Translate this page into:
Postpartum Hemorrhage in Humanitarian Settings: Heat-Stable Carbetocin and Tranexamic Acid Implementation Study in South Sudan

*Corresponding author: Nguyen Toan Tran, The Australian Centre for Public and Population Health Research (ACPPHR) Faculty of Health, University of Technology, Sydney, NSW, Australia. Tel: +1 929 523 5158 nguyentoan.tran@uts.edu.au
-
Received: ,
Accepted: ,
How to cite this article: Tran NT, Ochan AW, Sake J, Sukere O, Zeck W, Seuc A, et al. Postpartum hemorrhage in humanitarian settings: Heat-stable carbetocin and tranexamic acid implementation study in South Sudan. Int J MCH AIDS. 2024;13:S55-63. doi: 10.25259/IJMA_8_2023
Abstract
Background and Objective
Postpartum hemorrhage (PPH) remains a significant concern in crisis-affected contexts, where the implementation of heat-stable carbetocin (HSC) and tranexamic acid (TXA) for PPH prevention and treatment lacks evidence. This study aims to evaluate the effects of a capacity-strengthening package on the use of uterotonics for PPH prevention and detection, and the use of TXA for PPH treatment in basic maternity facilities in South Sudan.
Methods
In this implementation study, the six chosen facilities followed a stepwise sequence of PPH management: T1 (routine care), a transition period for package design; T2 (package without HSC and TXA); T3 (package and HSC); and T4 (package with HSC and TXA). The intervention comprised refresher training, an online provider community, PPH readiness kits, alarm bells, and displayed algorithms. The main outcomes were trends in prophylactic uterotonic use, including HSC, visual diagnosis of bleeding, and oxytocin and TXA use for PPH treatment. Analyses were adjusted for cluster effect and baseline characteristics. The study was registered in the Pan-African Clinical Trials Registry (PACTR202302476608339).
Results
From February 1, 2022, to February 17, 2023, 3142 women were recruited. Nearly all women received prophylactic uterotonics across all four phases, with a significant increase after T3 (T4-T1: 100%–98%; 95% CI: 4.4–0.4). Oxytocin alone was the most used in T1 (98%) and T2 (94%) and HSC alone in T3 (87%) and T4 (82%) (T4-T1: 95% CI: 75.5–83.3). PPH diagnosis tripled from 1.2% of all births to 3.6% (T2-T1: 95% CI: 0.4–5.2) and stayed roughly at 3% in T3 and T4. For treatment, universal oxytocin use in T1 and T2 decreased in T3 upon HSC initiation (T3-T2: 27%–100%; 95% CI: 95.5–49.9), whereas TXA use increased in T4 (T4-T1: 95%–0%; 95% CI: 54.6–99.0).
Conclusion and Global Health Implications
An intervention package to improve the quality of PPH prevention and treatment can effectively increase HSC and TXA use in crisis settings. It could be scaled up in similar contexts with ongoing supervision to mitigate confusion between the existing and new medications, such as the reduced use of oxytocin for PPH treatment. Sustaining cold chain investments remain vital to ensure oxytocin quality.
Keywords
Health Services Research
Postpartum Hemorrhage
Heat-Stable Carbetocin
Tranexamic Acid
Public Health Intervention Package
Humanitarian Settings
Fragile Settings
INTRODUCTION
Primary postpartum hemorrhage (PPH) is defined as excessive blood loss (≥ 500 mL after vaginal birth or ≥ 1000 mL after cesarean birth) within 24 hours.[1] PPH contributes to over 25% of maternal deaths worldwide, primarily in low- and middle-income countries affected by fragility and humanitarian disasters.[2]
Primary causes of PPH include uterine atony, trauma, retained placenta, tears, uterine rupture, clotting disorders, and uterine inversion.[3] Active management of the third stage of labor (AMTSL) can prevent most PPH deaths.[4] AMTSL includes prophylactic uterotonic use, delayed cord clamping, and controlled cord traction (if skilled attendants are available).[4] Oxytocin (10 IU, IM/IV) is the preferred uterotonic in settings with multiple options but requires cold-chain storage.[1,5] Heat-stable carbetocin (HSC), a long-acting oxytocin analog not requiring cold chain storage, is recommended for PPH prevention and was found cost-effective in reducing the number of PPH events and deaths as well as public healthcare system costs in India.[6–8] Studies, including a 2018 trial by the World Health Organization (WHO), have shown HSC effectiveness and noninferiority to oxytocin in preventing PPH in low-income countries.[9]
Prompt action is crucial for managing PPH.[10] WHO recommends a multidisciplinary approach, including fluid replacement and additional uterotonic administration (following the initial dose for PPH prevention) as the primary interventions.[1,5] Tranexamic acid (TXA), an antifibrinolytic agent, reduces bleeding risk in surgery and trauma.[11,12] It does not require cold chain, is affordable ($1.30 per 1 g ampoule), and is readily available in hospitals.[7] In obstetric care, TXA effectively controls bleeding in women with PPH regardless of the underlying cause.[13]
A 2018 Cochrane Review by Gallos et al. found that oxytocin, misoprostol, ergometrine, and HSC were generally effective for PPH prevention, with HSC being potentially more effective than oxytocin without an increase in side effects.[14] The review by Gallos et al. primarily relied on data from the 2018 trial by Widmer et al., which was conducted across 21 countries with varying income levels and in hospital settings.[9,14] It aimed to compare HSC with oxytocin for PPH prevention. In another 2018 Cochrane Review by Shakur et al., prompt administration of intravenous TXA after the onset of bleeding was found to decrease primary PPH mortality in vaginal and cesarean births without raising thromboembolic risks.[15] Additionally, in 2022, two scoping literature reviews highlighted the need for implementation research for PPH interventions, including HSC and TXA, in low-resource settings lacking cold chain systems.[16,17]
We searched PubMed using the term “randomized controlled trial” combined with “postpartum,” “hemorrhage,” “vaginal,” and “carbetocin” or “tranexamic” for publications in English, focusing on trials in low-income countries (as defined by the World Bank) over the past ten years.[18] We identified one trial since the 2022 scoping literature reviews—the E-MOTIVE trial (Early Detection of Postpartum Hemorrhage and Treatment), which took place in secondary-level hospitals in Kenya, Nigeria, South Africa, and Tanzania.[19] E-MOTIVE aimed to test a package of interventions to identify and treat PPH. It found that detecting PPH early using a calibrated blood-collection drape and implementing bundled treatments (uterine massage, oxytocic drugs, TXA, intravenous fluids, examination, and intervention escalation) resulted in a reduced risk of severe PPH, laparotomy for bleeding, or bleeding-related death compared to standard care in women undergoing vaginal delivery.
Hence, there is a gap in the current evidence base, including in humanitarian and fragile settings such as South Sudan, detailing programmatic approaches to introduce HSC and TXA and enhance providers’ capacity to do so, particularly in nonhospital environments.
In light of this context, the overall aim of our implementation research was to investigate the influence of a capacity-strengthening package that includes HSC and TXA for PPH on the use of uterotonics (including HSC) for PPH prevention, detection, and use of uterotonics and TXA for PPH treatment in cold chain-challenged Basic Emergency Obstetric and Newborn Care (BEmONC) facilities. These facilities are often found in humanitarian settings. Our implementation research is based on the hypotheses that the package would enhance the quality of PPH care, integrate healthcare provider perspectives, align with national health policies, and address resource limitations, particularly in humanitarian and fragile contexts.
Newly independent in 2011, South Sudan grapples with severe maternal health issues and had the world’s highest maternal mortality ratio at 1223 deaths per 100,000 live births in 2020.[2] Only 28% of births occurred in health facilities, and approximately 30% of married or in-union women in 2020 had unmet family planning needs.[2,20,21] Merely 29% of women are literate as of 2019.[21] With a population of 12.4 million, South Sudan shelters nearly 2.3 million Internally Displaced Persons (IDPs) and 308,000 refugees, constituting part of the 9.1 million people requiring humanitarian aid as of April 2023.[22] Challenges in providing reproductive, maternal, neonatal, child, and adolescent health services stem from a scarcity of personnel, limited medical resources, and insufficient national funding.[23] These hurdles are linked to the suspension of oil production in 2012, ongoing conflicts, governance deficiencies, a lack of accountability, and limited human resources, collectively resulting in inadequate healthcare and low service utilization.[23]
METHODS
Study Design and Participants
This study drew from implementation research principles, that is, to understand what, why, and how interventions work in “real world” settings and test approaches to improve them.[24] It was a pragmatic, multi-intervention, multi-stepped, cluster, non-blinded, non-randomized, controlled, quasi-experimental trial applied to six BEmONC health facilities across South Sudan. This approach was justified since some intervention components were applied at the facility level (e.g., service provider refresher training) and not directly to individual participants.
The research was conducted in six BEmONC facilities located in areas serving IDPs: Bentiu 1, Bentiu 2, Juba, Malakal, Mingkaman, and Wau. Facilities were eligible if they were BEmONC-only, experienced cold storage disruptions in the three months prior to enrollment, and were willing to participate. Facilities offering cesarean sections and blood transfusions, part of Comprehensive Emergency Obstetric and Newborn Care (CEmONC) services, were excluded. All eligible women arriving for childbirth were invited to participate, with no exclusion criteria except for refusal to provide informed consent (and assent for minors under 18).
Stepwise Approach
All study sites followed the same sequence [Figure 1]: Step 1 (T1) involved a four-week routine care period (see below). This was followed by a six-month intervention design and training phase (T2). Step 2 (T2) featured a four-week intervention package with refresher training for facility providers but without HSC and TXA. Step 3 (T3) included an eight-week intervention package with HSC but no TXA. Step 4 (T4) included an eight-week intervention package with both HSC and TXA.
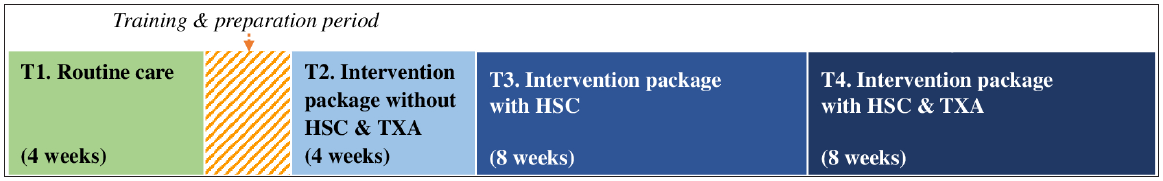
- The four steps of the study, T1-T4. HSC: Heat-stable carbetocin, TXA: Tranexamic acid.
Intervention
Our PPH package included five components introduced from T2 onwards. First, we aimed to enhance knowledge and skills through refresher training of service providers (component one of the packages). This training focused on providing hands-on PPH management skills, including visual estimation of blood loss, incorporating HSC and TXA using a low-dose and high-frequency training strategy (self-study and webinar for two weeks, a two-day in-person workshop, and monthly postworkshop, facility-based knowledge review and skill drills). Additionally, a WhatsApp-based Community of Practice, where participants posted questions, answers, and experiences related to PPH management, was moderated by the national study coordinator (component two). Furthermore, we either repackaged or provided key materials and supplies, including readying PPH treatment kits containing uterotonics (component three), and TXA once made available in T4, IV/IM materials, and equipment for emptying the bladder, examination, uterine balloon tamponade, and manual removal of the placenta; a 24/7 bell for calling assistance in the delivery room (component four); and displayed PPH prevention and treatment algorithm posters in the delivery room (component five). Routine care adhered to national guidelines, involving oxytocin and misoprostol as uterotonics and other necessary materials, although not assembled in PPH treatment kits.
Outcomes
The primary outcomes were assessed as follows: (i) the proportion of women receiving uterotonics for PPH prevention, categorized by the type of uterotonic; (ii) the proportion of visually diagnosed PPH cases; (iii) the proportion of diagnosed PPH cases treated with oxytocin; and (iv) the proportion of clinical PPH cases treated with TXA. Due to time and resource limitations, quantitative indicators were collected using facility reporting forms based on existing maternity registers and not individual participant case report forms. The national research coordinator meticulously reviewed all submitted copies, identified inconsistencies, and collaboratively addressed them with facility providers prior to transmitting the copies to the data manager.
Statistical Analysis
Assumptions were based on prospective data and literature from Uganda (no published paper from South Sudan).[25] It conservatively assumed that only 30% of women received uterotonics for PPH prevention in T1, increasing to 60% in T2–T4.[25] The total sample size across all facilities and phases was at least 504 (four phases * 126/phase). As there were six facilities and each of the four periods had a duration of two months, each facility needed at least 10.5 deliveries each month (504/6 facilities * four phases * two months) (based on results using the pwr package in R).[26] This allowed for a statistical power of 80% to detect a difference of 30% (60%–30%) to a two-sided significance level of 5% and a design effect of 3. An approximate design effect of 3 was obtained assuming an intracluster coefficient (ICC) of 0.02, sample size within each facility, and each period m = 89 (using the most conservative scenario of 30%–40% increase). Therefore, the design effect was = 1+ ([m-1]*ICC) = 2.76. We overestimated the design effect to increase the sample size within reasonable limits. In reality, the difference between T1 and T2–T4 in terms of the use of uterotonics was larger than the assumed 30%, which ultimately made a design effect of 1.5 more acceptable. The design effect was necessary because our sample consisted of clusters rather than a simple random sample.
Data analysis employed IBM SPSS Statistics, version 25.0 (IBM Corp. Released 2017. IBM SPSS Statistics for Windows, Version 25. 0. Armonk, NY: IBM Corp.) and WINPEPI (PEPI-for-Windows, version 11.50). Participants were assigned to one of the four phases based on clinic attendance. Overall proportions for key outcomes in each phase were calculated. A design effect of 1.5 was applied to account for facility clustering when comparing proportions between phases. Two-wise comparisons of proportions were performed using WINPEPI. To ensure result comparability, prevalences in T2–T4 were standardized using the T1 sample as a reference, considering variables such as age, gestational age, and parity. Missing data were not imputed. The reporting follows the Transparent Reporting of Evaluations with Nonrandomized Designs (TREND) statement,[27] enhancing the CONsolidated Standards Of Reporting Trials (CONSORT) statement for randomized controlled trials and its cluster study extension.[28]
Ethical Approval
Study approval was obtained by the ethics committee in South Sudan (RERB NO: 32/21/07/2022–MOH/RERB/29/2022).
RESULTS
Sociodemographic Characteristics
From February 1, 2022, to February 27, 2023, 3142 women from six facilities were enrolled in the study: 526 in T1, 532 in T2, 1136 in T3, and 948 in T4. There were no notable differences in participants’ baseline characteristics across phases in terms of age, gravidity, parity, gestational age, delivery mode, and living status upon discharge [Table 1].
| T1 (baseline) | T2 (post-training) | T3 (+HSC only) | T4 (+HSC & TXA) | |
|---|---|---|---|---|
| N | (N = 526) | (N = 532) | (N = 1136) | (N = 948) |
| Age: median (IQR) | 24 (20–30) | 23 (19–28) | 24 (19–30) | 24 (20–30) |
| Gravidity: median (IQR) | 3 (2–5) | 3 (1–5) | 3 (1–5) | 3 (2–5) |
| Parity: median (IQR) | 3 (1–4) | 2 (1–4) | 2 (0–4) | 2 (1–4) |
| Gestational age: median (IQR) | 38 (38–39) | 38 (38–39) | 38 (38–39) | 38 (38–40) |
| Delivery mode: n/N (%) | ||||
| Spontaneous vaginal delivery | 523/526 (99.4) | 521/532 (97.9) | 1119/1136 (98.5) | 929/948 (98.0) |
| Assisted | 0/526 (0.0) | 1/532 (0.2) | 1/1136 (0.1) | 1/948 (0.1) |
| Breech | 0/526 (0.0) | 4/532 (0.8) | 3/1136 (0.3) | 14/948 (1.5) |
| Cesarean section | 2/526 (0.4) | 6/532 (1.1) | 12/1136 (1.1) | 4/948 (0.4) |
| Unknown | 1/526 (0.2) | 0/532 (0.0) | 1/1136 (0.1) | 0/948 (0.0) |
| Women alive at discharge: n/N (%) | ||||
| Yes | 526/526 (100.0) | 532/532 (100.0) | 1136/1136 (100.0) | 942/948 (99.4) |
| Unknown | 0/526 (0.0) | 0/532 (0.0) | 0/1136 (0.0) | 6/948 (0.6) |
HSC: Heat-stable carbetocin, TXA: Tranexamic acid, IQR: Interquartile range, n: Number of observations, N: Total number of participants in time period, T1: Time period 1, T2: Time period 2, T3: Time period 3, T4: Time period 4.
Main Outcome Results
Primary outcomes are presented in Table 2. Almost all women received prophylactic uterotonics to prevent PPH across all phases, with a small but statistically significant increase after T3. There was a significant change in the types of administered uterotonic before and after HSC introduction: oxytocin alone was the most used in T1 ([97%] 487/500) and T2 ([93%] 464/497) and HSC alone in T3 ([86%] 935/1079) and T4 ([80%] 772/942). There were rare cases of combined uterotonics (data not shown): predominantly oxytocin with misoprostol in T2–T3 (0.1%–3.2%, unadjusted) and HSC with either oxytocin or misoprostol in T3–T4 (0.1%–0.6%, unadjusted). There was no reported use of HSC for treatment or of TXA for the prevention of PPH.
| T1 (baseline) | T2 (post-training) | T3 (+HSC only) | T4 (+TXA & HSC) | Treatment differences 95% CI† | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| T2-T1 | T3-T1 | T4-T1 | T3-T2 | T4-T2 | T4-T3 | |||||
| Uterotonics for PPH prevention* | ||||||||||
| None: n/N (%) | 12/500 (2.4) | 12/497 (2.4) | 2/1079 (0.1) | 0/942 (0.0) | (-2.8 to 2.9) | (-4.3 to -0.2) | (-4.4 to -0.4) | (-4.3 to -0.2) | (-4.4 to -0.4) | (-0.5 to 0.2) |
| HSC alone: n/N (%) | 1/500 (0.2) | 2/497 (0.2) | 935/1079 (86.0) | 772/942 (79.6) | (-0.8 to 1.0) | (82.6 to 88.9) | (75.5 to 83.3) | (82.6 to 88.9) | (75.5 to 83.3) | (-11.3 to -1.4) |
| Oxytocin alone: n/N (%) | 487/500 (97.4) | 464/497 (93.0) | 129/1079 (11.5) | 169/942 (19.7) | (-8.4 to -0.4) | (-89.4 to -82.4) | (-82.0 to -73.4) | (-85.9 to -77.1) | (-78.4 to -68.2) | (3.4 to 13.0) |
| Visually diagnosed with PPH*: n/N (%) | 6/500 (1.2) | 16/497 (3.6) | 33/1079 (2.9) | 40/942 (3.4) | (-0.4 to 5.2) | (-0.4 to 3.7) | (-0.1 to 4.4) | (-3.6 to 2.1) | (-3.2 to 2.8) | (-1.8 to 2.8) |
| For women with PPH** | ||||||||||
| Oxytocin administered - n/N (%) | 6/6 (100.0) | 16/16 (100.0) | 9/33 (27.3) | 29/40 (72.5) | NA | (-95.5 to -49.9) | (-48.2 to -6.7) | (-95.5 to -49.9) | (-48.2 to -6.7) | (14.4 to 76.0) |
| TXA administered - n/N (%) | 0/6 (0.0) | 9/16 (56.3) | 6/33 (18.2) | 38/40 (95) | (19.8 to 92.7) | (-1.6 to 37.9) | (84.9 to 100.0) | (-79.5 to 3.4) | (0.9 to 76.6) | (54.6 to 99.0) |
Notes: * Prevalences and 95% CI of treatment differences were adjusted via standardization by age, gestational age, and parity (using T1 as the standard population); a design effect of 1.5 was used to account for clustering of participants within facilities. ** Outcomes for women with PPH could not be adjusted by standardization due to small sample sizes involved, but 95% CI were adjusted to account for clustering of participants within facilities, using a design effect of 1.5. † No color: p > 0.05; in color: p < 0.05. HSC: Heat-stable carbetocin, TXA: Tranexamic acid, PPH: Postpartum hemorrhage, CI: Confidence interval, n: Number of observations, N: Total number of participants in time period, NA: Not applicable as difference=0, T1: Time period 1, T2: Time period 2, T3: Time period 3, T4: Time period 4.
The proportion of women visually diagnosed with PPH changed across phases, with an increase, although not statistically significant, between baseline T1 ([1%] 6/500) and post-training T2 ([4%] 16/497) as well as the following phases.
As part of the treatment of women with PPH, oxytocin was used universally in T1 (6/6) and T2 (16/16). However, its use decreased to 27% (9/33) in T3 and increased again in T4 but only to 73% (29/40), and not 100%, as was prior to the introduction of HSC. The differences in oxytocin use across phases were statistically significant (p < 0.05). The changes in TXA use were also statistically significant: 0% (0/6) in T1, 56% (9/16) in T2, 18% (6/33) in T3, and 95% (38/40) in T4. There were no adverse events related to the study and all participants were discharged alive.
DISCUSSION
Overall, our results showed that in humanitarian settings in South Sudan, where the availability of cold chain and cold storage is often unreliable, an HSC- and TXA-inclusive package of PPH prevention and treatment interventions that aimed at reinforcing providers’ capacity can change the trends in the type of uterotonic used for PPH prevention by replacing oxytocin with HSC, strengthen the visual diagnosis of PPH, and increase the uptake of TXA for PPH treatment. There was a momentary drop in oxytocin administration as treatment for women diagnosed with PPH coinciding with the introduction of prophylactic HSC. HSC was appropriately used for PPH prevention only and TXA was used appropriately for PPH treatment only.
To our understanding, our trial stands as one of the pioneering health implementation research studies at the primary care level conducted in South Sudan. Throughout the course of the study, we encountered various implementation challenges arising from the prevailing insecurity, characterized by intermittent intercommunal violence. This situation led to the displacement of communities into regions encompassed by our study sites, particularly Malakal, Bentiu, and Mingkaman. Adding to the complexity, severe flooding further exacerbated the circumstances. Given the dispersed nature of our study sites, we had to rely on air travel to commute between Juba and these locations. Due to the limited availability of flights and the occasional outbreaks of unrest and natural disasters, our WhatsApp-based Community of Practice proved invaluable in maintaining regular updates on the field situation, facilitating experience sharing, and promptly addressing any challenges that arose.
Uterotonic use for PPH prevention was already widespread at baseline, which is comparable to the results of the 2021 hospital-based EN-BIRTH study (Every Newborn Birth Indicators Research Tracking in Hospitals).[29] This study found that >99% of women in Bangladesh, Nepal, and Tanzania received uterotonic for PPH prevention. Introducing HSC did not decrease, but increased the prevalence of uterotonic use. Once given the choice, providers replaced oxytocin with HSC in most cases. The uptake was higher than planned and led to a shortage of HSC in T4, explaining the drop in HSC use and the increase in oxytocin use from T3 to T4. HSC has a longer half-life than oxytocin and misoprostol. The concomitant use of HSC with other uterotonics, such as oxytocin or misoprostol, has not been extensively researched and should not be recommended.[14] One study from Egypt examined the combination of oxytocin and carbetocin and observed an additive effect on preventing PPH during cesarean sections.[30] There were rare cases of combined HSC use in our study (no serious side effects were reported). Future training and ongoing supportive supervision should reinforce the importance of not combining HSC with other uterotonics for PPH prevention and the continuous relevance of oxytocin for PPH treatment.
The prevalence of PPH tripled between T1 and T2–T4 to approximately 3%. The PPH refresher training, which occurred before T2, may have contributed to the increase. The training included a skill drills station, where providers had to visually estimate different amounts of bleeding using drapes tainted with red-colored juice and clotted liquid in a dish. Most providers underestimated blood loss, a phenomenon documented in the literature—with accuracy as low as 28% in a study in Thailand.[31] Making trainees aware of their visual bias through short didactic and practical simulations effectively improves estimation and in our study, may have contributed to increased PPH detection.[32] However, the resulting detection rate of approximately 3% remains below the PPH prevalence reported globally (6%) and in sub-Saharan Africa (11%).[10] Calibrated drapes or other similar low-technology blood collection materials would be critical not only to document the incidence of PPH adequately but also to trigger detection and action in the treatment of PPH. Calibrated drapes were critical in the chain of PPH treatment measures illustrated in the 2023 E-MOTIVE study, which was based in referral hospitals.[19] The feasibility of calibrated drapes and other blood collection materials should be further researched in humanitarian and lower maternity care settings.
Almost all women with PPH received TXA after its official introduction in T4, although the strength of this evidence is low due to the small sample size. The study sites received supplies of both HSC and TXA before T2 to minimize transportation and logistics costs related to the option of delivering TXA just before T4. We reminded providers to use TXA only in T4. As providers were already trained on TXA usage during the refresher training before T2 started, a few administered it to women with PPH during T2, a trend that decreased in T3 after a reminder of the study’s stepwise approach during supportive supervision. Nonetheless, the mistimed use of TXA in T2 allows us to learn two implementation lessons. First, providers will likely use life-saving medications such as TXA as soon as these are available, despite reminders to wait until the right time. Second, the use of TXA for PPH treatment before introducing HSC for PPH prevention appears to have no adverse effect on the trends of oxytocin use for either PPH prevention or in particular, PPH treatment. What happened to the latter in T3 once HSC was introduced came as a surprise with valuable insights for future scale-up efforts.
Oxytocin is a cornerstone in PPH treatment, which appears to be universally applied in T1 and T2 (even when TXA is used for treatment). The alarming and significant drop in its use down to 27% of women diagnosed with PPH during T3 coincided with the introduction of HSC. However, the credibility of this finding is limited by the relatively low number of PPH cases in the study. We searched for and did not identify similar phenomena published in the literature. This may be because most studies focused on the safety and efficacy of PPH medications, not on how using one affected other available treatment of the PPH management toolkit. Supportive supervision offered insights into providers’ confusion: as both HSC and oxytocin are uterotonics and should not be used prophylactically together, a number of staff thought that oxytocin could not be used to treat PPH if HSC was used beforehand for PPH prevention. Close monitoring dispelled this misconception and allowed a more systematic use of oxytocin for treatment, which increased again in T4.
Strengths and Limitations of the Study
Our study has the added value of not being based in hospitals or middle- or high-income countries. It focused on BEmONC facilities operating in cold chain-challenged settings in low-income countries, specifically in fragile and humanitarian settings, making HSC and TXA fit-for-purpose in settings where the quality of medicines cannot be guaranteed.
Our study has several limitations. First, it was not randomized, involving only six clusters, which, though sufficient for our hypotheses, raises the risk of dissimilarities between groups. However, each cluster enrolled a large sample size and followed a similar phased approach. Age, gestational age, and parity were controlled for, with no significant resultant changes. Second, data relied on provider-reported indicators, potentially leading to reporting errors—but mitigated by weekly data reviews. The time of administering medication was not recorded. Third, blinding was not possible, resulting in potential assessment bias or the Hawthorne effect where participants modify behavior due to being monitored. However, high HSC and TXA uptake cannot be attributed solely to these factors. Fourth, we could not determine which specific intervention in the package had the most impact on HSC and TXA use, necessitating further research. However, interventions were chosen with inputs from stakeholders and integrated due to their suitability for resource-limited settings and capacity to enhance BEmONC services.
Conclusion and Global Health Implications
Despite these limitations, implementing an HSC and TXA-inclusive PPH intervention package in humanitarian settings significantly increased women’s access to HSC for PPH prevention and TXA for PPH treatment. Based on the current evidence and increasing availability and affordability of HSC and TXA for PPH management in high-mortality countries, policymakers from low-resource settings have various strategies for introducing these medications to prevent and treat PPH. Such strategies depend on health service and cold chain gaps, needs, and opportunities at different levels of care. One such strategy is the one this implementation research identified in humanitarian cold chain system-challenged settings—our strategy does not just “parachute” HSC and TXA but integrates them into a package of interventions to enhance the quality of PPH care. Additionally, replacing prophylactic oxytocin of unknown quality with HSC could significantly unburden cold chain storage systems in low-resource settings. The widespread adoption of this approach could mitigate the challenges associated with transporting and storing oxytocin for PPH prevention. However, effective scale-up necessitates (i) continuous capacity development for skill enhancement and addressing staff turnover; (ii) ongoing supportive supervision to reinforce clinical practices and dispel misconceptions; (iii) close monitoring and evaluation with revised maternity registers, capturing essential PPH indicators; and (iv) enhancing cold chain for oxytocin quality assurance, as it remains vital for PPH treatment. While further research is needed to determine cost-effectiveness, the nature of the interventions and the emphasis on strengthening PPH quality of care in existing cold chain-challenged BEmONC facilities could accelerate reductions in maternal mortality ratio in high-burden countries hosting humanitarian crises.
Key Messages
-
A package of postpartum hemorrhage (PPH) interventions reinforcing routine obstetric services can effectively increase the trends and change the types of uterotonics used for PPH prevention (by replacing oxytocin with HSC), increase the number of visually diagnosed PPH cases, and have tranexamic acid (TXA) used in most women with PPH.
-
The stepwise introduction of HSC and TXA in humanitarian and fragile settings is appropriate, feasible, and acceptable to providers.
-
Continuous capacity development and close monitoring is critical to prevent and correct confusion between existing and new medications.
Acknowledgments
We express our gratitude to Nadine Corner for conceptualizing the study and to Danielle Jurman and Agnes Chidanyika for effectively managing the in-country supply of both medications in a timely manner.
COMPLIANCE WITH ETHICAL STANDARDS
Conflicts of Interest
The authors declare no competing interests.
Financial Disclosure
Nothing to declare.
Funding/Support
Ferring Pharmaceuticals generously provided funding and supplies for the study components with HSC; the donor had no role in the design of the study and interpretation of the results. UNFPA Procurement Service Branch supported the implementation of the phase with TXA. The publication of this study was supported by funding from MSD through its MSD for Mothers initiative and is the sole responsibility of the authors. MSD for Mothers is an initiative of Merck & Co., Inc., Rahway, NJ, U.S.A.
Ethics Approval
The study strictly adhered to the ethical principles outlined in the Declaration of Helsinki and received approval from the ethics committee in South Sudan (RERB NO: 32/21/07/2022–MOH/RERB/29/2022).
Declaration of Patient Consent
Patient consent is not required as patients’ identity is not disclosed or compromised.
Use of Artificial Intelligence (AI)-Assisted Technology for Manuscript Preparation
The authors confirm that there was no use of AI-Assisted Technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The opinions expressed are those of the authors and do not necessarily reflect the views of the funding agencies. UNFPA is solely interested in studying the implementation of HSC and TXA from a public health and emergency response standpoint. The aim is to potentially include the drugs in the complementary items offered through UNFPA Procurement and Supply for certain contexts. It is important to note that the factors motivating UNFPA to consider adding HSC and TXA to its catalog for specific situations might differ from the considerations of national health authorities.
References
- WHO recommendations for the prevention and treatment of postpartum haemorrhage. Geneva: World Health Organization; 2012. [Accessed 2023 Nov 13]. Available from:https://www.who.int/reproductivehealth/topics/maternal_perinatal/pph-woman-trial/en/
- Trends in maternal mortality 2000–2020: Estimates by WHO, UNICEF, UNFPA, World Bank Group and UNDESA/Population Division. 2023.
- Postpartum hemorrhage: Epidemiology, risk factors, and causes. Clin Obstet Gynecol. 2010;53(1):147-56.
- [CrossRef] [PubMed] [Google Scholar]
- Active versus expectant management for women in the third stage of labour. Cochrane Database Syst Rev. 2019;2(2):CD007412.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- WHO recommendations: Uterotonics for the prevention of postpartum haemorrhage. Geneva: World Health Organization; 2018. [Accessed 2023 Nov 13]. Available from:https://apps.who.int/iris/bitstream/handle/10665/277276/9789241550420-eng.pdf
- WHO Model Lists of Essential Medicines, 21st List 2019. Geneva: World Health Organization; 2019. [Accessed 2023 Nov 13]. Available from:https://www.who.int/groups/expert-committee-on-selection-and-use-of-essential-medicines/essential-medicines-lists
- UNFPA Procurement Services: Product Catalogue 2021. [Accessed 2023 Nov 13]. Available from:www.unfpaprocurement.org/products.
- Cost-effectiveness and budget impact of heat-stable carbetocin compared to oxytocin and misoprostol for the prevention of postpartum hemorrhage (PPH) in women giving birth in India. BMC Health Serv Res. 2023;23(1):267.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Heat-stable carbetocin versus oxytocin to prevent hemorrhage after vaginal birth. N Engl J Med. 2018;379(8):743-52.
- [CrossRef] [PubMed] [Google Scholar]
- Epidemiology of postpartum haemorrhage: A systematic review. Best Pract Res Clin Obstet Gynaecol. 2008;22(6):999-1012.
- [CrossRef] [PubMed] [Google Scholar]
- Effect of tranexamic acid on surgical bleeding: Systematic review and cumulative meta-analysis. BMJ. 2012;344:e3054.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Antifibrinolytic drugs for acute traumatic injury. Cochrane Database Syst Rev. 2015;2015(5):CD004896.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Effect of early tranexamic acid administration on mortality, hysterectomy, and other morbidities in women with post-partum haemorrhage (WOMAN): An international, randomised, double-blind, placebo-controlled trial. Lancet. 2017;389(10084):2105-16.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Uterotonic agents for preventing postpartum haemorrhage: A network meta-analysis. Cochrane Database Syst Rev. 2018;12(12):CD011689.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Antifibrinolytic drugs for treating primary postpartum haemorrhage. Cochrane Database Syst Rev. 2018;2(2):CD012964.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Implementing heat-stable carbetocin for postpartum haemorrhage prevention in low-resource settings: A rapid scoping review. Int J Environ Res Public Health. 2022;19(7):3765.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Tranexamic acid for postpartum hemorrhage treatment in low-resource settings: A rapid scoping review. Int J Environ Res Public Health. 2022;19(12):7385.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- World Bank Group country classifications by income level for FY24 (July 1, 2023–June 30, 2024). World Bank Blog; [Accessed 2024 Mar 18]. Available from:https://blogs worldbank org/opendata/new-world-bank-group-country-classifications-income-levelfy24. 2023
- Randomized trial of early detection and treatment of postpartum hemorrhage. N Engl J Med. 2023;389(1):11-21.
- [CrossRef] [PubMed] [Google Scholar]
- United Nations Population Fund. Investment Cases Towards Ending Unmet Need for Family Planning, Preventable Maternal Deaths, and Gender-Based Violence; South Sudan Synthesis Report 2021. [Accessed 2023 Jun 18]. Available from:https://esaro.unfpa.org/sites/default/files/pub-pdf/south_sudan_synthesis_report.pdf.
- UIS Stat Bulk Data Download Service 2019. [Accessed 2023 Jun 18]. Available from:https://apiportal.uis.unesco.org/bdds.
- South Sudan: Humanitarian Snapshot (April 2023) 2023. [Accessed 2023 Jun 18]. Available from:https://reliefweb.int/sites/reliefweb.int/files/resources/south_sudan_humanitarian_snapshot_november_0.pdf.
- Health policy mapping and system gaps impeding the implementation of reproductive, maternal, neonatal, child, and adolescent health programs in South Sudan: A scoping review. Confl Health. 2020;14:1-16.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Implementation research: What it is and how to do it. BMJ. 2013;347:f6753.
- [CrossRef] [PubMed] [Google Scholar]
- A mixed-methods study of barriers and facilitators to the implementation of postpartum hemorrhage guidelines in Uganda. Int J Gynaecol Obstet. 2016;132(1):89-93.
- [CrossRef] [PubMed] [Google Scholar]
- Improving the reporting quality of nonrandomized evaluations of behavioral and public health interventions: the TREND statement. Am J Public Health. 2004;94(3):361-6.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Improving the reporting of pragmatic trials: An extension of the CONSORT statement. Bmj. 2008;337:a2390.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Uterotonics for prevention of postpartum haemorrhage: EN-BIRTH multi-country validation study. BMC Pregnancy and Childbirth. 2021;21(1):1-17.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Oxytocin infusion after oxytocin bolus and carbetocin bolus to reduce blood loss during and after cesarean section—a randomized clinical trial. Med J Cairo Univ. 2015;83(1):79-83.
- [Google Scholar]
- Postpartum blood loss: Visual estimation versus objective quantification with a novel birthing drape. Singapore Med J. 2016;57(6):325.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Estimating blood loss: Can teaching significantly improve visual estimation? Obstet Gynecol. 2004;104(3):601-6.
- [CrossRef] [PubMed] [Google Scholar]





