Translate this page into:
Pulmonary Injury as a Complication of Urinary Tract Infection in Pregnancy

*Corresponding author: Wael Hafez, MD, Department of Internal Medicine, Medical Research and Clinical Studies Institute, The National Research Centre, Ad Doqi, Dokki, Cairo Governorate, Egypt. Tel: +20233371615, Waeelhafez@yahoo.com
-
Received: ,
Accepted: ,
How to cite this article: Hafez W, Al shareef J, Alyoussef A, Ghanem M, Abazid RR, Yadav A, et al. Pulmonary injury as a complication of urinary tract infection in pregnancy. Int J MCH AIDS. 2024;13:e012. doi: 10.25259/IJMA_15_2024
Abstract
Background and Objective
Pulmonary injuries resulting from urinary tract infections (UTIs) during pregnancy are rare. Prompt detection of pulmonary complications in pregnant patients with UTIs is crucial to prevent adverse outcomes in both the mother and the fetus. These complications may include respiratory issues, pulmonary edema, and exacerbation of preexisting conditions, such as asthma. We aimed to detect reported cases of pulmonary injury after UTIs among pregnancies.
Methods
We retrospectively reviewed the reported cases and articles in the PubMed database up to September 2023 on pulmonary injury after UTIs among pregnancies through a detailed search strategy. The titles and abstracts of the selected 15 articles were assessed, and ultimately, 7 articles were chosen based on adherence to our inclusion and exclusion criteria.
Results
Approximately 1–2% of women may develop acute pyelonephritis due to persistent UTIs, which has been associated with an increased risk of pulmonary edema in certain cases. UTIs can affect pulmonary health. Uremia, a consequence of UTIs, can lead to alterations in the respiratory drive, mechanics, muscle function, and gas exchange. Furthermore, urinary infection–induced inflammation activates neutrophils and promotes their recruitment to the lungs, compromising lung function and damaging the surrounding tissue.
Conclusion and Global Health Implications
Although systematic research on this topic is limited, there may be a link between UTIs and pulmonary damage. However, it remains unclear whether pregnancy exacerbates this association. For maternal health, child health, and the whole public health, it is important to raise awareness of physicians and gynecologists, as well as the different specialties like emergency and intensive care units, with more information about pulmonary injury after UTI in pregnancy; it is important to note that UTIs may not directly cause pulmonary complications, but physiological changes associated with pregnancy can increase this risk, so more care, observation, early detection, and treatment are critical for treating these complications and achieving best outcome in pregnant women with UTIs. More research is needed in this area, as the mechanism underlying the existence of pulmonary damage post-UTI in pregnancy is unclear.
Keywords
Pregnancy
Pulmonary Injury
Respiratory Complications
Review
UTI
INTRODUCTION
Pulmonary injury as a complication of urinary tract infection (UTI) during pregnancy is a rare occurrence.[1] However, it is essential to recognize that any septic condition in pregnant individuals can lead to respiratory complications, including acute respiratory distress syndrome (ARDS).[2] Early identification of ARDS in pregnant patients with UTI is critical to prevent adverse outcomes in both the mother and fetus.[3] Therefore, healthcare professionals must be vigilant about the risk of respiratory issues during pregnancy and educate pregnant women about these potential complications.[4]
Hospitalization due to UTI during pregnancy has been associated with adverse outcomes in infants, such as preterm delivery and cesarean section.[5] However, there is currently insufficient evidence to establish a significant link between UTIs and premature membrane rupture, low Apgar scores, and perinatal mortality. In conclusion, while pulmonary injury resulting from UTI during pregnancy is infrequent, close monitoring of pregnant women with UTIs for signs of respiratory distress is paramount. This narrative review aimed to highlight the pulmonary complications associated with UTIs during pregnancy by examining pregnancy-related UTIs, pulmonary injuries, potential mechanisms, clinical presentations, management approaches, and prognoses.
METHODS
This study adhered to the guidelines outlined in the Cochrane Handbook of Systematic Reviews and followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) Statement.[6]
Eligibility Criteria and Study Selection
Primary research articles investigating the occurrence of pulmonary injury as a complication of tract infections in pregnant women were included. Conference abstracts, editorials, animal studies, and review articles were excluded.
Screening and Data Extraction
We manually screened references within the included studies and cross-referenced articles for additional citations using the Al-Rayyan method.[7] Subsequently, two authors independently conducted a thorough review of the full text and extracted the following information: (1) study design; (2) primary and secondary objectives or case presentations; and (3) results and conclusions.
Literature Search
We performed a literature search of PubMed through September 2023, inclusive of all studies published before this date, using the following search terms:
((Pulmonary Injury) OR (Lung Injury) OR (Pulmonary Injuries) OR (Lung Injuries) OR (EVALI) OR (TRALI) OR (Pneumoconioses) OR (Pneumoconiosis) OR (Bagassosis) OR (Anthracoses) OR (Anthracosis) OR (Black Lung) OR (Coalworker Pneumoconiosis) OR (Coal Miner’s Lung) OR (Coal Miner Lung) OR (Coal Miners Lung) OR (Anthracosilicoses) OR (Anthracosilicoses) OR (Anthracosilicosis) OR (Asbestoses) OR (Asbestosis) OR (Beryllioses) OR (Berylliosis) OR (Beryllium Disease) OR (Anthracosilicoses) OR (AnthracosilicosIs) OR (Silicotuberculoses) OR (Silicotuberculosis) OR (Pulmonary Fibrosis – from Asbestos Exposure) OR (Idiopathic Interstitial Pneumonitis – from Asbestos Exposure) OR (Byssinosis) OR (Byssinoses) OR (Brown Lung) OR (Caplan Syndrome) OR (Caplan’s Syndrome) OR (Caplans Syndrome) OR (Siderosis) OR (Sideroses) OR (Silicoses) OR (Silicosis) OR (Radiation Pneumonia) OR (Radiation Pneumonitis) OR (Bronchopulmonary Dysplasia) OR (Pulmonary Complication) OR (Shock Lung) OR (ARDS) OR (Lung Complication) OR (Respiratory Complication) OR (Respiratory Distress)) AND ((Urinary Tract Infection) OR (UTI) OR (Bacteriuria) OR (Pyuria) OR (Schistosomiasis hematobium) OR (Schistosoma hematobia) OR (Urinary Schistosomiases) OR (Urinary Schistosomiasis) OR (Urogenital Schistosomiasis) OR (Urogenital Schistosomiases) AND (Gestation) OR (Pregnancies) OR (Pregnancy) OR (Gravidities) OR (Nulligravidity) OR (Gravidity) OR (Nulligravidities) OR (Primigravidity) OR (Primigravidities) OR (Multigravidity) OR (Multigravidities) OR (Obstetric Labor) OR (Cervical Ripening) OR (Labor Onset) OR (Fetal Malpresentation) OR (Fetal Presentation) OR (Labor Malpresentation) OR (Labor Presentation) OR (Labor Trial) OR (Trial of Labor) OR (Uterine Contraction) OR (Myometrial Contraction) OR (Maternal Fetal Exchange) OR (Transplacental Exposure) OR (Maternal-Fetal Exchange) OR (Primiparity) OR (Parity) OR (Multiparity) OR (Nulliparity) OR (Parturition) OR (Birth) OR (Lamaze Technique) OR (Placental Development) OR (Hemochorial Development) OR (Hemochorial Placental Development) OR (Placentation) OR (Luteal Function Maintenance) OR (Luteal Maintenance) OR (Maintenance of Luteal Function) OR (Corpus Luteum Maintenance) OR (Abortion) OR (Miscarriage) OR (Litter Size) OR (Twin) OR (Superfetation) OR (Pseudocyesis) OR (Pseudopregnancies) OR (Pseudopregnancy) OR (Prenatal Nutritional Physiology) OR (Prenatal Nutrition Physiology) OR (Pregnant)).
Data Extraction
In total, 290 articles were retrieved from PubMed using a predefined search method. Duplicate articles were not identified after the comprehensive screening. The titles and abstracts of the initially selected 15 articles were assessed, and ultimately, 7 articles were chosen based on adherence to our inclusion and exclusion criteria, as well as the availability of full-text articles[8-14]. The final selection of these articles was achieved through consensus between the authors Wael Hafez and Youssef Hossam. For a visual representation of the selection process and article screening, please refer to Figure 1. An overview of the included studies is presented in Table 1.
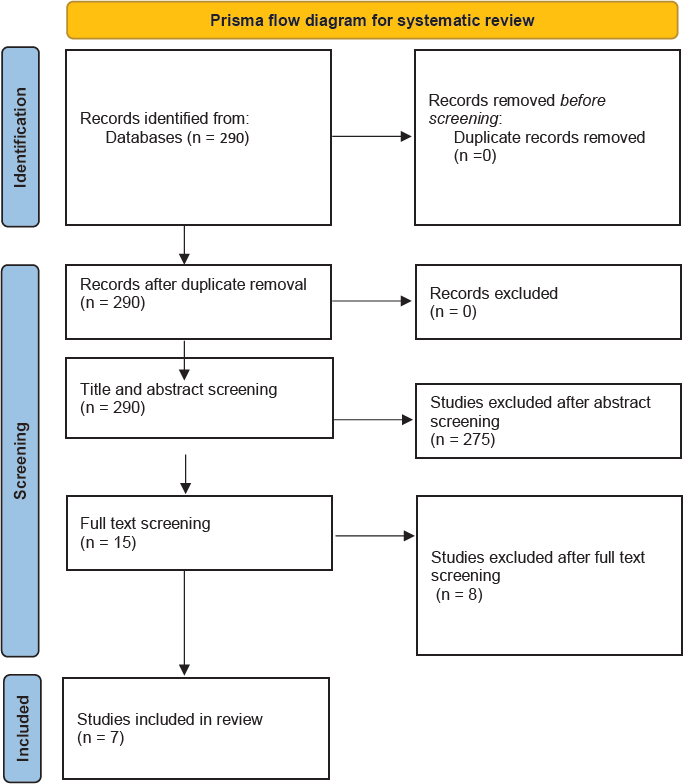
- Flow diagram illustrating the article selection process adhering to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA). n = Number of articles.
| Study ID (First author and period) | Title | Study Design | Major Aim\Case Presentation | Secondary Aims | Endpoints and Conclusion | |
|---|---|---|---|---|---|---|
| Soisson AP et al.,1986[8] | Acute pyelonephritis is complicated by respiratory insufficiency. A case report. | Case Report | Among the diverse clinical manifestations encompassed by urinary tract infections, a prominent instance is acute pyelonephritis. This condition is commonly encountered during pregnancy and has recently been associated with the emergence of acute respiratory insufficiency. | |||
| Gwóźdź AZ et al., 1989[9] | Pulmonary edema in a pregnant woman with ureteral calculi complicated by pyelonephritis | Case Report | In the case of a 36-year-old pregnant woman in her 31st week of pregnancy, the presence of pulmonary edema emerged during the course of renal calculi complications associated with a urinary tract infection. | The immediate termination of the pregnancy through a Cesarean section, along with the administration of appropriate pharmacological therapy, resulted in the resolution of pulmonary edema, effective control of the urinary tract infection, and 4 weeks later, the spontaneous discharge of uroliths. | ||
| Gurman G et al., 1990[10] | Adult respiratory distress syndrome as a complication of acute pyelonephritis during pregnancy | Case Report | Two cases of acute respiratory distress syndrome (ARDS) stemming from complications of acute pyelonephritis during pregnancy are delineated. The severity of their clinical state necessitated the implementation of mechanical ventilation, incorporating heightened positive-end expiratory pressure for both patients. | The consideration of ARDS becomes imperative in instances of urinary tract infection when indications of hypoxia manifest during the third trimester of pregnancy. Timely recognition of the syndrome, sustained monitoring, and proactive intervention can mitigate the risk of maternal complications and/or fetal distress. | ||
| Weiner Z et al., 1992[11] | Pulmonary complications of antepartum pyelonephritis: more alertness is needed | Case Report | Three cases of pulmonary complications associated with pyelonephritis during the antepartum period are outlined. Tracheal intubation and mechanical ventilation were deemed necessary in two of these cases. All three cases were characterized by recurring urinary infections, the inadequacy of initial antimicrobial treatment, and concurrent utilization of tocolytic therapy. | This discussion covers the potential causes, risk elements, and clinical strategies intended to mitigate pulmonary complications in cases of pyelonephritis during pregnancy. | ||
| Hill JB et al., 2005[12] | Acute pyelonephritis in pregnancy | longitudinal study | This study investigates the frequency of pyelonephritis occurrences and explores the prevalence of associated risk factors and microbial pathogens. | This study aims to identify obstetric complications in women experiencing acute pyelonephritis during the antepartum period. | The occurrence of pyelonephritis has stayed at a low level since the introduction of routine prenatal screening for asymptomatic bacteriuria. In more than one-fifth of antepartum cases, pyelonephritis occurs during the first trimester. As pregnancy advances, gram-positive uropathogens become more prevalent. Maternal complications persist, but adverse obstetrical outcomes are infrequent. | |
| Collier SA et al., 2009[13] | Prevalence of self-reported infection during pregnancy among control mothers in the National Birth Defects Prevention Study | Cross-sectional study | This study aims to calculate the frequency of self-reported infections in a group of 4967 women who gave birth to infants without major birth defects | This study evaluates the frequency of documented infections and instances of fever, categorized by infection type, specific ailments, and maternal factors such as race and age. | This investigation underscores the prevalence of infections during pregnancy, indicating that even a minor elevation in the risk of birth defects or other adverse pregnancy outcomes could have significant public health implications. This emphasizes the crucial need to understand the ramifications of prenatal infections. | |
| Wing DA et al., 2013[14] | 2013 | Acute pyelonephritis in pregnancy: an 18-year retrospective analysis | Retrospective cohort study | This study provides an account of the occurrence of acute pyelonephritis during pregnancy. | This study examines the link between acute pyelonephritis during pregnancy and perinatal outcomes within an integrated healthcare system. | This research delineates the prevalence of pyelonephritis within an integrated healthcare system employing routine prenatal screening for asymptomatic bacteriuria. Maternal complications are commonly identified, and there exists an increased risk of preterm birth when compared to the general obstetric population. |
RESULTS
UTIs in Pregnancy
Prevalence and types of UTIs in pregnancy
UTIs are prevalent among pregnant women and can present significant risks to the health of both the mother and the fetus. Expectant mothers often experience asymptomatic bacteriuria, a type of UTI that lacks noticeable symptoms[15,16] For instance, in one study, approximately 26.0% of pregnant women attending two private tertiary medical college hospitals in Dhaka were found to have asymptomatic bacteriuria,[17] whereas another study reported a prevalence rate of 35% among pregnant women.[18]
UTIs during pregnancy are characterized by the substantial presence of bacteria anywhere in the urinary tract, with pyelonephritis representing the most severe bacterial infection that can lead to perinatal and maternal complications.[8-12,19] Pregnancy-induced physiological changes create favorable conditions for bacterial colonization in both the lower and upper urinary tract.[13,18] Consequently, it is advisable for all pregnant women to undergo urine culture screening for bacteriuria, and asymptomatic bacteriuria should be promptly addressed to prevent potential complications.[20] Treatment should be guided by the results of urine culture and sensitivity tests, and antibiotics should be administered for seven days.[21]
Risk factors of UTIs in pregnancy
Various factors elevate the risk of UTIs during pregnancy, including lower socioeconomic status,[14,22,23] history of UTIs, sexual activity during pregnancy, anemia, multiparity,[24] and factors such as illiteracy and the first trimester of pregnancy. Screening for UTIs in pregnant women, especially those with these risk factors, is crucial to prevent complications, such as severe preeclampsia.
Clinical presentation, diagnosis, and screening of UTIs in pregnancy
UTIs in pregnant women can manifest with different symptoms, depending on several factors. Some women may experience increased incontinence, while others may report heightened nocturia.[25] Women with recurrent UTIs may exhibit less dysuria but more severe symptoms, significantly affecting their daily lives.[26] Premenopausal women suspected of having UTIs may present with higher symptom severity and discomfort scores, including symptoms such as feeling unwell, painful urination, and dysuria.[26]
The most effective method for diagnosing UTIs in pregnant women involves urine culture and antimicrobial susceptibility testing.[27] This entails collecting a clean voided midstream urine sample from pregnant women and sending it to the laboratory for analysis. Urine samples were examined and cultured to detect the presence of bacteria and other infection-causing pathogens. The isolated pathogens were then tested for susceptibility to various antibiotics to determine the most appropriate treatment.[28,29] Regular screening for significant bacteriuria in all pregnant women is crucial to mitigate adverse effects on both maternal and fetal health.[28] In addition, it is essential to consider the gestational age of the pregnant woman, as UTI occurrence tends to increase as the pregnancy progresses.
DISCUSSION
Pulmonary Complications in UTIs During Pregnancy
Types of pulmonary complications
Pulmonary complications can arise in pregnant women with UTIs due to various factors. These complications may include respiratory issues, pulmonary edema, and exacerbation of preexisting conditions, such as asthma. It is important to note that UTIs themselves may not directly cause pulmonary complications, but physiological changes associated with pregnancy can increase this risk.[3,30] In addition, respiratory conditions such as pneumonia and tuberculosis can also pose risks during pregnancy, potentially leading to maternal and fetal morbidity.[30] Early diagnosis and prompt treatment are crucial for managing these complications and ensuring positive outcomes in pregnant women with UTIs.
Frequency of pulmonary complications due to UTIs
In the available literature, a few cases of ARDS resulting from UTI pyelonephritis during pregnancy have been reported.[31-34] Approximately 1–2% of women develop acute pyelonephritis as a consequence of persistent UTIs, which has been associated with an increased risk of pulmonary edema under certain circumstances. In contrast, ARDS is infrequently associated with acute pyelonephritis in nonpregnant women. Therefore, a theoretical connection between UTIs and pulmonary injuries in pregnant women has been proposed. Pregnant women with UTI symptoms and signs of hypoxia during their third trimester should be monitored for ARDS.[31] Notably, no data in the literature explicitly addresses the co-occurrence of UTIs and pulmonary injuries, underscoring the need for systematic reviews to provide precise statistics on their frequency and prevalence.
Special attention to pulmonary health in pregnant women with UTIs
Pregnant women undergo significant physiological and immunological changes, which can increase their susceptibility to, or severity of, certain pulmonary infections. These alterations also affect drug metabolism and treatment decisions. Effective management of conditions such as tuberculosis, influenza, and varicella pneumonia in pregnant women can lead to improved outcomes for both the mother and the child.[35] Given that pregnancy brings about profound changes in the cardiovascular, respiratory, immune, and hematologic systems, which can affect the clinical presentation of respiratory disorders, it is crucial to be vigilant about pulmonary complications during pregnancy to ensure adequate oxygenation for both the pregnant woman and fetus. Conditions such as asthma, tuberculosis, cystic fibrosis, and pneumonia should be addressed during prenatal visits to promote favorable maternal and fetal outcomes.[3] Building on the information provided in the previous section, it is advisable to manage pregnant women with established UTIs by closely monitoring their pulmonary systems through frequent examinations and investigations.
Mechanisms and Etiologies
Connection between the urinary and respiratory systems
A close and intricate connection exists between kidney and lung function in both healthy and ill states. Renal and pulmonary functions play essential roles in maintaining acid-base balance, regulating the levels of carbon dioxide and bicarbonate, controlling blood pressure, and managing fluid balance. These interactions commence during fetal development and frequently contribute to the onset and progression of various diseases. In pregnancy, urine plays a critical role as a component of the amniotic fluid and influences pulmonary development and growth.[36] In addition, during the first trimester of pregnancy, the kidney serves as the primary source of proline, which plays a crucial role in the maturation of the lung parenchyma and collagen synthesis.[37]
How UTIs can lead to pulmonary injury?
UTIs can indeed have implications for pulmonary health. Uremia, which is a consequence of UTIs, can lead to alterations in various aspects of respiratory function, including respiratory drive, mechanics, muscle function, and gas exchange.[38] Furthermore, UTIs can result in a range of systemic effects including volume overload, anemia, immune suppression, extraosseous calcification, malnutrition, electrolyte imbalances, and acid-base disturbances. These systemic effects can indirectly affect the pulmonary system.[39]
In patients undergoing chronic peritoneal dialysis, adaptations may occur that help mitigate the typical reductions in lung volumes, oxygen levels, and respiratory muscle strength observed during acute peritoneal dialysis.[10]
The role of infection, inflammation, and immune response on pulmonary injury
The UTIs can lead to bacterial colonization of urine, potentially resulting in fulminant sepsis and subsequent respiratory failure.[40] Inflammation triggers lung injury by activating neutrophils and promoting their recruitment to the lungs, leading to impaired lung function and tissue damage.[41] The release of microbicidal substances by activated neutrophils into the extracellular space can paradoxically harm host tissues.[42] Early pulmonary inflammation in acute lung injury (ALI) involves the accumulation of activated neutrophils in the lungs.[43] Platelets have also been found to stimulate the development of neutrophil extracellular traps (NETs) in transfusion-related acute lung injury (TRALI), further exacerbating lung endothelial injury.[44] Proinflammatory cytokines, which play critical roles in ALI pathogenesis, are associated with inflammation-induced lung injury. Inflammation is a key factor in the initiation and progression of various diseases.
Clinical Presentation and Diagnosis
Symptoms and signs of pulmonary injury in pregnant women with UTIs
Severe pyelonephritis during pregnancy can lead to pulmonary injury due to a systemic inflammatory response, affecting approximately 2% of women.[45] Pyelonephritis is associated with significant maternal and fetal morbidities, including conditions such as ARDS, sepsis, pulmonary embolism, and maternal or fetal death.[46] Symptoms of pulmonary injury include shortness of breath, coughing (potentially with bloody sputum), dizziness, chest pain, and leg swelling. Other signs indicative of pulmonary injury may include acute onset of dyspnea, tachypnea, tachycardia, pleuritic chest pain, and severe dyspnea.[47,48]
Challenges in diagnosis and differentiation from other conditions
Diagnosing pulmonary injury in pregnant women can be challenging, primarily because the physiological changes that occur during pregnancy can mimic the symptoms of other conditions.[49] In addition, UTIs may mask the inflammatory symptoms of pulmonary injuries. For example, instead of an immediately suspected respiratory system pathology, symptoms such as fever, dyspnea, cough, leukocytosis, and tachycardia might be considered signs of septicemia or Systemic Inflammatory Response Syndrome (SIRS) resulting from an underlying UTI.
As a result, diagnosing pulmonary complications in pregnant women with UTIs can be clinically challenging. Nevertheless, specific tests and imaging techniques can aid in diagnosing particular conditions. Pulmonary embolism in pregnant women can be diagnosed using ventilation-perfusion (V/Q) scanning or CT pulmonary angiography, while the diagnosis of ARDS relies on the identification of bilateral pulmonary infiltrates on chest X-ray or CT scan, along with the PaO2/FiO2 ratio.[50]
Treatment and Prevention
Treatment
Managing pulmonary complications during pregnancy can be challenging because of the anatomical and physiological changes. Treatment strategies often focus on symptom management and ensuring adequate oxygenation. The following are specific treatment approaches for pulmonary complications during pregnancy:[49]
Bacterial Pneumonia: The primary treatment for bacterial pneumonia during pregnancy involves supportive care with oxygen, proper antibiotics, bronchodilators, and, if necessary, ventilator support.[51]
Pulmonary Hypertension and Pulmonary Edema: These complications can arise in benign hydatidiform pregnancies due to trophoblastic pulmonary embolism (PE). Management may include supportive care such as oxygen and diuretics to reduce fluid overload.
Aspiration Pneumonia: Treatment for aspiration pneumonia is primarily supportive and includes oxygen, bronchodilators, antibiotics, and ventilatory support if needed.
Asthma: A multidisciplinary care team can help pregnant women manage their asthma symptoms and prevent exacerbations that may lead to hospitalization.
Thromboembolic Disease: Pregnancy increases the risk of thromboembolic events. Treatment may involve anticoagulation therapy, such as low-molecular-weight heparin, to prevent and manage these complications.[52]
Amniotic Fluid Embolism: This rare but life-threatening condition during pregnancy requires supportive treatment that focuses on maintaining adequate oxygenation and managing hemodynamic stability.
Prevention
Preventive measures are essential to maintain respiratory health during pregnancy. The following are some recommendations:[53]
Asthma Management: Pregnant women with asthma should continue their medication as usual, as pregnancy does not significantly affect the peak expiratory flow rate (PEFR) and forced expiratory volume in one second (FEV1). Safe treatments include inhaled and nebulized b2-agonists, inhaled and oral steroids, oral and intravenous theophyllines, and intravenous magnesium sulfate.
Respiratory Infections: Aggressive treatment of respiratory infections before delivery is crucial to prevent complications.
Preventing Blood Clots: All pregnant women can take steps to prevent blood clots. These measures include wearing compression stockings, maintaining physical activity, and staying well-hydrated.
Ideally, women with chronic pulmonary conditions should be evaluated before pregnancy to establish baseline pulmonary function, assess disease chronicity, evaluate inflammatory activity, determine disease staging, and assess treatment responses. These steps can contribute to improved management and outcomes during pregnancy.
Outcomes and Prognosis
The outcome and prognosis of pulmonary injury in pregnant women depend on the severity of the injury and its underlying cause. For instance, pulmonary hypertension among pregnant women poses a high mortality risk for both the mother and fetus.[54] A multicenter retrospective study revealed a high incidence of major adverse cardiovascular events in critically ill pregnant patients with pulmonary hypertension.[55] Pregnant patients experiencing acute respiratory failure during pregnancy or the peripartum period typically present with respiratory distress, and outcomes are contingent on the underlying cause of respiratory failure.[49] In summary, the outcomes and prognosis of pulmonary injury in pregnant women are closely linked to the severity of the injury and its root cause, emphasizing the need for individualized management.
Limitations
One limitation with our review was the scarcity of systematic reviews and metaanalyses that specifically address this subject. This limitation may have affected the depth and quality of the results and conclusions. Our study utilized PubMed as the sole database for conducting the literature search. While PubMed is a widely recognized and extensively used repository of biomedical literature, this approach introduces a limitation in the scope of our findings.
CONCLUSION AND GLOBAL HEALTH IMPLICATIONS
Throughout this review, we explored the intricate interplay between the respiratory and urinary systems, recognizing that imbalances caused by pathology in either system can potentially affect the others. The primary objective of this review was to determine whether specific UTIs affect the respiratory system and cause lung damage, particularly in pregnant women. Although case reports have addressed this correlation,[31-34] it is important to note that systematic research on this topic is limited.
Although the studies we found did not exclusively focus on pregnant women, many have discussed the etiology and potential for respiratory complications arising from UTIs. Thus, it is reasonable to consider UTIs as a potential risk factor for pulmonary injury in a broader context. The clinical presentation, diagnosis, treatment, and outcomes of pulmonary complications stemming from UTIs do not differ significantly from those of primary pulmonary pathologies.
Key Messages
It is important to note that UTIs may not directly cause pulmonary complications, but physiological changes associated with pregnancy can increase this risk.
Early diagnosis and prompt treatment are crucial for managing these complications and ensuring positive outcomes in pregnant women with UTIs.
More studies are needed in this regard, as the mechanism of the presence of pulmonary injury post-UTI among pregnancies is not clear.
Acknowledgments
None
COMPLIANCE WITH ETHICAL STANDARDS
Conflicts of Interest
There are no conflicts of interest.
Financial Disclosure
Nothing to declare.
Funding/Support
There was no funding for this study.
Ethics Approval
Institutional Review Board approval is not required.
Declaration of Patient Consent
Patient’s consent is not required as there are no patients in this study.
Use of Artificial Intelligence (AI)-Assisted Technology for Manuscript Preparation
The authors confirm that there was no use of Artificial Intelligence (AI)-Assisted Technology for assisting in the writing or editing of the manuscript and no images were manipulated using the AI.
Disclaimer
None.
References
- Urinary tract infections complicating pregnancy. Baillieres Clin Obstet Gynaecol. 1987;1(2):891-908.
- [CrossRef] [PubMed] [Google Scholar]
- Adult respiratory distress syndrome as a complication of acute pyelonephritis during pregnancy. Eur J Obstet Gynecol Reprod Biol. 1990;36(1):75-80.
- [CrossRef] [PubMed] [Google Scholar]
- Pulmonary disorders complicating pregnancy: An overview. J Perinat Neonatal Nurs. 2016;30(1):45-53.
- [CrossRef] [PubMed] [Google Scholar]
- Upper respiratory tract infection during pregnancy: Is it associated with adverse perinatal outcome? Am J Perinatol. 2010;27(8):619-24.
- [CrossRef] [PubMed] [Google Scholar]
- Pulmonary disorders complicating pregnancy. Obstet Gynecol Clin North Am. 1992;19(4):697-717.
- [PubMed] [Google Scholar]
- The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ. 2021;n71
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Learning to identify relevant studies for systematic reviews using random forest and external information. Machine Learning 2015:1-18.
- [Google Scholar]
- Acute pyelonephritis complicated by respiratory insufficiency. A case report. J Reprod Med. 1986;31(6):525-7.
- [PubMed] [Google Scholar]
- Obrzek płuc u ciezarnej w przebiegu kamicy moczowodowej powikłanej odmiedniczkowym zapaleniem nerek [Pulmonary edema in a pregnant woman with ureteral calculi complicated by pyelonephritis] Ginekol Pol. 1989;60(2):128-31.
- [PubMed] [Google Scholar]
- Adult respiratory distress syndrome as a complication of acute pyelonephritis during pregnancy. Eur J Obstet Gynecol Reprod Biol. 1990;36(1-2):75-80.
- [CrossRef] [PubMed] [Google Scholar]
- Pulmonary complications of antepartum pyelonephritis: More alertness is needed. Eur J Obstet Gynecol Reprod Biol. 1992;47(3):257-60.
- [CrossRef] [PubMed] [Google Scholar]
- Acute pyelonephritis in pregnancy. Obstet Gynecol. 2005;105(1):18-23.
- [CrossRef] [PubMed] [Google Scholar]
- National birth defects prevention study. Prevalence of self-reported infection during pregnancy among control mothers in the national birth defects prevention study. Birth Defects Res A Clin Mol Teratol. 2009;85(3):193-201.
- [CrossRef] [PubMed] [Google Scholar]
- Acute pyelonephritis in pregnancy: An 18-year retrospective analysis. Am J Obstet Gynecol. 2014;210(3):219.e1-6.
- [CrossRef] [PubMed] [Google Scholar]
- Urinary tract infections during pregnancy. Obstet Gynecol Clin North Am. 2001;28(3):581-91.9.
- [CrossRef] [PubMed] [Google Scholar]
- Urinary tract infections in pregnancy: Old and new unresolved diagnostic and therapeutic problems. Arch Med Sci. 2015;11(1):67-77.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Prevalence of UTI among pregnant women and its complications in newborns. Indian Journal of Pharmacy Practice. 2017;10(1):45-9.
- [Google Scholar]
- Urinary tract infections during pregnancy. Ann Pharmacother. 2004;38(10):1692-701.
- [CrossRef] [PubMed] [Google Scholar]
- Urinary tract infections in pregnancy. Clin Perinatol. 2005;32(3):749-64.
- [CrossRef] [PubMed] [Google Scholar]
- Urinary tract infection in pregnancy. The Obstetrician and Gynaecologist. 2008;10(3):156-62.
- [Google Scholar]
- Risk factors during pregnancy for asymptomatic bacteriuria. Journal of Pharmaceutical Research 2021:21-6. doi: 10.9734/JPRI/2021/V33I28B31532
- [CrossRef] [Google Scholar]
- Maternal age and stage of pregnancy as determinants of UTI in pregnancy: A case of tamale, ghana. Infect Dis Obstet Gynecol. 2022;2022:1-6.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Urinary tract infection (UTI) as a risk factor of severe preeclampsia. Global Journal of Health Science. 2016;8(11):77.
- [Google Scholar]
- A correlation of 8-hour and 12-hour with 24-hour urinary protein among pregnant women with preeclampsia in a teaching hospital in South-Western Nigeria. Research Journal of Health Sciences. 2023;11(3):244-53.
- [Google Scholar]
- Extended-spectrum beta-lactamase and metallo-beta-lactamase production among escherichia coli and klebsiella pneumoniae strains from urine of pregnant women in Afikpo, Ebonyi State, Nigeria. Biotechnology Journal International. 2023;27(4):35-45.
- [Google Scholar]
- Spectrum of uropathogens and their susceptibility to antimicrobials in pregnant women: a retrospective analysis of 5-year hospital data. J Int Med Res. 2021;49(5):3000605211006540.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Recommendations on screening for asymptomatic bacteriuria in pregnancy. CMAJ. 2018;190(27) doi: 10.1503/CMAJ.171325
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Bacteriological profile of urinary tract infections among pregnant women (Clinically Suspected of Having UTIs) in a tertiary care hospital. International Journal of Health Sciences and Research. 2016;6(8):119-24.
- [Google Scholar]
- Respiratory insufficiency associated with pyelonephritis during pregnancy. Obstet Gynecol. 1984;63(1):121-5.
- [PubMed] [Google Scholar]
- Adult respiratory distress syndrome as a complication of acute pyelonephritis during pregnancy: Case report and discussion. Obstet Gynecol. 1986;67(3 Suppl):18S-20S.
- [CrossRef] [PubMed] [Google Scholar]
- Pulmonary injury associated with antepartum pyelonephritis: Can patients at risk be identified? Am J Obstet Gynecol. 1991;164(4):974-80.
- [CrossRef] [PubMed] [Google Scholar]
- Pulmonary infections in pregnancy. Semin Respir Crit Care Med. 2017;38(2):174-84.
- [CrossRef] [PubMed] [Google Scholar]
- Kidney-lung connections in acute and chronic diseases: current perspectives. J Nephrol. 2016;29:341-8.
- [CrossRef] [PubMed] [Google Scholar]
- Respiratory considerations in the patient with renal failure. Respir Care. 2006;51(4):413-22.
- [PubMed] [Google Scholar]
- Risk of acute lung injury associated with nitrofurantoin use for urinary tract infection. . ;3(4):16-9.
- [Google Scholar]
- Effect of uremia and its treatment on pulmonary function. Lung. 1990;168(1):1-14.
- [CrossRef] [PubMed] [Google Scholar]
- Acute kidney injury in sepsis: More than just a brief encounter. Critical care medicine. 2013;41(4):1155-6.
- [CrossRef] [PubMed] [Google Scholar]
- Contribution of neutrophils to acute lung injury. Molecular medicine. 2011;17(3):293-307.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Platelets induce neutrophil extracellular traps in transfusion-related acute lung injury. J Clin Invest. 2012;122(7):2661-71.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Anti–spike IgG causes severe acute lung injury by skewing macrophage responses during acute SARS-CoV infection. JCI Insight. 2019;4(4)
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Cytokine-mediated inflammation in acute lung injury. Cytokine Growth Factor Rev. 2003;14(6):523-35.
- [CrossRef] [PubMed] [Google Scholar]
- Urinary Tract Infections in Pregnancy Clinical Presentation: History, Physical Examination, Complications. n.d.. Retrieved [Accessed September 18, 2023], Available from: https://emedicine.medscape.com/article/452604-clinical
- [Google Scholar]
- Pyelonephritis in pregnancy: Relationship of fever and maternal morbidity. AJP Rep. 2019;9(4):e366-e371.
- [CrossRef] [PubMed] [Google Scholar]
- Pulmonary complications of obstetric and gynecologic conditions. Pulmonary Complications of Non-Pulmonary Pediatric Disorders 2017 Oct 24:139-61.
- [Google Scholar]
- n.d.. Retrieved [Accessed on 2023 Sep 18]. Available from: https://emedicine.medscape.com/article/303852-overview
- Acute respiratory failure in pregnancy. Obstet Med. 2015;8(3):126-32.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Pulmonary thrombo-embolism in pregnancy: Diagnosis and management. Breathe (Sheff). 2015;11(4):282-9.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Pulmonary disorders in pregnancy. Medical Management of the Pregnant Patient 2014 Aug 13:235-57.
- [Google Scholar]
- Acute pulmonary embolism: Imaging techniques, findings, endovascular treatment and differential diagnoses. Rofo. 2020;192(1):38-49.
- [CrossRef] [PubMed] [Google Scholar]
- Respiratory disease in pregnancy. Obstet Gynaecol Reprod Med. 2007;17(5):140-6.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Pulmonary hypertension in pregnancy: Challenges and solutions. Integr Blood Press Control. 2022;15:33-41.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Pregnant outcomes of critically ill pregnant patients with pulmonary hypertension: A multicenter retrospective study. Frontiers in Cardiovascular Medicine. 2022;9:872833.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]





