Translate this page into:
Association Between Social Determinants of Health Issues and Maternal Obesity Among American Racial/Ethnic Groups
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 4.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Background and Objective:
Social determinants of health impact various clinical health outcomes in the population. We conducted this study to examine the impact of adverse social determinants of health (SDOH) characteristics on maternal obesity among hospitalized pregnant women in the US and its potential differential impact on women of different races/ethnicities.
Methods:
The nationwide pregnancy hospitalization data analyzed in this study were collected through the Nationwide Inpatient Sample (NIS) database during 2016-2018. We conducted descriptive analyses to evaluate the relationship between patient characteristics and maternal obesity. Using the adjusted survey logistic regression model, we calculated the independent association between social determinants of health (SDOH) risk factors and hospitalization characteristics (exposure) and maternal obesity (outcome). Lastly, stratified survey logistic regression models were created for each racial/ethnic group to examine the differential impact in the association between SDOH issues and maternal obesity.
Results:
The prevalence of SDOH issues was highest in non-Hispanic (NH) Black women (6.59 per 1000 hospitalizations), whereas the prevalence of obesity among those with SDOH issues was highest in Hispanic women (15.3 per 100 hospitalizations). We observed that pregnant women with SDOH issues were 1.15 times as likely (95% CI: 1.05-1.25) to experience maternal obesity compared to those without SDOH issues. Relative to their counterparts without SDOH issues, Hispanics and NH-Others with SDOH issues had increased odds of obesity, whereas NH-White and NH-Black mothers with SDOH had similar odds of obesity (p>0.05).
Conclusion and Global Health Implications:
In conclusion, pregnant women with SDOH issues had an increased likelihood of obesity diagnosis and the association demonstrated differential impact across racial/ethnic sub-populations. This information has potential utility for counseling and formulation of targeted interventions for pregnant women.
Keywords
Social Determinants of Health
Maternal Obesity
Pregnant Women
Hospitalizations
Racial/Ethnic Differences
1. Introduction
Body mass index (BMI) is a statistical means of estimating an individual’s body fat by considering their height and weight.1 It is specifically calculated using the following formula: BMI = weight (in kg)/height2 (in m2), and a value of 30 kg/m2 is categorized as obese.1 Obesity is an increasing global health problem and a grave public health threat.2 In the last two decades, there has been a drastic increase in the prevalence of obesity in the United States (US) - from 30.5% in 1999-2000 to 42.4% in 2017-2018.3 Obesity is associated with an increase in mental health issues, and a decrease in quality of life,4 and it may lead to multiple serious yet preventable health concerns, such as heart disease, hypertension, dyslipidemia, stroke, type-2 diabetes, certain types of cancer and even premature death.3,5
The etiology of obesity is considered to be multifactorial, with contributors including individual factors, like behavior and genetics, as well as environmental factors.4-6 Environmental factors that can impact a person’s health outcomes are referred to as social determinants of health (SDOH) and include characteristics such as economic stability, quality of education, neighborhood conditions, access to healthcare, and social environment.7 Specific adverse SDOH characteristics can lead to an increased risk for obesity; for instance, those living in food deserts have limited access to nutrient-dense foods and are more likely to become obese.7
It has also been observed that certain demographic groups are more prone to developing obesity.3,8,9 Those aged 40 years or older have an increased prevalence of obesity when compared with those younger than 40 years; those belonging to non-Hispanic (NH) Black and Hispanic races/ethnicities are reported to have a higher prevalence of being obese than NH-Whites and NH-Asians.3 SDOH characteristics such as income and education level have an effect modifying role on obesity prevalence when considered alongside demographic characteristics such as sex or race/ethnicity.2 For example, it has been reported that obesity prevalence among men is generally similar across all income levels, with a tendency to be slightly higher at higher income levels, whereas obesity prevalence among women increases as income decreases.2 Similarly, no statistical difference has been observed between obesity and education level among men, whereas obesity prevalence in women increases with decreasing educational level.2
Maternal obesity is associated with multiple adverse maternal-fetal outcomes, neonatal complications, and morbidity.10 It has been noted that maternal obesity can impede normal placental function, thereby facilitating complications in fetal metabolism and overall neonatal health.11,12 Furthermore, specific SDOH characteristics, ranging from literacy issues to economic problems, can predispose obese mothers to gestational diabetes mellitus, pre-eclampsia, hyperlipidemia, and other distinct comorbidities, which contribute to adverse maternal-fetal outcomes by compounding the health risks that obesity already poses to mothers and infants.13
There have been some studies conducted in the past that examined the factors contributing towards maternal obesity,10,14 but the literature on the effect of SDOH issues on maternal obesity among various racial/ethnic groups in the US is very limited. Therefore, we undertook this study to 1) examine the combined impact of SDOH issues on maternal obesity among hospitalized pregnant women in the US and 2) examine the potential differential impact of SDOH issues on obesity among women of different races/ethnicities. We hypothesize that SDOH issues will aggravate the odds of maternal obesity among pregnant hospitalized women in the US and that the odds will be higher in racial/ethnic minority women.
2. Methods
This was a cross-sectional study using the Nationwide Inpatient Sample (NIS) - the largest all-payer inpatient database, made available by the Healthcare Cost and Utilization Project (HCUP),15 for the years 2016-2018. The information was obtained from discharge records of all hospitalizations occurring in the US during the study period. The NIS uses a sampling technique that stratifies all non-federal community hospitals from participating states into groups based on five major hospital characteristics: (a) rural/urban location, (b) number of beds, (c) geographic region, (d) teaching status, and (e) ownership. A 20% sample of hospitals is randomly drawn from each stratum, and all inpatient discharges from selected hospitals are included. HCUP includes information on hospitalizations occurring in 47 states in the US and when weighted, corresponds to about 35 million annual hospitalizations.
All pregnancy-related hospitalizations in women aged 15-49 years were included in this study. International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM) diagnosis and procedure codes were used to capture the up to 30 comorbidities and procedures associated with each hospitalization. ICD-10-CM diagnosis codes in the range Z55-Z65 were utilized to identify SDOH issues in patients’ discharge records. Problems related to education and literacy using codes Z55x, problems related to employment and unemployment – Z56x, occupational exposure to risk factors – Z57x, problems related to the physical environment – Z58x, problems related to housing and economic circumstances – Z59x, problems related to the social environment – Z60x, problems related to upbringing – Z62x, other problems related to the primary support group, including family circumstances – Z63x, problems related to certain psychosocial circumstances – Z64x, problems related to other psychosocial circumstances – Z65x.
We created one composite variable called ‘SDOH issues’ to identify any kind of SDOH characteristic that a patient may have, which was the exposure for the study. Maternal obesity (outcome for the study) was identified using codes O99.21x, E66.0x, E66.1x, E66.2x, E66.8x, and E66.9x in patients’ hospitalization discharge records, which included general obesity or obesity conditions complicating the ongoing pregnancy. The covariates for the study were categorized into clinically meaningful categories. Maternal age - (a) 15-24 years, (b) 25-34 years, and (c) 35-49 years; race-ethnicity was first determined by ethnicity (Hispanic or non-Hispanic), with the non-Hispanic (NH) group further subdivided by race (White, Black, or other); median household income quartile was estimated by HCUP using the zip code of residence on the mother’s delivery record and zip code-demographic data; primary payers for each hospital stay were classified into Medicare, Medicaid, private, self-pay and others. Hospital characteristics were assessed based on their teaching status (teaching vs. non-teaching), location (urban vs. rural), and US geographic region (Northeast, Midwest, South, or West). A hospital’s bed size, which assesses the number of short-term acute care beds set up and staffed in a hospital, was categorized as small, medium, large, or missing using US regions, the urban–rural designation of the hospital, and teaching status. Rural hospitals were not split based on teaching status for bed size categorization purpose because rural teaching hospitals were rare.
All statistical analyses were performed using R version 3·5· 1 (University of Auckland, Auckland, New Zealand), R Studio Version 1·1· 423 (Boston, MA). Descriptive statistics were utilized for hospitalization characteristics in patients with SDOH issues and obesity diagnosis. Using Pearson’s chi-squared test, we examined the bivariate association between each patient’s characteristics and each of the exposure (SDOH issues) and the outcome variable (obesity). We further calculated the prevalence of SDOH issues in pregnancy hospitalizations and the prevalence of obesity among pregnancy hospitalizations with SDOH issues stratified by race/ethnicity. Using the adjusted survey logistic regression model, we calculated the association between SDOH risk factors (exposure) and maternal obesity (outcome). Covariates such maternal age, race/ethnicity, discharge status, zipcode income quartile, primary payer, hospital’s location, teaching status, region and bedsize were utilized for adjustment in regression models. Lastly, stratified survey logistic regression models were created for each racial/ethnic group to examine the differential impact in the association between SDOH issues and maternal obesity. Survey logistic regression utilizes the weights, cluster and strata associated with the records to account for the complex survey design of the data. These models were created for each racial/ethnic group individually and compared against each other to examine the differential association of SDOH issues and maternal obesity across different race/ethnicities. All tests were two-tailed with type-I error set at 5%. Since the study was performed using de-identified publicly available data, the Institutional Review Board (approval ID H-36335) classified this study as exempt.
3. Results
We observed a total of 12,106,775 pregnancy-related hospitalizations during the study period (2016-2018), out of which 47,445 (0.4%) had SDOH issues and 1,240,870 (10.2%) had a diagnosis of maternal obesity. A total of 5,705 (12.0%) hospitalizations were identified with a diagnosis of both SDOH and obesity. Table 1 shows the proportional distribution and prevalence of various patient/hospital characteristics among pregnancy-related hospitalizations with a diagnosis of SDOH issues and obesity. Both SDOH issues and maternal obesity proportions were highest in patients 25-34 years, NH-White women, those belonging to the lowest quartile income group, and those insured by Medicaid.
| SDOH issues | Obesity | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| No | Yes | Prevalence | No | Yes | Prevalence | |||||
| N=12,059, 330 | %=100 | N=47, 445 | %=100 | N=10,865, 906 | %=100 | N=1,240, 870 | %=100 | |||
| Age | ||||||||||
| 15-24 years | 3,049,707 | 25.30% | 16,735 | 35.30% | 0.5% | 2,788,657 | 25.70% | 277,785 | 22.40% | 9.10% |
| 25-34 years | 6,879,939 | 57.10% | 23,520 | 49.60% | 0.30% | 6,187,025 | 56.90% | 716,435 | 57.70% | 10.40% |
| 35-49 years | 2,129,684 | 17.70% | 7,190 | 15.20% | 0.30% | 1,890,224 | 17.40% | 246,650 | 19.90% | 11.50% |
| Race/Ethnicity | ||||||||||
| NH-White | 5,975,909 | 49.60% | 20,430 | 43.10% | 0.30% | 5,440,825 | 50.10% | 555,515 | 44.80% | 9.30% |
| NH-Black | 1,815,835 | 15.10% | 12,050 | 25.40% | 0.70% | 1,548,990 | 14.30% | 278,895 | 22.50% | 15.30% |
| Hispanic | 2,388,708 | 19.80% | 9,150 | 19.30% | 0.40% | 2,129,743 | 19.60% | 268,115 | 21.60% | 11.20% |
| NH-Other | 1,326,104 | 11.00% | 3,650 | 7.70% | 0.30% | 1,239,509 | 11.40% | 90,245 | 7.30% | 6.80% |
| Missing | 552,774 | 4.60% | 2,165 | 4.60% | 0.40% | 506,839 | 4.70% | 48,100 | 3.90% | 8.70% |
| Discharge Status | ||||||||||
| Routine | 11,793,660 | 97.80% | 43,285 | 91.20% | 0.40% | 10,631,341 | 97.80% | 1,205,604 | 97.20% | 10.20% |
| Transfer | 61,905 | 0.50% | 1,860 | 3.90% | 2.90% | 57,470 | 0.50% | 6,295 | 0.50% | 9.90% |
| Died | 1,365 | 0.00% | 20 | 0.00% | 1.40% | 1,255 | 0.00% | 130 | 0.00% | 9.40% |
| DAMA | 40,025 | 0.30% | 1,360 | 2.90% | 3.30% | 36,940 | 0.30% | 4,445 | 0.40% | 10.70% |
| Other | 157,735 | 1.30% | 830 | 1.70% | 0.50% | 134,535 | 1.20% | 24,030 | 1.90% | 15.20% |
| Missing | 4,640 | 0.00% | 90 | 0.20% | 1.90% | 4,365 | 0.00% | 365 | 0.00% | 7.70% |
| Zip Income quartile | ||||||||||
| Lowest quartile | 3,416,872 | 28.30% | 16,950 | 35.70% | 0.50% | 3,018,213 | 27.80% | 415,610 | 33.50% | 12.10% |
| 2nd quartile | 3,041,272 | 25.20% | 12,655 | 26.70% | 0.40% | 2,726,303 | 25.10% | 327,625 | 26.40% | 10.70% |
| 3rd quartile | 2,920,507 | 24.20% | 9,630 | 20.30% | 0.30% | 2,632,353 | 24.20% | 297,785 | 24.00% | 10.20% |
| Highest quartile | 2,565,658 | 21.30% | 5,445 | 11.50% | 0.20% | 2,382,268 | 21.90% | 188,835 | 15.20% | 7.30% |
| Missing | 115,020 | 1.00% | 2,765 | 5.80% | 2.30% | 106,770 | 1.00% | 11,015 | 0.90% | 9.40% |
| Primary Payer | ||||||||||
| Medicare | 100,305 | 0.80% | 1,495 | 3.20% | 1.50% | 84,830 | 0.80% | 16,970 | 1.40% | 16.70% |
| Medicaid | 5,246,951 | 43.50% | 34,035 | 71.70% | 0.60% | 4,659,121 | 42.90% | 621,865 | 50.10% | 11.80% |
| Private Insurance | 6,046,480 | 50.10% | 8,370 | 17.60% | 0.10% | 5,498,375 | 50.60% | 556,475 | 44.80% | 9.20% |
| Self-Pay | 650,234 | 5.40% | 3,465 | 7.30% | 0.50% | 609,724 | 5.60% | 43,975 | 3.50% | 6.70% |
| Missing | 15,360 | 0.10% | 80 | 0.20% | 0.50% | 13,855 | 0.10% | 1,585 | 0.10% | 10.30% |
| Hospital Characteristics | ||||||||||
| Hospital Region | ||||||||||
| Northeast | 1,923,464 | 16.00% | 8,560 | 18.00% | 0.40% | 1,745,489 | 16.10% | 186,535 | 15.00% | 9.70% |
| Midwest | 2,528,863 | 21.00% | 9,700 | 20.40% | 0.40% | 2,277,278 | 21.00% | 261,285 | 21.10% | 10.30% |
| South | 4,728,879 | 39.20% | 15,220 | 32.10% | 0.30% | 4,251,579 | 39.10% | 492,520 | 39.70% | 10.40% |
| West | 2,878,124 | 23.90% | 13,965 | 29.40% | 0.50% | 2,591,559 | 23.90% | 300,530 | 24.20% | 10.40% |
| Hospital Bed Size | ||||||||||
| Small | 2,205,456 | 18.30% | 8,295 | 17.50% | 0.40% | 1,993,841 | 18.30% | 219,910 | 17.70% | 9.90% |
| Medium | 3,679,209 | 30.50% | 11,760 | 24.80% | 0.30% | 3,348,589 | 30.80% | 342,379 | 27.60% | 9.30% |
| Large | 6,174,665 | 51.20% | 27,390 | 57.70% | 0.40% | 5,523,475 | 50.80% | 678,580 | 54.70% | 10.90% |
| Hospital Location and Teaching Status | ||||||||||
| Rural | 1,089,650 | 9.00% | 3,755 | 7.90% | 0.30% | 1,003,235 | 9.20% | 90,170 | 7.30% | 8.20% |
| Urban non-teaching | 2,639,944 | 21.90% | 7,165 | 15.10% | 0.30% | 24,127,79 | 22.20% | 234,330 | 18.90% | 8.90% |
| Urban teaching | 8,329,736 | 69.10% | 36,525 | 77.00% | 0.40% | 7,449,892 | 68.60% | 916,370 | 73.80% | 11.00% |
SDOH - Social Determinants of Health; NH – non-Hispanic; DAMA – discharged against medical advice The ‘%=100’ column represents the proportion of each hospitalization characteristic in patients with SDOH issues and obesity. The sum of the proportions for each sub-group is 100%. Total N for SDOH issues and Obesity does not match because the data was weighted, and the numbers were rounded to the nearest integer. Prevalence shows the rate of SDOH issues or obesity in each of the patient’s hospitalization characteristics
Obesity prevalence was shown to increase with increased age, with a prevalence of 9.1% among 15-24 years and 11.5% among those who were 35-49 years, whereas the prevalence of SDOH issues was highest in the 15-24 years group (0.5%). Within race/ethnicity categories, obesity and SDOH were most prevalent among hospitalizations of NH-Black patients (15.3% and 0.7%, respectively) followed by Hispanic patients (11.2% and 0.4%, respectively). The prevalence of obesity and SDOH issues were highest among hospitalizations in which the patients were discharged against medical advice (10.7% and 3.3%, respectively). It was also observed that the prevalence of obesity and SDOH issues increased as the patient’s zip income quartile decreased, with an obesity prevalence of 12.1% and SDOH issues prevalence of 0.5% for the lowest quartile. With regards to insurance use, obesity prevalence in Medicare was 16.7% whereas the prevalence of SDOH issues in the same group was 1.5%.
Figure 1 shows the prevalence of SDOH issues among pregnancy-related hospitalizations, as well as the prevalence of maternal obesity among those with SDOH issues across different racial/ethnic groups. NH-Black patients had the highest prevalence of SDOH issues (6.59 per 1000 hospitalizations) followed by Hispanics (3.82 per 1000 hospitalizations). We further observed that Hispanic patients had the highest prevalence of obesity among those with SDOH issues (15.30 per 100 pregnancy hospitalizations with SDOH issues). Among hospitalizations with SDOH issues, NH-Whites had the lowest prevalence of obesity (10.01 per 100 pregnancy hospitalizations with SDOH issues) when compared to other racial/ethnic groups.
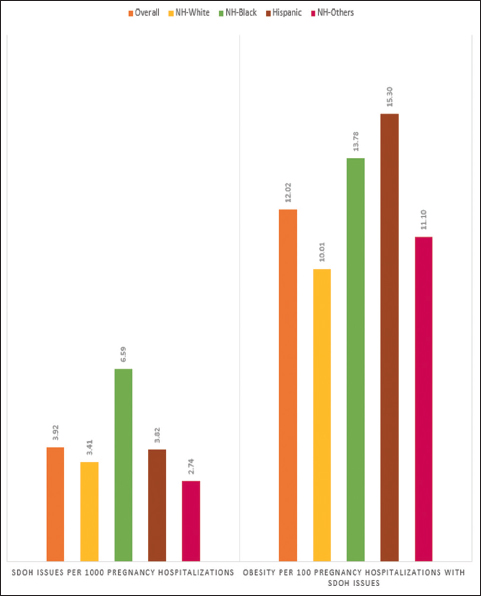
- Prevalence of SDOH issues in pregnancy hospitalizations and prevalence of obesity in pregnancy hospitalization with SDOH issues by race/ethnicity.
- For the left panel of the figure, prevalence of SDOH issues = hospitalizations with SDOH issues*1000/pregnancy-related hospitalizations.
- For the right panel of the figure, the prevalence of obesity = hospitalizations with obesity*100/pregnancy hospitalizations with SDOH issues
Table 2 highlights important associations between both SDOH issues and hospitalization characteristics as well as maternal obesity for pregnancy-related hospitalizations. Overall, when adjusted for covariates, we found that those experiencing SDOH issues had a 15% increased likelihood of experiencing maternal obesity as compared to those without SDOH issues (OR=1.15,95% CI=1.05-1.35). NH-Black patients were 1.56 times (95% CI: 1.50-1.61) as likely to experience SDOH issues when compared to the NH-Whites. We also noted that the likelihood of experiencing maternal obesity increased with age, with pregnancy-related hospitalizations in the 35-49 years group having a 34% (95% CI: 1.32-1.36) increased likelihood when compared to those less than 25 years. There was an inverse dose-response relationship between patients’ income and diagnosis of maternal obesity, with those from the highest quartile having the lowest likelihood of obesity (OR=0.64, 95% CI=0.61-0.66) and the risk increasing with decreasing income level. Those covered by Medicare and those admitted in hospitals in the West, in large and urban teaching hospitals were most likely to be obese.
| N=12,106,775 | ||
|---|---|---|
| OR (95% CI) | p-value | |
| SDOH issues | ||
| No | reference | |
| Yes | 1.15 (1.05-1.35) | <0.01 |
| Race/Ethnicity | ||
| NH-White | reference | |
| NH-Black | 1.56 (1.50-1.61) | <0.01 |
| Hispanic | 1.09 (1.05-1.15) | <0.01 |
| NH-Other | 0.69 (0.66-0.73) | <0.01 |
| Age | ||
| <25 years | reference | |
| 25-34 years | 1.03 (0.94-1.13) | 0.12 |
| 35-49 years | 1.34 (1.32-1.36) | <0.01 |
| Discharge Status | ||
| Routine | reference | |
| Transfer | 0.94 (0.87-1.00) | 0.05 |
| Died | 0.73 (0.48-1.11) | 0.14 |
| DAMA | 0.85 (0.79-0.91) | <0.01 |
| Other | 1.54 (1.43-1.65) | <0.01 |
| Zip Income quartile | ||
| Lowest quartile | reference | |
| 2nd quartile | 0.94 (0.92-0.97) | <0.01 |
| 3rd quartile | 0.89 (0.86-0.91) | <0.01 |
| Highest quartile | 0.64 (0.61-0.66) | <0.01 |
| Primary Payer | ||
| Medicare | reference | |
| Medicaid | 0.73 (0.69-0.77) | <0.01 |
| Private Insurance | 0.61 (0.58-0.65) | <0.01 |
| Self-Pay | 0.43 (0.40-0.46) | <0.01 |
| Hospital Characteristics | ||
| Hospital Region | ||
| Northeast | reference | |
| Midwest | 1.11 (1.02-1.20) | 0.03 |
| South | 1.07 (0.98-1.16) | 0.16 |
| West | 1.19 (1.09-1.29) | 0.13 |
| Hospital Bed Size | ||
| Small | reference | |
| Medium | 0.93 (0.87-0.99) | 0.02 |
| Large | 1.09 (1.03-1.16) | <0.01 |
| Hospital Location and Teaching Status | ||
| Rural | reference | |
| Urban non- teaching | 1.15 (1.07-1.23) | <0.01 |
| Urban teaching | 1.41 (1.33-1.50) | <0.01 |
Results obtained from survey logistic regression with SDOH issues as the exposure and maternal obesity as the outcome, while adjusting for covariates such as maternal age, race/ethnicity, discharge status, zip code income quartile, primary payer, hospital’s location, teaching status, region and bed size; SDOH - Social Determinants of Health NH – non-Hispanic; DAMA – discharged against medical advice
Supplemental Table 1 and Figure 2 show the relationship between SDOH issues and maternal obesity for those from various racial/ethnic groups. The Hispanic population had the highest likelihood (OR=1.45, 95% CI: 1.22-1.72) of maternal obesity if they had SDOH issues when compared to Hispanics without SDOH issues. NH-Others with SDOH issues had a 38% increased adjusted odds of obesity (95% CI: 1.09-1.75) when compared to NH-Others without SDOH issues. Conversely, hospitalizations for NH-White and NH-Black patients with SDOH issues had the same likelihood of obesity as compared to those without SDOH issues (i.e. p-value >0.05) within their respective racial/ethnic groups.
| Race/ethnicity | OR | Lower 95% CI | Upper 95% CI |
|---|---|---|---|
| NH-White | 0.99 | 0.85 | 1.14 |
| NH-Black | 0.9 | 0.87 | 1.13 |
| Hispanic | 1.45 | 1.22 | 1.72 |
| NH-Others | 1.38 | 1.09 | 1.75 |
Results obtained from stratified survey logistic regression models with SDOH issues as the exposure and maternal obesity as the outcome while adjusting for covariates such as maternal age, discharge status, zip code income quartile, primary payer, hospital’s location, teaching status, region, and bed size. Individual regression models were conducted for each racial/ethnic group. NH – non-Hispanic Total N=12,106,775
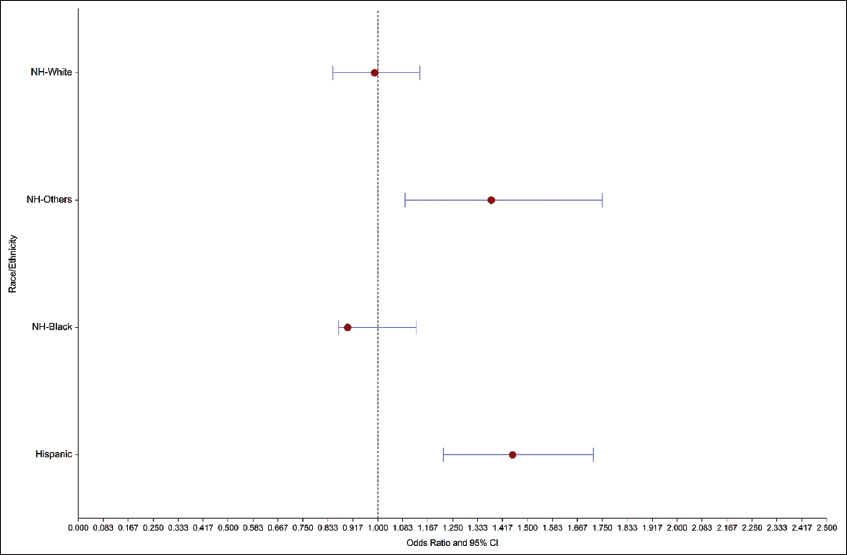
- Association between SDOH issues and maternal obesity among various racial/ethnic groups.
- Stratified survey logistic regression models to determine the association between SDOH issues (exposure) and obesity (outcome) were conducted for each racial/ethnic group separately. The covariates used for adjustment included maternal age, discharge status, zip code income quartile, primary payer, hospital’s location, teaching status, region, and bed size. Individual regression models were conducted for each racial/ethnic group. N=12,106,775
4. Discussion
Using a nationwide sample, our study examined the impact of SDOH issues on maternal obesity across various racial/ethnic groups in the United States. Similar to a previous study that reported an increased likelihood of maternal obesity in those with lower education and lower income level,14 we observed an overall increased likelihood of obesity in pregnant women with a diagnosis indicating SDOH issues, as well as for those in the lowest zip income quartile and those using Medicare or Medicaid as opposed to private insurance. We also found an increased prevalence of maternal obesity with increasing age.
It was previously reported that NH-Black and Hispanic adults had a higher age-adjusted prevalence of obesity than NH-Whites and NH-Asians.3 Our study findings revealed that across different racial/ethnic groups, the impact of SDOH issues on maternal obesity varied. We observed that pregnant Hispanic and NH-Other women with SDOH issues had a greater likelihood of maternal obesity than those without SDOH issues. However, contrary to what was reported previously,2 we witnessed that after adjusting for other patient characteristics, NH-Black and NH-White women with SDOH issues had similar odds of maternal obesity when compared to those without SDOH issues. When looking only at pregnant women with SDOH issues, we found Hispanic patients had the highest prevalence of obesity, followed by NH-Black patients.
There are a few limitations in this study. The NIS datasets are cross-sectional and lack patient identifiers that would facilitate the investigation of readmissions or repeat emergency department encounters. Since the study uses specific ICD-10 codes to identify patients with SDOH issues, patient hospitalizations that were not assigned an SDOH-related ICD-10 code (Z55-Z65) by a healthcare provider were not considered in this sample. The under-utilization of ICD-10 codes for patients with SDOH issues16 may impact the results, especially when comparing across different racial/ethnic groups. Furthermore, the study does not consider the association between SDOH issues and maternal obesity for patients who do not visit the hospital and instead rely on doula or midwife services during their pregnancy and postpartum care. A great strength of the study is the huge sample size, which makes the findings generalizable to the US population. Also, to our knowledge, this is the first-ever study to examine the association between maternal SDOH issues and obesity across various racial/ethnic groups in the pregnant hospitalized population in the US.
5. Conclusion and Global Health Implications
Overall, our study illustrated an association between maternal SDOH issues and obesity and that the impact of SDOH issues on the outcome of maternal obesity differed across racial/ethnic groups. Future research is needed to explain the varied influence of individual SDOH characteristics, such as income, education, living condition, etc., and to investigate the potential compounding effects of multiple SDOH issues on maternal obesity across racial/ethnic groups. We recommend that our study findings be considered in the design, adjustments, and monitoring of interventions and/or programs for the prevention and treatment of maternal obesity. Lastly, healthcare providers should consider pregnant women’s SDOH status when caring for women from diversified racial/ethnic subgroups.
Acknowledgments:
None.
Compliance with Ethical Standards
Conflicts of Interest: The authors declare no competing interests.
Financial Disclosure: Nothing to declare.
Funding/Support: There was no funding for this study.
Ethics Approval: Since the study was performed using de-identified publicly available data, the Institutional Review Board (approval ID H-36335) classified this study as exempt.
Disclaimer: None
References
- BMI Classification Percentile and Cut Off Points BMI Classification Percentile and Cut-Off Points. StatPearls Publishing LLC 2021
- [Google Scholar]
- Obesity and socioeconomic status in adults:United States 2005-2008. NCHS data briefs – no. 50 December 2010. Centers for Disease Control and Prevention. Page Last Reviewed November 6, 2015 https://www.cdc.gov/nchs/products/databriefs/db50.htm
- [Google Scholar]
- Centers for Disease Control and Prevention Published 2021 https://www.cdc.gov/obesity/data/adult.html
- Centers for Disease Control and Prevention Published 2021 https://www.cdc.gov/obesity/adult/causes.html
- Obesity:definition, comorbidities, causes, and burden. Am J Manag Care. 2016;22((7 Suppl)):176. doi:86672
- [Google Scholar]
- Causes of obesity. Abdom Imaging. 2012;37(5):730-732. doi:10.1007/s00261-012-9862-x
- [Google Scholar]
- Social determinants of health. Healthy People 2030 https://health.gov/healthypeople/objectives-and-data/social-determinants-health
- Obesity Epidemiology Worldwide. Gastroenterol Clin North Am. 2016;45(4):571-579. doi:S0889-8553(16)30069-3
- [Google Scholar]
- Mind the gap:race/ethnic and socioeconomic disparities in obesity. Curr Diab Rep. 2015;15(11):95-6. doi:10.1007/s11892-015-0666-6
- [Google Scholar]
- Maternal obesity and diabetes mellitus as risk factors for congenital heart disease in the offspring. J Am Heart Assoc. 2020;9((8)) doi:10.1161/JAHA.119.011541
- [Google Scholar]
- Effects of maternal obesity on placental function and fetal development. Reproduction. 2017;153(3):R97-R108. doi:10.1530/REP-16-0495
- [Google Scholar]
- Pre-eclampsia:pathogenesis, novel diagnostics and therapies. Nat Rev Nephrol. 2019;15(5):275-289. doi:10.1038/s41581-019-0119-6
- [Google Scholar]
- Adverse perinatal outcomes for obese women are influenced by the presence of comorbid diabetes and hypertensive disorders. Sci Rep. 2019;9(1):9793-8. doi:10.1038/s41598-019-46179-8
- [Google Scholar]
- Socio-economic indicators, dietary patterns, and physical activity as determinants of maternal obesity in middle-income countries:Evidences from a cohort study in Mexico. Int J Health Plann Manage. 2019;34((1)) doi:10.1002/hpm.2684
- [Google Scholar]
- Overview of the National Inpatient Sample (NIS) Agency for Healthcare Research and Quality 2012 www.hcup-us.ahrq.gov/nisoverview.jsp
- Z Codes utilization among medicare fee-for-service (FFS) beneficiaries in 2017. Centers for Medicare &Medicaid Services Office of Minority Health Published January 2020 https://www.cms.gov/files/document/cms-omh-january2020-zcode-data-highlightpdf.pdf
- [Google Scholar]





