Translate this page into:
Opioid Epidemic in the United States: Empirical Trends, and A Literature Review of Social Determinants and Epidemiological, Pain Management, and Treatment Patterns
*Corresponding author email: gsingh@hrsa.gov
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Objectives:
Dramatic increases in opioid and drug overdose mortality have occurred in the United States (US) over the past two decades. To address this national public health crisis and identify gaps in the literature, we analyzed recent empirical trends in US drug overdose mortality by key social determinants and conducted a selective review of the recent literature on the magnitude of the opioid crisis facing different racial/ethnic, socioeconomic, and rural-urban segments of the US population.
Methods:
We used the 1999-2017 mortality data from the US National Vital Statistics System to analyze trends in drug overdose mortality by race/ethnicity, age, and geographic area. Log-linear regression was used to model mortality trends. Using various key words and their combinations, we searched PubMed and Google Scholar for select peer-reviewed journal articles and government reports published on the opioid epidemic between 2010 and 2018.
Results:
Our original analysis and review indicate marked increases in drug overdose mortality overall and by race/ethnicity and geographic regions, with adolescents and young adults experiencing steep increases in mortality between 1999 and 2017. Our selective search yielded 405 articles, of which 39 publications were selected for detailed review. Suicide mortality from drug overdose among teens aged 12-19 increased consistently between 2009 and 2017, particularly among teen girls. The rise of efficient global supply chains has increased opioid prescription use and undoubtedly contributed to the opioid epidemic. Many other important contributing factors to the epidemic include lack of education and economic opportunities, poor working conditions, and low social capital in disadvantaged communities.
Conclusions and Global Health Implications:
Our analysis and review indicate substantial disparities in drug overdoses and related mortality, pain management, and treatment outcomes according to social determinants. Increases in drug overdoses and resultant mortality are not only unique to the US, but have also been observed in other industrialized countries. Healthcare systems, community leaders, and policymakers addressing the opioid epidemic should focus on upstream structural factors including education, economic opportunity, social cohesion, racial/ethnic disadvantage, geographic isolation, and life satisfaction.
Keywords
Opioids
Drug overdose
Mortality
Pain management
Treatment
Race/Ethnicity
Social determinants
Health disparities
1. Introduction
Drug overdose mortality, driven primarily by illicit (heroin) and prescription opioids (natural and synthetic opioids such as morphine, codeine, hydrocodone, oxycodone, fentanyl, and tramadol) have contributed significantly to the recent rise in mortality among middle-aged white Americans and to the declining life expectancy among US men and women in the past three years.1-4 During the last 18 years, the rate of drug-overdose deaths has more than tripled in the United States, the rates of drug-overdose mortality involving natural and semisynthetic opioids increased more than 4 fold, those involving synthetic opioids other than methadone increased 30 fold, and those involving heroin increased 7 fold.1-4 The number of drug overdose deaths in the US increased 4 fold, from 16,849 in 1999 to 70,237 in 2017.1,2,4 In 2016 and 2017, opioid-related deaths accounted for two-thirds of all drug overdose deaths.4,5
The impact of the opioid epidemic cuts across age, gender, racial/ethnic, socioeconomic, and geographic/rural-urban groups. Due to dramatic increases in opioid and drug overdose mortality among various population groups and geographic areas over the past two decades, the current opioid epidemic in the US has been declared a national public health crisis.4,6,7 Despite these adverse trends in opioid and drug overdose mortality, no studies, to our knowledge, have looked at epidemiology and risk factors, pain management, and treatment disparities underlying the opioid epidemic in the same context. In order to better understand the opioid crisis, all three areas need to be addressed. Epidemiologic and surveillance studies identify population groups and geographic areas at the highest risks of drug and opioid overdose morbidity and mortality and indicate changes in the magnitude of the opioid problem over time. Since prescription opioids are used to treat pain, they can be highly addictive and cause substance dependence.8 Inequalities in pain management are therefore a critical area of study when addressing the opioid epidemic. Moreover, there are effective treatments for opioid dependence such as naloxone that can reverse the effects of opioid overdose and prevent overdose deaths, but there are substantial treatment gaps that require attention from researchers and policymakers.9
To address these gaps in the literature, our aim was to analyze the latest empirical trends in US drug overdose mortality by key social determinants. This is followed by a selective but comprehensive review of the recent literature that looks at the magnitude of the opioid crisis facing different racial/ethnic, socioeconomic, and rural-urban segments of the US population, summarizing evidence on epidemiology, social determinants, prevention, treatment, and pain management.
2. Methods
We used the 1999-2017 National Mortality Database from the US National Vital Statistics System to analyze temporal trends in drug overdose mortality.1-4 The national mortality database, maintained by the National Center for Health Statistics, has been the primary source of mortality analyses and surveillance by age, sex, race/ethnicity, cause of deaths, and place of residence for over a century.10,11 Drug overdose mortality rates for each racial/ethnic and gender group, rural/urban area, and geographic region were age-adjusted by the direct method using the 2000 US standard population. Drug overdose or poisoning deaths from 1999 to 2017 were coded according to the International Classification of Diseases, 10th Revision (ICD-10) with underlying cause-of-death codes of X40-X44 (unintentional), X60-X64 (suicide), X85 (homicide), or Y10-Y14 (undetermined intent).4 Log-linear regression models were used to estimate annual rates of change (increase) in mortality trends from 1999 through 2017.11
To conduct a selective research literature review, we searched the PubMed database and Google Scholar to select peer-reviewed journal articles and government reports published on the opioid epidemic between 2010 and 2018. PubMed, maintained by the US National Library of Medicine, comprises more than 29 million citations for biomedical literature from MEDLINE, life science journals, and online books.12 Citations may include links to full-text content from PubMed Central and publisher websites.12 PubMed focuses on biomedical and clinical literature.12 However, many of the government reports and research articles published on the opioid epidemic in social and behavioral sciences are not indexed for Medline or PubMed, but are generally indexed in Google Scholar. Google Scholar allows the researcher the flexibility to search across various disciplines and sources like journal articles, government and non-governmental reports, books, abstracts, and opinions.13 Since our search key words were very specific, use of the two databases yielded the most relevant publications (articles and reports) for our selective research literature review.
The following key words were used to conduct the search in our selective research literature review:
The search using the above key words yielded 405 articles and reports, which were reviewed by two researchers, including the lead author. Abstracts, synopses, and titles were briefly examined to see if they contained comprehensive analyses or description of opioid related outcomes by key social determinants as identified above. Commentaries, opinion pieces, review articles, and government data and policy reports were included in the search process. Figure 1 depicts our search process and outcomes.

- Flow Diagram Showing Results of the Selection Process Related to the Opioid Literature Review
Articles and reports published outside the period 2010-2018 were excluded. Fifteen articles and reports were excluded because they did not adequately cover racial/ethnic, socioeconomic, and geographic disparities or did not explicitly examine opioid related outcomes, including epidemiology, pain management, and/or treatment. We selected 10% of these articles and reports that met all criteria in terms of their national scope or broad geographic focus, social determinants, opioid outcomes, and recency of publication. Those published from 2015 to 2018 were preferred and given greater weights for selection. This resulted in the selection of 39 articles for which we conducted detailed individual reviews (Figure 1).4,5,14-50 Each selected paper was reviewed by one or more of the study authors adopting a template that was used in the 2003 study on migration and health by McKay and colleagues.51 Each of the selected articles and reports was reviewed and categorized into three broad categories of epidemiology/surveillance, pain management, and treatment/health policy (see Appendix 1). This study used existing de-identified publicly available data and was deemed exempt.
3. Key Empirical Findings
3.1. Trends in drug overdose mortality by race/ethnicity and gender
Figure 2 shows increasing trends in drug overdose mortality among all major racial/ethnic groups, with mortality rates being the highest among non-Hispanic whites and the lowest among Asian/Pacific Islanders (APIs). The average rate of increase in drug overdose mortality during 1999-2017 was the fastest among non-Hispanic whites (7.6% per year), followed by American Indians and Alaska Natives [AIANs] (6.1%), APIs (5.9%), Blacks/African Americans (3.6%), and Hispanics (3.3%).

- Racial/Ethnic Trends in Drug Overdose Mortality, Both Sexes, United States, 1999-2017
- Source: Data derived the National Vital Statistics System, National Mortality Database.
During 1999-2017, drug overdose mortality rates increased significantly faster in women than in men (annual rate of increase 6.7% vs. 6.1%) [Figures 3 and 4]. During 1999-2017, the average annual rates of increase in drug overdose mortality for different racial/ethnic and gender groups were as follows: non-Hispanic white males (7.4%), non-Hispanic white females (7.9%), black males (3.3%), black females (4.2%), AIAN males (6.0%), AIAN females (6.1%), API males (6.8%), API females (4.0%), Hispanic males (2.8%), and Hispanic females (4.8%) [Figures 3 and 4].

- Racial/Ethnic Trends in Drug Overdose Mortality, Males, United States, 1999-2017
- Source: Data derived the National Vital Statistics System, National Mortality Database.

- Racial/Ethnic Trends in Drug Overdose Mortality, Females, United States, 1999-2017
- Source: Data derived the National Vital Statistics System, National Mortality Database.
3.2. Trends in drug overdose mortality by age
Figure 5 shows a markedly upward trend in drug overdose mortality among children and adolescents, with young adults aged 20-24 years experiencing more than a 4 fold increase in mortality rates between 1999 and 2017. Rates of suicide mortality from drug overdose among teens aged 12-19 years increased consistently between 2009 and 2017, particularly among all teenaged girls and white girls whose suicides rates rose nearly three-fold during the period (Figure 6). During 2014-2017, suicide mortality from drug overdose was almost twice as high among teenage girls as teenage boys.
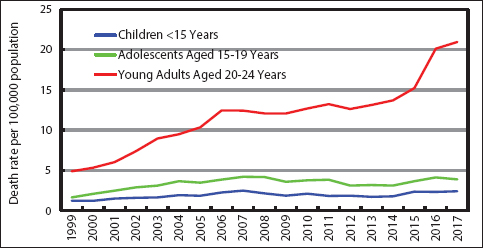
- Trends in Drug Overdose Mortality among Children, Adolescents, and Young Adults, United States, 1999-2017
- Death rates for children aged <15 years are per million, while death rates for adolescents and young adults are per 100,000 population.
- Source: Data derived the National Vital Statistics System, National Mortality Database.
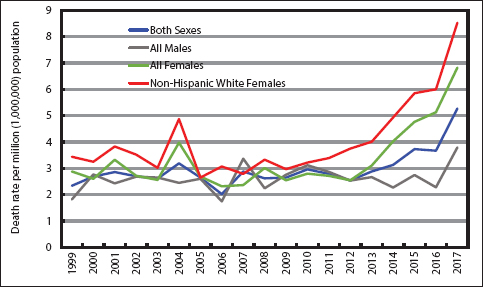
- Trends in Suicide Mortality from Drug Overdose among Teens Aged 12-19 Years, United States, 1999-2017
- Source: Data derived the National Vital Statistics System, National Mortality Database.
3.3. Trends in drug overdose mortality by geographic region
Figure 7 shows rapid increases in drug overdose mortality during 1999-2007 in both metropolitan/urban and non-metropolitan/rural areas of the US. Figure 8 shows steep increases in drug overdose mortality between 1999 and 2017 for all 9 geographic regions, with residents of the New England, Middle Atlantic, and East North Central regions (primarily the east coast region of the US) experiencing the greatest mortality increase (149% to 220% increase) during 2009-2017. Regional patterns have changed and geographic disparities in drug overdose mortality have widened over time. In 2017, the New England, Middle Atlantic, and East North Central regions had the highest drug-overdose mortality rates, while the Mountain and Pacific regions had the lowest mortality rates.
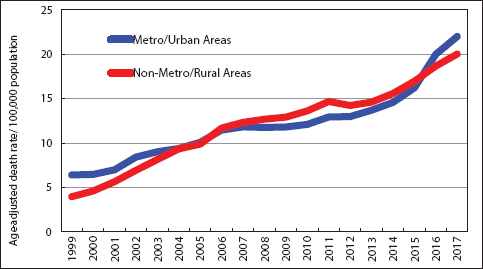
- Trends in Drug Overdose Mortality in Urban and Rural Areas, United States, 1999-2017
- Source: Data derived the National Vital Statistics System, National Mortality Database.
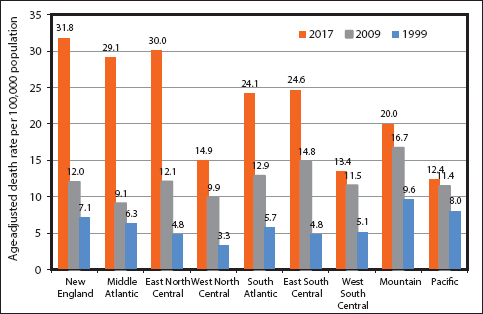
- Trends in Drug Overdose Mortality in 9 Census Regions, United States, 1999-2017
- Source: Data derived the National Vital Statistics System, National Mortality Database.
- Notes: States within each census region. New England = Maine + New Hampshire + Vermont + Massachusetts + Rhode Island + Connecticut; Middle Atlantic = New York + New Jersey + Pennsylvania; East North Central = Ohio + Indiana + Illinois + Michigan + Wisconsin; West North Central = Minnesota + Iowa + Missouri + North Dakota + South Dakota + Nebraska + Kansas.
-
South Atlantic = Delaware + Maryland + District of Columbia + Virginia + West Virginia + North Carolina + South Carolina + Georgia + Florida; East South Central = Kentucky + Tennessee + Alabama + Mississippi; West South Central = Arkansas + Louisiana + Oklahoma + Texas; Mountain = Montana + Idaho + Wyoming + Colorado + New Mexico + Arizona + Utah + Nevada; Pacific = Washington + Oregon + California + Alaska + Hawaii.
4. Key Findings for Reviews
Appendix 1 shows the summaries of all studies identified in our selective review. Of the 39 articles reviewed and included within this paper, 29 were epidemiological, 15 focused on pain management, and 14 described treatment patterns and outcomes.4,5,14-50 It should be noted that there was overlap in topic areas, as several articles covered all three components within their respective reports.
4.1. Epidemiology and surveillance
The studies reviewed indicate increasing trends and marked disparities in overall drug overdose mortality and in opioid-related morbidity and mortality by age, gender, race/ethnicity, and place and state of residence.4,5,17,21 During 1999-2017, drug overdose mortality in the US increased more than 3-fold.4 Adults aged 25-34, 35-44, and 45-54 years had the drug overdose mortality rates, although those aged 55-64 experienced the largest relative increase during this period.4 The rates of drug overdose mortality involving natural and semisynthetic opioids (such as morphine, codeine, hydrocodone, and oxycodone) increased more than 4-fold, and those involving such drug as fentanyl, fentanyl analogs, and tramadol increased 30-fold, and those involving heroin increased 7-fold.4 In 2016, opioid-related deaths in the US resulted in approximately 1.7 million years of life lost (YLL), with those aged 25-34 and 35-44 experiencing the highest burden in terms of YLL per 1000 population.5 In 2016 and 2017, states such as West Virginia, Ohio, New Hampshire, Pennsylvania, and the District of Columbia had the highest mortality rates for overall drug overdose and several drug categories.4,17
Micro-level social and demographic factors such as race/ethnicity, gender, age, family composition, socioeconomic status, peer influence, family stress, social isolation, and hopelessness have been identified as important correlates of substance use and misuse and mortality.20,22,25,30 Several macro-level structural factors such as increased availability of and access to prescription opioids, low social capital, area poverty rate, unemployment rate, lack of economic opportunities, poor working conditions, racial/ethnic composition, and out-migration have been identified as determinants of drug overdose mortality, opioid-related morbidity, and prevalence of prescription opioids.23-25,30
4.2. Pain management
During the past 20 years, there has been a rise in the therapeutic use, abuse, and nonmedical use of opioids, with hydrocodone becoming the leading prescribed medication in the US.36 Researchers have determined that there is a concrete connection between prescribed average daily dose of opioids and opioid-related mortality in adults presenting with nonmalignant pain.40 The research included in this review underscores the significant gaps that remain in mitigating incidences of opioid addiction.22 Despite novel practices for pain management, overprescribing patterns remain undefined by clinicians, which has the potential to serve as one of the myriad contributing factors leading to increases in overdose mortality.46
Studies have also indicated that women are more likely to experience chronic pain and use prescription opioid pain medications for longer periods and in higher doses than men. Furthermore, women who use opioids become dependent more quickly and experience more cravings than men.22 Thus, health care workers should remain cognizant of environmental differences, variances in motivations for treatment utilization, and barriers to seeking treatment for substance use disorders.22 Additionally, researchers suggest primary, secondary, and tertiary prevention strategies for decreasing the incidence of addiction. In an effort to mitigate disparities, federal, state, and local decision makers should target low-income areas.14,23
4.3. Treatment/Health policy
Substance misuse and use disorders cause severe damage at both the individual and community-level. Moreover, treatment differences contribute significantly to disparities in overdose mortality. Compared to white patients, black and Hispanic patients are significantly less likely to receive antidotes for acute overdose when presenting to the emergency department.52 Thus, researchers highlight the importance of more extensive and comprehensive research being performed regarding the connection between social determinants and opioid use and the most appropriate method for training providers on treatment options.22 Additionally, it is critical that health care providers are adequately trained in “structural competency” while policymakers remain vigilant in addressing the economic, racial, and social issues related to opioid misuse.25
Research shows that most opioid-related deaths are preventable.40 Noting that there are biological and psychological factors involved in opioid substance misuse, researchers stress the importance of prevention, treatment, and recovery support services and the integration of services for substance use disorders into the rest of healthcare.15 Research shows that a primary strategy with potential positive outcomes could be for health care providers to remain cognizant of current and accurate information regarding opioid use and strategies for prescription drug monitoring, while reorienting themselves with harm reduction approaches for overdose reversal.14 Regarding medication, research suggests that increased use of Naxolene by health care providers and Emergency Medical Technicians could contribute to a reduction in overdose deaths.50 Furthermore, researchers highlight the importance of physicians being trained on making the distinction between patient “suffering” and “pain,” with the intention of shedding light on the various other factors of the opioid crisis and not simply relegating it to over prescribing.25
5. Limitations
Our analysis of drug overdose mortality trends involves both opioids and non-opioid drugs such as cocaine, methamphetamine, and other psychostimulants.4,53-55 Because of the unavailability of data on types of drugs involved as indicated by ICD-10 multiple-cause-of-death codes: heroin (T40.1); natural and semisynthetic opioids (T40.2); methadone (T40.3); and synthetic opioids other than methadone (T40.4), we were unable to calculate opioid-related mortality trends by race/ethnicity, gender, age, rural/urban, and region of residence.4 Since our study used national vital statistics data, underreporting of mortality statistics for AIANs, APIs, and Hispanics on the death certificate may have led to an underestimation of drug overdose mortality rates for these racial/ethnic groups.10,11 Moreover, our analysis does not include analyses of drug overdose mortality trends and patterns by other important sociodemographic factors such as educational attainment, family income, occupation, marital status, nativity/immigrant status, and community-level socioeconomic conditions.
Since we performed a selective rather than a systematic literature review, it is conceivable that our review failed to include important studies on the opioid epidemic that focused on social determinants of drug overdose and opioid-related outcomes. However, the use of both PubMed and Google scholar in our selection process and review and emphasis on scientific and empirical evidence may very well indicate the comprehensiveness of the review conducted.
6. Summary, Conclusions and Global Health Implications
Our paper makes an important and unique contribution to the burgeoning empirical literature on the opioid epidemic by analyzing the latest drug overdose mortality trends for the US and by presenting a selective but comprehensive review of the literature on drug overdose and opioid-related outcomes. Presented below is a brief summary of the reviews conducted, highlighting trends in US drug overdose morbidity and mortality by major socioeconomic and demographic groups as well as patterns of disparities in opioid-related pain management and treatment outcomes.4,5,14-50
During 1999-2017, the rate of drug overdose deaths in the US more than tripled, with adults aged 55-64 years experiencing the largest percentage increase of 6 fold.4 Substantial geographic, racial/ethnic, gender, and socioeconomic disparities in drug overdose mortality exist.2,4 As our analysis shows, geographic disparities in drug overdose mortality have changed and widened over time, while both urban and rural areas have seen marked increases in mortality during the past two decades. Rural areas such as those in the Appalachia, parts of the West and Midwest, and New England are experiencing an increasing number of overdose deaths and opioid prescriptions.3,23 Additionally, a study demonstrated that while whites had significantly higher representation among opioid poisoning patients in the state of New York, Asians had significantly less representation.18 Studies have also shown significant correlations between amounts of prescribed opioids in 2008 and greater population size, lower education level, higher percentage of non-Hispanic whites and African-Americans, higher poverty, higher percentage of population without insurance and younger than 65 years, higher physicians per capita, and higher percentages of all surgeons, psychiatrists, and pediatricians.41 While men have experienced two times higher drug overdose mortality rates than women during the past two decades, the relative increases in overall drug overdose mortality and in suicide and unintentional injury mortality from drug overdose have been more rapid for women than men.2,4 Studies have also indicated that women are more likely to experience chronic pain and use prescription opioid pain medications for longer periods and in higher doses than men. Furthermore, women who use opioids become dependent more quickly and experience more cravings than men.22
While the rise of efficient global supply chains has increased opioid prescription use and undoubtedly contributed to the opioid epidemic, there are many other significant contributing factors to the epidemic including a lack of economic opportunity, poor working conditions, and meager social capital in depressed communities.25 These factors have collectively led to substantial socioeconomic and racial/ethnic disparities in drug overdose rates. For example, recent studies have demonstrated a strong and statistically significant inverse association between county-level social capital and age-adjusted mortality due to drug overdose, suggesting that social capital protects communities against drug overdose.24 Similarly, Baggett et al. found that compared to Massachusetts adults, homeless people had tobacco-attributable mortality rates that were 3-5 times higher, alcohol-attributable mortality rates that were 6-10 times higher, and drug-attributable mortality rates that were 8-17 times higher. Disparities in substance use-attributable deaths accounted for 57% of this mortality disparity between the homeless and Massachusetts adults.56 In the 1990s, rates of overdose deaths in New York City were consistently higher among blacks/African-Americans and Hispanics/Latinos compared to whites,57 while our analysis showed higher mortality rates among whites than blacks and Hispanics nationally during 2002-2017.2 Disparities in overdose mortality may be related to differences in treatment, as Wilder et al. found that compared to white patients, black and Hispanic patients are significantly less likely to receive antidotes for acute overdose when presenting to the emergency department.52 Thus, instead of simply reducing opioid prescribing, policymakers addressing the opioid epidemic should focus on upstream structural factors, including economic opportunity, social cohesion, racial disadvantage, and life satisfaction.24
Opioid misuse in rural areas may be related to several interrelated factors including economic deprivation and unemployment, out migration, and close kinship and social networks that facilitate faster diffusion of nonmedical prescription opioids.30 Racial differences in heroin and prescription opioid control resemble the crack/powder cocaine epidemic, which led the US to have the highest incarceration rates in the world, with black and Hispanic men at 6- and 3-times higher likelihood of incarceration, respectively, than white men.46 Additionally, in samples collected from emergency department visits from 1993-2005 for pain-related diagnoses, non-Hispanic whites accounted for the majority of these visits and also accounted for the highest percentage of prescriptions given for opioid analgesics.34 With regard to pain management and treatment, the US is the largest consumer of opioids worldwide.47 Although opioids are used to treat individuals with chronic pain, the literature challenges the benefits of use when opioid overdose deaths due to abuse, misuse, and overprescribing remain a major public health issue. Despite new protocols for pain treatment, overprescribing patterns have yet to be determined by clinicians, which can serve as one of the many contributing factors leading to increases in overdose mortality.47
While provider education regarding opioid prescribing remains a focus, there is an opportunity to reorient US drug policies to make proven harm reduction strategies widely available, such as naloxone for overdose reversal, treatment facilities, medication assisted treatments, psychosocial treatments, behavior therapy, and relapse prevention. Racial/ethnic disparities in the perception, assessment, and treatment of pain suggest improved training for providers, and educational intervention for patients, to address complex sources of pain treatment inequities that include bi-directional patient provider communication.49 According to Hansen et al., the US should focus efforts on decriminalizing personal possession of drugs and expunging arrest records, which typically are young men of color. Additionally, the authors recommend that narcotics policies be scrutinized for racial targeting and reinforcing inequalities in health and law enforcement.46 The Surgeon General’s Report on Alcohol, Drugs, and Health highlights that addiction is not a moral failure or character flaw but rather a health condition.15 The report states that resolving the opioid crisis will require the coordination of the healthcare system, community leaders, researchers, and other public, private, and voluntary entities that are part of the public health system.15
In conclusion, our analysis and the studies reviewed here report substantial disparities in drug overdoses and related mortality, pain management, and treatment outcomes, according to social determinants. Increases in drug overdoses and resultant mortality are not only unique to the US, but have also been observed in other industrialized countries.39,58 As several of the studies indicate, healthcare systems, community leaders, and policymakers addressing the opioid epidemic should focus on upstream structural factors including education, economic opportunity, social cohesion, racial/ethnic disadvantage, geographic isolation, and life satisfaction.3,15,23
Appendix
Funding/Support: None.
Conflicts of Interest: The authors declare that there are no conflicts of interest.
Disclaimer: The views expressed are those of the authors’ and not necessarily those of the U.S. Department of Health and Human Services or the Health Resources and Services Administration.
Ethical approval: This study used existing de-identified publicly available data and was deemed exempt.
References
- 2018. National Vital Statistics System, Mortality Multiple Cause-of-Death Public Use Data File Documentation. Hyattsville, MD: US Department of Health and Human Services; http://www.cdc.gov/nchs/nvss/mortality_public_use_data.htm
- Social Determinants of Health in the United States:Addressing Major Health Inequality Trends for the Nation, 1935-2016. Int J MCH AIDS. 2017;6(2):139-164.
- [Google Scholar]
- Drug Overdose Deaths in the United States, 1999 –2017. 2018. NCHS Data Brief. :1-8. https://www.cdc.gov/nchs/data/databriefs/db329-h.pdf
- [Google Scholar]
- The Burden of Opioid-Related Mortality in the United States. JAMA Network Open. 2018;1(2):180217. doi:10.1001/jamanetworkopen.2018.0217
- [Google Scholar]
- Ending America's Opioid Crisis. https://www.whitehouse.gov/opioids//
- Increases in Drug and Opioid Overdose Deaths –United States, 2000-2014. Am J Transplant. 2016;16(4):1323-1327.
- [Google Scholar]
- 2018. Management of Substance Abuse:Information Sheet on Opioid Overdose. Geneva, Switzerland: WHO; https://www.who.int/substance_abuse/information-sheet/en/
- Socioeconomic and racial/ethnic disparities in cancer mortality, incidence, and survival in the United States, 1950-2014: over six decades of changing patterns and widening Inequalities. J Environ Public Health doi: 2017/2819372, Epub March 2017
- [Google Scholar]
- National Institutes of Health. PubMed. https://www.ncbi.nlm.nih.gov/pubmed/
- The Prescription Opioid and Heroin Crisis:A Public Health Approach to an Epidemic of Addiction. Annu Rev Public Health. 2015;36:559-574.
- [Google Scholar]
- Office of the Surgeon General. Washington, DC: US Department of Health and Human Services; 2016.
- The President's Commission on Combating Drug Addiction and the Opioid Crisis:Origins and Recommendations. Clin Pharmacol Ther. 2018;103(6):943-945.
- [Google Scholar]
- Overdose Deaths Involving Opioids, Cocaine, and Psychostimulants –United States, 2015-2016. MMWR. 2018;67(12):349-358.
- [Google Scholar]
- Large-scale Analysis of Opioid Poisoning Related Hospital Visits in New York State. AMIA Annu Symp Proc 2017:545-554.
- [Google Scholar]
- Disability Status and Prescription Drug Misuse Among U.S. Adults. Addict Behav. 2018;85:64-69.
- [Google Scholar]
- Correlates of Prescription Opioid Misuse Among Black Adults:Findings from the 2015 National Survey on Drug Use and Health. Drug Alcohol Depend. 2018;186:264-267.
- [Google Scholar]
- Drug Overdose Deaths Among Adolescents Aged 15-19 in the United States: 1999-2015. NCHS Data Brief. 2017;282:1-8.
- [Google Scholar]
- White Paper:Opioid Use, Misuse, and Overdose in Women. Washington, DC: US Department of Health and Human Services;December 2016;
- The Opioid Crisis and Economic Opportunity:Geographic and Economic Trends. Office of the Assistant Secretary for Planning and Evaluation. ASPE Research Brief 2018
- [Google Scholar]
- Bowling Alone, Dying Together:The Role of Social Capital in Mitigating the Drug Overdose Epidemic in the United States. Drug Alcohol Depend. 2017;173:1-9.
- [Google Scholar]
- Opioid Crisis:No Easy Fix to Its Social and Economic Determinants. Am J Public Health. 2018;108(2):182-186.
- [Google Scholar]
- Association Between Opioid Prescribing Patterns and Opioid Overdose-Related Deaths. JAMA. 2011;305(13):1315-1321.
- [Google Scholar]
- Determinants of Increased Opioid-Related Mortality in the US and Canada, 1990-2013: A Systematic Review. Am J Public Health. 2014;104(8):32-37.
- [Google Scholar]
- Prescription Opioid Poisoning Across Urban and Rural Areas:Identifying Vulnerable Groups and Geographic Areas. Addiction. 2016;112:103-112.
- [Google Scholar]
- Understanding the Rural-Urban differences in Nonmedical Prescription Opioid Useand Abuse in the US. Am J Public Healthd. 2014;104(2):52-59.
- [Google Scholar]
- Trends in Opioid Analgesic Abuseand Mortality in the U.S. Engl J Med. 2015;372(3):241-248.
- [Google Scholar]
- Prescription Opioid Misuse, Abuse, and Treatment in the United States:An Update. Am J Psychiatry. 2016;173(1):18-26.
- [Google Scholar]
- Curtailing Diversion and Abuse of Opioid Analgesics without Jeopardizing Pain Treatment. JAMA. 2011;305(13):1346-1347.
- [Google Scholar]
- Trends in Opioid Prescribing by Race/Ethnicity for Patients Seeking Care in US Emergency Departments. JAMA. 2008;299(1):70-78.
- [Google Scholar]
- Ethnic Disparities in Opioid Prescriptions at Emergency Department Visits for Conditions Commonly Associated with Prescription Drug Abuse. PLoS One. 2016;11(8):0159224. doi:10.1371/journal.pone.0159224
- [Google Scholar]
- Revisiting the ‘Paradigm Shift’ in Opioid Use:Developments and Implications 10 years Later. Drug Alcohol Rev. 2018;37(Suppl 1):199-202.
- [Google Scholar]
- Non-Medical Use of Prescription Opioids and Prescription Opioid-Related Harms:Why So Markedly Higher in North America Compared to the Rest of the World? Addiction. 2014;109(2):177-81.
- [Google Scholar]
- Worldwide Prevalence and Trends in Unintentional Drug Overdose:A systematic review of the literature. Am J Public Health. 2015;105(11):29-49.
- [Google Scholar]
- Opioid Dose and Drug-Related Mortality in Patients with Nonmalignant Pain. Arch Intern Med. 2011;171(7):686-691.
- [Google Scholar]
- Introduction to the Opioid Epidemic:The Economic Burden on the Healthcare System and Impact on Quality of Life. Am J Manag Care. 2018;24:200-206.
- [Google Scholar]
- Understanding the Provider Contribution to Race/Ethnicity Disparities in Pain Treatment:Insights from Dual Process Models of Stereotyping. Pain Med. 2006;7(2):119-134.
- [Google Scholar]
- Addressing the Opioid Epidemic in the United States:Lessons from the Department of Veterans Affairs. JAMA Intern Med. 2017;177(5):611-612.
- [Google Scholar]
- Centers for Disease Control Guideline for Prescribing Opioids for Chronic Pain - United States 2016. JAMA. 2016;315(15):1624-1645.
- [Google Scholar]
- Evaluation of American Indian Health Service Training in Pain Management and Opioid Substance Use Disorder. Am J Public Health. 2016;106(8):1427-1429.
- [Google Scholar]
- Is the Prescription Opioid Epidemic a White Problem? Am J Public Health. 2016;106(12):2127-2129.
- [Google Scholar]
- Racial Differences in Primary Care Opioid Risk Reduction Strategies. Ann Fam Med. 2011;9(3):219-225.
- [Google Scholar]
- The Unequal Burden of Pain:Confronting Racial and Ethnic Disparities in Pain. Pain Med. 2003;4(3):277-294.
- [Google Scholar]
- Disparity in Naloxone Administration by Emergency Medical Service Providers and the Burden of Drug Overdose in US Rural Communities. Am J Public Health. 2015;105(Suppl 3):26-32.
- [Google Scholar]
- Migration and Health:A Review of the International Literature. 2003. Medical Research Council, Glasgow, Scotland. http://www.sphsu.mrc.ac.uk/library/occasional/OP012.pdf.
- [Google Scholar]
- Racial Disparities in the Treatment of Acute Overdose in the Emergency Department. Clin Toxicol (Phila). 2018;56(12):1173-1178.
- [Google Scholar]
- Contribution of Opioid-Involved Poisoning to the Change in Life Expectancy in the United States. JAMA. 2017;318(11):1065-1067.
- [Google Scholar]
- Trends in Black and White Opioid Mortality in the United States. Epidemiology. 2018;29(5):707-715.
- [Google Scholar]
- Prenatal Risk Factors and Perinatal and Postnatal Outcomes Associated With Maternal Opioid Exposure in an Urban, Low-Income, Multiethnic US Population. JAMA Network Open. 2019;2(6):196405. doi:10.1001/jamanetworkopen.2019.6405
- [Google Scholar]
- Tobacco-, Alcohol-, and Drug-Attributable Deaths and their Contribution to Mortality Disparities in a Cohort of Homeless Adults in Boston. Am J Public Health. 2015;105(6):1189-1197.
- [Google Scholar]
- Racial/Ethnic Disparities in Overdose Mortality Trends in New York City, 1990-1998. J Urban Health. 2003;80(2):201-21.
- [Google Scholar]
- Drug Deaths: Record Number in Scotland Prompts Calls for Urgent UK Policy Reform. BMJ. 2019;366:14731. doi:10.1136/bmj.l4731
- [Google Scholar]





