Translate this page into:
Child Development Monitoring in Well-baby Clinics in Kenya
*Corresponding author email: msuhl@iu.edu
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Background:
Maternal and child health (MCH) clinics represent an integrated approach for providing healthcare to pregnant women and children 0-59 months of age. Although MCH clinics are also charged with monitoring child development, which involves tracking developmental milestones, it is unclear how these services are provided or perceived within the clinic. This study aimed to describe self-reported knowledge, perceptions, and practice of developmental monitoring in selected MCH clinics in western Kenya.
Methods:
This cross-sectional descriptive study was conducted within six clinics. We administered a descriptive survey to measure caregiver and healthcare staff attitudes towards and awareness of developmental monitoring; we also reviewed MCH booklets to identify services received at the clinic. Data collection occurred over a period of one day at each of the six clinic sites. The data were analyzed using descriptive statistics.
Results:
During the study period, 78 caregiver-child pairs presented to the clinics and had their MCH booklets reviewed. The median child age was three months (interquartile range [IQR]: 1-8 months). Most caregivers were aware of weight monitoring and immunization services; however, when asked specifically about developmental monitoring, only 2.6% of caregivers were aware this service was available at the clinics. Nearly 80% of caregivers reported that they would be very interested in developmental monitoring services. Thirty-three MCH healthcare staff were interviewed about services provided and goals of clinical care. Fewer healthcare staff (60.6%) identified their roles in developmental monitoring compared to their roles in growth (90.9%) and nutritional monitoring (84.8%). Developmental milestones had not been recorded in any of the 78 MCH booklets. However, 78.1% of healthcare staff indicated support for developmental screening.
Conclusion and Global Health Implications:
While developmental monitoring was valued by healthcare providers, it was not consistently performed at the six clinics in our study. We recommend further work to raise awareness about developmental monitoring and to measure the implications of increased caregiver knowledge and perceptions on developmental monitoring practice.
Keywords
Child development
Development monitoring
Child health
Growth monitoring and promotion
Kenya
Screening
1. Introduction
Well-baby clinics offer caregivers direct contact with healthcare staff during the early growth and development of their children.1, 2 During these visits, medical professionals recognize and treat illnesses, screen for growth and developmental delays, and provide health education to the child’s caregiver. Although there is limited data to evaluate the quality of care received by babies who visit the well-baby clinics generally, there is evidence that early childhood development and the monitoring of developmental milestones are evaluated less consistently than linear and ponderal growth. A 2018 study in South Africa found that immunization and weight monitoring were performed for almost all babies, but developmental milestones were assessed in only 34% of babies.3 Another study showed that only 26% of children were assessed for developmental milestones.4 Even in high-resource settings, developmental monitoring may be inconsistent—one study in the United States found that only 57% of mothers reported that their babies had ever received developmental screening in a pediatric office.5 Paired with nutrition, early childhood development interventions have shown promise for improving developmental outcomes.6, 7 However, children cannot be directed towards these interventions without early recognition of developmental delay.
In Kenya, well-baby services are offered through integrated clinics called maternal and child health (MCH) clinics. Growth charts are a central tool in these clinics and are included in the Kenya Ministry of Health-sponsored Mother and Child Health Booklet (MCH booklet).8, 9 In addition to age- and sex-specific growth charts, the MCH booklet includes birth history, the immunization schedule, illness records, and a checklist of developmental milestones. The MCH booklet were introduced in Kenya to ensure continuity of care between the prenatal period and postnatal life,8 and a recent systematic review suggests that the use of such booklets improves vaccination adherence and breastfeeding practices.10 During each visit, an MCH staff member—often a trained nurse—takes a history from the mother, examines the baby, and records findings in the booklet. The healthcare staff then implements interventions or connects the family to services and offers health education as needed.
MCH clinics are established in most public health facilities in Kenya and represent an opportunity for the early identification of children who have growth faltering and developmental delays.1 The extent to which MCH clinics deliver their mandate, however, is not known. The objective of this study was to describe the knowledge, perceptions, and practice of caregivers and healthcare staff around services offered at well-baby clinics, with a particular emphasis on developmental monitoring.
2. Methods
This cross-sectional observational study was conducted in six clinics in Bungoma, Nandi, Trans Nzoia, and Uasin Gishu counties in western Kenya between November 7 and December 7, 2016. Within each of these clinics, 1-2 days per week are designated as pediatrics clinic, when caregivers bring their infants and children, and the other days are primarily focused on prenatal care services. Study activities occurred at each clinic during one of their pediatric clinic days, from opening (approximately 9:00 AM) to close (approximately 5:00 PM). During pediatric clinic days, approximately 10-30 caregivers and their children attend these clinics, and clinics are usually staffed by 5-8 healthcare staff, typically including clinical officers, nurses, counselors, nutritionists, and mentor mothers. Caregivers were eligible to participate in the study if they were seeking care for a child under five years of age and identified the MCH clinic as their primary clinic on the pre-determined day a member of the study staff was present. All healthcare staff working at the MCH clinic on the pre-determined interview dates were eligible to participate; as such, the participants included constitute a convenience sample of caregivers and staff in this region. Written informed consent was obtained from all participants. No staff member declined to participate, and only one caregiver declined to participate, citing time constraints.
For both caregivers and MCH staff, data were collected through a brief verbal interview guided by a custom questionnaire that included both coded and open-ended questions. A single interviewer conducted all interviews in this study. For caregivers, data collected included demographic information, reasons for MCH clinic attendance, and knowledge and perceptions around specific services. Caregivers were additionally asked whether they had concerns about their child’s development, and where they would seek guidance if they had concerns about their child’s development. For staff, data collected included information about demographics and occupation, knowledge and perceptions around clinic services, and specific practices in developmental monitoring. Additional data were abstracted from each child’s MCH booklet using a checklist to indicate whether a particular intervention had been documented. The age at which the following developmental milestones are achieved should be recorded in the MCH booklet: social smile, head control, turning head to sound, extend hand to grasp toy, sitting, standing, walking, and talking. Responses to open-ended questions were binned for analytic purposes using common key words to form categories. Demographic characteristics and survey responses were assessed using frequencies and percentages. Summary data and plots were created using R 4.0.0 (R Core Team, 2020). This study was approved by ethics committees at Moi University in Kenya (IREC/2016/171) and at the Indiana University School of Medicine (1609357843).
3. Results
3.1. Knowledge and perceptions of caregivers
A total of 78 caregivers with their children were interviewed. The plurality of caregivers (46.2%) were between 25 and 29 years old, and the median age of children attending the MCH clinic was three months (interquartile range [IQR]: 1-8 months). All caregivers were female, and 24 (30.8%) had at least one other child under five years of age living in their households.
Caregivers identified weight monitoring (77/78, 98.7%), nutrition (29/78, 37.2%), prevention of mother-to-child HIV transmission (pMTCT) (7/78, 9.0%), vitamin A supplementation (6/78, 7.7%), and developmental monitoring (2/78, 2.6%) as the services offered in the clinic (Figure 1). Caregivers most often cited weight monitoring and immunization as reasons for bringing their babies to the clinic (Figure 1).
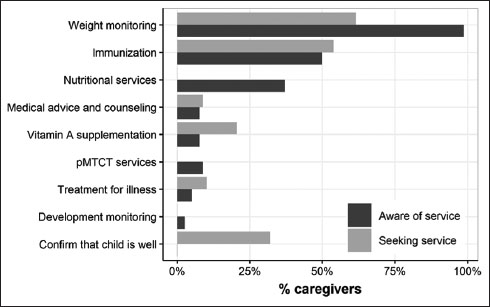
- Caregiver knowledge of MCH services and reasons for attending MCH clinics, pMTCT = prevention of mother-to-child HIV transmission, MCH- maternal-child health.
Although only two caregivers identified developmental screening as services provided at MCH clinics, 62 caregivers (79.4%) indicated that they would like developmental screening services to be provided. Only two caregivers (2.6%) indicated that they were not interested in developmental screening; both cited concerns about the duration of the visit. In all, 94.9% of caregivers (74/78) had no concerns about their child’s current development. When asked whom they would discuss developmental concerns with, 76.9% (60/78) said that they would consult a healthcare provider, while 20.5% (16/78) would consult with a family member, including the father or grandparent of the child.
3.2. Knowledge, perceptions, and practice of healthcare staff
Thirty-three healthcare staff were on duty in the six MCH clinics during the pre-specified interview days, and all agreed to be interviewed. Nearly all (32/33) were female; 17 (56.7%) were nurses, five (16.7%) were nutritionists, and four (13.3%) were pMTCT counsellors. Others were clinical officers, counsellors, and mentor mothers. The majority (63.6%) had worked in the unit between one and three years. Nineteen people (57.6%) were involved in anthropometric measurements, 18 (54.5%) performed record keeping, 13 (39.4%) performed pMTCT services, and 10 (30.3%) were involved in nutrition counselling. Respondents were also involved in patient check-in, home visits, health education, treatment and immunization, and antenatal services. None were explicitly involved in developmental monitoring.
The majority of the staff mentioned growth monitoring (30/33, 90.9%), nutrition (28/33, 84.8%), pMTCT services (32/33, 97.0%), and development monitoring (20/33, 60.6%) as services the MCH clinic provides (Figure 2). There were 78.1% (25/32) who said that they would be willing to conduct a child development screening using a set of four or five questions. Those who did not indicate that they would be willing to conduct the screening cited concerns about workload. The majority of staff members (22/33, 66.7%) thought they could identify resources to assist children with developmental delays in the community. Staff reported that they would refer children with developmental delay to physicians (19/22, 86.4%), nurses (1/22,4.5%), and physical therapists (2/22, 9.1%).
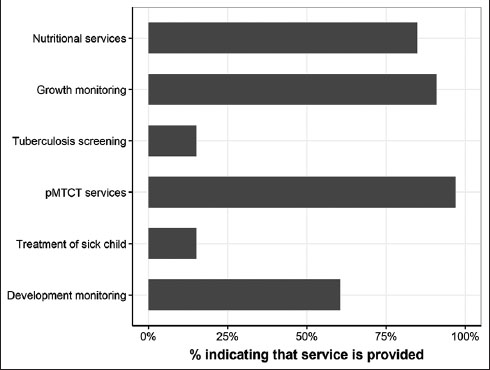
- Awareness of healthcare staff of services offered at the clinic, pMTCT = prevention of mother-to-child HIV transmission.
Twenty-six staff members (78.8%) reported that they were involved in entering data into the MCH booklet. Staff most often indicated that they recorded anthropometry (15/26, 57.7%) and immunizations (15/26, 57.7%); only two staff members (2/26, 8.0%) indicated that they often completed the page of the booklet that included developmental milestones. When asked directly whether they fill in data on child development, 21 (21/26, 80.8%) said yes. However, the analysis of the booklets revealed that the section on developmental milestones was not completed in any of the MCH booklets.
4. Discussion
Even as child mortality falls in low-resource countries, social and economic inequalities persist, including increased loss of developmental potential among the very poorest children in the world.7, 11 In clinical practice, we have observed that this aspect of child health has received less attention from caregivers and clinicians than infectious disease prevention, nutrition, and growth. In our study, only two caregivers recognized screening for developmental delay as a core service of the MCH, and none said that they attended the clinic expressly for developmental delay screening. However, more than half of MCH staff reported that their clinic provides screening for developmental delays and that they personally assess children. The discordance between documentation and staff report may imply that staff assess development, but do not fill out the MCH booklet, or that they informally gather information about development over the course of the visit. However, it is also possible that developmental screenings are performed only intermittently or rarely.
Although caregivers were generally unaware of existing developmental delay screening services, nearly all expressed acceptance of these services. This finding is consistent with a study from the United States, which also found that parents desired additional attention to their children’s developmental needs.12 As in our study, healthcare staff often voiced concerns about time constraints as a barrier to formal screening.12 Our study suggests a need for additional MCH staff sensitization to the benefits of services for developmental delay and their role in referral.
This study provides new data on the knowledge, perceptions, and practice of child development MCH services in western Kenya. However, our study is limited in a number of ways. First, because of time and resource constraints, we relied upon a convenience sample of respondents. As such, respondents may not be representative of all caregivers and MCH staff. Although all eligible caregivers were invited to participate, and although participation rates were very high, our respondents were primarily caregivers to young infants (<6 months of age). These children had not yet reached the typical age for many developmental milestones (i.e., standing, walking, talking), and it is possible that caregivers and staff pay more attention to these later milestones than to early ones.
Additionally, because we were not expecting all MCH booklets to be missing information on developmental screenings, the MCH staff interview was not structured in a way to directly ascertain why staff reports and records were discrepant. Because this data was collected in 2016, it is possible that clinical practice has changed in the intervening years; in Siaya County, Kenya, for example, nurturing care and childhood development have recently started to receive wider consideration and additional resources.13 However, we do not have any reason to believe that practice has changed significantly in the areas where this study took place. Future research should focus on ascertaining specific activities MCH staff carry out for developmental screening.
5. Conclusion and Global Health Implications
In conclusion, Kenya’s MCH clinics have the potential to improve the provision of preventive health services for children 0-59 months of age, increasing their survival and improving developmental outcomes. However, we observed that the clinics’ stated goals were not met in clinical practice. Although growth was routinely measured and immunizations were appropriately administered, there was no documentary evidence that children were assessed for developmental delay.
Acknowledgements:
We would like to thank and acknowledge the clinics who allowed us to visit their sites for study data collection. We would also like to thank the caregivers who took time to participate in our study.
Compliance with Ethical Standards
Conflicts of Interest: All authors have no conflicts of interest to disclose.
Financial Disclosure: All authors have no financial disclosures.
Funding/Support: This study was in part by a training grant entitled “Training in STIs and Other Infections of Global Health Significance” (T32AI007637, PI: Dr. Wools Kaloustian) from the National Institute of Allergy and Infectious Diseases, Bethesda, MD, USA and the Indiana University Morris Green Physician Scientist Program, both awarded to MM during her time as a fellow. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Ethics Approval: This study was approved by ethics committees at Moi University in Kenya (IREC/2016/171) and at the Indiana University School of Medicine (1609357843).
Disclaimer: None.
References
- A guide for monitoring child development in low- and middle-income countries. Pediatrics. 2008;121(3):e581-9. doi:10.1542/peds.2007-1771
- [Google Scholar]
- Primary care services promoting optimal child development from birth to age 3 years:review of the literature. Arch Pediatr Adolesc Med. 2001;155(12):1311-22. doi:10.1001/archpedi.155.12.1311 PMID:11732949
- [Google Scholar]
- Quality of care offered to children attending primary health care clinics in Johannesburg. SA Journal of Child Health. 2010;4(3):5.
- [Google Scholar]
- Monitoring well-baby visits in primary health care facilities in a middle income country. South African Journal of Child Health. 2018;12(2) doi:10.7196/SAJCH.2018.v12i2.1262
- [Google Scholar]
- Assessing development in the pediatric office. Pediatrics. 2004;113(6 Suppl):1926-33.
- [Google Scholar]
- Global health and development in early childhood. Annu Rev Psychol. 2015;66:433-57. doi:10.1146/annurev-psych-010814-015128
- [Google Scholar]
- Strategies for reducing inequalities and improving developmental outcomes for young children in low-income and middle-income countries. The Lancet. 2011;378(9799):1339-1353. doi:10.1016/s0140-6736(11)60889-1
- [Google Scholar]
- Enhancing Maternal and Child Health using a Combined Mother &Child Health Booklet in Kenya. J Trop Pediatr. 2015;61(6):442-7. doi:10.1093/tropej/fmv055
- [Google Scholar]
- Mother &child health booklet (Afya ya mama na mtoto) 2013
- Are Parent-Held Child Health Records a Valuable Health Intervention?A Systematic Review and Meta-Analysis. Int J Environ Res Public Health. 2019;16(2) doi:10.3390/ijerph16020220
- [Google Scholar]
- Child development:risk factors for adverse outcomes in developing countries. The Lancet. 2007;369(9556):145-157. doi:10.1016/s0140-6736(07)60076-2
- [Google Scholar]
- Challenges to implementation of developmental screening in urban primary care:a mixed methods study. BMC Pediatr. 2014;14:16. Published 2014 Jan 21 doi:10.1186/1471-2431-14-16
- [Google Scholar]





