Translate this page into:
Progresses and challenges of utilizing traditional birth attendants in maternal and child health in Nigeria
*Corresponding author’s email: ndidiamaka.amutah_onukagha@tufts.edu
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Background and Objectives:
Despite advances in modern healthcare, Traditional Birth Attendants (TBA) have continued to be heavily utilized in rural communities in Nigeria. Major disparities in maternal health care in Nigeria remain present despite the goal of the United Nations Millennium Development Goal to reduce maternal mortality by 2015. The objective of this study is to review the contribution of TBAs in the birthing process in Nigeria, and to examine barriers and opportunities for utilizing TBAs in improving maternal and child health outcomes in Nigeria.
Methods:
A literature review of two major electronic databases was conducted using the PRISMA framework to identify English language studies conducted between 2006 and 2016. Inclusion criteria included articles that examined the role of traditional birth attendants as a factor influencing maternal health in Nigeria.
Results:
The value of TBAs has not been fully examined as few studies have aimed to examine its potential role in reducing maternal mortality with proper training. Eight manuscripts that were examined highlighted the role of TBAs in maternal health including outcomes of utilizing trained versus non-trained TBAs.
Conclusion and Global Health Implications:
Specific areas of training for TBAs that were identified and recommended in review including: recognizing delivery complications, community support for TBA practices through policy, evaluation of TBA training programs and increasing collaboration between healthcare facilities and TBAs. Policies focused on improving access to health services and importantly, formal health education training to TBAs, are required to improve maternal health outcomes and underserved communities.
Keywords
Maternal and Child Health in Nigeria
Traditional birth attendant
Training
Birthing process
1. Background and Objectives
Nigeria is comprised of 774 local governments and 374 ethnic groups, thus setting the stage for great variability in customs and traditions regarding childbirth and postnatal practices.[1] Table 1 describes Millennium Development Goal 5 (MDG 5) and the factors that influence maternal health in Nigeria. The MDG 5 goal set by the United Nations is to improve maternal health by reducing the maternal mortality rate (MMR) by three-fourths by 2015.[2] Nigeria was identified as one of the countries that needed to achieve MDG 5 due to the high maternal mortality rates occurring in the country.[2] The 2013 Nigerian National Demographic and Health Survey (NDHS) reported the maternal mortality ratio was 576 deaths per 100,000 live births. Exposure to hemorrhages, infections, unsafe abortions, obstetric emergencies, HIV/AIDS and meningitis leave women at risk of mortality due to unsafe practices.[3] Lack of access to quality health care, lack of skilled health workers, education and poverty are some of the structural factors that have contributed to maternity and infant mortality rates in Nigeria especially in rural areas, leaving women and children at higher risk of exposure to dangerous delivery practices that contribute to high mortality.[3] Before modern medicine, mothers and mothers-in-law often assisted their daughters with delivery and would depend on Traditional Birth Attendants (TBAs), if issues or complications were to arise.
| Maternal mortality | |
|---|---|
|
MDG 5 goal: The MDG 5 goal set by the United Nations is to improve maternal health by reducing the maternal mortality rate by three-fourths by 2015 (WHO: Partnership for Maternal, Newborn, and Child Health). Why it’s important: Disparities are present in maternal mortalities. Sub-Saharan Africa made up around 56% of global maternal deaths and Southern Asia made up 29% in 2010, totaling 85% of global maternal deaths (Odusola, 2013). Nigeria has a high maternal mortality rate. The reported maternal mortality ratio was 576 deaths per 100,000 live births (Nigerian National Demographic and Health Survey, 2013). |
Causes of maternal mortality: Exposure to hemorrhages, infections, unsafe abortions, HIV/AIDS and meningitis leave women at risk of mortality due to unsafe practices (Owens-Ibie, 2011). Lack of access to quality health care, lack of skilled health workers, education and poverty are structural factors that have contributed to maternity mortality rates in Nigeria, especially in rural areas (Odusola, 2013). |
Traditional Birth Attendants (TBAs) in Nigeria have the potential to contribute significantly to maternal health outcomes because of their high utilization within the country. TBAs are defined as providers who are traditionally independent of the health system, and are community-based providers of care during pregnancy, childbirth and the postnatal period.[2] TBAs do not receive formal medical training when compared to other health professionals such as obstetricians and gynecologists. However, TBA’s are much more affordable and accessible than skilled birth attendants (SBAs) in most parts of the country. Most TBAs are middle-aged or older women and are highly respected in their roles as midwives to rural communities.[3,4]
Nigeria has an estimated population of over 100 million and about 80% of the population live in rural conditions.[5] Women living in rural areas are 77% more likely to give birth at home than in a health facility, which contributes to the high demand for TBAs.[6] Nigeria has made slow but progressive results in reducing maternal mortality rates since 1990 with a baseline figure of 1000 deaths per 100,000, 545 per 100,000 in 2007, 350 deaths per 100,000 live births in 2012 and then 243 per 100,000 live births in 2014.[6] However, maternal mortality rates remain high compared to other developing countries and it is important to address structural factors that are contributing to the high MMR witnessed in Nigeria.
In this paper, a purposive literature review examining the role of traditional birth attendants (TBAs) maternal health in Nigeria was conducted. An emphasis was placed on identifying the maternal health progresses and challenges, in order to examine the association of the utilization of TBAs and attainment of MDG. In examining the literature, the relationship between maternal health in Nigeria and current healthcare practices was explored to identify strategies that can aid in the reduction of maternal mortality through interventions that include TBAs. In addition, the current review sought to 1) compile current practices of TBAs in Nigeria and 2) to provide effective implications to policy pertaining to traditional birth attendants in order to improve the health of women and children in Nigeria.
2. Methods
Electronic databases (PubMed and EBSCOhost) were utilized to identify published empirical studies, review articles and policy briefs in order to: 1) compile current practices of traditional birth attendants in Nigeria 2) evaluate the progress of Nigeria’s plan according to Millennium Development 5 goals, and 3) provide effective implications on policies pertaining to traditional birth attendants in order to improve the health of women and children in Nigeria. Figure 1 illustrates the PRISMA model used for article selection.
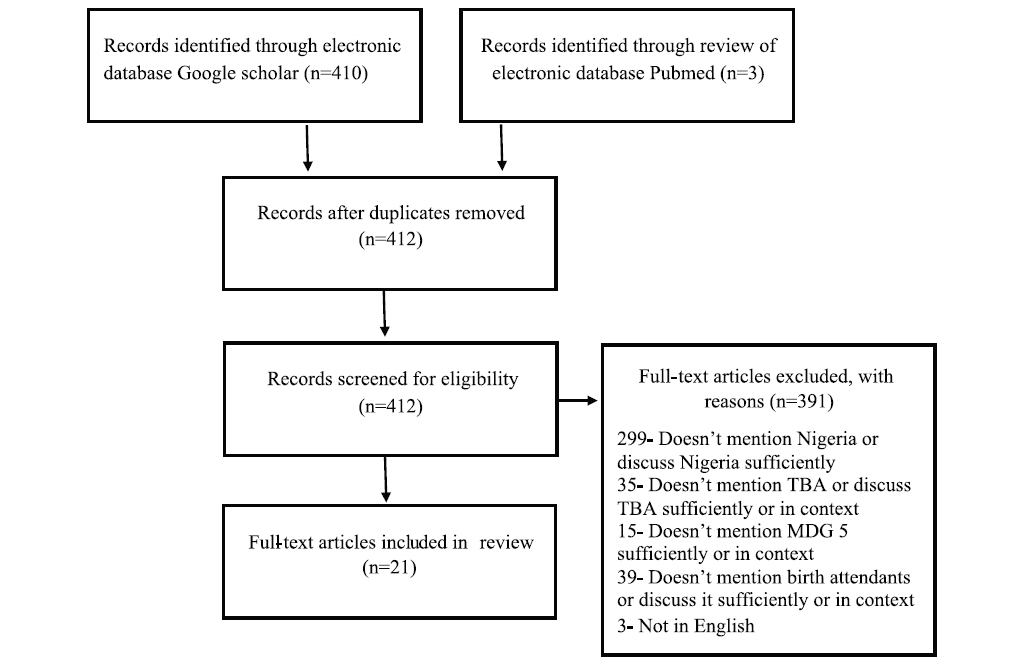
- Illustrates the PRISMA model for the literature review conducted on TBA and MDG 5
2.1. Inclusion criteria
We reviewed published abstracts and journal articles that reported on studies conducted in Nigeria pertaining to TBA utilization and practices, and reviewed articles that involved maternal and child health practices in Nigeria. In order to be included in this review, all studies and articles had to be published after January 2005. Search terms used were: “traditional,” “birth attendant,” “Nigeria,” “MDG 5.” It was found that the combination of these terms in addition to exclusion of articles before 2005 resulted in a number of articles that were related to Nigeria’s maternal health status while also sufficiently pertaining to traditional birth attendants and maternal death reduction.
Qualitative studies conducted in Nigeria were included in order to a) incorporate the lived experiences of Nigerian mothers who have utilized traditional birth attendant services in their communities and b) understand the experiences of traditional birth attendants and barriers that they perceived in providing quality healthcare through semi-structured interviews.
Quantitative studies were utilized in order to show statistical significance regarding the evaluation of training programs of traditional birth attendants, and to determine the effectiveness of such interventions in reducing the maternity and infant mortality ratio. Studies incorporating the quality of skilled services compared to traditional birth attendants were screened and included in order to investigate the advantages and disadvantages of such services and to provide implications on collaboration of care in order to reduce maternal and infant mortality rates in Nigeria. In addition, the Nigeria Millennium Development Goals 2015 report was reviewed in order to document the progress that Nigeria has made since the establishment of the MDG.
2.2. Exclusion criteria
Articles that were published before 2005 were not included as this review aims to incorporate a) current infant and maternal mortality prevalence, b) present community beliefs and practices of traditional birth attendants, and c) current utilization of traditional birth attendants; in order to have an accurate depiction of the phenomena in discussion. As the Millennium Development Goal 5 was established in 2000, it was important to incorporate literature that currently monitored progress of Millennium Development Goals specifically for Nigeria.
3. RESULTS
3.1. Characteristics of TBA Utilization
TBAs are often thought of as the bridge between formal healthcare and cultural methods.[7] TBAs provide a broad range of reproductive health services including antenatal care, labor and delivery, infertility treatment, and management of threatened abortion.[8] In a study conducted amongst the users of these services, 74.7 % were satisfied with their services.[9] Reasons individuals prefer TBA services were due to greater accessibility, better relationships, lower cost, convenience, and freedom to use traditional birthing positions.[10] Younger women, those who were not married, as well as grand multiparous women, were more likely to have delivered either by TBA/maternity; in many cases TBA services were the only maternity service that individuals are aware of.[11] In addition, one study found that some women only sought out health care from TBAs because they needed permission from their husbands to go to a healthcare facility.[12]
According to the latest NDHS data, 63% of all live births deliveries are delivered at home compared to 23 % that are delivered in public sector health facilities and 13% in private sector health facilities.[13] NDHS surveillance data shows that women with lower levels of educational attainment and lower income are most likely to deliver at home.[13] Duration of labor and financial constraints were also found to be a common reason for home birth preferences.[1]
Although home delivery is not associated with high maternity rates, much higher rates of intrauterine infections were observed in women who were attended at home by a TBAas compared to those who were attended in a hospital by skilled professionals.[14] A study found that typically following delivery, women can develop genital sepsis, wound infection or peritonitis and without proper postnatal care, these common complications can put a mother’s life at risk.[15]
3.2. TBA Training
An important predictor in MDG 5 attainment is the prevalence of women who use Skilled Birth Attendants (SBAs) during delivery.[16] A shortage of midwives, nurses and doctors exists worldwide. Approximately 4.3 million, and 57 countries experience the shortage most severely, including Nigeria.[17] In Nigeria, 41.2% of live births were assisted by skilled health workers. [2] A study found that 60% of TBAs had no formal education, 62.2% of TBAs acquired their skills by learning from a relative or family member and 8.9% had no training at all.[7]
To improve maternal health outcomes in northern Nigeria, a program was created that combined pivotal health system and community-based changes through trainings for staff of primary health care centers, and antenatal care services. [18] The results of the program showed a change from asking family, friends or TBAs for pregnancy and delivery advice to asking trained health workers. Deliveries attended by a TBA decreased from 54.7% to 39.1% from 2009 to 2013. An increase in deliveries attended by a SBA doubled to 23.9% and women receiving at least antenatal care service also doubled to 48.8%.[18] The findings demonstrate the potential that the health system and community-based services can have on helping to achieve the MDG 5.
Studies documented discrepancies in determining whether training TBAs are effective in achieving MDG 5. Studies have found postpartum hemorrhaging in mothers, which often leads to death. Lack of proper supervision, and an absence of emergency bacKUp systems during delivery have also been cited as barriers that are present even with the trained TBAs.[19, 20] In contrast, training of TBAs was shown to possibly increase the number of hospital referrals when obstetric complications occur in comparison to non-trained birth attendants, thus reducing maternal morbidity and mortality rates.[21] The lack of quality clinical trials that can produce significant results in determining whether training programs for TBAs are effective are not present, thus leading to the discrepancy in research regarding their effectiveness.[20]
Antenatal care by a healthcare professional is described as one of the most important maternal health services due to its ability to “detect, treat and/or prevent potentially dangerous complications,” which could lead to reducing maternal mortality.[22] Awareness and utilization of antenatal care services are recommended to achieve MDG 5. A study conducted in Northwestern Nigeria revealed that 28% of the 246 women cited non-use of antenatal care services due to preferring services of a TBA and 38.1% utilized a TBA. [23] A study conducted in India among trained and untrained TBAs found that 64% of untrained TBAs felt it was important for women to receive antenatal care services (ANC). [24] Additionally, over 80% of trained TBAs and 60% of untrained TBAs in the study expressed that safe delivery practices will reduce maternal and infant deaths.
Table 2 presents the ten areas in which training for TBAs is discussed and recommended by eight scholarly journal articles. The most salient topic that emerged was on training and sanitary delivery practices. Other areas that were mentioned frequently were: safe delivery practices (3), high risk indicators and referral (3 times) and breastfeeding practices (3 times). Additional areas mentioned include maternal nutrition, antenatal care/referral, immunization referral, HIV/AIDS awareness and prevention measures, postnatal care and family planning and contraceptive use.
| Source (Author, Year) | TBA training areas discussed/suggested | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Maternal nutrition | Antenatal care/referral | Immunization referral | Sanitary delivery practices: | Safe delivery practices | HIV/AIDS awareness and prevention measures | High risk indicators and referral | Breastfeeding practices | Postnatal care | Family planning and contraceptive use | |
| Balogun & Odeyemi, 2010 | X | |||||||||
| Dehinde, 2011 | X | |||||||||
| Bukar & Jauro, 2013 | X | |||||||||
| Agbo, 2013 | X | X | X | X | X | X | ||||
| Sibley & Sipe, 2006 | X | X | X | X | X | X | X | |||
| Satishchandra, Naik, Wantamutte, Mallapur & Sangolli, 2013 | X | X | X | X | ||||||
| Bassey, Elemuwa & Anukam, 2007 | X | X | X | |||||||
| Mboho, Eyo, Agbaje, 2012 | X | |||||||||
4. DISCUSSION
An analysis of the literature reveals an immense public health need for quality health education and training of TBAs in rural communities. Although Nigeria has reached its target regarding reducing maternal mortality rates, other indicators such as reducing maternal morbidity and increasing access to antennal care have not been met. Recommendations for improvements include: the recruitment and retention of skilled birth attendants, balancing the maldistribution of skilled health workers and encouraging women to deliver in a health care facility.[25]
Prior published research has focused on either: promoting skilled birth attendants, omitting TBAs from rural communities or additional training of TBAs. The research presented in this paper details what efforts are needed to improve the care of pregnant women and mothers and the need to accelerate progress in field of maternal health through a collaborative approach. In order to achieve this, policy makers, professional midwives, medical practitioners and funding organizations involved in the provision of maternity services must develop collaborative opportunities with TBA’s that encompasses mutual trust and respect for each other.[26]
Future research should focus on evaluating the impact of TBA trainings to ensure improvements in maternal health. Models have existed before in which Western-trained professionals work well alongside TBAs.[26] Even without training, TBA’s provide services that are beneficial to women that is founded on the intimacy of the relationships with mothers. Increases in trust between mothers and trained health professionals can build relationships similarly to those shared with TBAs. In addition, providing adequate health education and training to TBAs can have the potential to increase access to skilled birth attendant services through referrals.[27]
5. Conclusions and Global Health Implications
Training TBAs has been shown to increase the utilization of prenatal, antenatal, and postnatal healthcare of women who otherwise are unable to seek treatment from a skilled birth attendant.[28] Without formal training, TBAs are unable to identify the signs of a critical pregnancy or labor and delivery danger signs which can significantly put a mother’s life at risk.[29] Training of TBAs is recommended in addition to an increase of hospital births and informing women who utilize TBAs to request that they refer them to a health facility if they are unable to care for them properly.[1]
Providing quality maternal health training to TBAs will help them recognize their scope and limitations, and possibly refer mothers and their infants for immunization, family planning, and emergency services as needed.[7] TBAs, in addition to other community members who are influential in decision making, should be included in educational and communication activities. An example of this includes community mobilization to recommend oral misoprostol to prevent postpartum hemorrhaging, which has been effective.[19]
A lack of comprehensive maternal and child health infrastructure and a need for policy improvements were found as factors that influence maternal health in Nigeria. A reason for the high utilization rates of TBAs in rural areas is due largely to lack of access to health care facilities. Eliminating the utilization of TBAs in rural areas will not alleviate mortality rates but may actually exacerbate rates as it would leave mothers without access to any form of assistance. Policy makers, such as the International Confederation of Midwives (ICM), can advocate for the inclusion of TBAs as an important bridge to health care without excluding them. [27] WHO and the United Nations have acknowledged the importance of integrating TBAs in health care interventions and training TBAs in an aim to reduce mortality rates. Furthermore, government agencies should provide support in the strengthening of relationships between skilled health workers and TBAs. To improve the quality of care for women, cooperation and communication is needed between TBAs and health care workers. The communities’ input and participation can help improve programs and health service delivery. Policies that incorporate an ecological systems view, which acknowledges and recognizes the contributions of TBAs and socio-historical factors that encourage their utilization, is a step forward. This highlights the relevance of the important cultural and social roles that TBAs fulfill in their communities.
To reduce maternal mortality and improve maternal healthcare in Nigeria, an increase in quality health education for women and their family is essential. Additionally, the inclusion of culturally appropriate and sensitive health care practices is warranted.[10] With improvements in education for both men and women, in addition to improving the overall economic status of the families; a reduction in maternal deaths in communities is possible and likely.[27]
Paternal attitude is an important factor that influences many women when it comes seeking quality care due to negative outlooks within the health system. When men gave their wives more permission to go to a health care center, health care utilization increased.[18] Increasing the focus on the role of men in the pregnancy and postpartum period can be done by providing education, incentives, and support that can be instrumental in reducing maternal mortality and increasing health care usage among both men and women.
It is important to note that westernized medicine is often viewed as the preferred form of care which has contributed to the role of TBAs being devalued. Western medical knowledge is often used as the standard of acceptable medical practice, intentionally ignoring the cultural perspective and tradition into utilization thus perpetuating the roles of TBAS as inferior and unsafe. Reasons for the recent devaluation of TBAs role is also due to lack of evidence based literature and research that can support utilization of TBAs positively. Though there is no direct link to high utilization of TBAs and mortality rates in infant and mothers, researchers tend to attribute the use of TBAs to morbidity and mortality in countries where they are heavily utilized.
The high utilization rates of TBAs in rural areas and developing countries are not solely due to comfort level mothers but also to lack of access to health care facilities. Therefore, eliminating TBAs in rural areas will not alleviate mortality but may exacerbate rates as it would leave mothers and children without access to any form of assistance. When establishing goals for MDG 5, there should be more of a positive lens that highlights TBAs that have good intentions but are limited in skills and knowledge. TBAs are the bridge to reaching the community and providing the quality care needed for mothers.
Acknowledgements
This publication is/was fully/partially supported by the Global Health and Education Projects, Inc. (GHEP) under the Emerging Scholar’s Grant Program (ESGP). The information, contents and conclusions are those of the authors and should not be construed as the official position or policy of, nor should any endorsements be inferred by, ESGP or GHEP.
Conflict of Interest: The authors declare no relevant conflict of interest.
Ethics Approval: This study was approved by an Institutional Review Board
References
- Home births and postnatal practices in Madagali, North-Eastern Nigeria. Nigerian Journal of Clinical Practice. 2013;16(2):233-245.
- [Google Scholar]
- 2015. Partnership for Maternal, Newborn and Child Health. http://www.who.int/topics/millennium_development_goals/maternal_health/en/
- Traditional birth attendance and the pursuit of maternal and child health in Nigeria. Advances in Social Norms 2011
- [Google Scholar]
- Knowledge and practice of prevention of mother-to-child transmission of HIV among traditional birth attendants in Lagos State, Nigeria. Pan African Medical Journal. 2010;5(7):1-12.
- [Google Scholar]
- Assessing the role of traditional birth attendants (TBAs) in health care delivery in Edo State, Nigeria. African Journal of Reproductive Health. 2002;6(2):94-100.
- [Google Scholar]
- A Summary of Nigeria's Trends and End Point Status for Eight MDGs. 2015.
- Training of traditional birth attendants: a strategy for reduction of maternal and infant mortality. West African Journal of Nursing 2013:42-52.
- [Google Scholar]
- Assessment of the role of traditional birth attendants in maternal health care in Oredo local government area, Edo State, Nigeria. Journal of Community Medicine and Primary Health Care. 2005;17(1):55-60.
- [Google Scholar]
- Perception and utilization of traditional birth attendants by pregnant women attending primary health care clinics in a rural Local Government Area in Ogun State, Nigeria. International Journal of Women's Health. 2012;4:25-34.
- [Google Scholar]
- Maternal health-seeking behavior and associated factors in a rural Nigerian community. Maternal and Child Health Journal. 2006;10(2):159-169.
- [Google Scholar]
- Socio-demographic determinants of maternal health-care service among rural women in Anambra State, South East Nigeria. Annals of Medical and Health Sciences Research. 2014;4(3):376-382.
- [Google Scholar]
- Intergenerational differences in antenatal care and supervised deliveries in Nigeria. Health and Place. 2011;17:480-489.
- [Google Scholar]
- Nigeria Demographic and Health Survey 2013. Rockville (MD): National Population Commission and ICF International. Joint publication of ICF International. http://dhsprogram.com/pubs/pdf/FR293/FR293.pdf
- [Google Scholar]
- Maternal Birth Outcomes: Processes and Challenges in Anambra State, Nigeria. Health Care for Women International. 2011;32(6):492-514.
- [Google Scholar]
- Bacterial contamination of women in the labor supervised by traditional birth attendants. International Journal of Gynecology and Obstetrics. 2006;92:126-127.
- [Google Scholar]
- Determinants of noninstitutional deliveries in an urban community in Nigeria. Journal of Medical Investigations and Practice. 2014;9(3):102.
- [Google Scholar]
- Midwifery workforce management and innovation. The State of the World's Midwifery 2011:1-11.
- [Google Scholar]
- Reinvigorating health systems and community-based services to improve maternal health outcomes: case study from northern Nigeria. Journal of Primary Care and Community Health. 2015;6(2):88-99.
- [Google Scholar]
- Skilled birth attendance-lessons learnt. BJOG: An International Journal of Obstetrics & Gynaecology. 2009;116(1):33-40.
- [Google Scholar]
- Services of the traditional birth attendants: how relevant in achieving millennium development goal 5? Academic Research International. 2012;2(3):710-717.
- [Google Scholar]
- Using community-based research to shape the design and delivery of maternal health services in northern Nigeria. Reproductive Health Matters. 2012;20(39):104-112.
- [Google Scholar]
- Awareness and utilisation of antenatal care services and delivery services in a rural community, Northwestern Nigeria. Kanem Journal of Medical Sciences. 2011;5(2):43-49.
- [Google Scholar]
- Impact of training of traditional birth attendants on maternal health care: a community-based study. The Journal of Obstetrics and Gynecology of India. 2013;63(6):383-387.
- [Google Scholar]
- Knowledge of and challenges experienced by health workers managing maternity patients in primary health care clinics of Yobe State, Nigeria. [master's thesis]. Johannesburg, ZA: Witwatersrand University; 2014.
- Effect of shifting policies on traditional birth attendant training. Journal of Midwifery & Women's Health. 2004;49(4):306-311.
- [Google Scholar]
- Utilization of antenatal care and delivery services in Sgamu, south western Nigeria. African Journal of Reproductive Health. 2009;13(2):111-122.
- [Google Scholar]
- Transition to skilled birth attendance: is there a future role for traditional birth attendants? Journal of Health Population Nutrition. 2006;24(4):472-478.
- [Google Scholar]
- Awareness of critical danger signs of pregnancy and delivery preparations for delivery and utilization of skilled birth attendants in Nigeria. Journal of Health Care for the Poor and Underserved. 2013;24(1):152-170.
- [Google Scholar]





