Translate this page into:
Urogenital Schistosomiasis among Primary School Children in Rural Communities in Obudu, Southern Nigeria
*Corresponding author email: yaro.ca@uniuyo.edu.ng
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Background:
Schistosomiasis is a Neglected Tropical Disease (NTD) that constitutes a public health problem in Sub-Saharan Africa (SSA), including Nigeria. There is need for updated information on the extent of the disease burden at community level to facilitate effective prioritization and monitoring of the disease.
Methods:
A cross-sectional study was conducted among school-aged children in Obudu Local Government Area (LGA), one of the 18 LGAs in Cross River State, Southern Nigeria. Seven schools from seven communities were randomly selected for this study. A total of 1,113 urine samples obtained from school-aged children were screened for Schistosoma haematobium (S. haematobium) eggs using standard parasitological method of diagnosis. Proteinuria and hematuria were evaluated using reagent test strips.
Results:
In this study, 153 (13.7%) children were infected with S. haematobium. More males (86 or 14.7%) were infected than females (67 or 12.7%); the differences were not statistically significant. The overall geometric mean intensity of infection was 13.3 eggs/10ml of urine. Females (13.69 eggs/10ml of urine) had the highest intensity of infection than males (12.91eggs/10ml of urine). Prevalence of hematuria was 152 (13.7%) (95% C.I. = 10.649 – 18.751%) while the prevalence of proteinuria was 172 (15.5%) (95% C.I. = 5.162 – 38.712%). Prevalence of infection significantly (p<0.001) varied among the schools from 7.8% to 28.9%. Children aged 5-9 years old had the highest prevalence of infection 46 (17.1%). The prevalence of urogenital schistosomiasis was 28.9%, 20.5% and 13.2%, respectively, among Betukwel, Ibong, and Ohong communities.
Conclusion and Global Health Implications:
Urinary schistosomiasis is still endemic in Obudu, Southern Nigeria but with decreased prevalence. Public health mitigation efforts such as mass chemotherapy, provision of safe water supply and sanitation facilities are recommended. Furthermore, health education should be encouraged within schools and communities.
Keywords
Schistosoma haematobium
Communities
Schools
Neglected tropical diseases
School-aged children
Parasitology
Chemotherapy
Proteinuria
Hematuria
Obudu
Cross River State
Nigeria
1. Introduction
1.1. Background of the Study
Urogenital schistosomiasis caused by infection with Schistosoma haematobium (S. haematobium) is widespread and causes morbidity on the African continent.1 The World Health Organization (WHO) regards the disease as a Neglected Tropical Disease (NTD) with an estimated 732 million persons being vulnerable to infection worldwide in renowned transmission areas.2 However, 85% of the cases reported annually occur in sub-Saharan Africa (SSA) and over 150,000 deaths are attributable to chronic infection with S. haematobium within regions.3 Within SSA, Nigeria has the highest prevalence of human schistosomiasis5 with about 29 million infected people.4 Other SSA countries such as Kenya6 and Ethiopia7 estimate that 6 million and over 5 million people are infected with 15 million and 37 million people at risk of infection, respectively.
Humans are infected with this disease when they come in contact with water bodies infested with skin penetrating cercariae. Adult S. haematobium inhabit the venules surrounding organs of the pelvis where they lay between 20 and 200 eggs daily.2 During infection, the parasites deposit terminal spine eggs which clog the venous plexus, impeding blood flow.8 The eggs of S. haematobium provoke granulomatous inflammation, ulceration and pseudo-polyposis of the vesical and ureteral walls. Hematuria is a very common sign of infection but other signs include dysuria, pollakisuria and proteinuria while the mortality caused by schistosomiasis is very low, subtle and indirect morbidities such as fatigue, physical or cognitive impairment are common in children.9
In Nigeria, urogenital schistosomiasis is widespread in both rural and urban communities.10,11 and the national policy on schistosomiasis control adopted praziquantel as the main drug of choice in the control strategy aimed at reducing morbidity. Dishearteningly, not much progress has been made in the control of urogenital schistosomiasis in the country. Presumably, the disease is more endemic in poor rural communities especially places where fishing and agricultural activities are dominant. There is a high level of the risk of becoming infected as a result of low literacy level, poverty, sub-standard hygiene and inadequate public infrastructure.12
Prior studies have reported the endemicity of urinary schistosomiasis in Southern Nigeria13,14 and specifically in Obudu.15 However, there is paucity of current scientific information on the endemicity of urinary schistosomiasis in many parts of the country especially in the rural areas where the high-risk population are school aged children. Therefore, there is need to provide updated information on the status of urinary schistosomiasis in Southern Nigeria. In addition, previous studies10,15,16 on urinary schistosomiasis from this region obtained their samples from one or two communities, but this study increased the geographical coverage to seven communities to provide larger and adequate information on the disease.
1.2. Objective of the Study
Despite considerable efforts to scale-up treatment activities in all states of Nigeria, coverage still remains poor in most rural and hard to reach communities. This study was designed with the aim of providing updated information on the extent of disease burden among primary school children of rural, communities at risk in Obudu Local Government Area (LGA), Cross River State, Nigeria. It is hoped that the result from this study will add to the existing baseline data on the endemicity of this disease in the country.
2. Methods
2.1. Study Area
This cross-sectional study was carried out in seven purposively selected communities’ in Obudu LGA. Obudu LGA is one out of the 18 LGAs of Cross River State, Nigeria with a population of 215,800 people in 2016. In each of the selected community, a simple random sampling was used to select the school using the lottery method. The communities are; Udigie (Lat. 6.6667°N, Long. 9.1679°E); Utugwang (Lat.5.6208°N, Long. 9.0336°E); Ibong (Lat. 6.5794°N, Long. 9.1273°E); Ukwortong (Lat. 6.5942°N, Long. 9.0721°E); Betukwel (Lat. 6.6054°N, Long. 9.1060°E); Ugboro (Lat. 6.6621°N, Long. 8.8419°E); and Ohong (Lat. 6.5963°N, Long. 9.1172°E). Cross River state is situated within the tropical rainforest belt of Nigeria. It lies within latitudes 4.4500°N to 5.5333°N and longitude 7.8333°E and 9.4666°E. The coastal area has an annual rainfall of about 350 mm while rainfall in the hinterland is between 120 and 200 mm annually with maximum precipitation occurring from July to September. Most of the communities depend on streams, rivers, rapids and shallow wells as their domestic water supply. These water bodies are frequently visited for water contact activities like bathing, swimming, washing and other domestic activities. Agriculture especially swamp-rice cultivation, cocoyam cultivation and fishing are the major occupations of the inhabitants of these communities.
2.2. Study Design and Population
A school based cross-sectional study was conducted between June to December 2016. School- aged children aged 4-14 years were enrolled from 7 primary schools in each of the seven communities. Participants were selected by first stratifying the children according to the different classes (1-6) and then randomly selecting equal proportion of children in the different grades. This was done for all the seven schools.
2.3. Exclusion Criteria
Primary school children given chemotherapy for schistosomiasis during the national deworming program by WHO through the state ministry of health three weeks prior to and during the data collection at home were excluded during the study. The deworming status was verified while seeking their consent to participate in the study.
2.4. Sample Size Determination
This was estimated using the sample size formula17 as calculated below:
Z = 1.96 (95%)
P = prevalence of urogenital schistosomiasis = 50%
e = error rate 0.05 (5%)
n ~ = 384 + 20% non-respondent value = 384 + 77 = 461.
The minimum sample size is 461 pupils.
A total of 1113 individuals, comprising of 587 males and 526 females were selected randomly from the surveyed schools.
2.5. Ethical Consideration
This study was performed under a protocol that was reviewed and approved by the Research Ethics Committee of Cross River State Ministry of Health (CRSMoH), Calabar. Ethical approval was also obtained from the Local Government Education Authority Consent was verbally obtained from parents and Head teachers of children of the various schools. The village heads and opinion leaders were briefed on the objectives and purpose of the study. The respondents were interviewed in their classrooms with the assistance of their teachers.
2.6. Sample Collection
Each consenting child was provided with a 50 ml capacity autoclaved wide-mouthed screw capped container for collection of a mid-day urine sample. Samples were obtained between 10.00 hours and 14.00 hours, when egg excretion is usually maximal.10 Samples with visible hematuria were noted. The specimens were approximately labelled with identification numbers and placed in cold box with 16 packs immediately after collection. They were processed 1-2 hours from collection. In situations where delay in transportation of specimen to laboratory was inevitable, 0.2 ml of 37% formalin was added to urine sample as a preservative.
2.7. Parasitological Examination
Sedimentation quantitative technique was employed for the detection of S. haematobium eggs in the urine samples as previously described.18 Briefly, 10ml of each thoroughly mixed urine sample was put in a centrifuge tube. The centrifuge was spun for 5 minutes at 1500 rpm. The supernatant was decanted leaving about 0.5ml of the fluid with the sediment at the bottom of the tube undisturbed. The remaining fluid and sediment were mixed, then a drop of the mixture was transferred to a microscope slide and covered with a cover slip. The slide was meticulously examined for S. haematobium using x10 objectives. The eggs seen were counted and the intensity of infection per 10ml of urine accordingly determined. The intensity of S. haematobium was classified as light infection: 1-49 egg/10ml of urine; and heavy infection: ≥50 egg/10ml of urine.19
2.8. Examination of Urine for Hematuria and Proteinuria
Within 2 hours of urine sample collection, hematuria and proteinuria were detected in the field using dipsticks (Medi-Test Combi-9 manufactured by Machery-Hagel Duren, Germany). The reagent end of the test strip was dipped into fresh, well-mixed uncentrifuged urine for 40 seconds. Upon removal, the test area was compared with a standard color as described by the manufacturer.10
2.9. Statistical Analysis
Data obtained were entered into Microsoft Excel for Windows, version 2013 (Microsoft Corporation, Redmond, Washington, USA). Descriptive statistics and chi-square tests were performed on data at 95% Confidence Interval (C.I.) and Level of significance (P) set at p≤0.05 using the Statistical Package for Social Sciences (SPSS) for Windows, version 20.0 (SPSS Inc. Chicago, IL, USA).
3. Results
3.1. Demographic Characteristics
A total of 1,113 school children were examined for urogenital schistosomiasis comprising of 587 males (52.7%) and 526 females (47.3%). The age group of 10-14 years were the highest respondents with 830 (74.6%) children followed by 5-9 year-olds with 269 (24.6%) (Table 1).
| Characters | Total (%) |
|---|---|
| Sex | |
| Male | 587 (52.7) |
| Female | 526 (47.3) |
| Age group (Years) | |
| 0 – 4 | 8 (0.7) |
| 5 – 9 | 269 (24.2) |
| 10 – 14 | 830 (74.6) |
| 15 – 19 | 6 (0.5) |
| Communities/primary school | |
| Lishegie Kushu Primary School, Udigie | 150 (13.5) |
| Universal Primary School, Utugwang | 152 (13.7) |
| Saint Pius Primary School, Ibong | 166 (14.9) |
| Saint John Primary School, Ukwortong | 168 (15.1) |
| Saint Joseph Primary School, Betukwel | 159 (14.3) |
| Community Primary Sch.ool Ugboro | 167 (15.0) |
| Bediagin Primary School, Ohong | 151 (13.6) |
| Total | 1113 |
3.2. Prevalence of Urogenital Schistosomiasis
Among the 1,113 school children examined, 153 were observed shedding eggs of S. haematobium in their urine giving an overall prevalence of 13.7% (95% C.I. = 6.207 – 21.193 %). Prevalence in schools ranged from 7.8% to 28.9% and 42.9% (3/7) of the schools had infection prevalence of >10%. Significant difference (p<0.001) was observed in the prevalence of the parasites among the selected schools (Table 2). Males (86 (14.7%) (95% C.I. = 6.871 – 22.329%): were more infected than females (67 (12.7%) (95% C.I. = 4.442 – 20.615%)). There was no significant difference (p=0.355) in the prevalence between male and female pupils (Table 2).
| Schools | Male | Female | Total | |||
|---|---|---|---|---|---|---|
| Number Examined | Number Infected (%) | Number Examined | Number Infected (%) | Number Examined | Number Infected (%) | |
| Lishegie Kushu Primary School, Udigie | 82 | 8 (9.8) | 68 | 4 (5.9) | 150 | 12 (8.0) |
| Universal Primary School, Utugwang | 84 | 9 (10.7) | 68 | 4 (5.9) | 152 | 13 (8.6) |
| Saint Pius Primary School, Ibong | 85 | 19 (22.4) | 81 | 15 (18.5) | 166 | 34 (20.5) |
| Saint John Primary School, Ukwortong | 83 | 4 (4.8) | 85 | 11 (12.9) | 168 | 15 (8.9) |
| Saint Joseph Primary School, Betukwel | 84 | 24 (28.6) | 75 | 22 (29.3) | 159 | 46 (28.9) |
| Community Primary School Ugboro | 83 | 8 (9.6) | 84 | 5 (6.0) | 167 | 13 (7.8) |
| Bediagin Primary School, Ohong | 86 | 14 (16.3) | 65 | 6 (9.2) | 151 | 20 (13.2) |
| Total | 587 | 86 (14.7) | 526 | 67 (12.7) | 1113 | 153 (13.7) |
| χ2 | 27.928 | 30.971 | 53.233 | |||
| Df | 6 | 6 | 6 | |||
| p value | <0.001* | <0.001* | <0.001* | |||
| 95% C.I. | 6.871 – 22.329 | 4.442 – 20.615 | 6.207 – 21.193 | |||
Children age 5 to 9 years old (46 pupils or 17.1%) had the highest prevalence compared to those in the age groups of 15-19 years (16.7%), 10- 14 years (12.7%) and 0-4 years (12.5%) (Fig. 1). There was no significant difference in prevalence among the age groups (χ2 = 3.446, df = 3, p=0.328) (Table 3).
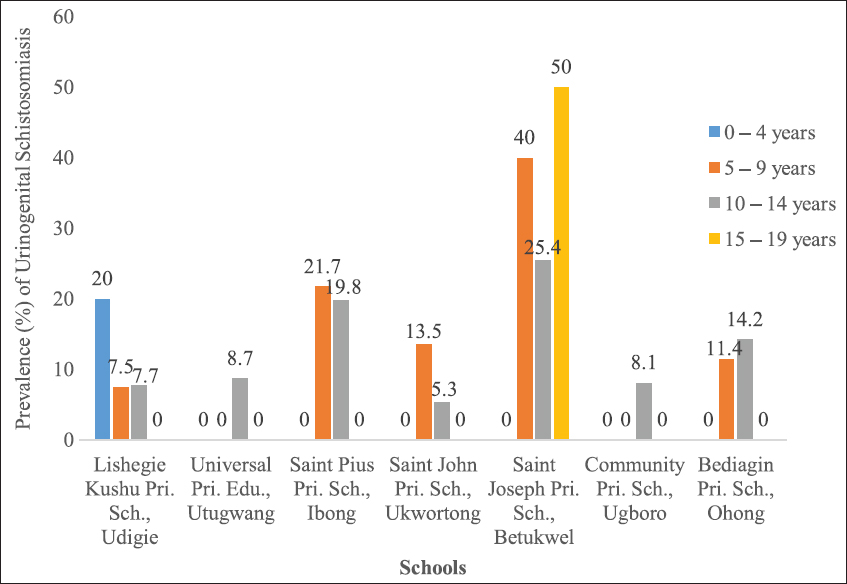
- Prevalence of Urogenital Schistosomiasis in Relation to Age and School in the Study Area
| Age group (Years) | Number examined | Number infected (%) | Number with proteinuria (%) | Number with hematuria (%) |
|---|---|---|---|---|
| 0 – 4 | 8 | 1 (12.5) | 0 (0.0) | 1 (12.5) |
| 5 – 9 | 269 | 46 (17.1) | 53 (19.7) | 46 (17.1) |
| 10 – 14 | 830 | 105 (12.7) | 117 (14.1) | 104 (12.5) |
| 15 – 19 | 6 | 1 (16.7) | 2 (33.3) | 1 (16.7) |
| Total | 1113 | 153 (13.7) | 172 (15.5) | 153 (13.7) |
| χ2 | 3.446 | 7.818 | 3.654 | |
| Df | 3 | 3 | 3 | |
| p value | 0.328ns | 0.050* | 0.301ns | |
| 95% C.I. | 10.789 – 18.711 | 5.162 – 38.712 | 10.649 – 18.751 | |
3.3. Prevalence of Hematuria and Proteinuria
Hematuria is the presence of blood in urine while proteinuria is the presence of protein in urine. The total prevalence of hematuria was 152 (13.7%) (95% C.I. = 10.649 – 18.751). The 5-9 years age group had the highest hematuria rate of 46 (17.1%) (Fig. 2). The prevalence of proteinuria was 172 (15.5%) (95% C.I. = 5.102 – 38.712.), with the 15-19 age group having the highest prevalence of 2 (33.3%) (Fig. 3). Proteinuria was not observed in the age group of 0-4 years, significant difference (χ2 = 7.818, df = 3, p=0.050) was observed in the prevalence of proteinuria among the age groups (Table 3).
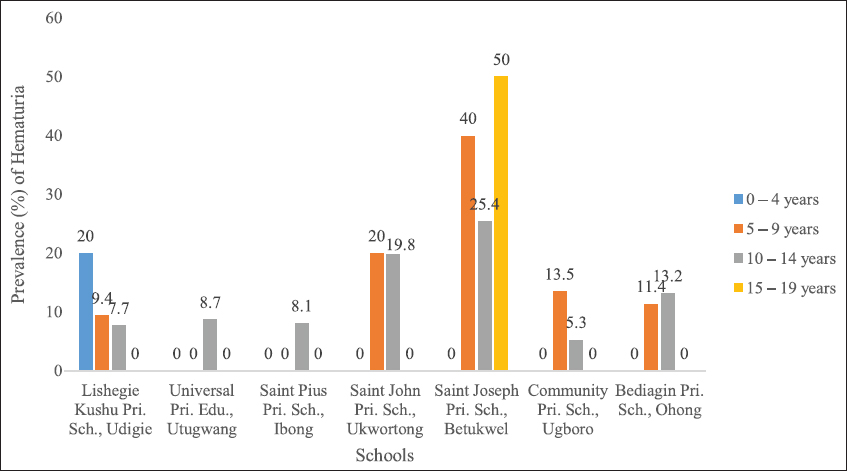
- Prevalence of Hematuria in Relation to Age and School in the Study Area
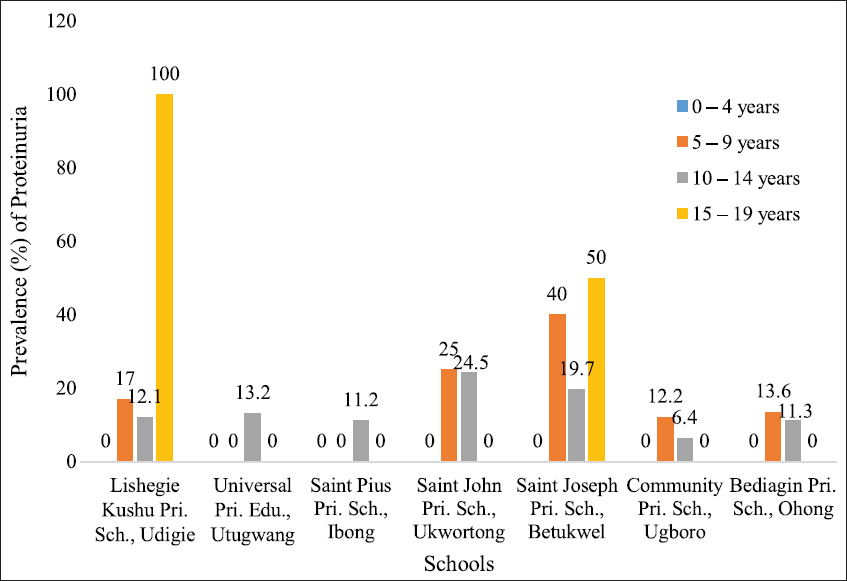
- Prevalence of Proteinuria in Relation to Age and School in the Study Area
3.4. Mean Intensity
Mean intensity represents the arithmetic mean of the number of individual S. haematobium parasites per infected host in a sample. The overall ova intensity (eggs/10ml of urine) among the infected children was 13.30 eggs/10ml urine (range 2.0 eggs/10ml urine to 63 eggs/10ml urine). Females had a higher intensity of 13.69 eggs/10ml urine than males of 12.91 eggs/10ml urine (pp=0.236). Community-level intensity varied among schools from 10.0 eggs/10ml urine in Ibong to 26.2 eggs/10ml urine in Ohong, while the age group 15-19 years had the highest intensity (34.0 eggs/10ml of urine) when compared to other age groups (Table 4).
| Schools | Geometric mean intensity | Total | |||
|---|---|---|---|---|---|
| 0 – 4 years | 5 – 9 years | 10 – 14 years | 15 – 19 years | ||
| Lishegie Kushu Primary School, Udigie | 25.0 | 11.6 | 12.9 | - | 13.2 |
| Universal Primary School, Utugwang | - | - | 10.6 | - | 10.6 |
| Saint Pius Primary School, Ibong | - | 9.62 | 10.24 | - | 10.0 |
| Saint John Primary School, Ukwortong | - | 20.9 | 31.6 | - | 24.0 |
| Saint Joseph Primary School, Betukwel | - | 16.0 | 10.3 | 34.0 | 12.11 |
| Community Primary School Ugboro | - | - | 18.4 | - | 8.4 |
| Bediagin Primary School, Ohong | - | 16.2 | 30.7 | - | 26.2 |
| Total | 25.0 | 14.3 | 12.6 | 34.0 | 13.3 |
Comparison between male and female: χ2 = 0.856, df = 1, p Value = 0.355
4. Discussion
This study has reconfirmed the endemicity of urinary schistosomiasis in Obudu, Cross River State, Nigeria. Also, the study revealed decreased prevalence from 91.0% previously in Obudu15 to 13.7% and geometric mean intensity of 86.84 eggs/10ml to 13.3 eggs/10ml of urine. This study provides an updated information on the decreased burden of urinary schistosomiasis in Obudu communities, Southern Nigeria.
Understanding the geographical distribution of a disease is fundamental prior to initiation of control program based on mass drug distribution. This is to determine where to target mass treatment. The overall prevalence of 13.7% reported in this study is similar to 19.8% and 10.2% reported other parts of Cross River State.10,20 A study in Malawi21 obtained a similar prevalence of 10.4% among school children. However, higher prevalence rates of 32%, 40.1%, and 41.1% were obtained by prior studies among school children.22-24 According to WHO guidelines on preventive chemotherapy in human helminthiasis, school children living in communities where the prevalence of infection with the parasites lies between 10% and 50% require mass drug administration with praziquantel every two years to control schistosomiasis morbidity.25 Prevalence was observed to vary between the schools in different communities (7.8% to 28.9%), demonstrating the focal distribution characteristic of schistosomiasis. The socioeconomic status and the local environmental conditions of the communities where the schools are located may be responsible for these variations. In addition, the different degrees of exposures of the children to infested bodies of water might also have accounted for the variation in prevalence. In Nigeria, rural communities’ access to potable water is limited or non-existent. Consequently, the inhabitants of these communities depend on natural bodies of water such as lakes, streams, ponds and rivers for their daily domestic chores. It is plausible that these water bodies may have been infested with schistosome parasites thereby serving as veritable source of infection.
A higher prevalence of infection was observed among males than females with no significant difference. This is indicative that both sexes are equally exposed to infection through risk factors such as swimming, playing, washing and fetching water in infested bodies. This finding is consistent with prior studies.10,26-28 Furthermore, the study observed that females were not restricted in carrying out activities that may expose them to infection based either on cultural or religious grounds.
The age-related prevalence may be attributed to the frequency and duration of contact with the water and the nature of the water-contact activities at the index site.29 In this study, the high prevalence observed among the 5-9 year-old age group may be due to the adventurous tendencies of this group that expose them to various activities that serve as risk factors for S. haematobium infection. This finding is consistent with documented reports.22,24,30 This, however, contrasts with other conducted elsewhere31-32 which reported a higher prevalence in among the age group 11 – 13 years. Our study showed that there as an increasing trend of infection among children from 5 years to 14 years with a decline after 15 years. This could be attributed to the fact that as the children grow older, they become more aware and begin to follow basic rules of hygiene limiting their contact with infested water bodies.24
This study showed lower mean intensity of urogenital schistosomiasis (13.3 eggs/10 ml of urine) when compared to 149 eggs/10ml urine reported by Babatunde et al.7 Our finding is consistent with 14.9 eggs/10ml documented in similar studies.33,34 The difference in intensity of infection could be associated with differences in seasonality in transmission and types of water contact among study participants.35,36
Proteinuria and hematuria often associated with schistosomiasis have often been regarded as important markers for diagnosing the disease.37,38 The prevalence rates of 13.7% and 15.5% for hematuria and proteinuria, respectively, in the study schools were quite significant; these rates may potentially change over time with their attendant pathological damages, if not treated early.
Poverty, ignorance, poor living conditions, inadequate sanitation and water supplies as well as deplorable personal and environmental hygiene characteristics of many rural communities in Nigeria are important factors that contribute to increased transmission of schistosomiasis.39 These factors may singly or collectively contributed to the moderate prevalence observed in this study.
Although urogenital schistosomiasis is perceived by the residents in our study communities as a public health problem, knowledge about the parasite causing the disease and the vector is poor. Members of the communities were aware of the fact that some of their children pass bloody urine referred to as “betiela anu” or “giabetie la anu” the local name for urogenital schistosomiasis. They were willing to support and participate in any community-based control program.
4.1. Limitations
This study has some limitations. The geographic distribution of schistosomiasis species is closely dependent on the presence of appropriate freshwater snails (Bulinus and Biomphalaria) that serve as obligatory molluscan host. In this study a detailed malacological studies of the community streams was not carried out. However, on-the-spot check of the streams revealed the presence of Bulinus snail vectors of Schistosoma haematobium. Additionally, cases of high-risk infection were not recorded, however, those of moderate to low-risk infection were quite high and could transform to high-risk if they remain untreated. Our study results should therefore be interpreted within the context of these limitations.
4.2. Recommendations for Further Studies
Given the presence of urogenital schistosomiasis in Obudu LGA, there is need to initiate control programs so as to arrest the progression of the disease to an alarming rate. The national schistosomiasis control program should consider targeted treatment every two years in schools and surrounding communities with prevalence of between 10% but less than 50%. In addition, potable water should be provided in the schools and communities to reduce human-vector contact. Adequate snail vector control program should also be implemented to check intermediate snail host population expansion in the study area.
5. Conclusion and Global Health Implications
This study established the presence of urogenital schistosomiasis in Obudu LGA. It has also enriched the baseline studies of the disease in the state and findings would be relevant for other parts of the country. The state Ministry of Health should consider public health intervention programs aimed at reducing the burden of urogenital schistosomiasis in these communities as well as the entire state.
Acknowledgements:
We gratefully acknowledge the Chief Medical Director, Cross River State Ministry of Health (CRSMoH), Calabar and the Education Secretary, Obudu Local Government Education Authority for the permission to carry out the study in the state. The Village Heads of each of the community are appreciated for their cooperation. Tremendous assistance was received from the Head Teacher, Teachers and Students of the respective Schools.
Compliance with Ethical Standards
Conflicts of Interest: The authors declare that they have no competing interest.
Funding/Support: There was no funding for this study.
Ethics Approval: This study was performed under a protocol that was reviewed and approved by the Research Ethics Committee of Cross River State Ministry of Health (CRSMoH), Calabar.
Disclaimer: None
References
- Examining the Relationship between Urogenital Schistosomiasis and HIV Infection. PLOS Negl Trop Dis. 2011;5(12):e1396. https://doi.org/10.1371/journal.pntd.0001396
- [Google Scholar]
- Schistosomiasis - Biology. https://www.cdc.gov/parasites/schistosomiasis/index.html
- Quantification of clinical morbidity associated with schistosome infection in sub-Saharan Africa. Acta Trop. 2003;86(2-3):125-139. https://doi.org/10.1016/s0001-706x(03)00029-9
- [Google Scholar]
- Neglected tropical diseases in sub-Saharan Africa:review of their prevalence, distribution and disease burden. PLOS Negl Trop Dis. 2009;3:e412. https://doi.org/10.1371/journal.pntd.0000412
- [Google Scholar]
- Nigeria. ''Ground Zero''for the High Prevalence Neglected Tropical Diseases. PLOS Negl Trop Dis. 2012;6(7):e1600. https://doi.org/10.1371/journal.pntd.0001600
- [Google Scholar]
- Neglected Tropical Diseases in Sub-Saharan Africa:Review of Their Prevalence, Distribution, and Disease Burden. PLOS Negl Trop Dis. 2009;3(8):e412. https://doi.org/10.1371/journal.pntd.0000412
- [Google Scholar]
- The burden of neglected tropical diseases in Ethiopia, and opportunities for integrated control and elimination. Parasit Vectors. 2012;5:240. https://doi.org/10.1186/1756-3305-5-240
- [Google Scholar]
- Urinary schistosomiasis among pre-school and school aged children in two peri-urban communities in Southwest Nigeria. J Parasitol Vector Biol. 2013;5(7):96-101. https://doi.org/10.5897/JPVB2013.0113
- [Google Scholar]
- Genitourinary schistosomiasis among pre-primary schoolchildren in rural community within the Cross River Basin, Nigeria. J Helminthol. 2007;81:393-397. https://doi.org/10.1017/S0022149X07853521
- [Google Scholar]
- Factors associated with urinary schistosomiasis in two peri-urban communities in south-western Nigeria. Ann Trop Med Parasitol. 2010;104(5):409-419. https://doi.org/10.1179/136485910X12743554760469
- [Google Scholar]
- Soil transmitted helminth infections and schistosomiasis in school age children in sub-Saharan Africa. Efficacy of chemotherapeutic intervention since World Health Assembly Resolution 2001. Tanzan J Health Res. 2010;12(1):1-15. https://doi.org/10.4314/thrb.v12i1.56366
- [Google Scholar]
- Schistosomiasis in Cross River State, Nigeria. Prevalence and intensity of infection in Adim –Akamkpa Local Government Area. J Hyg Epidemiol Microbiol Immunol. 1991;35:141-147.
- [Google Scholar]
- Efficacy of a combination of praziquantel and artesunate in the treatment of urinary schistosomiasis in Nigeria. Trans R Soc Trop Med Hyg. 2009;103(1):38-44. https://doi.org/10.1016/j.trstmh.2008.08.002
- [Google Scholar]
- Distributors of urinary schistosomiasis among high school students in Otukwang, Obudu, Cross River State of Nigeria. Glob J Med Sci. 2003;2:19-22. https://doi.org/10.4314/gjms.v2i1.10090
- [Google Scholar]
- The Prevalence of Urinary Schistosomiasis among School Children in Nkarasi and Edor Communities in Ikom Local Government Area of Cross River State, Nigeria. Pyrex J Med Med Sci. 2017;4(1):1-4.
- [Google Scholar]
- Diagnosis and management of schistosomiasis. BMJ. 2011;342:D22651. https://doi.org/10.1136/bmj.d2651
- [Google Scholar]
- Parasitological examinations:District Laboratory Practices in Tropical Countries, Part 2. Cambridge: Cambridge University Press, UK; 2010.
- Spatial distribution of urinary schistosomiasis in Cross River State, Nigeria using geographical information system and school-based questionnaire. Pak J Biol Sci. 2013;16(20):1166-1172. https://doi.org/10.3923/pjbs.2013.1166.1172
- [Google Scholar]
- Prevalence, distribution and risk factors of Schistosoma haematobium infection among school children in Blantyre, Malawi. PLOS Negl Trop Dis. 2009;3:361. https://doi.org/10.1371/journal.pntd.0000361
- [Google Scholar]
- Co-infection with Schistosoma haematobium and soil transmitted helminths among school-aged children in Saki Oyo state Nigeria. J Public Health Epidemiol. 2014;6(12):417-423. https://doi.org/10.5897/JPHE2014.0664
- [Google Scholar]
- Urogenital schistosomiasis and soil transmitted helminthiasis STH) in Cameroon:An epidemiological update at Barombi Mbo Barombi Kotto crater Lakes assessing prospects for intensified control intervention. Infect Dis Poverty. 2017;6:49. https://doi.org/10.1186/s40249-017-0264-8
- [Google Scholar]
- Prevalence and risk factors asssociated with urogenital schistosomiasis among primary school children in Barage, Magba sub division of Cameroon. BMC Public Health. 2017;17:618.
- [Google Scholar]
- Schistosomiasis and soil-transmitted parasite infections:Preliminary estimates of the number of children treated with Albendazole or Mebendazole. Published 2006 https://www.who.int/schistosomiasis/resources/who_wer8116/en/
- Factors affecting infection or reinfection with Schistosoma haematobium in coastal Kenya:survival analysis during a nine-year, school-based treatment program. Am J Trop Med Hyg. 2006;75(1):83-92.
- [Google Scholar]
- Urinary Schistosomiasis:Water contact frequency and infectivity among secondary school students in Ibadan, Nigeria. Nigerian J Parasitol. 2011;32(1):129-134.
- [Google Scholar]
- Micro-epidemiology of urinary schistosomiasis in Zanzibar:local risk factors associated with distribution of infections among school children and relevance for control. Acta Trop. 2008;105:45-84. https://doi.org/10.1016/j.actatropica.2007.09.006
- [Google Scholar]
- Human community ecology of urinary schistosomiasis in relation to snail vector bionomics in the Igwun River Basin of Nigeria. Trop Med Parasitol. 1990;141(2):131-135.
- [Google Scholar]
- The Prevalence of schistosoma haematobium among Primary school pupils in Mayo Belwa Local Government Area of Adamawa Stale. Nigeria J Parasitol. 2000;21:15-20.
- [Google Scholar]
- Prevalence of urinary schistosomiasis among school children in Ukwelo-Obudu and Abini communities in Cross River State, Nigeria. Port Harcourt Med J. 2009;3(3) http://dx.doi.org/10.4314/phmedj.v3i3.45251
- [Google Scholar]
- Endemicity of schistosomiasis in some parts of Anambra State, Nigeria. J Med Lab Diagn. 2013;4(5):54-61. https://doi.org/10.5897/JMLD2013.0072
- [Google Scholar]
- Profile of an epidemiological study of urinary schistosomiasis in two local government areas of Benue state, Nigeria. Int J Med Biomed Res. 2012;1(1):39-48.
- [Google Scholar]
- Impact of Annual Praziquantel Treatment on Urogenital Schistosomiasis in a Seasonal Transmission Focus in Central Senegal. PLOS Negl Trop Dis. 2016;10(3):e0004557. https://doi.org/10.1371/journal.pntd.0004557
- [Google Scholar]
- Age and gender effects in self-reported urinary schistosomiasis in Tanzania. Trop Med Int Health. 2008;13(5):713-721. https://doi.org/10.1111/j.1365-3156.2008.02048.x
- [Google Scholar]
- Prevalence and intensity of urinary schistosomiasis among school children in the district of Njakhar, region of fatick, Senegal. Parasit Vector. 2014;7:5. https://dx.doi.org/10.1186%2F1756-3305-7-5
- [Google Scholar]
- The performance of hematuria reagent strips for the rapid mapping of urinary schistosomiasis:field experience from Southern Sudan. Trop Med Int Health. 2009;14(12):1484-1487. https://doi.org/10.1111/j.1365-3156.2009.02407.x
- [Google Scholar]
- Diagnostic performance of screening methods for urogenital schistosomiasis in a school-based control programme in Ibadan, Nigeria. J Commun Med Primary Health Care. 2005;17:24-27.
- [Google Scholar]
- Report of the WHO Informal Consultation on Schistosomiasis Control Geneva. Published 1998 https://www.who.int/schistosomiasis/resources/who_cds_cpc_sip_99.2/en/





