health initiatives and country health systems. Lancet (London, England). 2009;373(9681):2137-2169.
- [Google Scholar]
- National spending on health by source for 184 countries between 2013 and 2040. Lancet (London, England). 2016;387(10037):2521-2535.
- [Google Scholar]
- Horizontal and vertical delivery of health services:what are the tradeoffs. Washington, DC: The World Bank 2004/2005;
- Integration of targeted health interventions into health systems:a conceptual framework for analysis. Health Policy Plan. 2010;25(2):104-111.
- [Google Scholar]
- Achieving Effective Universal Health Coverage And Diagonal Approaches To Care For Chronic Illnesses. Health Affairs (Project Hope). 2015;34(9):1514-1522.
- [Google Scholar]
- Integration of HIV/AIDS services with maternal, neonatal and child health, nutrition, and family planning services. Cochrane Database Syst Rev. 2012;9:CD010119. doi:10.1002/14651858.CD010119
- [Google Scholar]
- The uptake of integrated perinatal prevention of mother-to-child HIV transmission programs in low- and middle-income countries:a systematic review. PloS ONE. 2013;8(3):e56550.
- [Google Scholar]
- Integrating antiretroviral therapy into antenatal care and maternal and child health settings:a systematic review and meta-analysis. Bull World Health Organ. 2013;91(1):46-56. doi:10.2471/BLT.12.107003
- [Google Scholar]
- Implementation and Operational Research:Effect of Integration of HIV Care and Treatment Into Antenatal Care Clinics on Mother-to-Child HIV Transmission and Maternal Outcomes in Nyanza, Kenya:Results From the SHAIP Cluster Randomized Controlled Trial. J Acquir Immune Defic Syndr. 2015;69(5):e164-171.
- [Google Scholar]
- Implementation and Operational Research:Effects of Antenatal Care and HIV Treatment Integration on Elements of the PMTCT Cascade:Results From the SHAIP Cluster-Randomized Controlled Trial in Kenya. J Acquir Immune Defic Syndr. 2015;69(5):e172-181.
- [Google Scholar]
- The impact of the President's Emergency Plan for AIDS Relief on expansion of HIV care services for adult patients in western Kenya. AIDS (London, England). 2009;23(2):195-201.
- [Google Scholar]
- Responding to the HIV pandemic:the power of an academic medical partnership. Acad Med. 2007;82(8):812-818.
- [Google Scholar]
- A Case Study in Global Health:Harnessing the Power of Partnerships. Indianapolis, Indiana: Sagamore Institute; 2015.
- In:National AIDS and STI Control Programme ed. Nairobi, Kenya: Ministry of Health; 2012. p. :46.
- Integrating prevention of mother-to-child HIV transmission (PMTCT) programmes with other health services for preventing HIV infection and improving HIV outcomes in developing countries. The Cochrane Database Syst Rev. 2011;6:Cd008741.
- [Google Scholar]
- A systematic review of the evidence on integration of targeted health interventions into health systems. Health Policy Plan. 2010;25(1):1-14.
- [Google Scholar]





