Translate this page into:
Social Determinants of Health in the United States: Addressing Major Health Inequality Trends for the Nation, 1935-2016
*Corresponding author email: gsingh@hrsa.gov
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Objectives:
This study describes key population health concepts and examines major empirical trends in US health and healthcare inequalities from 1935 to 2016 according to important social determinants such as race/ethnicity, education, income, poverty, area deprivation, unemployment, housing, rural-urban residence, and geographic location.
Methods:
Long-term trend data from the National Vital Statistics System, National Health Interview Survey, National Survey of Children’s Health, American Community Survey, and Behavioral Risk Factor Surveillance System were used to examine racial/ethnic, socioeconomic, rural-urban, and geographic inequalities in health and health care. Life tables, age-adjusted rates, prevalence, and risk ratios were used to examine health differentials, which were tested for statistical significance at the 0.05 level.
Results:
Life expectancy of Americans increased from 69.7 years in 1950 to 78.8 years in 2015. However, despite the overall improvement, substantial gender and racial/ethnic disparities remained. In 2015, life expectancy was highest for Asian/Pacific Islanders (87.7 years) and lowest for African-Americans (75.7 years). Life expectancy was lower in rural areas and varied from 74.5 years for men in rural areas to 82.4 years for women in large metro areas, with rural-urban disparities increasing during the 1990-2014 time period. Infant mortality rates declined dramatically during the past eight decades. However, racial disparities widened over time; in 2015, black infants had 2.3 times higher mortality than white infants (11.4 vs. 4.9 per 1,000 live births). Infant and child mortality was markedly higher in rural areas and poor communities. Black infants and children in poor, rural communities had nearly three times higher mortality rate compared to those in affluent, rural areas. Racial/ethnic, socioeconomic, and geographic disparities were particularly marked in mortality and/or morbidity from cardiovascular disease, cancer, diabetes, COPD, HIV/AIDS, homicide, psychological distress, hypertension, smoking, obesity, and access to quality health care.
Conclusions and Global Health Implications:
Despite the overall health improvement, significant social disparities remain in a number of health indicators, most notably in life expectancy and infant mortality. Marked disparities in various health outcomes indicate the underlying significance of social determinants in disease prevention and health promotion and necessitate systematic and continued monitoring of health inequalities according to social factors. A multi-sectoral approach is needed to tackle persistent and widening health inequalities among Americans.
Keywords
Social Determinants
Race/Ethnicity
Socioeconomic Status
Health Disparities
Life Expectancy
Leading Causes Of Death
Chronic Disease
Health Care
1. Introduction
Achieving health equity involves examining the existence of and reduction of inequities in health, health care access, and use of quality health services according to major social determinants of health over time. The US Department of Health and Human Services (HHS) has a long history of examining social inequities in health, disease, and mortality and developing programs to reduce health inequities among populations that experience increased risk of poor health based on race/ethnicity, gender, socioeconomic status (SES), rural/urban residence, and housing status.[1-4] One of the earliest studies undertaken more than a century ago examined the impact of poverty, housing condition, sanitation, nutrition, and medical care during pregnancy on infant mortality in the United States.[5] Decades of studies have found marked socioeconomic, racial/ethnic, and occupational disparities in mortality and life expectancy among Americans, identifying population groups that have not fully shared the Nation’s health and longevity gains.[6-8] Described below are some of the key population health concepts that are commonly used in research on social determinants of health and health disparities and defining which is one of the main goals of this study.
1.1. Social determinants of health
Social determinants of health are conditions in the social environment in which people are born, live, learn, work, and play that affect a wide range of health, functioning, and quality-of-life outcomes and risks.[1,9] These social and/or demographic characteristics of individuals, groups, communities, and societies have been shown to have powerful influences on health and well-being at the individual and population levels. Examples of individual or group-level social determinants include gender, race/ethnicity, SES, social class, education, income, occupation, employment status, housing tenure, immigrant status, language use, disability status, and social capital. Social determinants at the population level include socioeconomic deprivation, poverty rate, income inequality, educational opportunity, labor market structure, affordable housing, access to healthy foods/good nutrition, provision of health services, access to essential goods and services, transportation infrastructure, physical and built environments, racial/ethnic population composition, medically underserved or health professional shortage areas, and spending on public safety, social and welfare services. Social determinants at the population level are considered underlying, upstream, or more fundamental determinants of health and disease and are amenable to change through public policy.[10,11]
1.2. Population health research
Population health research is concerned with the investigation of differences in health status and health determinants among social and demographic groups and geographically-defined populations. This approach involves examining interrelationships between the distribution of social, economic, demographic, cultural, political, and other valued societal resources and health at the community level and is aimed at improving the health of the entire population rather than individuals.[11,12] The causes of health inequities at the population level may differ from those at the individual level.[11,12]
1.3. Health equity
Health equity is defined as the absence of disparities or avoidable differences among socioeconomic and demographic groups or geographic areas in health status and health outcomes such as disease, disability, or mortality. Health inequities refer to inequalities that are deemed to be unfair, unjust, avoidable or unnecessary that can be reduced or remedied through policy action.[13,14] The concepts of health inequities and health disparities (broadly defined as systematic differences in health between social groups) are generally similar in that they both involve normative judgements about the nature of social-group differences.[14] In this study, the terms, health inequities, health disparities, and health inequalities are used interchangeably.
1.4. Healthy People Initiative
In 1980, HHS introduced a national initiative in disease prevention and health promotion called Healthy People.[1] This health initiative presents a national strategy for increasing the span of healthy life among Americans, reducing and ultimately eliminating health disparities among Americans, and providing access to preventive health services for all Americans.[1] Since the launching of this national effort, states and other geographic areas, such as counties, cities, metropolitan areas, and rural communities have become increasingly interested in population health monitoring and in providing background data needed to understand a population=s health equity issues.[11] The health initiative sets objectives for each decade. The current initiative, Healthy People 2020, was launched in 2010, while Healthy People 2030 is currently being developed.[1]
Population health monitoring includes documenting health-related data over time for various communities and subgroups of the population. It also involves analyses of health differentials and inequities according to important personal and societal characteristics that are amenable to change through social and public policy interventions. In recent decades, health statistics in the US have become increasingly available according to a wide array of relevant socioeconomic, demographic, behavioral, and health care characteristics. Availability of these data has created opportunities for us to enhance our understanding of the most fundamental reasons for changes in population health or persistent health disparities among various societal groups and geographic areas and to develop and implement effective evidence-based policies.[11]
Remarkable achievements have been made in improving the overall health of the US population during the past several decades, particularly in terms of increasing the life expectancy and reducing overall mortality among Americans.[2,3,15] However, substantial variations in health among various social groups and geographic areas continue to exist, and, in many instances, health disparities appear to be widening.[2,3,16-25] Social factors, whether expressed in terms of education, occupation, income, wealth, social class, ethnicity, family structure, or living arrangements, remain underlying and fundamental determinants of health and disease. While these social characteristics themselves may not be direct determinants of health, they can create conditions or circumstances that give rise to risk factors (e.g., smoking, alcohol and drug use, unhealthy diet, lack of physical activity, obesity, and hypertension) which cause disease, ill health, and death.[11,22] The social determinants involve such resources as “knowledge, money, power, prestige, and social connections that strongly influence people’s ability to avoid risks and to minimize the consequences of disease once it occurs”.[26] Inequities in health are closely linked to social inequities through several intervening mechanisms, including health behaviors, medical care, working conditions, environmental exposure, personality, and early life conditions.[14,27]
1.5. Objectives
In this paper, we analyze major health inequality trends for the United States according to important social determinants such as race/ethnicity, education, income, poverty, area deprivation, unemployment, housing, rural-urban residence, and geographic location. Analysis covers a broad range of areas, including maternal and child health, health care access and quality, HIV/AIDS, mental and behavioral health, chronic disease prevention and health promotion, rural-urban and geographic disparities, with a particular focus on social inequalities in life expectancy, infant mortality, and mortality from leading causes of death.
Emphasizing the role of social determinants of health is important for several reasons.[11,28] First, documenting health disparities between the least and most advantaged social groups can tell us about the extent to which a society’s health can be improved. However, health inequities are not just about addressing differences between the rich and the poor. Rather, the consistently inverse socioeconomic gradients in health found across many industrialized societies indicate that the health deficit of a population is concentrated in the middle classes because of the large numbers of people in those categories.[11,12] To achieve health equity and to maximize health improvement, it therefore makes sense to focus on health differences across the entire social hierarchy or socioeconomic continuum. Second, documenting health inequities according to social factors can help identify social groups who are at greatest risk of poor health and who are therefore in need of social and medical services. Third, considering social factors along with behavioral and health care factors can help us understand the mechanisms through which social factors affect health. A better understanding of the pathways through which social determinants influence health and disease outcomes should help us develop and implement more effective social and public health interventions for population health improvement.[11,12]
2. Methods
Temporal data (1935-2016) from the National Vital Statistics System, National Health Interview Survey (NHIS), National Survey of Children’s Health (NSCH), American Community Survey (ACS), and Behavioral Risk Factor Surveillance System were used to examine racial/ethnic, socioeconomic, rural-urban, and geographic inequalities and trends in health and health care.[2,15,29-34] Life tables, age-adjusted rates, prevalence, and risk ratios were used to examine health differentials, which were tested for statistical significance at the 0.05 level. Specifically, we used county-level 2013 rural-urban continuum codes linked to the national mortality database to analyze rural-urban disparities in mortality and life expectancy over time.[17] All-cause and cause-specific mortality rates were age-adjusted by the direct method using the age composition of the 2000 US population as the standard.[15] For income-specific infant and child mortality analyses, we linked county-level poverty data from the 2000 census and 2010-2014 ACS with county-level mortality statistics for 1999-2001 and 2010-2014, respectively.[32,33] Area-based deprivation indices linked to mortality data were used to derive HIV/AIDS mortality rates and relative risks over time according to levels of socioeconomic deprivation.[19,23] All analyses were conducted using public-use data and were thus exempt from the institutional review board (IRB) approval.
3. Results
3.1. Disparities in social determinants of health
Several of the racial/ethnic minorities in the US have historically been disadvantaged in terms of social and economic attainment. In the US, data on Hispanic origin and race/ethnicity are collected separately in the census and numerous other programs.[3,32] Hispanics can be of any race; however, a majority (65%) of Hispanics identify themselves as whites.[32] To develop a mutually exclusive and exhaustive variable of race/ethnicity, the Hispanic-origin item is often cross-classified with race.[32] About 85% of the total white population is non-Hispanic, while 97% of the black or African American population is non-Hispanic.[32] The 2015 data in Figure 1 indicate two times higher poverty rates among American Indians/Alaska Natives [AIANs] (26.6%), black/African-Americans (25.4%), Hispanics (22.6%), and Native Hawaiians and other Pacific Islanders (18.9%), compared with non-Hispanic whites (10.4%).[32] Unemployment rates are more than two times higher among AIANs and blacks compared to non-Hispanic whites. Hispanics and Native Hawaiians and other Pacific Islanders have 50% higher unemployment rates than non-Hispanic whites. There are substantial disparities in educational attainment; 52.3% of Asian Americans in 2015 had a college degree, compared with 34.2% of non-Hispanic whites, 20.2% of blacks, 14.1% of AIANs, 15.7% of Native Hawaiians and other Pacific Islanders, and 14.8% of Hispanics.[32]

- Poverty, Unemployment, and Health Uninsurance Rates (%) by Race/Ethnicity, United States, 2015
- Source: US Census Bureau. 2015 American Community Survey.
Ethnic-minority groups are also more likely to live in low-income and disadvantaged neighborhoods and communities than their non-Hispanic white counterparts.[23] Geographic patterns in educational attainment indicate that the population in the Southeastern region of the US has had the lowest percentage of adults with a college degree although education levels in all regions have improved over time (Figure 2). The geographic pattern in poverty rates has remained essentially the same over time, with communities in the Southeastern and Southwestern regions experiencing higher poverty rates than those in the other regions of the US (Figure 3). The unemployment map shows wide geographic disparities; many counties in the Southeastern, Southwestern, and Western United States had at least 9% of their workforce unemployed during the 2011-2015 time period (Figure 4). The geographic map of English language proficiency shows many counties in the Western and Southwestern United States with at least 10% of the population speaking English not well or not at all (Figure 5).

- Percentage of Population aged ≥25 Years with a College Degree, United States, 2000 and 2011-2015 (3,143 Counties)
- Source: Data derived from the 2000 Census and 2011-2015 American Community Survey.
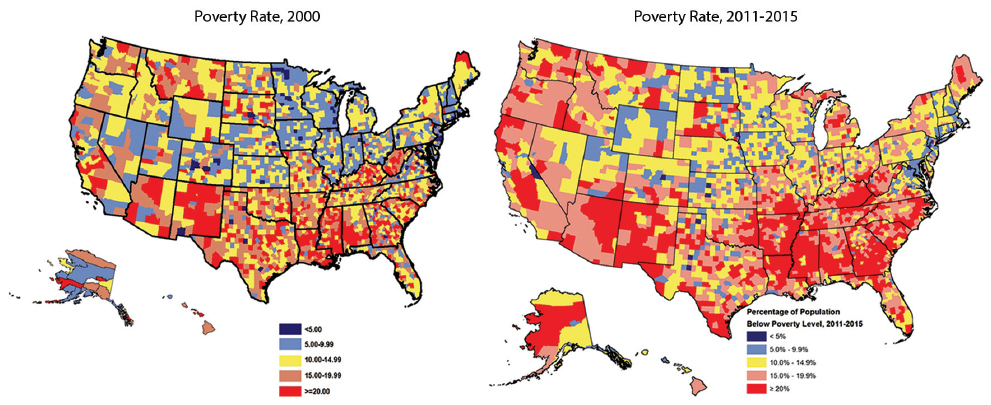
- Percentage of Population Below the Federal Poverty Level, United States, 2000 and 2011-2015 (3,143 Counties)
- Source: Data derived from the 2000 Census and 2011-2015 American Community Survey.
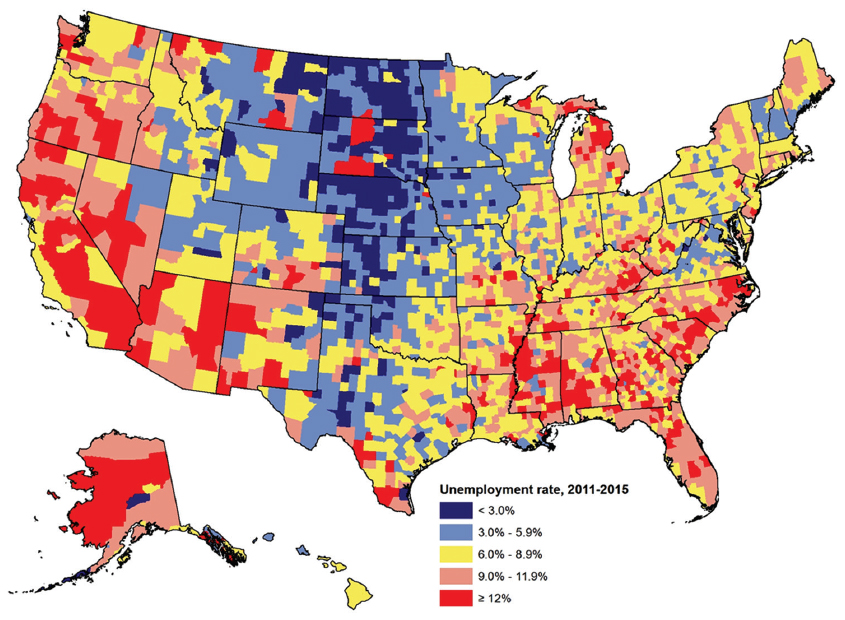
- Unemployment Rate (Percentage of Civilian Labor Force that is Unemployed), United States, 2011-2015 (3,143 Counties)
- Source: Data derived from the 2011-2015 American Community Survey.
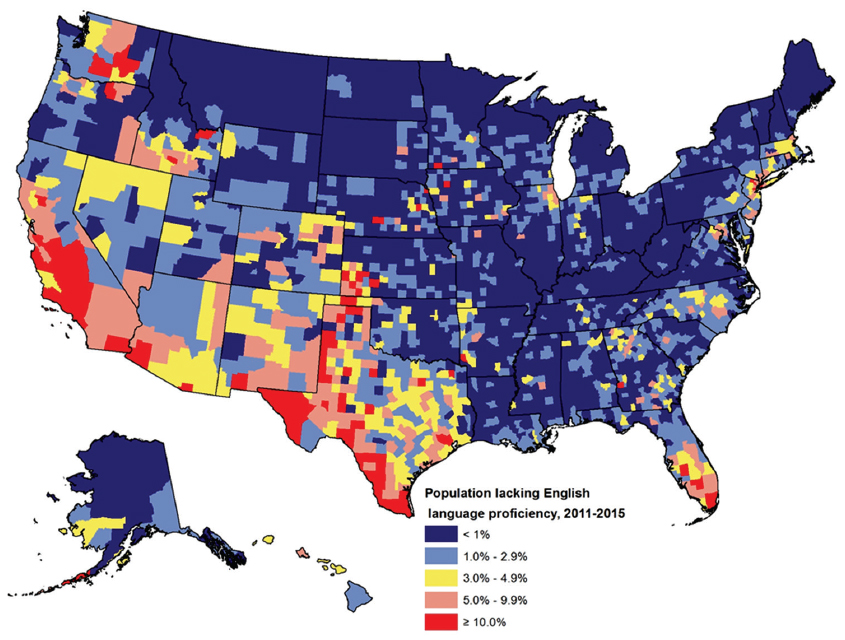
- Population Lacking English Language Proficiency (Percentage of Population Aged 5 Years and Older Speaking English Not Well or Not At All), United States, 2011-2015 (3,143 Counties)
- Source: Data derived from the 2011-2015 American Community Survey.
Ethnic-minority groups are more likely to be without health insurance than non-Hispanic whites. In 2015, 6.3% of non-Hispanic whites lacked health insurance, compared with 11.0% of blacks, 20.7% of AIANs, 19.5% of Hispanics, 7.8% of Asians, and 9.9% of Native Hawaiians and other Pacific Islanders (Figure 1). Access to health insurance also varies by education, income, and employment status. In 2015, 22.8% of adults with less than a high school education lacked health insurance, compared with only 3.9% of adults with a college degree. Nearly 28% of unemployed individuals lacked health insurance, compared with 11% of employed individuals. In 2015, 17.2% of those with income levels below 138% of the poverty threshold were uninsured, compared with 3.3% of those with incomes at or above 400% of the poverty threshold.[32]
3.2. Disparities in life expectancy
Life expectancy at birth has improved substantially during the past six and half decades, increasing from 69.7 years for the total US population in 1950 to 78.8 years in 2015.[15] However, despite the overall improvement, racial and gender disparities in life expectancy persist (Figure 6). In 1950, blacks had a life expectancy of 60.8 years compared with 69.1 years for whites. In 2015, the black and white life expectancies were 76.2 and 79.2 years respectively. In 1950, the life expectancy at birth for white males, white females, black males, and black females was 66.2, 72.2, 59.1, and 62.9 years respectively. In 2015, the corresponding figures for these race-gender groups were 76.4, 81.2, 72.9, and 79.2 years. In 2015, life expectancy at birth was 87.7 years for Asian/Pacific Islanders (APIs), 83.7 years for Hispanics, 82.2 years for AIANs, 78.9 years for non-Hispanic whites, and 75.7 years for non-Hispanic blacks (Figure 7).

- Life Expectancy at Birth (in Years) by Race and Sex, United States, 1950-2015
- Source: CDC/NCHS. National Vital Statistics System.
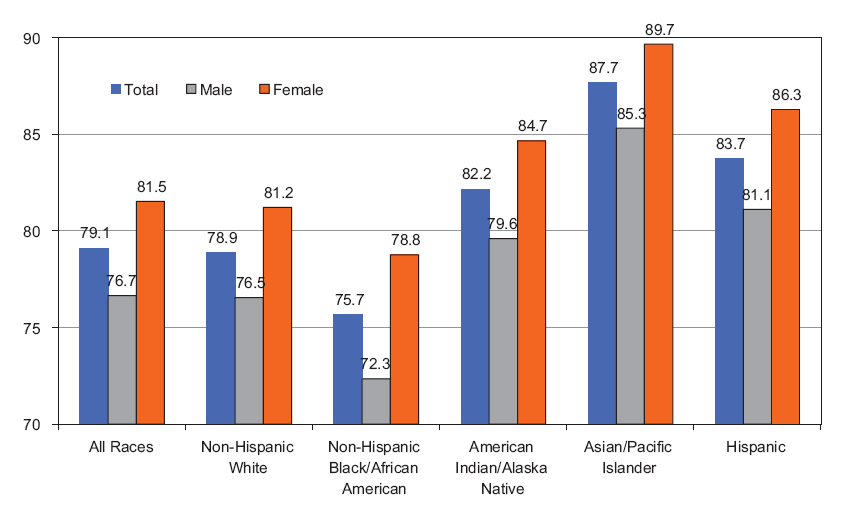
- Life Expectancy at Birth (Years) by Race/Ethnicity and Sex, United States, 2015
- Source: Data dervied from the National Vital Statistics System.
Life expectancy at birth varies by rural-urban residence and is substantially lower in rural areas of the US (Figure 8). For example, during the 2010-2014 time period, the life expectancy of men in rural/non-metro areas and small urban/non-metro towns was 74.5 and 74.8 years respectively, compared with life expectancy of 77.6 years for men in large metro areas. Rural-urban disparities in life expectancy increased during 1990-2014 as increases in life expectancy were smaller in rural/non-metro areas compared to urban/metro areas (Figure 8).
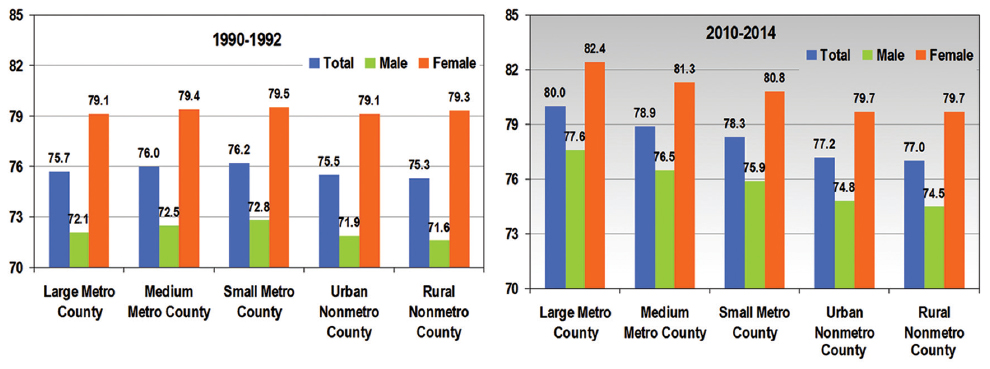
- Life Expectancy at Birth (Years) by Levels of Urbanization, United States, 1990-1992 and 2010-2014
- Source: Singh GK, Siahpush M. American Journal of Preventive Medicine. 2014; 46(2):e19-e29 (updated data). Data derived from the US National Vital Statistics System.
3.3. Disparities in child health
3.3.1. Infant and child mortality
The infant mortality rate in the US has declined dramatically over the past several decades, from a rate of 55.7 per 1,000 live births in 1935 to 5.9 in 2015. The mortality rates have declined impressively over time for both white and black infants. However, the racial disparity has continued to grow in relative terms (Figure 9). In 2015, the mortality rate for black infants was 11.4 per 1,000 live births, 2.3 times higher than the mortality rate of 4.9 for white infants. In 1935, the infant mortality rate for black infants was 81.9 per 1,000 live births, 1.6 times higher than the mortality rate of 51.9 for white infants.

- Infant Mortality Rate by Race, United States, 1935-2015
- Source: Singh GK, van Dyck PC. Infant Mortality in the United States. A 75th Anniversary title V Publication. HRSA. 2010 (updated data) and CDC/NCHS.
Infant and child mortality rates are substantially higher in rural than in urban areas (Figures 10 and 11). Within rural areas, black and AIAN infants have higher infant mortality rates than white infants. Infant and child mortality rates are also higher in communities with higher poverty rates, regardless of rural-urban residence or race/ethnicity. For example, the infant mortality rate for black infants in 2010-2014 was 9.0 per 1,000 live births in rural counties with a poverty rate of ≥20%. This rate was almost three times as high as the black infant mortality rate in rural counties with a poverty rate of <5%.

- Infant Mortality Rate by County-Level Family Poverty Rate, United States, 1999-2001 and 2010-2014
- Source: Data derived from the National Vital Statistics System.
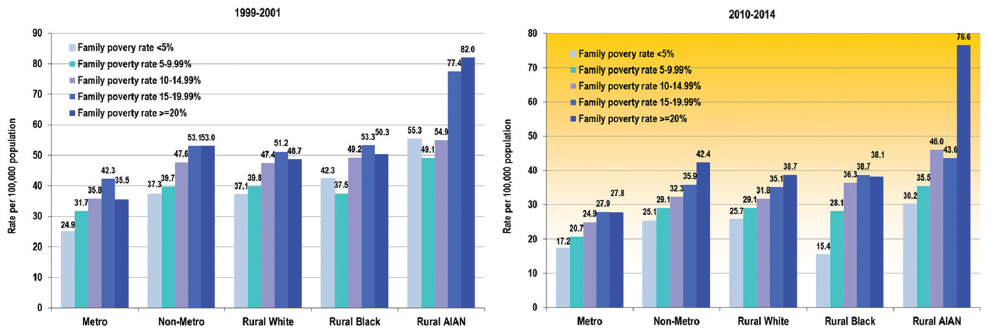
- Child and Adolescent (1-19) Mortality Rates by County-Level Family Poverty Rate, United States, 1999-2001 and 2010-2014
- Source: Data derived from the National Vital Statistics System.
3.3.2. Childhood asthma
Asthma is the most common chronic condition among children in the United States. According to the 2015 NHIS, 9.5 million or 13.0% of US children were reported by their parents to have ever been diagnosed with asthma, with 8.4% of them still having asthma.[30] According to the 2011-2012 NSCH, 8.8% of children were reported to have asthma currently (Table 1).[31] The prevalence of asthma varied by a number of sociodemographic factors, including race/ethnicity, family structure, household language use, education, income/poverty level, housing tenure, and place of residence. Non-Hispanic black children had two times higher asthma prevalence than non-Hispanic white children. Children living below the poverty line were 56% more likely to have asthma than children with family incomes at or above 400% of the poverty threshold. Children living in unsafe neighborhoods or in neighborhoods with poor housing were 32% more likely to be diagnosed with asthma than children in safe neighborhoods or neighborhoods with good housing. Asthma rates varied by state of residence, with children in the South and Northeast regions having higher prevalence than those living in the Western region of the US (Figure 12).
| Characteristic | Prevalence | SE |
|---|---|---|
| United States | 8.78 | 0.20 |
| Child’s age | ||
| 0-5 years | 5.81 | 0.28 |
| 6-11 years | 10.02 | 0.36 |
| 12-17 years | 10.43 | 0.38 |
| Child’s gender | ||
| Male | 9.58 | 0.28 |
| Female | 7.95 | 0.28 |
| Race/ethnicity | ||
| Hispanic | 6.81 | 0.46 |
| Non-Hispanic White | 7.57 | 0.22 |
| Non-Hispanic Black | 16.72 | 0.76 |
| Mixed Race | 13.42 | 1.00 |
| Other | 6.28 | 0.56 |
| Household composition | ||
| Two-parent biological | 6.91 | 0.21 |
| Two-parent stepfamily | 11.29 | 0.77 |
| Single mother | 12.76 | 0.55 |
| Other family type | 12.03 | 0.91 |
| Place of residence | ||
| Metropolitan | 8.70 | 0.22 |
| Non-metropolitan | 9.50 | 0.44 |
| Primary language spoken at home | ||
| English | 9.63 | 0.22 |
| Any other language | 4.20 | 0.45 |
| Household/parental education level | ||
| <12 years | 9.15 | 0.68 |
| 12 years | 10.72 | 0.54 |
| >12 years | 8.29 | 0.22 |
| Household poverty status | ||
| (Ratio of family income to poverty threshold) | ||
| Below 100% | 11.43 | 0.50 |
| 100-199% | 8.76 | 0.47 |
| 200-399% | 8.14 | 0.36 |
| At or above 400% | 7.31 | 0.31 |
| Household employment status | ||
| Employed for ≥ 50 weeks during past year | 8.47 | 0.22 |
| Not employed | 10.76 | 0.54 |
| Housing tenure/home ownership | ||
| Own home | 7.94 | 0.23 |
| Rent/other | 10.27 | 0.37 |
| Neighborhood safety | ||
| Safe | 8.46 | 0.20 |
| Unsafe | 11.15 | 0.72 |
| Neighborhood housing condition | ||
| Poor/dilapidated housing | 11.08 | 0.58 |
| Good | 8.39 | 0.21 |
The Chi-square test for the overall association between each covariate and asthma prevalence was statistically significant at P<0.05 level. SE=standard error.
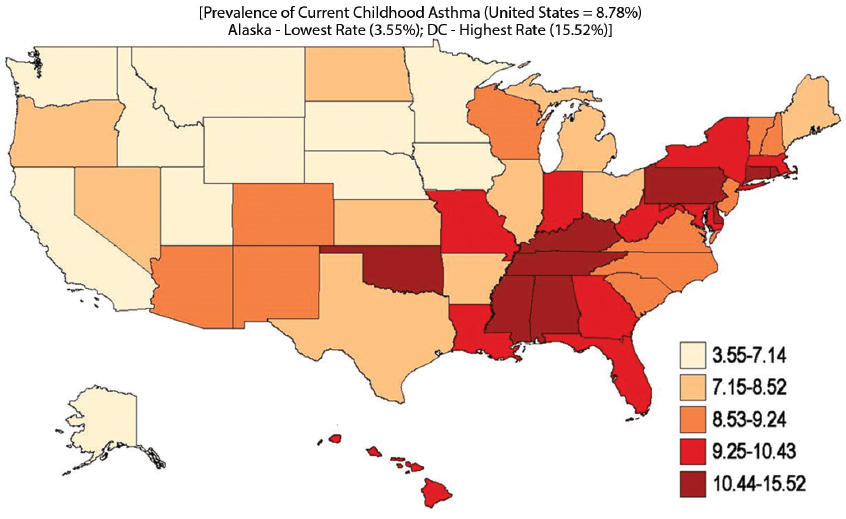
- State Variation in Prevalence of Current Asthma among US Children and Adolescents Aged Under 18 Years, 2011-2012 National Survey of Children’s Health.
3.4. Disparities in mortality from leading causes of death
Heart disease, cancer, chronic obstructive pulmonary disease (COPD), unintentional injuries, stroke, Alzheimer’s disease, diabetes, influenza and pneumonia, kidney disease, and suicide are the 10 leading causes of death and accounted for 74.2% of all deaths in the United States in 2015.[15,29] There are marked gender, racial/ethnic, socioeconomic, and geographic disparities in all-cause mortality and mortality from leading causes of death. Although cardiovascular disease (CVD) (including heart disease and stroke) mortality rates declined for all major racial/ethnic groups over the past several decades, compared to whites in 2015, blacks had 28% higher CVD mortality and APIs, AIANs, and Hispanics had 29-42% lower mortality (Figure 13).[15,19] Geographic differences in all-cause and CVD mortality show higher risks of CVD mortality in the Southeastern region of the US even though mortality rates have declined in all regions and states (Figures 14 and 15).[20]
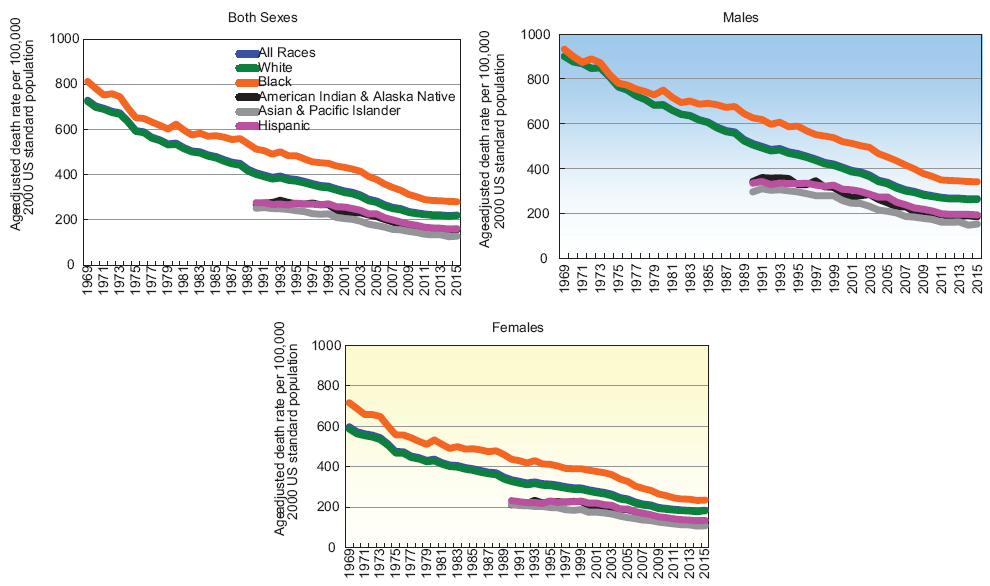
- Trends in CVD Mortality by Race/Ethnicity and Sex, United States, 1969-2015
- Source: Singh GK, Siahpush M, Azuine RE, Williams SD. Widening Socioeconomic and Racial Disparities in Cardiovascular Disease Mortality in the United States, 1969-2013. International Journal of MCH and AIDS. 2015; 3(2)106-118 (updated data).

- Age-Adjusted All-Cause Mortality Rates per 100,000 Population for the United States (3,143 Counties), 1999-2003 and 2011-2015
- Source: Derived from the 1999-2015 National Vital Statistics System.
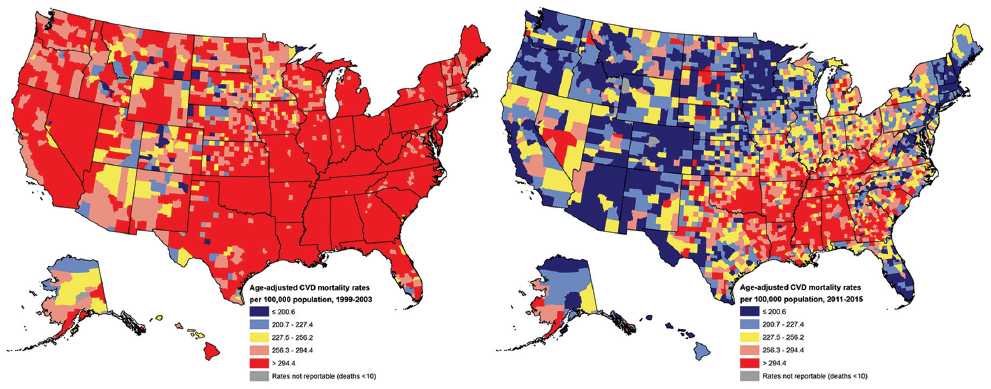
- Age-Adjusted Cardiovascular Disease (CVD) Mortality Rates per 100,000 Population for the United States (3,143 Counties), 1999-2003 and 2011-2015
- Source: Derived from the 1999-2015 National Vital Statistics System.
CVD mortality rates are higher among individuals and areas with lower SES.[19] For example, men and women with low education and incomes have 46-76% higher CVD mortality than their counterparts with high education and income levels. Men in clerical, service, farming, craft, repair, construction, and transport occupations, and manual laborers have 30-58% higher CVD mortality risks than those employed in executive and managerial occupations. Among women, those employed in sales and service occupations, respectively, have 17% and 29% higher CVD mortality risks, and those in transport occupations have 2.6 times higher mortality risks than those in executive and managerial occupations.[19]
Compared to whites, cancer mortality rates in 2014 were 15% higher for blacks but 34% lower for AIANs, 39% lower for APIs, and 32% lower for Hispanics.[15] SES is inversely related to overall cancer mortality as well as mortality from major cancer sites such as lung, colorectal, cervical, stomach, liver, and esophageal cancer.[22] During the 2003-2011 time period, men with less than a high school education had 68% higher cancer mortality than those with a college degree, whereas men below the poverty level had 80% higher cancer mortality than men with incomes ≥600% of the poverty level. Men with less than a high school education and those below the poverty level had 2.6 times higher lung cancer mortality than their more educated and affluent counterparts. Education and income levels were also inversely related to lung cancer mortality among women. Men and women with less than a high school education had, respectively, 42% and 120% higher colorectal cancer mortality risks than those with a college degree. During the 2003-2011 time period, women with less than a high school education and below the poverty level had 6.3 and 4.0 times higher cervical cancer mortality than women with the highest education and income levels, respectively.[22] Compared to white women in 2014, black women had 3.3 times higher cervical cancer mortality and API, AIAN, and Hispanic women had 1.3-1.5 times higher mortality rates.[15] County maps indicate higher risks of all-cancer mortality in the Southeastern region and Eastern half of the US, with mortality rates declining in several regions during 1998-2014 (Figure 16).

- Age-Adjusted All-Cancer Mortality Rates per 100,000 Population for the United States (3,143 Counties), 1998-2002 and 2010-2014
- Source: Derived from the 1998-2014 National Vital Statistics System.
COPD mortality is highest among whites, who have a 4-fold higher mortality risk than APIs. COPD mortality is also substantially lower in blacks, AIANs, and Hispanics compared to whites.[15] Figure 17 indicates higher COPD mortality rates in Appalachia and the Western half of the US, with rates increasing in many counties over time. Compared to whites, diabetes mortality is two times higher among blacks and at least 60% higher among AIANs and Hispanics. Geographic maps indicate substantially higher rates of diabetes mortality in the Southeast, Southwest and Appalachian regions than elsewhere in the US (Figure 18). Blacks experience 2.5 times higher kidney disease mortality than whites. AIANs have higher unintentional injury mortality than whites, who, in turn, have higher mortality rates than blacks, Hispanics, and APIs. County maps indicate higher rates of unintentional injury mortality in the Western and Appalachian counties, with rates increasing over time in several parts of the country (Figure 19). Unintentional injury mortality rates for non-Hispanic whites rose by 39% during 1999-2015, with steep increases in drug overdose deaths contributing greatly to the rising trend. Suicide rates are 2.7 times higher among whites and 2.0 times higher among AIANs compared to blacks. There has been an upward trend in suicide mortality, with rates increasing consistently from 10.5 in 1999 to 13.3 per 100,000 population in 2015.[15,29] Geographic maps show higher suicide mortality rates in many counties of the Western United States, with suicide risks increasing over time in the Western and Appalachian regions (Figure 20).

- Age-Adjusted COPD Mortality Rates per 100,000 Population for the United States (3,143 Counties), 1998-2002 and 2010-2014
- Source: Derived from the 1998-2014 National Vital Statistics System.

- Age-Adjusted Diabetes Mortality Rates per 100,000 Population for the United States (3,143 Counties), 1998-2002 and 2010-2014
- Source: Derived from the 1998-2014 National Vital Statistics System.
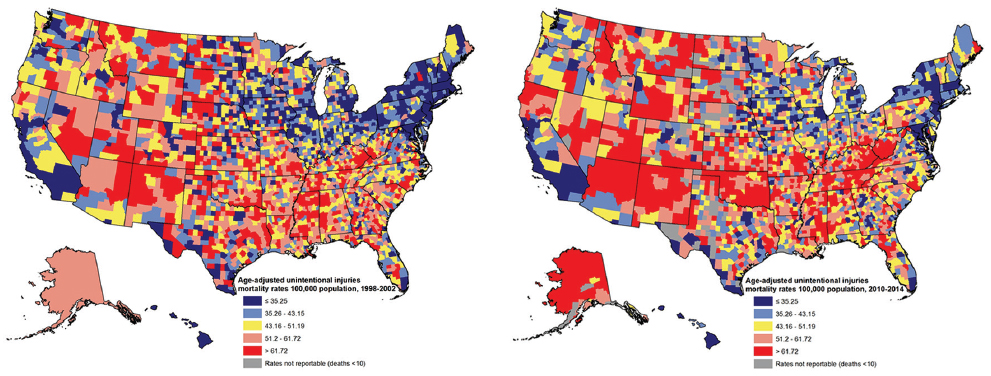
- Age-Adjusted Unintentional Injury Mortality Rates per 100,000 Population for the United States (3,143 Counties), 1998-2002 and 2010-2014
- Source: Derived from the 1998-2014 National Vital Statistics System.

- Age-adjusted Suicide Mortality Rates per 100,000 Population, United States, 1999-2015 (3,143 Counties)
- Source: Data derived from the US National Vital Statistics System.
Homicide is the third leading cause of death among American youth aged 15-34. The overall homicide rate is nearly 8 times higher among blacks and 2 times higher among AIANs and Hispanics compared to whites.[15] Homicide rates were stable between 1999 and 2015. Homicide rates are higher in the Southeast and Southwest regions than elsewhere in the US (Figure 21).
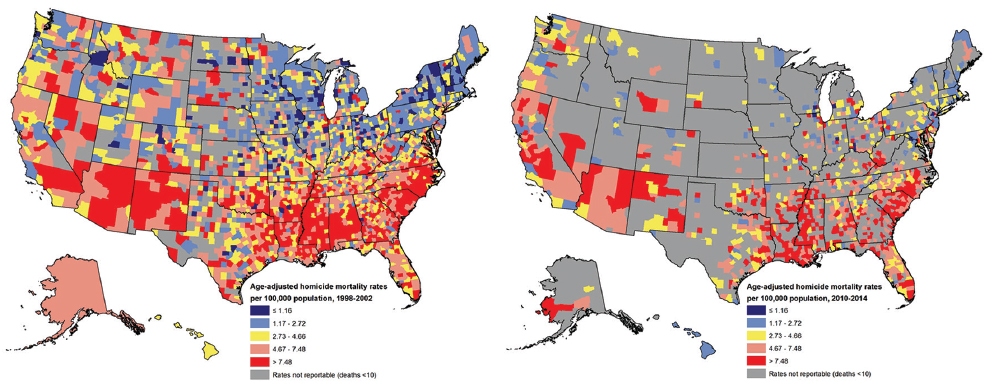
- Age-Adjusted Homicide Rates per 100,000 Population for the United States (3,143 Counties), 1998-2002 and 2010-2014
- Source: Derived from the 1998-2014 National Vital Statistics System.
Drug overdose deaths have contributed to the recent rise in mortality among middle-aged white Americans.[21] Rising deaths from drug overdose have been identified as a major public health problem in the United States.[35] In 2015, non-Hispanic whites had the highest rate of drug overdose mortality, 79% higher than the rate for Blacks, 7.6 times higher than the rate for APIs, and 2.8 times higher than the rate for Hispanics.[35] Geographic patterns in drug overdose mortality show a marked increase in drug overdose mortality between 2000 and 2015 in most areas, with higher rates of mortality observed in many counties of Appalachia and the Western United States (Figure 22).[36] Between 2010 and 2015, drug overdose mortality increased more rapidly in rural areas than in urban areas (270% vs. 150%). In 2015, non-metropolitan counties had slightly higher drug overdose mortality than metropolitan counties although rates tended to be the highest in the mid- and small-size metropolitan counties and the lowest in large metropolitan counties (Figure 23).
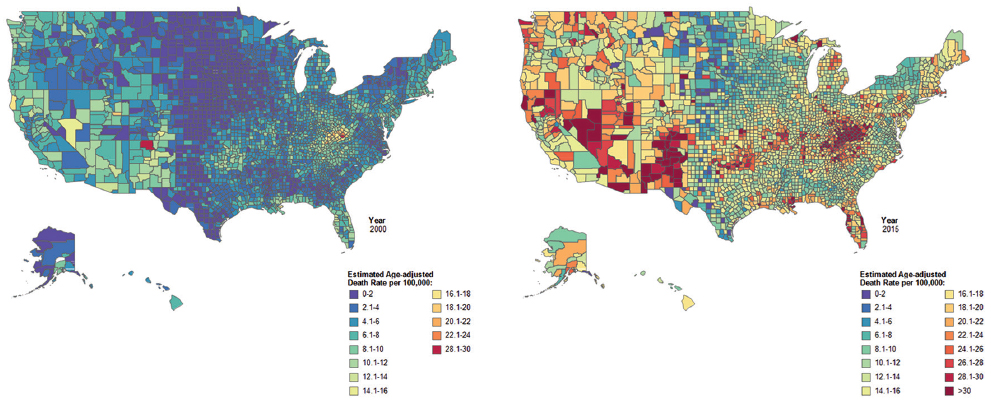
- Estimated Age-Adjusted Drug Overdose Mortality Rates per 100,000 Population by County, United States, 2000 and 2015
- Source: CDC/NCHS, National Vital Statistics System.
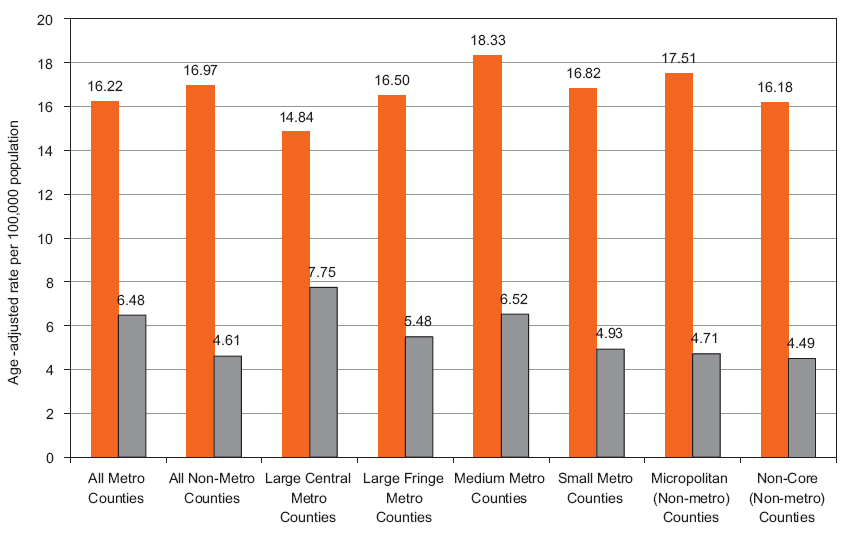
- Age-adjusted Drug Overdose Mortality Rate per 100,000 Population by Urbanization Level, United States, 2000 and 2015
- Source: CDC/NCHS. Data derived from the National Vital Statistics System.
Although HIV/AIDS is not a leading cause of death for the total US population, it is the sixth leading cause of death among blacks aged 20-54 years.[15] In 2014, HIV/AIDS mortality was 9.6 times higher among blacks and 2.2 times higher among Hispanics compared to whites.[15] Although HIV/AIDS mortality has declined dramatically since 1987, socioeconomic disparities remain substantial. During the 2010-2014 time period, individuals in the lowest socioeconomic quintile had 3.0 times higher HIV/AIDS mortality than those in the highest socioeconomic quintile (Figure 24).[23] County maps in Figure 25 show huge reductions in HIV/AID mortality since the peak years of the epidemic in the early 1990s for most counties and geographic regions, with higher HIV/AIDS mortality being concentrated in the Southern US in more recent time periods.[23]

- Trends in HIV/AIDS Mortality by County Socioeconomic Status, Both Sexes Combined, United States, 1987-2014
- Source: Singh GK, Azuine RE, Siahpush M. Widening Socioeconomic, Racial, and Geographic Disparities in HIV/AIDS Mortality in the United States, 1987-2011. Advances in Preventive Medicine. 2013. DOI: 10.1155/2013/657961. Updated data derived from the US National Vital Statistics System.
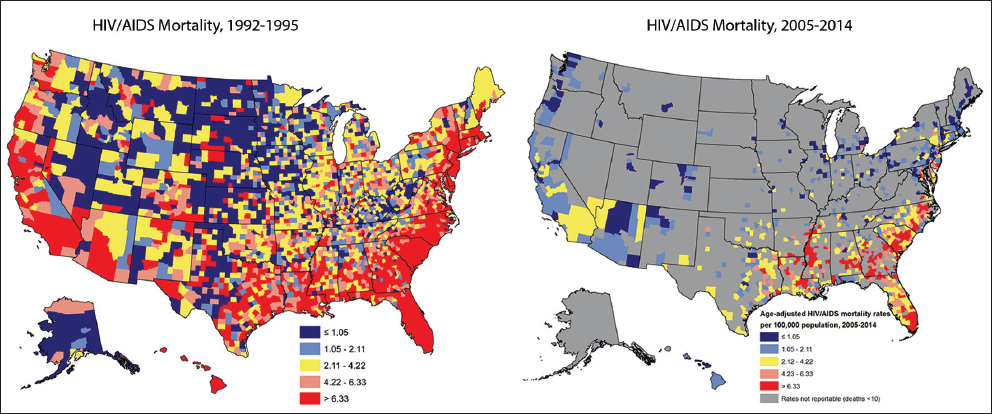
- Age-adjusted HIV/AIDS Mortality Rates per 100,000 Population, United States, 1992-2014 (3,143 Counties)
- Source: Singh GK, Azuine RE, Siahpush M. Widening Socioeconomic, Racial, and Geographic Disparities in HIV/AIDS Mortality in the United States, 1987-2011. Advances in Preventive Medicine. 2013. DOI: 10.1155/2013/657961. Updated data derived from the US National Vital Statistics System.
3.5. Disparities in prevalence of major chronic conditions and risk factors
Heart disease, cancer, diabetes, and COPD are the leading chronic diseases affecting the US adult population. Overall, 28.4 million or 11.0% of US adults aged 18 and over in 2015 had ever been told by a doctor or other health professional that they had heart disease (Table 2).[30] AIANs had a 21% higher heart disease prevalence and Asians 37% lower prevalence than whites. Unemployed adults had a 55% higher heart disease prevalence than adults with full-time employment. Those with lower education and income levels had higher heart disease prevalence than their high education or income counterparts. Residents of rural/nonmetropolitan areas had a 40% higher heart disease prevalence than urban/metropolitan residents.
| Characteristic | Heart disease | All cancers combined | Diabetes | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Prevalence | SE | RR | Prevalence | SE | RR | Prevalence | SE | RR | ||||
| Sex/gender | 11.0 | 0.23 | 8.0 | 0.17 | 8.9 | 0.20 | ||||||
| Male | 12.2 | 0.33 | 1.22* | 7.7 | 0.24 | 0.92* | 9.4 | 0.29 | 1.12* | |||
| Female | 10.0 | 0.30 | 1.00 | 8.4 | 0.25 | 1.00 | 8.4 | 0.25 | 1.00 | |||
| Race/ethnicity | ||||||||||||
| White | 11.3 | 0.27 | 1.00 | 8.8 | 0.21 | 1.00 | 8.1 | 0.22 | 1.00 | |||
| Black/African American | 9.5 | 0.50 | 0.84* | 4.7 | 0.36 | 0.53* | 13.1 | 0.55 | 1.62* | |||
| American Indian/Alaska Native | 13.7 | 2.25 | 1.21* | 5.1 | 1.57 | 0.58* | 20.9 | 2.94 | 2.58* | |||
| Asian | 7.1 | 0.78 | 0.63* | 3.0 | 0.50 | 0.34* | 9.0 | 0.81 | 1.11* | |||
| Native Hawaiian/Other Pacific Is | 8.9 | 4.33 | 0.79* | 8.0 | 3.34 | 0.91* | 11.7 | 3.38 | 1.44* | |||
| Hispanic or Latino | 8.2 | 0.45 | 0.73* | 4.3 | 0.37 | 0.49* | 12.2 | 0.56 | 1.51* | |||
| Multiple race | 16.8 | 1.91 | 1.49* | 7.3 | 1.41 | 0.83* | 11.9 | 1.74 | 1.47* | |||
| Marital status | ||||||||||||
| Married | 10.9 | 0.33 | 1.00 | 8.7 | 0.27 | 1.00 | 8.5 | 0.27 | 1.00 | |||
| Widowed | 11.7 | 1.66 | 1.07* | 7.5 | 0.67 | 0.86* | 12.3 | 2.65 | 1.45* | |||
| Dovorced/separated | 13.3 | 0.78 | 1.22* | 8.6 | 0.49 | 0.99* | 11.1 | 0.57 | 1.31* | |||
| Never married | 8.9 | 0.54 | 0.82* | 5.7 | 0.52 | 0.66* | 9.3 | 0.6 | 1.09* | |||
| Living with a partner | 12.7 | 1.24 | 1.17* | 9.4 | 1.12 | 1.08* | 9.5 | 1.15 | 1.12* | |||
| Place of residence | ||||||||||||
| Large metropolitan area | 10.0 | 0.29 | 1.00 | 7.4 | 0.25 | 1.00 | 8.6 | 0.27 | 1.00 | |||
| Small metropolitan area | 11.2 | 0.42 | 1.12* | 8.8 | 0.34 | 1.19* | 8.9 | 0.36 | 1.03* | |||
| Non-metropolitan area | 14.2 | 0.78 | 1.42* | 8.8 | 0.41 | 1.19* | 10.0 | 0.5 | 1.16* | |||
| Educational attainment | ||||||||||||
| < High school | 14.4 | 0.71 | 1.32* | 7.6 | 0.51 | 0.76* | 14.9 | 0.67 | 2.10* | |||
| High school graduate | 12.1 | 0.51 | 1.11* | 8.5 | 0.40 | 0.85* | 11.5 | 0.46 | 1.62* | |||
| Some college/associate degree | 12.9 | 0.47 | 1.18* | 10.2 | 0.37 | 1.02 | 10.2 | 0.41 | 1.44* | |||
| College graduate or higher | 10.9 | 0.42 | 1.00 | 10.0 | 0.38 | 1.00 | 7.1 | 0.34 | 1.00 | |||
| Family income | ||||||||||||
| <$35,000 | 14.2 | 0.44 | 1.49* | 7.9 | 0.31 | 0.82* | 12.40 | 0.38 | 2.03* | |||
| $35,000 - $49,999 | 11.3 | 0.69 | 1.19* | 8.3 | 0.50 | 0.86* | 10.50 | 0.60 | 1.72* | |||
| $50,000 - $74,999 | 10.3 | 0.54 | 1.08* | 7.5 | 0.43 | 0.78* | 8.40 | 0.51 | 1.38* | |||
| $75,000 - $99,999 | 9.8 | 0.69 | 1.03 | 8.7 | 0.53 | 0.91* | 7.50 | 0.58 | 1.23* | |||
| $100,000 or more | 9.5 | 0.53 | 1.00 | 9.6 | 0.47 | 1.00 | 6.10 | 0.43 | 1.00 | |||
| Employment status | ||||||||||||
| Employed, full time | 9.5 | 0.62 | 1.00 | 6.4 | 0.55 | 1.00 | 6.5 | 0.48 | 1.00 | |||
| Employed, part time | 9.7 | 0.71 | 1.02 | 7.4 | 0.65 | 1.16* | 8.4 | 0.69 | 1.29* | |||
| Not employed, but has | ||||||||||||
| Worked previously | 14.7 | 0.47 | 1.55* | 10.7 | 0.40 | 1.67* | 11.6 | 0.39 | 1.78* | |||
Rates are age-adjusted to the 2000 US standard population. SE=Standard error. RR. = prevalence rate ratio.
The prevalence of diabetes in the US has more than doubled during the past two decades. In 2015, 21.1 million adults aged 18 and over reported having diabetes. In 2015, the prevalence of physician-diagnosed diabetes varied from 8.1% for white adults to 20.9% for AIANs (Table 2).[30] Compared to whites, all major racial/ethnic minority groups had significantly higher diabetes prevalence. Higher diabetes prevalence was observed for lower socioeconomic groups. Adults with less than a high education, below the poverty line, or unemployed had almost twice the prevalence of diabetes as their advantaged counterparts. Geographical patterns indicate higher prevalence of adult diabetes in the South than in the Midwestern or Western states, with prevalence increasing markedly in all states between 2000 and 2016 (Figure 26).[34]

- Age-adjusted Prevalence of Diagnosed Diabetes among Adults Aged ≥18 years, by State, United States, 2000 and 2016
- Source: CDC. Behavioral Risk Factor Surveillance System. https://www.cdc.gov/brfss/index.html.
The prevalence and sociodemographic patterns in cancer vary according to cancer type. In 2015, 24.3 million or 8% of adults aged 18 and over had ever been told by a doctor or other health professional that they had some form of cancer (Table 2). Compared to white adults, all other racial/ethnic groups had lower prevalence of cancer. Adults with higher education and income levels had higher rates of cancer. However, unemployed adults were 67% more likely to be diagnosed with cancer than those working full time.
Regarding mental health problems, 8.3 million or 3.6% of US adults in 2015 experienced serious psychological distress during the past one month. Asians reported the lowest prevalence of psychological distress, whereas Native Hawaiians/Other Pacific Islanders and mixed-race adults had the highest prevalence, 9.3% and 9.5% respectively (Table 3). Adults without a job or with lower education and income levels were at an increased risk of psychological distress. Adults with an annual family income <$35,000 were 5.4 times more likely to experience serious psychological distress than those with annual family incomes of $100,000 or more.
| Characteristic | Serious psycholgical distress1 | Did not receive medical care due to cost2 | Delayed seeking medical care due to cost2 | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Prevalence | SE | RR | Prevalence | SE | RR | Prevalence | SE | RR | |
| Sex/gender | 3.6 | 0.15 | 4.4 | 0.10 | 6.3 | 0.13 | |||
| Male | 2.9 | 0.20 | 0.67* | 4.0 | 0.12 | 0.83* | 9.4 | 0.29 | 1.12* |
| Female | 4.3 | 0.22 | 1.00 | 4.8 | 0.13 | 1.00 | 8.4 | 0.25 | 1.00 |
| Race/ethnicity | |||||||||
| White | 3.5 | 0.15 | 1.00 | 4.3 | 0.11 | 1.00 | 6.4 | 0.14 | 1.00 |
| Black/African American | 3.5 | 0.38 | 1.00 | 5.8 | 0.27 | 1.35* | 6.6 | 0.29 | 1.03 |
| American Indian/Alaska Native | 14.0 | 3.54 | 4.00* | 5.0 | 0.84 | 1.16* | 6.8 | 0.91 | 1.06 |
| Asian | 2.1 | 0.46 | 0.60* | 2.7 | 0.34 | 0.63* | 3.6 | 0.38 | 0.56* |
| Native Hawaiian/OPI | 6.2 | 2.48 | 1.44* | 9.3 | 2.84 | 1.45* | |||
| Hispanic or Latino | 4.0 | 0.32 | 1.14* | 5.4 | 0.37 | 1.26* | 7.0 | 0.28 | 1.09 |
| Multiple race | 8.3 | 1.78 | 2.37* | 7.5 | 0.76 | 1.74* | 9.5 | 0.86 | 1.48* |
| Marital status | |||||||||
| Married | 2.3 | 0.17 | 1.00 | ||||||
| Widowed | 2.9 | 0.46 | 1.26* | ||||||
| Dovorced/separated | 6.9 | 0.72 | 3.00* | ||||||
| Never married | 4.6 | 0.45 | 2.00* | ||||||
| Living with a partner | 4.3 | 0.60 | 1.87* | ||||||
| Place of residence | |||||||||
| Large metropolitan area | 3.2 | 0.20 | 1.00 | 4.1 | 0.13 | 1.00 | 5.9 | 0.17 | 1.00 |
| Small metropolitan area | 3.7 | 0.29 | 1.16* | 4.6 | 0.19 | 1.12* | 6.7 | 0.24 | 1.14* |
| Nonmetropolitan area | 4.9 | 0.44 | 1.53* | 5.3 | 0.28 | 1.29* | 6.8 | 0.32 | 1.15* |
| Educational attainment | |||||||||
| < High school | 8.3 | 0.70 | 5.93* | 8.7 | 0.40 | 2.90* | 10.4 | 0.45 | 1.96* |
| High school graduate | 4.2 | 0.37 | 3.00* | 6.5 | 0.26 | 2.17* | 8.3 | 0.30 | 1.57* |
| Some college/associate degree | 3.6 | 0.28 | 2.57* | 7.1 | 0.25 | 2.37* | 9.8 | 0.30 | 1.85* |
| College graduate or higher | 1.4 | 0.16 | 1.00 | 3.0 | 0.15 | 1.00 | 5.3 | 0.20 | 1.00 |
| Family income | |||||||||
| <$35,000 | 7.3 | 0.37 | 5.21* | 9.5 | 0.27 | 10.56* | 11.3 | 0.28 | 5.38* |
| $35,000 - $49,999 | 3.6 | 0.45 | 2.57* | 6.3 | 0.36 | 7.00* | 9.4 | 0.15 | 4.48* |
| $50,000 - $74,999 | 2.8 | 0.39 | 2.00* | 4.1 | 0.25 | 4.56* | 6.6 | 0.33 | 3.14* |
| $75,000 - $99,999 | 1.8 | 0.31 | 1.29* | 2.3 | 0.24 | 2.56* | 4.2 | 0.33 | 2.00* |
| $100,000 or more | 1.4 | 0.23 | 1.00 | 0.9 | 0.09 | 1.00 | 2.1 | 0.17 | 1.00 |
| Employment status | |||||||||
| Employed, full time | 1.4 | 0.12 | 1.00 | 6.4 | 0.55 | 1.00 | 6.5 | 0.48 | 1.00 |
| Employed, part time | 2.9 | 0.39 | 2.07 | 7.4 | 0.65 | 1.16* | 8.4 | 0.69 | 1.29* |
| Not employed, but has | |||||||||
| Worked previously | 8.1 | 0.45 | 5.79* | 10.7 | 0.40 | 1.67* | 11.6 | 0.39 | 1.78* |
Rates are age-adjusted to the 2000 US standard population. SE=standard error. RR=prevalence rate ratio.
Smoking, obesity, and hypertension are major risk factors that are associated with increased risk of mortality and morbidity from several chronic diseases such as CVD, cancer, diabetes, and COPD. Marked socioeconomic and racial/ethnic disparities exist in smoking; adults with annual family incomes <$35,000 have a 3.6 times higher current smoking rate than those with family income ≥100,000 (Figure 27). Lower income levels are also associated with significantly higher rates of obesity and hypertension. Compared to non-Hispanic whites, AIANs and blacks have higher rates and APIs lower rates of smoking and obesity.[30] In 2015, Black adults (34.4%) and AIANs (28.4%) had higher prevalence of hypertension than non-Hispanic whites (24.1%), whereas Asians had lower prevalence (20.6%). Educational disparities in these risk factors are also large. For example, in 2015, 25.9% of those with less than a high school education were current smokers, compared with 5.8% of those with a college degree.[30]
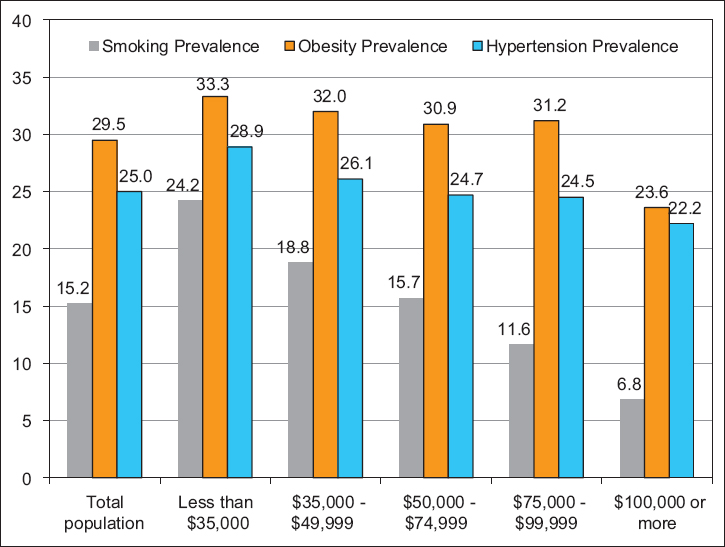
- Age-Adjusted Prevalence (%) of Current Smoking, Obesity, and Hypertension by Family Income, US Adults Aged 18 Years and Older, 2015
- Source: CDC/NCHS. 2015 National Health Interview Survey.
3.6. Disparities in health care access and quality
An important measure of access to quality health care is affordability. There are marked disparities in unmet medical need among the US population according to various sociodemographic factors (Table 3).[30] In 2015, 6.2% of Native Hawaiians/Other Pacific Islanders and 7.5% of mixed-race individuals reported not receiving medical care because they could not afford it, compared with 2.7% of Asians and 4.3% of whites. Additionally, 9.3% of Native Hawaiians/Other Pacific Islanders and 7.5% of mixed-race individuals delayed seeking medical care because of the worry about the cost, compared with 3.6% of Asians and 6.4% of whites. Affordability of health care costs is a significant issue in health care decision making among those in lower socioeconomic strata or among those living in rural areas. Individuals with an annual family income <$35,000 were 10.6 times more likely to forgo needed medical care due to cost than those with annual family incomes of $100,000 or more. Individuals without a job were 1.7 to 1.8 times more likely to forgo or delay needed medical care due to cost than those with a full-time job.
Emergency room (ER) visits are associated with substantially increased health care costs. The likelihood of an ER visit is greater among AIAN children (13.9%) and black children (7.6%), compared to Asian (2.7%) and white (4.9%) children (Figure 28). Likelihood of an ER visit is significantly higher among children in rural areas as well as among children in single-mother households and in low-income families.[30]

- Emergency Room (ER) Visits by Sociodemographic Factors, Children <18 Years of Age, United States, 2015 National Health Interview Survey
4. Discussion, Conclusions, and Global Health Implications
In this paper, we have analyzed major health inequality trends affecting America’s diverse, vulnerable, and socially disadvantaged populations. Although substantial progress has been made in improving the health and well-being of all Americans, health inequities between population groups and geographic areas have persisted and remain marked, which represents a major area of policy concern. Striking disparities are found in a number of health indicators, including life expectancy, infant mortality, CVD, cancer, diabetes, COPD, HIV/AIDS, health care access and utilization, health insurance, mental health, smoking, obesity, drug overdose mortality, suicide, homicide, and unintentional injuries. Social inequalities in health tend to be larger in the US than in many other industrialized countries. This gap is particularly true for infant mortality and life expectancy, where the US lags behind other industrialized countries as the pace of improvements in these indicators has not kept up with that for other nations.[24,37,38]
There are wide racial/ethnic and gender disparities in life expectancy, including a gap of more than 17 years in life expectancy between black men (72.3 years) and API women (89.7 years). Rural-urban disparities in life expectancy have widened over time as rural residents recorded smaller gains in life expectancy during 1990-2014 than their urban counterparts. Life expectancy currently ranges from 74.5 years for men in rural areas to 82.4 years for women in large metropolitan areas. Although infant mortality rates declined dramatically during the past eight decades, racial disparities widened over time. Currently black infants have 2.3 times higher mortality rates than white infants (11.4 vs. 4.9 per 1,000 live births). Infant and child mortality is markedly higher in rural areas and poor communities. Black infants and children in poor, rural communities have nearly three times higher mortality rates compared to those in affluent, rural areas.
Causes of the health disparities reported here are multifactorial in nature. Research indicates that differences in social and built environments, socioeconomic and living conditions, health-risk behaviors such as tobacco use, obesity, lack of access to healthy foods, and access to and use of quality health care services are important social determinants contributing to persistent health disparities between population groups and geographic areas.[1,2,21]
Although reduced smoking, greater physical activity, lower obesity, healthy diet, higher seatbelt use, avoiding substance use, and improved access to and use of health care services can lead to improvements in population health and health equity, these factors are themselves primarily influenced by broader, more upstream social determinants such as education, income, social and welfare services, affordable housing, job creation, labor market opportunities, and transportation.[16,17,21,22] Addressing inequities in these social determinants should be an important area of focus from both research and policy standpoints. Since policy action on many of the social determinants goes beyond the traditional health sector and since health inequities are multifaceted, a multi-sectoral approach involving health, education, nutrition, housing, urban planning, transportation, and economic sectors is needed to tackle health inequalities effectively.[10,39] Such an approach calls for increased collaboration between public and private sectors and various stakeholders including state and local agencies and emphasizes the need for community-based approaches to reducing health disparities in the United States.[10,39,40]
Investing in early childhood education and development has been suggested as a cost-effective strategy for preventing disease and increasing productivity later in life.[41] Several US federal programs, such as Healthy Start, Maternal, Infant, and Early Childhood Home Visiting, and Title V MCH Block Grant Programs, are excellent programmatic efforts that emphasize investments in early child development, leading to positive health outcomes not only during childhood but throughout the life course.[42] Other federally sponsored community-based programs have proven effective in reducing smoking and obesity-related chronic diseases and promoting positive health behaviors such as good nutrition and increased physical activity.[21] Federal health care programs, particularly the Health Center Program, work to mitigate adverse health effects of social disadvantage, poverty, and unfavorable living conditions by providing increased access to health and social services to vulnerable populations who otherwise would lack or be unable to afford such services.[43,44]
Acknowledgements
The views expressed are the authors’ and not necessarily those of the US Department of Health and Human Services or the Health Resources and Services Administration.
Conflicts of Interest: The authors declare that they have no conflicts of interest.
Financial Disclosure: None to report.
Funding/Support: None.
Ethics Approval: All analyses were conducted using public-use data and were thus exempt from the institutional review board (IRB) approval.
References
- Healthy People 2020. http://www.healthypeople.gov/2020/default.aspx
- Health, United States, 2011 with Special Feature on Socioeconomic Status and Health. Hyattsville, MD: U.S. Department of Health and Human Services; 2012.
- Health, United States, 2015 with Special Feature on Racial and Ethnic Health Disparities. Hyattsville, MD: US Department of Health and Human Services; 2016.
- Health Resources and Services Administration. In: Eliminating Health Disparities in the United States. 2000.
- [Google Scholar]
- Maternal and Child Health Bureau. MCH Timeline: History, Legacy and Resources for Education and Practice, In-Depth Issues. https://mchb.hrsa.gov/about/timeline/in-depth-2-infant-mortality.asp
- Differential Mortality in the United States: A Study in Socioeconomic Epidemiology. Cambridge, MA: Harvard University Press; 1973.
- Mortality, Occupation, and Socioeconomic Status. In: Vital Statistics – Special Reports, Selected Studies 33 No. 10. Washington, DC: National Center for Health Statistics; 1951.
- [Google Scholar]
- Vital Statistics Rates in the United States 1940-1960. In: National Center for Health Statistics. Washington, DC: US Department of Health, Education, and Welfare; 1968.
- [Google Scholar]
- 2003. Social Determinants of Health: The Solid Facts. (Second Edition). Copenhagen, Denmark: World Health Organization, Regional Office for Europe; http://www.euro.who.int/__data/assets/pdf_file/0005/98438/e81384.pdf
- Socioeconomic and behavioral differences in health, morbidity, and mortality in Kansas: empirical data, models, and analyses. In: Tarlov AR, St. Peter RF, eds. The Society and Population Health Reader, Volume II: A State and Community Perspective. New York: The New Press; 2000. p. :15-56.
- [Google Scholar]
- Society and Health. New York: Oxford University Press; 1995.
- A glossary of health inequalities. Journal of Epidemiology and Community Health. 2006;56(9):647-652.
- [Google Scholar]
- Widening socioeconomic inequalities in US life expectancy 1980-2000. International Journal of Epidemiology. 2006;35(4):969-979.
- [Google Scholar]
- Widening rural-urban disparities in life expectancy, U.S. 1969-2009. American Journal of Preventive Medicine. 2014;46(2):e19-e29.
- [Google Scholar]
- Increasing inequalities in all-cause and cardiovascular mortality among US adults aged 25-64 years by area socioeconomic status 1969-1998. International Journal of Epidemiology. 2002;31(3):600-613.
- [Google Scholar]
- Widening socioeconomic and racial disparities in cardiovascular disease mortality in the United States 1969-2013. International Journal of MCH and AIDS. 2015;3(2):106-118.
- [Google Scholar]
- Widening geographical disparities in cardiovascular disease mortality in the United States 1969-2011. International Journal of MCH and AIDS. 2015;3(2):134-149.
- [Google Scholar]
- Widening disparities in infant mortality and life expectancy between Appalachia and the rest of the United States 1990-2013. Health Affairs. 2017;36(8):1423-1432.
- [Google Scholar]
- Socioeconomic and racial/ethnic disparities in cancer mortality, incidence, and survival in the United States 1950-2014: over six decades of changing patterns and widening Inequalities. Journal of Environmental and Public Health 2017 DOI: 2017/2819372. Epub March 2017
- [Google Scholar]
- Widening socioeconomic, racial, and geographic disparities in HIV/AIDS Mortality in the United States 1987-2011. Advances in Preventive Medicine 2013 DOI: 10.1155/2013/657961. Epub 7 May 2013
- [Google Scholar]
- 2010. Infant Mortality in the United States, 1935-2007: Over Seven Decades of Progress and Disparities. A 75th Anniversary Publication. Health Resources and Services Administration, Maternal and Child Health Bureau. Rockville, Maryland: U.S. Department of Health & Human Services; http://www.hrsa.gov/healthit/images/mchb_infantmortality_pub.pdf
- 2010. Child Mortality in the United States, 1935-2007: Large Racial and Socioeconomic Disparities Have Persisted Over Time. A 75th Anniversary Publication. Health Resources and Services Administration, Maternal and Child Health Bureau 2010. Rockville, Maryland: US Department of Health and Human Services; http://www.hrsa.gov/healthit/images/mchb_child_mortality_pub.pdf
- Understanding the sociodemographic differences in health: the role of fundamental social causes. American Journal of Public Health. 1996;86(4):471-473.
- [Google Scholar]
- US socioeconomic and racial differences in health: patterns and explanations. Annual Review of Sociology. 1995;21:349-386.
- [Google Scholar]
- Social determinants of health: socioeconomic status, social class, and ethnicity. American Journal of Public Health. 1995;85(7):903-905.
- [Google Scholar]
- 2016. National Health Interview Survey 2015. Hyattsville, MD: US Department of Health and Human Services; https://www.cdc.gov/nchs/nhis/
- The Health and Well-Being of Children: A Portrait of States and the Nation 2011-2012 2014
- Summary File 3, Technical Documentation 2000 Census of Population and Housing. Washington, DC: US Department of Commerce; 2005.
- Drug overdose deaths in the United States 1999-2015. NCHS Data Brief. 2017;273:1-8.
- [Google Scholar]
- Drug Poisoning Mortality: United States 1999-2015. 2017. Data Visualization Gallery. Hyattsville, MD: US Department of Health and Human Services; https://www.cdc.gov/nchs/data-visualization/drug-poisoning-mortality/
- [Google Scholar]
- The Spirit Level: Why Greater Equality Makes Societies Stronger. New York, NY: Bloomsbury Press; 2009.
- Health at a Glance 2015. Paris: OECD Publishing; 2015.
- 2016. Road Map for the Plan of Action on Health in All Policies. Washington, DC: World Health Organization, Regional Office for the Americas; http://iris.paho.org/xmlui/bitstream/handle/123456789/31313/9789275074541-eng.pdf?sequence=1&isAllowed=y
- Strategies for reducing health disparities –selected CDC-sponsored interventions, United States 2016, background and rationale. Morbidity and Mortality Weekly Report (MMWR). 2016;65(1):2-3.
- [Google Scholar]
- Addressing social issues affecting health to improve US health outcomes. The Journal of the American Medical Association (JAMA). 2017;315(15):1552-1553.
- [Google Scholar]
- Maternal and Child Health. Programs and Initiatives. https://mchb.hrsa.gov/maternal-child-health-initiatives/mchb-programs
- Bureau of Primary Health Care. Health Center Program. https://www.bphc.hrsa.gov/about/healthcenterfactsheet.pdf
- 2017. HRSA: Agency Overview. https://www.hrsa.gov/sites/default/files/hrsa/about/budget/hrsabudgetoverview-2018.pdf





