Translate this page into:
Postpartum Hemorrhage in Humanitarian Settings: Heat-Stable Carbetocin and Tranexamic Acid Implementation Study in Uganda

*Corresponding author: Nguyen Toan Tran, The Australian Centre for Public and Population Health Research (ACPPHR) Faculty of Health, University of Technology, Sydney, NSW, Australia. Tel: +1 929 523 5158 nguyentoan.tran@uts.edu.au
-
Received: ,
Accepted: ,
How to cite this article: Tran NT, Mugerwa K, Muwanguzi S, Mwesigwa R, Wasswa D, Zeck W, et al. Postpartum hemorrhage in humanitarian settings: Heat-stable carbetocin and tranexamic acid implementation study in Uganda. Int J MCH AIDS. 2024;13:S46-54. doi: 10.25259/IJMA_9_2023
Abstract
Background and Objective
Postpartum hemorrhage (PPH) remains a major concern in crisis-affected settings. There is a lack of strategies for implementing heat-stable carbetocin (HSC) and tranexamic acid (TXA) in humanitarian settings. This study aims to investigate the impact of a capacity-strengthening package on the utilization of uterotonics for PPH prevention, PPH detection, and utilization of TXA for PPH treatment in basic obstetric care clinics in humanitarian settings in Uganda.
Methods
A multi-stepped implementation research study was conducted, wherein six select facilities utilized an intervention package encompassing provider training, an online community of practice, and wall-displayed PPH algorithms. Facilities were conveniently assigned to the same study sequence: T1 (routine care), a transition period for training; T2 (package without HSC and TXA); T3 (package with HSC); and T4 (package with HSC and TXA). The primary outcomes assessed trends in prophylactic uterotonic use (including HSC), visual diagnosis of hemorrhage, and HSC and TXA use for hemorrhage treatment. Analysis followed an intention-to-treat approach, adjusting for cluster effect and baseline characteristics. Pan-African Clinical Trials Registry: PACTR202302476608339.
Results
From April 10, 2022, to April 4, 2023, 2299 women were recruited (T1: 643, T2: 570, T3: 580, T4: 506). Over 99% of all women received prophylactic uterotonics across the four phases, with oxytocin alone primarily used in T1 (93%) and T2 (92%) and HSC alone in T3 (74%) and T4 (54%) (T4–T1 95% CI: 47.8–61.0). Hemorrhage diagnosis ranged from 1% to 4%. For hemorrhage treatment, universal oxytocin use in T1 and T2 decreased in T3 and T4 after HSC introduction (T4–T1: 33%–100%; 95% CI: –100.0 to –30.9), and TXA use increased in T4 (T4–T1: 33%–0%; 95% CI: –2.4 to 69.1).
Conclusion and Global Health Implications
An intervention package to reinforce providers’ capacity to prevent and treat PPH can result in substantial HSC utilization and a moderate TXA adoption in cold-chain-challenged humanitarian settings. It could be scaled up with continuous capacity development and supportive supervision to mitigate confusion between existing and new medications, such as the decreased use of oxytocin for PPH treatment. Maintaining investments in cold-chain strengthening remains critical to ensure the quality of oxytocin.
Keywords
Health Services Research
Postpartum Hemorrhage
Heat-Stable Carbetocin
Tranexamic Acid
Public Health Intervention Package
Humanitarian Settings
Fragile Settings
INTRODUCTION
Background of the Study
Postpartum hemorrhage (PPH) is defined as excessive blood loss (≥ 500 mL after vaginal birth or ≥ 1000 mL after cesarean birth within 24 hours). This condition contributes to over 25% of maternal deaths worldwide, primarily in low and middle-income countries (LMIC) affected by fragility and humanitarian disasters.[1,2] Active management of the third stage of labor (AMTSL) can prevent most PPH deaths.[3] It includes prophylactic uterotonic use, delayed cord clamping, and controlled cord traction (if skilled birth attendants are available).[4] Oxytocin (10 IU, IM/IV) is the standard uterotonic recommended in settings with multiple options but requires cold-chain storage.[1,5] Heat-stable carbetocin (HSC), a long-acting oxytocin analog, is recommended for PPH prevention but does not require cold-chain storage. Studies, including a 2018 trial by the World Health Organization (WHO), have shown HSC effectiveness and noninferiority to oxytocin in preventing PPH in low-income countries.[6-8] Furthermore, it was found cost-effective in reducing the number of PPH events and deaths, as well as public healthcare system costs in India.[6-8]
The WHO recommends prompt action in a multidisciplinary approach for treating PPH, including fluid replacement and additional uterotonic administration (following the initial dose for PPH prevention) as the primary interventions.[1,5,9] Tranexamic acid (TXA), an antifibrinolytic agent, reduces bleeding risk in surgery and trauma.[10,11] In obstetric care, TXA effectively controls bleeding in women with PPH regardless of the underlying cause.[12] It does not require cold chain systems, is affordable ($1.30 per 1g ampoule), and is readily available in hospitals.[7]
In 2022, two scoping literature reviews examined the existing implementation experience of HSC and TXA in low-resource countries, emphasizing their suitability in environments with limited cold-chain storage facilities.[13,14] The reviews found that most research originated from hospital-based studies and lower-middle-income countries with limited findings from low-resource or humanitarian settings, including rural or basic emergency obstetric facilities. On August 21, 2023, we searched PubMed using the term “randomized controlled trial” combined with “postpartum,” “hemorrhage,” “vaginal,” and “carbetocin” or “tranexamic” for publications in English, focusing on trials in LMIC (as defined by the World Bank) over the past ten years.[15] We identified one trial since the 2022 scoping literature reviews, the E-MOTIVE trial (Early Detection of Postpartum Hemorrhage and Treatment), which took place in hospitals—and not in lower maternity care facilities— in Kenya, Nigeria, South Africa, and Tanzania. It found that detecting PPH early using a calibrated blood-collection drape and implementing bundled treatments (uterine massage, oxytocic drugs, tranexamic acid, intravenous fluids, examination, and intervention escalation) resulted in a reduced risk of severe PPH, laparotomy for bleeding, or bleeding-related death, compared to standard care in women undergoing vaginal delivery.
Consequently, a gap exists within the extant body of evidence that describes strategies for implementing and building capacity to introduce HSC and TXA in humanitarian and fragile settings, and specifically in non-hospital contexts.
Objectives of the Study
Against this background, the overall objective of our implementation research consisted of examining the impact of an HSC and TXA-inclusive PPH capacity-strengthening package on the utilization of uterotonics (including HSC) for PPH prevention, PPH detection, and utilization of uterotonics and TXA for PPH treatment in low-resource cold-chain-challenged Basic Emergency Obstetric and Newborn Care (BEmONC) facilities. These facilities are commonly found in humanitarian settings. The intervention package is detailed under Methods.
Country Context
Uganda has witnessed a notable decline in its maternal mortality ratio over the past two decades. According to recent data, this ratio has decreased from 461 deaths per 100,000 live births in 2010 to 336 and 284 deaths per 100,000 live births in 2016 and 2020, respectively.[2] In a study conducted by Ononge et al. in 2016, the overall incidence of PPH was found to be 9%.[16] Another study revealed that merely 34% of women received all three AMTSL components, namely prophylactic uterotonics, delayed cord clamping, and controlled cord traction.[17]
As of June 2023, Uganda, a country with a population of approximately 46 million inhabitants, provided shelter to 1.5 million refugees and 48,953 asylum seekers, with women and girls constituting 51% of this population.[18] Approximately 60% of these individuals originate from South Sudan and have settled in the West Nile region, while 30% come from the Democratic Republic of Congo and have found refuge in Western Uganda.
METHODS
Study Design and Participants
Our study utilized implementation research to thoroughly examine the effectiveness and mechanisms of the intervention in real-world scenarios, aiming to identify avenues for improvement.[19] Our research study adopted a pragmatic, multi-intervention, multi-stepped, cluster-based design, which was non-blinded, non-randomized, but controlled. Clustering was appropriate since the PPH capacity-strengthening strategy focused on healthcare facilities rather than individual women. The study encompassed six facilities—Bidibidi Health Center (HC) III, Barakala HCIII, Uriama HCIII, Yinga HCIII, Ucea HCIII, and Nakivale HCIII—located in West Nile and the Western Region of Uganda. Facilities were included if classified as BEmONC-only and had recent cold storage disruptions, expressing willingness to participate. Facilities offering Comprehensive Emergency Obstetric and Newborn Care (CEmONC) were excluded. All birthing women were eligible without specific exclusions and were invited to participate in the study.
Stepwise Approach
A standardized sequence [Figure 1] was followed across the six sites. Step 1 (T1) encompassed 6 weeks of routine care. This was followed by a one-month period to prepare for step 2 (T2), which involved a 6-week period without HSC and TXA. Step 3 (T3) featured a 6-week interval with HSC but no TXA. Step 4 (T4) comprised 6 weeks with both HSC and TXA.
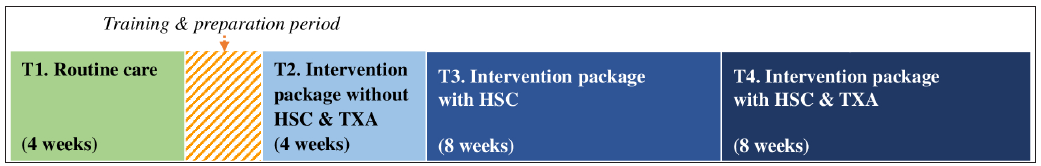
- The four steps of the study. HSC: Heat-stable carbetocin, TXA: Tranexamic acid.
Intervention
The PPH package incorporated three interventions for provider enhancement. First, refresher training focused on PPH skills through a low-dose, high-frequency method: 2-week self-study/webinars followed by a 2-day workshop. Monthly facility-based skills drills and reviews were used to bolster learning. Second, a WhatsApp-based community of practice promoted provider communication and collaboration. Third, PPH algorithm posters in delivery rooms aided adherence to protocols. Routine care included oxytocin, misoprostol, HSC, but not TXA, following national guidelines, although HSC was not yet available nationally at the time of the study.
Outcomes
The evaluation of primary outcomes encompassed four indicators. The first indicator was the proportion of women who received a uterotonic for PPH prevention by type of uterotonic utilized. Second was the proportion of women visually diagnosed with PPH. Third was the proportion of women diagnosed with PPH who received oxytocin for PPH treatment. Finally, was the proportion of women diagnosed with clinical PPH who received TXA for PPH treatment. Due to time and resource constraints in this implementation research study, the collection and management of quantitative data were streamlined. For example, instead of utilizing specifically designed case-report forms at the individual participant level, maternity registers were employed. The national research coordinator thoroughly examined all submitted documents, identified discrepancies, and worked with facility providers to resolve them before sending the documents to the data manager. Furthermore, quantitative outcome variables were not collected to evaluate the level of implementation of the intervention package, as recommended by Peters et al.[19] Instead, qualitative research methodologies were employed to assess the perspectives of healthcare providers in this regard, constituting the study’s secondary outcomes, which are reported elsewhere.
Statistical Analysis
For robustness, we estimated the sample size in our quasi-experimental research based on uterotonic usage assumptions for PPH prophylaxis. Starting from an initial 30% uterotonic usage (T1),[17] we conservatively anticipated 60% in T2, persisting in T3 and T4. Hence, ≥504 participants (6 facilities * 4 phases * 21) were required. Statistical power calculations employed R’s pwr package, yielding 80% power to detect a 30% difference (60%–30%) at a 5% two-sided significance level with a design effect of 1.5.[20] The use of the design effect was necessary due to the cluster-based sampling approach employed in the study.
Data were analyzed using IBM SPSS Statistics (v25.0) (IBM Corp. Released 2017. IBM SPSS Statistics for Windows, Version 25.0. Armonk, NY: IBM Corp.) and WINPEPI (v11.50). Participants served as assignment and analysis units. Considering patient sequential attendance, proportions satisfying key outcomes per phase were calculated, applying a clustering-based design effect of 1.5. Two-wise proportion comparisons were computed with WINPEPI. Result comparability was ensured by standardizing T2–T4 prevalences with T1 as the reference, accounting for variables like age, gestational age, and parity. Missing data were not imputed. Findings adhere to TREND and CONSORT reporting guidelines.[21,22]
Ethical Approval
Ethical approval was granted by the Uganda National Council for Science and Technology (reference HS2456ES).
RESULTS
Sociodemographic Characteristics
During the period spanning from April 10, 2022 to April 4, 2023, a total of 2299 women from six healthcare facilities were included in the study. The participants were distributed as follows: 643 in T1, 570 in T2, 580 in T3, and 506 in T4. Noteworthy variations in baseline characteristics of the participants, including age, gravidity, parity, gestational age, delivery mode, and alive status upon discharge, were not observed across the different phases of the study, as indicated in Table 1.
| N | T1 (baseline) | T2 (post training) | T3 (+HSC only) | T4 (+HSC & TXA) |
|---|---|---|---|---|
| (N=643) | (N=570) | (N=580) | (N=506) | |
| Age - median (IQR) | 25 (21-29) | 25 (22-30) | 25 (21-30) | 25 (21-30) |
| Gravidity - median (IQR) | 3 (2-5) | 3 (2-5) | 3 (2-5) | 3 (2-5) |
| Parity- median (IQR) | 2 (1-4) | 2 (1-4) | 2 (1-4) | 2 (1-4) |
| Gestational Age- median (IQR) | 38 (38-39) | 38 (38-39) | 38 (37-39) | 38 (38-40) |
| Delivery mode - n/N (%) | ||||
| Spontaneous vaginal delivery | 642/643 (99.8) | 569/570 (99.8) | 580/580 (100.0) | 506/506 (100.0) |
| Assisted | 0/643 (0.0) | 1/570 (0.2) | 0/580 (0.0) | 0/506 (0.0) |
| Breech | 0/643 (0.0) | 0/570 (0.0) | 0/580 (0.0) | 0/506 (0.0) |
| Cesarean section | 0/643 (0.0) | 0/570 (0.0) | 0/580 (0.0) | 0/506 (0.0) |
| Unknown | 1/643 (0.2) | 0/570 (0.0) | 0/580 (0.0) | 0/506 (0.0) |
| Women alive at discharge - n/N (%) | ||||
| Yes | 642/643 (99.8) | 570/570 (100.0) | 579/580 (99.8) | 506/506 (100.0) |
HSC: Heat-stable carbetocin, IQR: Interquartile range, n: Number of observations, N: Total number of participants in time period, T1: Time period 1, T2: Time period 2, T3: Time period 3, T4: Time period 4, TXA: Tranexamic acid.
Main Outcome Results
The primary outcomes of the study are presented in Table 2. The administration of uterotonics to prevent PPH was observed in nearly all participants, with no significant differences noted across the different phases. Notably, a significant change was observed in the types of uterotonic agents administered before and after the introduction of HSC. In the two initial phases (T1 and T2), oxytocin was predominantly used in 580 (93%) of 622 in T1 and 521 (92%) of 558 in T2), whereas HSC alone was the primary choice in the subsequent phases (421 (74%) of 560 in T3 and 270 (54%) of 494). Additionally, combined administration of uterotonics was recorded, with oxytocin and misoprostol being commonly used during the initial two phases (6% in T1 and T2, 2% in T3, and 1% in T4, unadjusted). Furthermore, during the later phases, HSC was administered in combination with either oxytocin (2% in T3 and 8% in T4, unadjusted) or misoprostol (1% in T3 and 3% in T4, unadjusted). There was no reported use of HSC for treatment or of TXA for prevention.
| T1 (baseline) | T2 (post training) | T3 (+HSC only) | T4 (+TXA & HSC) | Treatment differences 95% CI† | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| T2-T1 | T3-T1 | T4-T1 | T3-T2 | T4-T2 | T4-T3 | |||||
| Uterotonics for PPH prevention* | ||||||||||
| None - n/N (%) | 5/622 (0.8) | 1/558 (0.2) | 3/560 (0.5) | 0/494 (0.0) | (-1.8, 0.5) | (-1.7, 1.1) | (-1.9, 0.2) | (-0.7, 1.4) | (-0.7, 0.3) | (-1.4, 0.4) |
| HSC alone - n/N (%) | 0/622 (0.0) | 0/558 (0.0) | 421/560 (74.4) | 270/494 (54.4) | NA | (69.0, 79.8) | (47.8, 61.0) | (69.0, 79.8) | (47.8, 61,0) | (-28.5, -11.5) |
| Oxytocin alone - n/N (%) | 580/622 (93.2) | 521/558 (92.2) | 99/560 (16.9) | 163/494 (32.2) | (-5.5, 3.4) | (-81.8, -70.8) | (-67.9, -54.2) | (-81.0, -69.5) | (-67.0, -53.0) | (7.6, 23.0) |
| Visually diagnosed with PPH* - n/N (%) | 24/622 (3.9) | 25/558 (4.4) | 8/560 (1.3) | 15/494 (2.7) | (-2.9, 4.0) | (-5.2, 0.1) | (-4.3, 1.9) | (-6.0, -0.2) | (-5.0, 1.6) | (-1.1, 3.9) |
| For women with PPH** | ||||||||||
| Oxytocin administered - n/N (%) | 24/24 (100.0) | 25/25 (100.0) | 4/8 (50.0) | 5/15 (33.3) | NA | (-100.0, 2.0) | (-100.0, -30.9) | (-100.0, 2.0) | (-100.0, -30.9) | (-79.8, 46.4) |
| TXA administered - n/N (%) | 0/24 (0.0) | 2/25 (8.0) | 0/8 (0.0) | 5/15 (33.3) | (-7.9, 23.9) | NA | (-2.4, 69.1) | (-23.9, 7.9) | (-13.8, 64.5) | (-2.4, 69.1) |
Notes: * Prevalences and 95% CI of treatment differences were adjusted (standardized) by age, gestational age, and parity (using T1 as the standard population); a design effect of 1.5 was used to account for clustering of participants within facilities. ** Outcomes for women with PPH could not be adjusted/standardized due to small sample sizes involved, but 95% CI were adjusted to account for clustering of participants within facilities, using a design effect of 1.5. † No color: p>0.05; in color: p<0.05. CI: Confidence interval, PPH: Postpartum hemorrhage, HSC: Heat-stable carbetocin, TXA: Tranexamic acid, n: Number of observations, N: Total number of participants in time period, NA: Not applicable as difference=0, T1: Time period 1, T2: Time period 2, T3: Time period 3, T4: Time period 4.
The incidence of visually diagnosed PPH in women ranged from 3% to 4%, with a notable decrease to 1% in T3. In terms of PPH treatment, oxytocin was administered universally in T1 (24 of 24) and T2 (25 of 25). However, its usage decreased to 50% in T3 (4 of 8) and further declined to 33% in T4 (5 of 15; T4–T1 95% CI: –100.0 to –30.9). TXA use varied across phases, but the differences were not statistically significant: 0% (0 of 24) in T1, 8% (9 of 16) in T2, 0% (0 of 8) in T3, and 33% (5 of 15) in T4. No serious adverse events related to the study were reported, and all participants were discharged alive.
DISCUSSION
In Ugandan refugee-hosting settings with limited cold chain reliability, our implementation research study aimed at assessing an HSC and TXA-inclusive capacity-building strategy on PPH prevention and treatment. We found that a stepwise approach incorporating HSC and TXA into a PPH intervention package significantly changed uterotonic selection for PPH prevention, with HSC being the primary choice of uterotonic in T3 and T4. While the rate of PPH diagnosis stayed consistent, there was a moderate increase in the use of TXA for treatment. The introduction of HSC for prevention led to a substantial and worrying reduction in oxytocin administration for PPH. Neither HSC nor TXA were used for treatment and prevention, respectively.
Throughout the study, challenges typical in humanitarian settings emerged. These included refugee influxes not only in the Western Uganda region due to increased insecurity in the Eastern Democratic Republic of Congo but also in the West Nile region due to the onset of civil war in Sudan, along with Ebola outbreaks hindering monitoring. Communication platforms like WhatsApp, zoom meetings, and phone calls proved valuable in addressing these challenges.
Baseline data indicated widespread uterotonic use for PPH prevention, similar to a Tanzanian hospital-based study.[23] Introducing HSC did not notably change prophylactic uterotonic trends. However, in the related study conducted in South Sudan, the use of uterotonics significantly increased from 98% in earlier phases (T1 and T2) to 100% in later phases (T3 and T4). A Ugandan National Drug Authority cold-chain assessment in selected study facilities revealed gaps in oxytocin storage conditions. This reinforced the understanding of our providers about the need to use quality uterotonics, emboldening them to administer HSC to about three-quarters of women in T3, and half in T4, due to supply shortages and staff turnover. Consequently, oxytocin use increased.
HSC’s longer half-life than oxytocin and misoprostol is noteworthy. Combined oxytocin and misoprostol use occurred in T1 and T2 (6%) and less in T3 (3%), mainly for high-risk PPH cases (e.g., grand multiparity, previous postpartum bleeding). Combining HSC with other uterotonics occurred in T4 (approximately 10%), but no severe side effects emerged. However, it is essential to note that the combined use of HSC with other uterotonics has not undergone extensive study, and therefore, its recommendation should be withheld at this stage.[24] A study from Egypt noted added PPH prevention benefits with oxytocin and HSC combined for cesarean sections.[25] Future training must stress avoiding HSC combination with other uterotonics for PPH prevention.
During PPH refresher training, a skill drills station required providers to visually estimate bleeding using stained drapes and dishes. Providers often underestimated blood loss, aligning with documented phenomena. For example, a Thailand study reported a 28% accuracy rate.[26] However, by introducing short didactic sessions and practical simulations, trainees can become aware of their visual bias and improve their estimation skills.[27] This improvement, albeit not statistically significant, was observed in the study conducted in South Sudan but not Uganda. PPH detection rates ranged from 3% to 4%, which remains lower than the prevalence reported in Uganda (9%) and sub-Saharan Africa (11%).[9,16] Accurate PPH documentation and early detection require calibrated drapes or low-technology blood collection tools. Post-training, a facility introduced quantification via a calibrated container. This approach was subsequently disseminated within the community of practice, leading to its eventual adoption by colleagues from four additional facilities. In 2023, the E-MOTIVE hospital-based study highlighted the role of calibrated drapes in triggering prompt PPH treatment measures.[28] While calibrated measurement gained traction in the context of quality improvement efforts following our study’s refresher training, further research is needed for feasibility in humanitarian and lower maternity care settings.
Following the official introduction of TXA in T4, only a third of women diagnosed with PPH received this treatment, in contrast to a much higher rate of 95% observed in a similar study conducted in South Sudan. Several factors contributed to this lower incidence as reported during monitoring and review visits. One factor was the turnover of staff during the later phases of the study, resulting in new staff members who were less familiar and confident with the use of TXA. Some staff members had a mistaken impression that TXA was a uterotonic. Additionally, in some cases of PPH, the bleeding subsided significantly with the implementation of other recommended measures, including the common use of misoprostol, leading to the perception that TXA was unnecessary.
During the refresher training prior to T2, healthcare providers had already been trained on the use of TXA. As a result, two women with PPH received TXA during T2. But none received it during T3, following a reminder about the study’s stepwise approach during supportive supervision.
Untimely TXA administration yielded insights; providers are inclined to use life-saving medications, even if reminded to wait. Access to TXA from external sources in T2 further confirmed this. TXA use for PPH treatment before HSC introduction for prevention did not adversely affect oxytocin use for either PPH prevention or treatment. However, T3 unexpectedly saw reduced PPH treatment with HSC introduction, revealing insights for future scaling efforts. This underscores the complexity of medication integration and provider behavior in introducing new interventions.
Oxytocin is widely recognized as a crucial component in treating PPH, and its use was universally commonly observed in T1 and T2, even when TXA was already employed for treatment during T2 before its official timing in T4. However, there was a concerning decline in its utilization, with only 50% of women with PPH receiving oxytocin during T3, and this further decreased to one-third in T4, coinciding with the introduction of HSC. A similar trend was observed in a study conducted in South Sudan, where universal oxytocin use during T1 and T2 decreased to 27% during T3, but then increased to 73% in T4 following close supportive supervision.
Upon reviewing the existing literature, we found no similar trends documented. This may be attributed to the fact that most studies primarily focused on investigating the safety and effectiveness of PPH medications for either prevention or treatment, without specifically monitoring the potential impact of using one medication on the usage of other available medications in the PPH management toolkit. Through close supportive supervision, we gained valuable insights into the confusion experienced by healthcare providers. Recognizing HSC’s derivation from oxytocin, certain providers postulated that the utilization of oxytocin for treatment might be redundant if HSC had been previously employed for prevention—instead, misoprostol was used for treatment. Despite close monitoring, this misconception persisted in T4, partly due to staff turnover, as previously highlighted.
Strengths and Limitations of the Study
While our study merits attention for its focus on humanitarian and fragile settings, it has limitations. First, data collection relied on providers’ reports in maternity registers, potentially introducing errors. To mitigate this, weekly data reviews were conducted. Medication timing was not recorded due to its absence in registers. Second, blinding was not feasible in pragmatic facility-based implementation research, posing assessment bias risk. However, the observed HSC uptake could not be solely attributed to the Hawthorne effect, reporting errors, or bias. Third, our implementation research was not randomized and had six clusters, raising the risk of dissimilarities between the groups. However, each cluster had sizable samples, followed similar phased approaches, and included controlled phases. After adjustment for factors like age, gestational age, and parity, and accounting for clustering, results remained largely unchanged.
CONCLUSION AND GLOBAL HEALTH IMPLICATIONS
Despite limitations, implementing an HSC and TXA-based intervention for BEmONC services in humanitarian contexts yielded marked benefits. Notably, it led to a significant increase in the proportion of women receiving HSC for PPH prevention and a moderate uptake of TXA for PPH treatment. This study’s unique approach diverged from conventional hospital-focused research, concentrating on BEmONC facilities within fragile, humanitarian, and cold-chain-challenged settings. Given mounting evidence supporting HSC and TXA effectiveness and accessibility in high maternal mortality countries, resource-constrained settings can leverage strategies like our intervention package. This approach goes beyond simple HSC and TXA provision but instead integrates them within an intervention package aimed at improving the quality of care. Replacing oxytocin with HSC for prophylaxis may significantly alleviate cold-chain storage burdens in low-resource contexts. While cost-effectiveness, the key implementation research question from this study, requires additional research, the intervention’s nature and focus on strengthening providers’ BEmONC skills render its broad application feasible, including in Uganda and similar humanitarian contexts.
However, effective scale-up necessitates specific investments. Ongoing training and skill refreshment for new and existing staff are essential for successful implementation. Ongoing supportive supervision reinforces clinical practices and counters misconceptions, particularly regarding the necessity of continuing to use oxytocin for PPH treatment following prophylactic HSC. As oxytocin remains vital for PPH treatment, enhancing cold chains to ensure its quality is essential. Finally, close monitoring, assessing key PPH prevention and treatment indicators, and updating maternity registers are crucial. Sharing this intervention package with comparable facilities grappling with cold-chain limitations could accelerate progress against PPH and maternal mortality in high-burden humanitarian and fragile settings.
Key Messages
-
A postpartum hemorrhage (PPH) intervention package, enhancing routine obstetric services, can effectively increase the trends and types of uterotonics employed for PPH prevention [replacing oxytocin with heat-stable carbetocin (HSC)] while enabling tranexamic acid (TXA) administration for one-third of PPH cases.
-
The gradual integration of HSC and TXA in humanitarian and fragile contexts is feasible and acceptable to clinicians.
-
Continuous capacity enhancement and vigilant oversight is needed to avert and rectify potential confusion between established and novel pharmaceutical agents.
Acknowledgments
We express our gratitude to Nadine Corner for conceptualizing the study and to Danielle Jurman and Agnes Chidanyika for effectively managing the in-country supply of both medications in a timely manner.
COMPLIANCE WITH ETHICAL STANDARDS
Conflicts of Interest
The authors declare no competing interests.
Financial Disclosure
Nothing to declare.
Funding/Support
Ferring Pharmaceuticals generously provided funding and supplies for the study components with heat-stable carbetocin—the donor had no role in the design of the study and interpretation of the results. The UNFPA Procurement Service Branch supported the implementation of the phase with tranexamic acid. The publication of this study was supported by funding from MSD, through its MSD for Mothers initiative and is the sole responsibility of the authors. MSD for Mothers is an initiative of Merck & Co., Inc., Rahway, NJ, U.S.A.
Ethics Approval
The study strictly adhered to the ethical principles outlined in the Declaration of Helsinki and received approval from the Uganda National Council for Science and Technology (UNCST; HS2456ES). Data was collected and extracted from maternity registers without any identification of the individual study participants. Given that information was not directly obtained from participants but from routine maternity registers, and participant interviews did not occur, the UNCST advised that individual informed consent from study participants was not deemed necessary. It is worth noting that a similar approach, without individual informed consent, was also adopted for the WHO multicountry survey on maternal and newborn health, which encompassed Uganda as one of its participant countries (Souza JP et al. The WHO multicountry survey on maternal and newborn health: study protocol. BMC Health Services Research 2011, 11:286).[29] In addition to obtaining the UNCST approval, authorization to conduct the study and utilize its results in reports and publications was acquired from the responsible authority in all the health facilities involved in the research.
Declaration of Patient Consent
Patient consent is not required as patients’ identity is not disclosed or compromised.
Use of Artificial Intelligence (AI)-Assisted Technology for Manuscript Preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The opinions expressed are those of the authors and do not necessarily reflect the views of the funding agencies. The UNFPA is solely interested in studying the implementation of HSC and TXA from a public health and emergency response standpoint. The aim is to potentially include the drugs in the complementary items offered through UNFPA Procurement and Supply for certain contexts. It is important to note that the factors motivating UNFPA to consider adding HSC and TXA to its catalog for specific situations might differ from the considerations of national health authorities.
Special Collection
This article is published as part of the special collection on prevention and treatment of postpartum hemorrhage in high-burden low- and middle-income countries: building cross-national evidence through implementation research.
REFERENCES
- WHO recommendations for the prevention and treatment of postpartum haemorrhage. Geneva: World Health Organization; 2012.
- Trends in maternal mortality 2000 to 2020: estimates by WHO, UNICEF, UNFPA, World Bank Group and UNDESA/Population Division; 2023.
- Postpartum hemorrhage: Epidemiology, risk factors, and causes. Clin Obstet Gynecol.. 2010;53(1):147-56.
- [CrossRef] [PubMed] [Google Scholar]
- Active versus expectant management for women in the third stage of labour. Cochrane Database Syst Rev. 2019;2(2):CD007412.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- WHO recommendations: Uterotonics for the prevention of postpartum haemorrhage. Geneva: World Health Organization; 2018.
- WHO Model Lists of Essential Medicines, 21st List 2019. Geneva: World Health Organization; ; 2019.
- UNFPA Procurement Services: Product Catalogue; 2021.
- Cost-effectiveness and budget impact of heat-stable carbetocin compared to oxytocin and misoprostol for the prevention of postpartum hemorrhage (PPH) in women giving birth in India. BMC Health Serv Res. 2023;23(1):267.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Epidemiology of postpartum haemorrhage: A systematic review. Best Pract Res Clin Obstet Gynaecol. 2008;22(6):999-1012.
- [CrossRef] [PubMed] [Google Scholar]
- Effect of tranexamic acid on surgical bleeding: Systematic review and cumulative meta-analysis. BMJ. 2012;344:e3054.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Antifibrinolytic drugs for acute traumatic injury. Cochrane Database Syst Rev. 2015;2015(5):CD004896.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Effect of early tranexamic acid administration on mortality, hysterectomy, and other morbidities in women with post-partum haemorrhage (WOMAN): An international, randomised, double-blind, placebo-controlled trial. Lancet. 2017;389(10084):2105-16.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Implementing heat-stable carbetocin for postpartum haemorrhage prevention in low-resource settings: A rapid scoping review. Int J Environ Res Public Health. 2022;19(7):3765.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Tranexamic acid for postpartum hemorrhage treatment in low-resource settings: A rapid scoping review. Int J Environ Res Public Health. 2022;19(12):7385.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- World Bank Group country classifications by income level for FY24 (July 1, 2023-June 30, 2024). World Bank; 2023.
- Incidence and risk factors for postpartum hemorrhage in Uganda. Reprod Health. 2016;13:38.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- A mixed-methods study of barriers and facilitators to the implementation of postpartum hemorrhage guidelines in Uganda. Int J Gynaecol Obstet. 2016;132(1):89-93.
- [CrossRef] [PubMed] [Google Scholar]
- Uganda - population dashboard: Overview of refugees and asylum-seekers in Uganda as of 30-June-2023.
- Implementation research: What it is and how to do it. BMJ. 2013;347:f6753.
- [CrossRef] [PubMed] [Google Scholar]
- Improving the reporting quality of nonrandomized evaluations of behavioral and public health interventions: the TREND statement. Am J Public Health. 2004;94(3):361-6.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Improving the reporting of pragmatic trials: an extension of the CONSORT statement. BMJ. 2008;337:a2390.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Uterotonics for prevention of postpartum haemorrhage: EN-BIRTH multi-country validation study. BMC Pregnancy and Childbirth. 2021;21(1):1-17.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Uterotonic agents for preventing postpartum haemorrhage: A network meta‐analysis. Cochrane Database Syst Rev. 2018;12(12):CD011689.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Oxytocin infusion after oxytocin bolus and carbetocin bolus to reduce blood loss during and after cesarean section—a randomized clinical trial. Med J Cairo Univ. 2015;83(1):79-83.
- [Google Scholar]
- Postpartum blood loss: Visual estimation versus objective quantification with a novel birthing drape. Singapore Med J. 2016;57(6):325.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Estimating blood loss: Can teaching significantly improve visual estimation? Obstet Gynecol. 2004;104(3):601-6.
- [CrossRef] [PubMed] [Google Scholar]
- Randomized trial of early detection and treatment of postpartum hemorrhage. N Engl J Med. 2023;389(1):11-21.
- [CrossRef] [PubMed] [Google Scholar]
- The world health organization multicountry survey on maternal and newborn health: study protocol. BMC health services research. 2011;11:1-0.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]





