Translate this page into:
Reinventing the Pregnancy Wheel to Improve Pregnancy Dating and Antenatal Care Visits: A Pilot Randomized Trial in Malawi
*Corresponding author email: ato8@case.edu
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Background and Objectives:
The purpose of this study was to evaluate the feasibility of a customized, culturally sensitive pregnancy wheel given to pregnant women to improve gestational age dating accuracy at the time of delivery and to improve antenatal care attendance.
Methods:
This was a pilot randomized trial involving pregnant women presenting to a regional hospital in Lilongwe, Malawi. The primary outcome was accuracy of gestational age at the time of presentation to the hospital in labor. The secondary outcome was the number of antenatal visits.
Results:
At final analysis, 14 subjects were included in the pregnancy wheel (intervention) arm and 11 in the standard care arm. Fifty percent (n=7) of women in the intervention arm were accurately dated at the time of presentation for delivery, compared to only 9% (n=1) in the standard antenatal care arm (p=0.04). There was not a significant difference in the number of antenatal visits between the two study arms. No patients met the World Health Organization’s recommended eight antenatal care visits for prenatal care.
Conclusion and Global Health Implications:
The customized pregnancy wheel given to patients could improve gestational age dating accuracy, and as a result, clinical decision making. However, the barriers to greater antenatal care access are more complex and likely require a more complex solution. Significant attrition in this pilot trial limited statistical power, suggesting the need for future larger interventions. Accurate gestational dating requires access to ultrasonography and early antenatal care initiation, both of which are inadequate in Malawi. Although the customized pregnancy wheel did not improve antenatal care attendance, it improved gestational age dating accuracy in a pilot study at a central hospital in Lilongwe, Malawi.
Keywords
Antenatal care
Feasibility
Gestational age
Low-resource Settings
Malawi
Pregnancy Dating
Pregnancy Wheel
Randomized Trial
The Malawian Pregnancy Wheel
1. Background and Objectives
Valid maternal and child health indicators and appropriate clinical decisions both rely on the accurate determination of the gestational age at which an infant is born.1-2 Accurate gestational dating often requires both ultrasound access and early antenatal care initiation, both of which are often lacking in low-resource areas.3-4 Guidelines for accurate dating combine both a woman’s recall of the first day of her last menstrual period (LMP) and a first trimester ultrasound to determine the estimated due date (EDD) of the pregnancy.3 However, in many low-resource countries, ultrasonography is not available due to its prohibitive cost and requirement for trained technicians.1 Therefore, in addition to LMP, crude estimates of gestational age using symphysial fundal height (SFH) measurements, even at the time of admission for labor, are commonly used for gestational dating.5
In Malawi, antenatal care and gestational dating are tracked by a government-issued health passport, though few women present for care prior to 16 weeks of gestation due to a variety of cultural and systemic factors.6 Each woman keeps her own pocket-sized book, which she brings to each visit and then to delivery. The passport serves as a mobile medical record and the primary form of communication between providers. If the EDD based on LMP or ultrasound is not clearly documented in the passport, a woman may be re-dated later in pregnancy, contributing to inaccurate gestational age estimation.
This feasibility trial proposes using the simple and widely used pregnancy dating wheel, customized for the setting in Malawi, as a tool to accurately calculate gestational age and improve antenatal care. This wheel is based off the standard gestational age wheel, which is used to predict gestational age based off LMP.7 The objective of this study is to determine whether a customized, culturally sensitive pregnancy wheel (The Malawian Pregnancy Wheel) improves the accuracy of gestational dating and enhances antenatal care attendance.
2. Methods
We designed a Malawian Pregnancy Wheel to give to the pregnant woman at her first antenatal visit for the primary objective of improving accuracy of gestational dating and the secondary objective to increase total antenatal visits, compared to women who did not receive the wheel (Figure 1). After consulting a variety of Malawian health care providers and women, we created the Malawian Pregnancy Wheel based on the months of the year in Chichewa (the local language) and the farming season of Malawi. Since 80% of the Malawian population lives through subsistence farming, we hypothesized that tracking a pregnancy via the farming seasons will help Malawian women conceptualize their accurate gestational age and the timing of the events throughout their pregnancy.8 The outer wheel features a pictorial guide to the seasons corresponding to a 12-month calendar, and the inner wheel features a pictorial guide corresponding to recommended antenatal visits with corresponding treatment and monitoring. Checkboxes above each antenatal visit remind women and their care providers to address appropriate tasks according to gestational age, such as albendazole treatment, intermittent malaria treatment, and regular blood pressure evaluations.
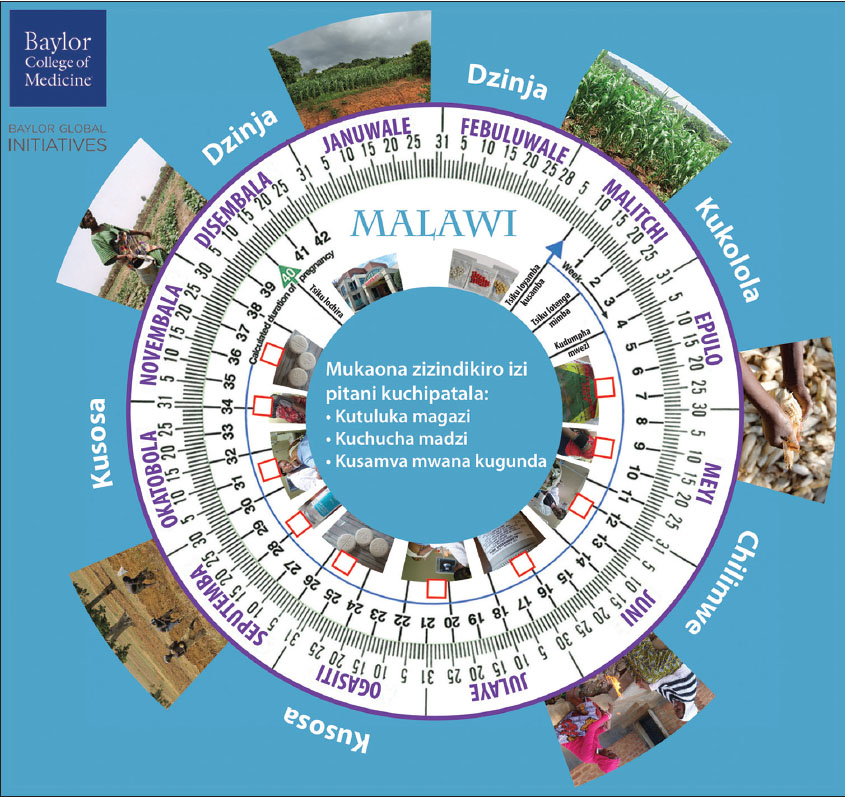
- The Malawian Pregnancy Wheel
This is a feasibility randomized trial to compare outcomes between pregnant women who received a customized pregnancy wheel at their first antenatal visit and pregnant women who received standard antenatal care at a central hospital in Lilongwe, Malawi. This study was approved by the Malawian National Health Sciences and Research Committee and the Baylor College of Medicine Institutional Review Board.
The primary outcome of this study was accuracy of gestational dating as recorded at the time of admission for labor. Accurate gestational dating was defined as within 1 week of the date recorded at the first antenatal visit, as any difference greater than this would be considered clinically significant. We hypothesized that women receiving the wheel would have a statistically significant improvement in accuracy of gestational dating. The secondary outcome was the total number of antenatal visits. We hypothesized that women receiving the pregnancy wheel would attend 30% more antenatal visits over their 9-month prenatal period compared to their counterparts not using the wheel.
Power analysis was conducted using 80% power, a two-tailed test, and assuming an alpha = 0.05. No clear literature describing gestational age dating could be found, therefore, we assumed approximately 20% of all patients had accurate gestational age dating. A clinically significant improvement in dating would be a change in proportion of 60%. Based on these assumptions, a total of 12 participants were required in each arm of the feasibility trial for a total of 24 study participants. However, we also powered the study to account for patterns of antenatal care in Malawi. The proportion of women currently attending 4 or more visits in an urban Malawi setting was found to be 46%.8 A desired difference in the proportion of women obtaining 4 or more visits with the intervention was 50%. Based on these assumptions, a sample size of 20 patients is required in each arm (total of 40 study participants).
Women presenting for their first antenatal visit at Kamuzu Central Hospital in Lilongwe, Malawi from June-July 2018 were eligible to enroll in the study. After undergoing informed consent, the participant had an initial ultrasound to assign gestational age and estimated date of delivery. Gestational age was calculated using the first day of the last menstrual period (LMP) with first ultrasound as confirmation of dates (or if LMP was unknown), according to ACOG guidelines.1 This gestational age and estimated day of delivery was written in the participant’s health passport as typically done at a first antenatal visit. An opaque envelope containing a number determining randomization to the pregnancy wheel arm versus the standard treatment arm was then opened. Randomization had been pre-determined using a computer-generated allocation. For participants allocated to the treatment arm, a customized pregnancy wheel was given and briefly explained. The same clinician performing the ultrasound also explained the pregnancy wheel: including the gestational age dating according to the outer wheel, and the images guiding antenatal milestones on the inner wheel aligned to months and seasons. Health care providers admitting participants for labor were blinded to the identity of study participants.
Participants’ contact information was collected regardless of which arm of the study the participant was enrolled. Research personnel explained that the participant should continue her normal antenatal care and inform us when she delivered. We also emphasized that the research team would need to see her health passport and pregnancy wheel after delivery and that she should contact us even if she delivered early, had a miscarriage, or a stillbirth.
After a participant contacted the research team at the time of her delivery, we reviewed her delivery record for gestational age and estimated due date assigned at the time of her labor admission. We reviewed the health passport to record the number of antenatal visits. If the subject was in the pregnancy wheel arm, the wheel was inspected for items checked off of the list. Accurate gestational age was determined to be a gestational age determined at the time of labor admission within 1 week of the date recorded at the first antenatal visit, as any difference greater than this would be considered clinically significant. Statistical analysis was performed using SAS OnDemand for Academics software (free cloud SAS version). Copyright © 2016 SAS Institute Inc. SAS and all other SAS Institute Inc. product or service names are registered trademarks or trademarks of SAS Institute Inc., Cary, NC, USA. Fisher exact tests were used to analyze categorical variables. Student t-test and Wilcoxon rank-sum test were used for normally and non-normally distributed continuous variables, respectively. P values of < 0.05 were considered significant.
3. Results
3.1 Study Participants
Forty women were eligible for enrollment. One participant in the standard arm was excluded after enrollment when no intrauterine pregnancy was seen on ultrasound. Of the 39 enrolled participants, three patients experienced a miscarriage in the second trimester. Four delivered at outlying hospitals where records were not retrievable. One patient died at delivery, and her record was not for available for review. Six records of patients who delivered at our hospital were missing and could not be located after multiple searches. Finally, one patient was lost to follow-up. At final analysis, 14 subjects were included in the intervention arm and 11 in the standard care arm.
Those randomized to the standard antenatal arm and the pregnancy wheel arm were not statistically significantly different in baseline demographics (Table 1). The rate of cesarean delivery was the same in both arms (36%). The mean gestational age for first antenatal visit was similar in both arms (18-21 weeks).
| Malawian Pregnancy Wheel N = 14 | Standard Antenatal Care N = 11 | P level | |
| Age | 0.10 | ||
| Mean (SD) | 33.1 (6.14) | 28.2 (6.63) | - |
| Median | 35 | 27 | - |
| Parity | 0.62 | ||
| Primiparity Mean (SD) | 2 (0.14) | 3 (0.27) | - |
| Multiparity Mean (SD) | 12 (0.86) | 8 (0.73) | - |
| GA at enrollment | 0.19 | ||
| Mean (SD) | 21.4 (4.11) | 18.82 (2.96) | - |
| Median | 22.5 | 19 | - |
| GA at delivery (based on dating at enrollment) | 0.06 | ||
| Mean (SD) | 38.6 (1.45) | 39.5 (1.69) | - |
| Median | 38.5 | 40 | - |
| GA recorded at delivery | 0.31 | ||
| Mean (SD) | 38.5 +/- 0.93 | 39.3 +/- 1.50 | - |
| Median | 39 | 39 | - |
| Mode of delivery | 1.0 | ||
| SVD Mean (SD) | 9 (0.64) | 7 (0.64) | - |
| CD Mean (SD) | 5 (0.36) | 4 (0.36) | - |
GA=gestational age (weeks), SVD=spontaneous vaginal delivery, CD=cesarean delivery
3.2. Accuracy of Gestational Dating
Objective outcomes are listed in Table 2. Fifty percent (n=7) of women in the intervention arm were accurately dated at the time of presentation for delivery, compared to only 9% (n=1) in the standard antenatal care arm (p=0.04). The pregnancy wheel intervention improved dating accuracy by over 5-fold compared to the standard arm, a statistically significant result; but the eleven patients in the standard arm falls short of the twelve calculated to power the study for clinical significance.
| Malawian Pregnancy Wheel N = 14 | Standard Antenatal Care N = 11 | P level | |
|---|---|---|---|
| Patients accurately dated, mean (SD) | 7 (0.50) | 1 (0.09) | 0.04 |
| Number of antenatal visits, mean (SD) | 4.3 (1.11) | 4.7 (1.25) | 0.40 |
| Percent meeting WHO recommendations | 0 | 0 | N/A |
3.3. Total Number of Antenatal Care Visits
Women in the intervention arm presented for 4.3 (+/- 1.11) antenatal care visits and women in the standard care arm presented for 4.7 (+/- 1.25) visits – no significant difference. No patients in our study met the WHO recommended eight visits for antenatal care.
4. Conclusion and Global Health Implications
The Malawian Pregnancy Wheel demonstrates the potential to improve the accuracy of the determination of gestational age at delivery. It is a simple, tangible, and culturally sensitive indicator for gestational age that both pregnant women and health care providers can refer to throughout the pregnancy. There is an unmet need in Malawi to improve the health literacy of pregnant women to motivate them to seek antenatal care.9,10 The Malawian Pregnancy Wheel has the future potential to fill this need, as women learn to track their pregnancy milestones, learn about necessary antenatal care visits, and recognize that their EDD should not change with subsequent evaluations by providers.
In low-resource settings, many women will not have access to ultrasound confirmation of their gestational age at their first antenatal visit. Without access to ultrasound, LMP can be used as a reliable estimation of gestational age, but only during early pregnancy.1 After the first trimester, a recent study comparing methods for gestational age estimation found that a single SFH measurement at 13-25 weeks gestation correlated best with ultrasound estimation.4 Perhaps these techniques, coupled with concrete documentation and tracking with the pregnancy wheel, would improve the accuracy of gestational age dating as the pregnancy progresses in areas where women lack access to ultrasound. In many of the delivery records, no gestational age was recorded anywhere in the chart, although it should have been available in the woman’s standard health passport. This omission indicates a missed opportunity in the standard antenatal and intrapartum care of women, and the pregnancy wheel can offer valuable supplement documentation to improve obstetric care.
However, the pregnancy wheel intervention did not increase the number of antenatal visits. Nor did it affect the gestational age at which women presented for their first antenatal care visit. Our finding that no women presented prior to 18 weeks is consistent with a previous study investigating barriers to antenatal care in Malawi, where only one in three women initiated antenatal care before 16 weeks, and only one in two before 20 weeks.6 The problem of late and scant antenatal care is multi-faceted, requiring a complex solution that would address both “socio-cultural factors” and “service delivery factors,” as recently observed by Chimatiro, et al. in their investigation of barriers to antenatal care in Malawi.11 Still, only 46% of Malawian pregnant women reach at least 4 antenatal care visits during their pregnancy.9 A recent commentary suggested that too many challenges remain in Malawi for women to meet the 2016 WHO recommendation of eight antenatal visits, and so four visits remains a more reasonable goal.12
The Malawian Pregnancy Wheel can be utilized as low-cost tool to manage obstetric complications. As many pregnancy complications occur in the first and third trimester, access to skilled antenatal care must be improved during these critical times. For example, first trimester care is essential to screen for ectopic pregnancy and medical co-morbidities, and third trimester care is necessary to screen for hypertensive disorders of pregnancy; but none of our cohort presented for care before 18 weeks, and few attended care in the final weeks before delivery. Our sample also included several miscarriages and even a maternal death. Although we did not survey pregnancy complications systematically, we did note that one patient was delivered by cesarean for pre-eclampsia with severe features and one for previous cesarean delivery when labor began. Such complications underscore a need for increased frequency and quality of antenatal care. Therefore, the Malawian Pregnancy Wheel tool would be especially useful in centers offering antenatal care for high-risk pregnancies. Future studies are warranted in order to further understand how to optimally utilize the pregnancy wheel to increase access to antenatal care.
Strengths of this study include the low-tech, cost-effective, culturally sensitive solution to a problem with large clinical impact. The Malawian Pregnancy Wheel is a portable tool that does not require electricity or literacy. The wheel could easily be transferred to another low-resource setting. Although this was a small sample as a pilot, the prospective nature of the study is a strength.
Limitations include the significant loss to follow-up and lack of access to delivery records. Although we anticipated such challenges in this setting, the extent was larger than we accounted for with our sample size. The significant limitations of record access, loss to follow-up, and maternal mortality should inform the sample size of future studies to account for expected attrition. Although this attrition limited our statistical power, this feasibility trial serves to lay the foundation for larger trials on interventions to improve gestational dating and antenatal care in low-resource settings.
Although the Malawian Pregnancy Wheel did not directly impact the initiation or frequency of antenatal care, the observation that no patient in either arm of the study meets the WHO recommended prenatal care reflects a larger problem related to access to and resources for adequate antenatal care. Cultural norms discourage women from reporting pregnancy and presenting for care before 18 weeks gestational age, and a mainstream sentiment that eight visits is not attainable in Malawi persists.11-13
The Malawian Pregnancy Wheel may be an effective and inexpensive intervention to improve the accuracy of gestational dating at delivery. A larger randomized controlled trial is warranted, as accurate dating has the potential to greatly improve maternal and neonatal care. While it may help reinforce the need for antenatal services, a larger-scaled intervention is needed to address the complex barriers to adequate antenatal care in low resource settings.
Acknowledgments:
Special thanks to the Malawian obstetricians/gynecologists and nurses who informed and consulted on the cultural appropriateness of the pregnancy wheel design. Thanks also to Ms. Abiba Matengula and Ms. Leslie Shrover who helped to develop this idea at the Baylor College of Medicine Global Health Hackathon.
Compliance with Ethical Standards
Conflicts of Interest: The authors declare that they have no conflict of interest.
Financial Disclosure: The authors declare that they have no financial disclosures.
Funding/Support: Funding for this study was from the generous donation of the Rottman Family Foundation and through the Baylor College of Medicine Global Health Hackathon prize.
Ethics Approval: This study was approved by the Malawian National Health Sciences and Research Committee and the Baylor College of Medicine Institutional Review Board.
Disclaimer: The authors declare that they have no disclaimers.
References
- Reliability and validity of last menstrual period for gestational age estimation in a low-to-middle-income setting. J Obstet Gynaecol Res. 2019;45(1):217-225.
- [Google Scholar]
- World Health Organization 2016
- Obstet Gynecol. 2017;129(5):e150-e154.
- The assessment of gestational age:a comparison of different methods from a malaria pregnancy cohort in sub-Saharan Africa. BMC Pregnancy Childbirth. 2019;19(1):1-9.
- [Google Scholar]
- Gestational age at first antenatal care visit in Malawi. Matern Child Health J. 2015;19(11):2366-2374.
- [Google Scholar]
- Paper gestational age wheels are generally inaccurate. Am J Obstet Gynecol. 2014;210(2):145.e1-4. doi:10.1016/j.ajog.2013.09.013 Epub 2013 Sep 11 PMID:24036402
- [Google Scholar]
- USAID. https://www.usaid.gov/malawi/agriculture-and-food-security Updated January 8, 2021
- Factors affecting antenatal care attendance:results from qualitative studies in Ghana, Kenya and Malawi. PloS One. 2013;8(1):e53747. Doi:10.1371/journal.pone.0053747
- [Google Scholar]
- The role of cultural beliefs in accessing antenatal care in Malawi:a qualitative study. Public Health Nurs. 2016;34(1):42-49.
- [Google Scholar]
- Understanding barriers preventing pregnant women from starting antenatal clinic in the first trimester of pregnancy in Ntcheu District-Malawi. Reprod Health. 2018;15(1):158.
- [Google Scholar]
- WHO guidelines not feasible for Malawi. The Nation Online. https://www.mwnation.com/who-guidelines-not-feasible-for-malawi/ Updated January 22, 2019
- [Google Scholar]
- The patient-provider relationship and antenatal care uptake at two referral hospitals in Malawi:A qualitative study. Malawi Med J. 2015;27(4):145-150.
- [Google Scholar]





