Translate this page into:
Acceptance of Cervical Cancer Screening and its Correlates Among Women of a Peri-Urban High-Density Residential Area in Ndola, Zambia
*Corresponding author email: Chiluba.kabalika20@gmail.com
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Background:
Zambia has one of the highest cervical cancer incidence and mortality rates in the world. Cervical cancer screening leads to reduction in the incidence of invasive disease. The objectives of the study were to determine the level of acceptance of cervical cancer screening and its correlates among women of a peri-urban high-density residential area in Ndola, Zambia.
Methods:
A cross sectional study was conducted. With a population size of 12,000 women in reproductive age and using an expected frequency of 50 + 5% and at 95% confidence interval, the required sample size was 372. A stratified sampling method was used to select participants. Independent factors that were associated with the outcome were established using multi-variate logistic regression. Adjusted odds ratios and their 95% confidence intervals are reported.
Results:
In total, 355 out of 372 questionnaires were administered, achieving a response rate of 95.4%. Out of 355 participants, 9 (2.5%) had ever been screened for cervical cancer. In bivariate analyses, factors associated with screened were knowledge of body part affected, screening as a prevention tool, whether cervical cancer was curable in its early stages or not, awareness of cervical cancer screening, knowledge on frequency of screening and cervical cancer screening causing harm. However, in multivariate analysis, participants who knew that cervical cancer screening prevented cervical cancer were 3.58 (95% CI [1.49, 8.64]) times more likely to have been screened than those who did not have the knowledge. Participants who knew that cervical cancer is curable were 2.76 (95% CI [1.92, 8.31]) times more likely to have been screened than those who did not have the knowledge.
Conclusion and Global Health Implications:
The uptake of screening was low. Interventions should be designed to increase uptake of screening for cervical cancer by considering factors that have been identified in the current study that are independently associated with cervical cancer screening among this population.
Keywords
Knowledge
Cervical Cancer
Pap Smear
Screening
Zambia
1. Introduction
Cervical cancer is the second-most common cancer among women globally.1 At least 3 in 4 cases of cervical cancer per year globally occur in developing countries.2 Zambia has one of the highest incidence and mortality rates of cervical cancer in the world.3,4 Among the cancers reported among females to the Zambia National Cancer Registry between 1990 and 2009, cervical cancer was the most common (48.5%).5 Bowa et al3 also reported that cervical cancer was the most common cancer among women. In 2008, Zambia had an age-adjusted incidence rate of 52.8 per 100,000 World Standard Population.6 Although Pap smear combined with treatment of cervical precancerous and early stage cancer can prevent up to 80% of invasive cervical cancer cases in developed countries,7 high rates of mortality due to cervical cancer persist in developing countries because of low rates of cervical cancer screening.8 Evidence suggests that Pap smear screening is associated with 70% lower odds of cervical cancer among women who undergo the Pap smear test compared to women who do not take the test.9 The uptake of cervical cancer screening has varied between countries (from 12.3% in Kenya,10 14.7% in Ethiopia,11 22.6% in Tanzania,12 to 37% in Botswana); and within country (from 4.2% in South eastern part of Nigeria13 to 10.2% in North central of Nigeria); In a study conducted in Zambia none of the participants reported ever having done a pap smear.15 Women in the age group 21-65 years may be screened for cervical cancer using cytology (Pap smear) every three years and for women in the age group 30-65 years may be screened using cytology and human papillomavirus testing every five years.16
Age, education, contraception use and being married have been associated with cervical cancer screening.17-22 Reasons for not screening include perception of not being at risk and fear that abnormal test results mean existing cancer.10,23-25 Other factors associated with undergoing cervical cancer screening include: women’s perceptions of the cervical cancer screening, awareness of factors associated with cervical cancer, having financial resources and support from the spouse.20-22,24,26 Accessibility, costs, waiting time, and quality of services serve as major barriers to routine screening.27,28 The discomfort associated with the procedure and mistrust of health providers to keep confidentiality can also affect screening behavior.29 Furthermore, characteristics of health providers, such as negative attitudes or a lack of suggesting that a woman obtain a Pap smear, have also been correlated with cervical cancer screening.25,30 Because of the variations in study designs,31,32 study populations and levels of acceptance of cervical cancer screening within countries and that no similar study has been carried out in the Northern part of Zambia, a study was conducted to determine the level of acceptance of cervical cancer screening and its correlates among women of a peri-urban high-density residential area in Ndola, Zambia.
2. Methods
A cross sectional study was conducted in Chipulukusu, Ndola, Zambia, during the month of July 2015. Chipulukusu is a peri-urban community in Ndola which is the capital of the Copperbelt province, one of the 10 provinces in Zambia. According to a 2015 local clinic census, Chipulukusu had a total population of 41,837 with 12,000 women in reproductive age. The socio-economic status of Chipulukusu was low, with most of the adult population employed as maids and Garden boys or self-employed (carrying out small businesses at home). The majority of the women in Chipulukusu were housewives and the level of education attained was low, with most of the women ending their education at primary level.
The Statcalc program in Epi Info version 6 [33] was used to determine sample size, considering population size of 12,000, expected frequency of 50+ 5% (screening rate unknown in the population) and 95% confidence level, the required sample size was 372.
During this study, a stratified sampling method was used to select participants. Chipulukusu is divided into 9 zones with no significant political or economic differences between the zones. Five zones were picked out at random and households were randomly selected from each of these zones. Seventy one questionnaires were administered to willing women between the ages of 21 and 65 in each of the five selected zones. A semi structured questionnaire that contained 37 questions elicited information on respondent’s bio data, knowledge about cervical cancer and screening, and participation in screening. It also sought information about attitudes towards screening and perception of own risk of getting cervical cancer, and accessibility factors regarding screening centers. The questionnaire was administered through a one-on-one interview with participants. This was the most effective method to obtain data because most participants were unable to read or write.
Data entry was done using Epi data version 3.1 and analysed using Statistical Package for Social Sciences (SPSS) version 16.0.34 The Chi square test was used to establish associations between exposure factors and the outcome at 5% significance level. Independent factors that were associated with the outcome were established using a multi-variate logistic regression analysis. Adjusted odds ratios and their 95% confidence intervals are reported. The Department of Clinical Sciences of the Copperbelt University School of Medicine approved the study protocol. Permission was granted by the District Health Office to conduct the study. Before administering the questionnaire, consent was sought from the participants. The participants were informed that participation was voluntary and that if they so wished they may not participate in the study with no consequences for non-participation. Furthermore participants were informed that they could stop the interview at any time without repercussions. The questionnaires were anonymous.
3. Results
A total of 355 out of 372 questionnaires were administered, achieving a response rate 95.4%. Table 1 shows the demographic characteristics of the study participants. The proportion of respondents with lower levels of education was significantly higher in the age group 30 years or older compared to those below 30 years (p <0.001). However, more participants aged 30 years or older were employed compared to those below 30 years (p <0.001). Among those aged less than 30, 21.8% were single women compared to 2.4% in those aged 30 years or more. Majority of respondents above aged 30 years or older had more than five children (52.4%) compared to 5.4% in the less than 30 years age group. Significantly more persons in the age group of 30 years and above (20.2%), than in the less than 30 age group (10.9%) used tobacco. Most of the participants used contraceptives (69.3%) and were non-Catholics including Pentecostal, Seventh Day Adventist and Muslim (78.6%) with no significant difference between age groups. Overall, nine (2.5%) of the participants had ever been screened for cervical cancer.
| Factor | Total n (%) | Age (years) | p-value | |
|---|---|---|---|---|
| < 30 n (%) | 30+ n (%) | |||
| Level of education | ||||
| None | 44 (12.4) | 7 (4.8) | 37 (17.8) | < 0.001 |
| Primary | 185 (52.1) | 59 (40.1) | 126 (60.6) | |
| Basic | 79 (22.3) | 43 (29.3) | 36 (17.3) | |
| Secondary | 47 (13.2) | 38 (25.9) | 9 (4.3) | |
| Employment | ||||
| Employed | 37 (10.4) | 12 (8.2) | 25 (12.8) | <0.001 |
| Selfemployed | 113 (31.8) | 28 (19.0) | 85 (40.9) | |
| House wife | 150 (42.3) | 74 (50.3) | 76 (36.5) | |
| Unemployed | 55 (15.5) | 33 (22.4) | 22 (10.6) | |
| Marital status | ||||
| Single | 37 (10.4) | 32 (21.8) | 5 (2.4) | < 0.001 |
| Married | 253 (71.3) | 106 (72.1) | 147 (70.7) | |
| Separated/divorced | 30 (8.5) | 8 (5.4) | 22 (10.6) | |
| Widowed | 35 (9.9) | 1 (0.7) | 34 (16.3) | |
| Number of children | ||||
| 0 | 30 (8.5) | 21 (14.3) | 9 (4.3) | < 0.001 |
| 1-5 | 208 (58.6) | 118 (80.3) | 90 (43.3) | |
| 5+ | 117 (33.0) | 8 (5.4) | 109 (52.4) | |
| Religion | ||||
| Catholic | 76 (21.4) | 26 (17.7) | 50 (24.0) | 0.151 |
| Non-Catholic | 279 (78.6) | 121 (82.3) | 158 (76>0) | |
| Tobacco use | ||||
| Yes | 58 (16.3) | 16 (10.9) | 42 (20.2) | 0.019 |
| No | 279 (83.7) | 131 (89.1) | 166 (79.8) | |
| Contraceptive use | ||||
| Yes | 246 (69.3) | 108 (73.5) | 138 (66.3) | 0.152 |
| No | 109 (30.7) | 39 (26.5) | 70 (33.7) | |
| Ever screened | ||||
| Yes | 9 (2.5) | 3 (2.0) | 6 (2.9) | 0.741 |
| No | 346 (97.5) | 144 (98.0) | 202 (97.1) | |
Table 2 shows that there were no significant associations between the demographic, contraceptive use, and tobacco use factors of participants on one hand and uptake of cervical cancer screening. on the other, except for knowledge about Cancer of the cervix (p<0.001). Table 3 highlights associations between knowledge of cervical cancer and cervical cancer screening uptake. The only significant associations observed were screening as a prevention tool, and whether cervical cancer was curable in its early stages or not on one hand with uptake with screening on the other. Significantly more participants who had knowledge of cervical cancer being curable in early stages (17.4%) were observed to have screened compared to 2.3% among those that did not (p=0.030). A significantly higher proportion of the participants who believed that screening can prevent cervical cancer (50%) had been screened compared to 6.1% in the group that did not (p =0.003).
| Factor | Total n (%) | Screened | p-value | |
|---|---|---|---|---|
| Yes n (%) | No n (%) | |||
| Age (years) | ||||
| < 30 | 41 (100) | 3 (7.3) | 38 (92.7) | 0.502 |
| ≥ 30 | 49 (100) | 6 (12.2) | 43 (87.8) | |
| Education | ||||
| None/primary | 47 (100) | 3 (6.4) | 44 (93.6) | 0.301 |
| Basic/secondary | 43 (100) | 6 (14.0) | 37 (86.0) | |
| Employment | ||||
| Employed/selfemployed | 34 (100) | 5 (14.7) | 29 (85.3) | 0.290 |
| House wife/unemployed | 56 (100) | 4 (7.1) | 52 (92.9) | |
| Marital status | ||||
| Married | 65 (100) | 7 (10.8) | 58 (89.2) | 1.000 |
| Separated/divorced/ widowed/single | 25 (100) | 2 (8.0) | 23 (92.0) | |
| Number of children | ||||
| 0 | 5 (100) | 0 (0) | 5 (100) | 1.000 |
| 1+ | 85 (100) | 9 (10.6) | 76 (89.4) | |
| Religion | ||||
| Catholic | 12 (100) | 1 (8.3) | 11 (91.7) | 1.000 |
| NonCatholic | 78 (100) | 8 (10.3) | 70 (89.7) | |
| Tobacco use | ||||
| Yes | 9 (100) | 1 (11.1) | 8 (88.9) | 1.000 |
| No | 81 (100) | 8 (9.9) | 73 (90.1) | |
| Contraceptive use | ||||
| Yes | 69 (100) | 8 (11.6) | 61 (88.4) | 0.679 |
| No | 21 (100) | 1 (4.8) | 20 (95.2) | |
| Knowledge about cervical cancer | ||||
| Yes | 90 (100) | 9 (10.0) | 81 (90.0) | <0.001 |
| No | 265 (100) | 0 (0) | 265 (100) | |
As outlined in Figure 1, awareness of cervical cancer screening and knowledge on frequency of screening were significantly associated with uptake of cervical cancer screening (p =0.027). A higher proportion of participants who were aware of the above-mentioned factors had been screened (15.0%) compared to those who were not (0%) Table 4 shows associations between attitudes and perception of own risk on one hand and uptake of cervical cancer screening on the other. The only significant finding was the association between cervical cancer screening causing harm and uptake of screening (p =0.007). A higher proportion (25.7%) of those who believed screening caused no harm had screened compared to 0% of those who did not. The accessibility factors outlined in Figure 2 were not significantly associated with uptake of screening. In multivariate analysis, those who believed that cervical cancer screening prevented cervical cancer were 3.58 (95% CI 1.49, 8.64) times more likely to have been screened than those who did not. Participants who believed cervical cancer to be curable were 2.76 (95% CI 1.92, 8.31) times more likely to have been screened than those who did not.
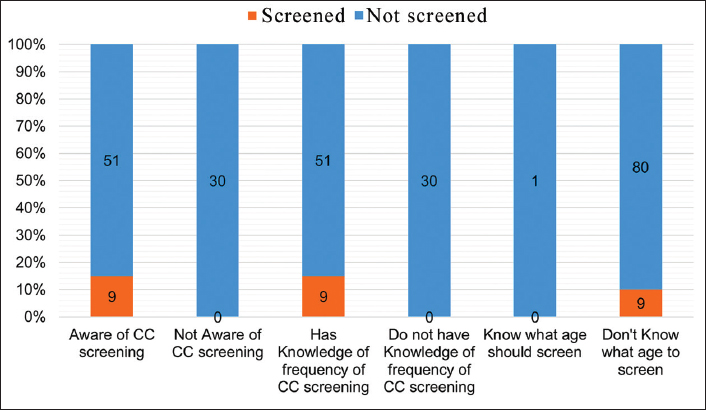
- Knowledge on screening associated with uptake of cervical cancer screening
| Factor | Total n (%) | Screened | p-value | |
|---|---|---|---|---|
| Yes n (%) | No n (%) | |||
| Learnt about cervical cancer through: | ||||
| News/media | ||||
| Yes | 22 (100) | 2 (9.1) | 20 (90.9) | 1.000 |
| No | 68 (100) | 7 (10.3) | 61 (89.7) | |
| Brochures/posters/other printed material | ||||
| Yes | 3 (100) | 0 (0) | 3 (100) | 1.000 |
| No | 87 (100) | 9 (10.3) | 78 (89.7) | |
| Health worker | ||||
| Yes | 50 (100) | 6 (12.0) | 44 (88.0) | 0.726 |
| No | 40 (100) | 3 (7.5) | 37 (92.5) | |
| Family/friends/neighbours/colleagues | ||||
| Yes | 14 (100) | 1 (7.1) | 13 (92.9) | 1.000 |
| No | 76 (100) | 9 (11.8) | 67 (88.2) | |
| Teachers | ||||
| Yes | 1 (100) | 0 (0) | 1 (100) | 1.000 |
| No | 89 (100) | 9 (10.1) | 80 (89.9) | |
| Knowledge of symptoms of cervical cancer: | ||||
| Vaginal bleeding | ||||
| Yes | 2 (100) | 0 (0) | 2 (100) | 1.000 |
| No | 88 (100) | 9 (10.2) | 79 (89.8) | |
| Vaginal discharge (foul smelling) | ||||
| Yes | 3 (100) | 1 (33.3) | 2 (66.7) | 0.274 |
| No | 87 (100) | 8 (9.2) | 79 (90.8) | |
| Cause of cervical cancer | ||||
| Do not know | 90 (100) | 9 (10.0) | 81 (90.0) | |
| Risk factors: | ||||
| Multiple sexual partners | ||||
| Yes | 9 (100) | 2 (22.2) | 7 (77.8) | 0.221 |
| No | 81 (100) | 7 (8.6) | 74 (91.4) | |
| Cigarette smoking | ||||
| Yes | 1 (100) | 0 (0) | 1 (100) | 1.000 |
| No | 89 (100) | 9 (10.1) | 80 (89.9) | |
| Prevention of cervical cancer: | ||||
| Avoid multiple sex partners | ||||
| Yes | 8 (100) | 2 (25.0) | 6 (75.0) | 0.181 |
| No | 82 (100) | 7 (8.5) | 75 (91.5) | |
| Quit smoking | ||||
| Yes | 2 (100) | 0 (0) | 2 (100) | 1.000 |
| No | 88 (100) | 9 (10.2) | 79 (89.8) | |
| Regular screening | ||||
| Yes | 8 (100) | 4 (50.0) | 4 (50.0) | 0.003 |
| No | 82 (100) | 5 (6.1) | 77 (93.9) | |
| Curable in early stages | ||||
| Yes | 46 (100) | 8 (17.4) | 38 (82.6) | 0.030 |
| No | 44 (100) | 1 (2.3) | 43 (97.7) | |
| Treatment: | ||||
| Surgery | ||||
| Yes | 7 (100) | 2 (28.6) | 5 (71.4) | 0.144 |
| No | 83 (100) | 7 (8.4) | 76 (91.6) | |
| Specific drugs (hospital) | ||||
| Yes | 29 (100) | 1 (3.4) | 28 (96.6) | 0.262 |
| No | 61 (100) | 8 (13.1) | 53 (86.9) | |
| Factor | Total n (%) | Screened | p-value | |
|---|---|---|---|---|
| Yes n (%) | No n (%) | |||
| Cervical cancer highly preventive common cause of death | ||||
| Agree | 33 (100) | 7 (21.2) | 26 (78.8) | 0.160 |
| Disagree | 27 (100) | 2 (7.4) | 25 (92.6) | |
| Any woman can get cervical cancer including you | ||||
| Agree | 54 (100) | 9 (16.7) | 45 (83.3) | 0.578 |
| Disagree | 6 (100) | 0 (0) | 6 (100) | |
| Screening helps prevent cervical cancer | ||||
| Agree | 56 (100) | 8 (14.3) | 48 (85.7) | 0.488 |
| Disagree | 4 (100) | 1 (25.0) | 3 (75.0) | |
| Sreening process not painful | ||||
| Agree | 25 (100) | 6 (24.0) | 19 (76.0) | 0.145 |
| Disagree | 35 (100) | 3 (8.6) | 32 (91.4) | |
| Screening causes no harm | ||||
| Agree | 35 (100) | 9 (25.7) | 26 (74.3) | 0.007 |
| Disagree | 25 (100) | 0 (0) | 25 (100) | |
| Screening is not expensive | ||||
| Agree | 46 (100) | 9 (19.6) | 37 (80.4) | 0.100 |
| Disagree | 14 (100) | 0 (0) | 14 (100) | |
| Will you screen if causes no harm/not expensive? | ||||
| Agree | 57 (100) | 9 (15.8) | 48 (84.2) | 1.000 |
| Disagree | 3 (100) | 0 (0) | 3 (100) | |
| Screening process is embarrassing | ||||
| Agree | 32 (100) | 5 (15.6) | 27 (84.4) | 1.000 |
| Disagree | 28 (100) | 4 (14.3) | 24 (85.7) | |
| Preferred sex of health practitioner | ||||
| Female | 31 (100) | 5 (16.1) | 26 (83.9) | 1.000 |
| Any sex | 29 (100) | 4 (13.8) | 25 (86.2) | |
| If preferred health practioners not available | ||||
| Undergo screening with available practitioners | 22 (100) | 5 (22.7) | 17 (77.3) | 0.286 |
| Go home | 9 (100) | 0 (0) | 9 (100) | |
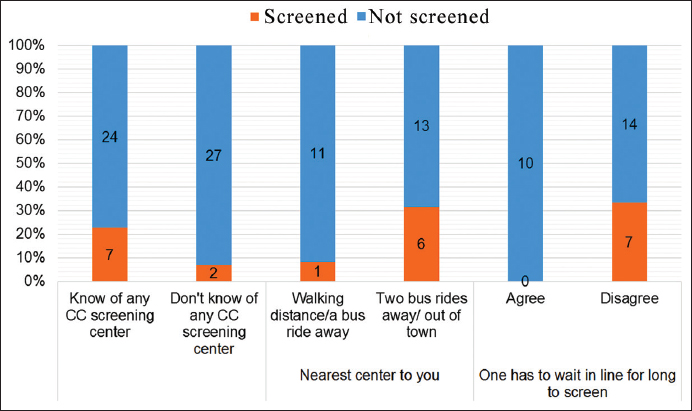
- Accessibility factors associated with cervical cancer screening
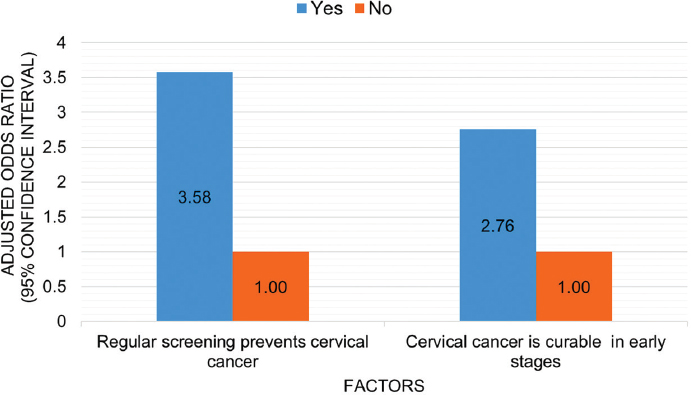
- Independent factors associated with cervical cancer screening
4. Discussion
Several significant findings are revealed in this study. First, 2.5% of women in this peri-urban community of Zambia had ever screened for cervical cancer. This proportion is much lower than what was expected considering the launching of the government’s campaign for cervical cancer in 2006 and the fact that it was offered free of charge in some government institutions in Zambia. This proportion is also much lower than what has been observed in studies done in other African countries where at least more than 10% of the respondents had been screened.1,10-12 These differences can be attributed to variations in study populations in terms of socio-economic status.6 The uptake of cervical cancer screening in a study done in another part of Zambia in a similar population in 2013 was found to be much lower at 0%.15 This could be a result of the time differences in which the studies were conducted or may be an indication of the different variations within the country.
There was a positive association between knowledge that regular screening prevents cervical cancer and uptake of screening. Participants who agreed that regular screening prevents cancer were more likely to have been screened than those who did not. This, however, is contradicted in a study done in Botswana that found no significant association between perceived benefits of screening and cervical cancer screening.1 A statistically significant relationship was observed between knowledge that cervical cancer is curable in early stages and uptake of cervical cancer screening in the current study. This association is echoed in studies done in Nigeria14 and Ethiopia11 that found that the belief that cervical cancer may not be cured and hinder uptake of the screening test. Another study done in Botswana indicated that although cervical cancer was perceived as a serious disease by most participants, believing that there was no treatment for cervical cancer made them not to undergo screening for the disease.1
4.1. Limitations of the Study
The study was not powered to determine associations due to the small number of persons who had been screened. Hence, it is possible that some factors that could have been associated with screening were not established. A case control study is recommended to establish if there are more factors associated with screening.
5. Conclusion and Global Health Implications
Uptake of screening was low in the population where the current study was conducted. Health education interventions considering factors that have been identified to be associated with uptake of cervical cancer in the current study may help to increase the uptake of screening for cervical cancer.
Acknowledgements
We are grateful to the women that participated on the survey. We would like to thank Chipulukusu Clinic stuff for their assistance in divulging information used in the sample size calculation.
Ethics Approval: This study was approved by an Institutional Review Board.
Conflict of Interest: None.
References
- Perceived Benefits of Cervical Cancer Screening among Women Attending Mahalapye District Hospital, Botswana. Asian Pacific Journal of Cancer Prevention. 2010;11(4):1021-1027.
- [Google Scholar]
- World Health Organization. Global burden of disease report:Causes of death in 2004. Global Burden of Disease Report. Geneva: World Health Organization; 2004.
- A review of the epidemiology of cancers at the University Teaching Hospital, Lusaka, Zambia. Tropical Doctor. 2009;39(1):5-7.
- [Google Scholar]
- Pattern of adult malignancies in Zambia (1980–1989) in light of the human immunodeficiency virus type 1 epidemic. Journal of Tropical Medicine and Hygiene. 1995;98(4):281-284.
- [Google Scholar]
- Distribution of cancers in Zambia:Evidence from the Zambia National Cancer Registry (1990–2009) Journal of Public Health and Epidemiology. 2013;5(2):95-100.
- [Google Scholar]
- Global inequalities in cervical cancer incidence and mortality are linked to deprivation, low socioeconomic status, and human development. International Journal of MCH and AIDS. 2012;1(1):17-30.
- [Google Scholar]
- Knowledge and practice about cervical cancer and Pap smear testing among patients at Kenyatta National Hospital, Nairobi, Kenya. International Journal of Gynecological Cancer. 2003;13(6):827-833.
- [Google Scholar]
- Limited Pap screening associated with reduced risk of cervical cancer in South Africa. International Journal of Epidemiology. 2003;32(4):573-577.
- [Google Scholar]
- Perceptions of risk and barriers to cervical cancer screening at Moi Teaching and Referral Hospital (MTRH), Eldoret, Kenya. African Health Sciences. 2011;11(1):58-64.
- [Google Scholar]
- Comprehensive knowledge about cervical cancer is low among women in Northwest Ethiopia. BMC Cancer. 2013;13:2.
- [Google Scholar]
- Demographic, knowledge, attitudinal, and accessibility factors associated with uptake of cervical cancer screening among women in a rural district of Tanzania:Three public policy implications. BMC Public Health. 2012;12:22.
- [Google Scholar]
- Knowledge attitudes and practices of cervical cancer screening among urban and rural Nigerian women:a call for education and mass screening. European Journal of Cancer Care (Engl). 2011;20(3):362-367.
- [Google Scholar]
- Cervical Cancer and Pap Smear Awareness and Utilization of Pap Smear Test among Federal Civil Servants in North Central Nigeria. PloS ONE. 2012;7(10):e46583.
- [Google Scholar]
- Cervical Cancer Awareness and uptake of Pap-Smear Services among Women above 18 years of Age. Medical Journal of Zambia. 2013;40(1):19-23.
- [Google Scholar]
- US Preventive Services Task force. Final Recommendation Statement. Cervical Cancer:Screening. Retrieved March 30, 2018 from https://www.uspreventiveservicestaskforce.org/Page/Document/RecommendationStatementFinal/cervical-cancer-screening
- Determinants of women's participation in cervical cancer screening trial, Maharashtra, India. Bulletin of the World Health Organization. 2007;85(4):264-272.
- [Google Scholar]
- Knowledge attitude and practice of cervical cancer screening among sexually active women in Onitsha, southeast Nigeria. Nigerian Journal of Medicine. 2009;18(4):384-387.
- [Google Scholar]
- Factors associated with awareness and knowledge of cervical cancer in a community:implication for health education programmes in developing countries. Journal of the Royal Society of Health. 1993;113(4):184-186.
- [Google Scholar]
- An ethnographic study of cervical cancer among women in rural Kenya:is there a folk causal model? International Journal of Gynecological Cancer. 2005;15(6):1049-1059.
- [Google Scholar]
- Women's perceptions and social barriers determine compliance to cervical screening:results from a population based study in India. Cancer Detection and Prevention. 2006;30(4):369-374.
- [Google Scholar]
- Cervical screening:Perceptions and barriers to uptake among Somali women in Camden. Public Health. 2009;123(10):680-685.
- [Google Scholar]
- Knowledge, attitudes and practices on cervical cancer screening among the medical workers of Mulago Hospital, Uganda. BMC Medical Education. 2006;6:13.
- [Google Scholar]
- Women's participation in a cervical cancer screening program in northern Peru. Health Education Research. 2008;23(1):10-24.
- [Google Scholar]
- Knowledge, attitudes and practices of rural women in South Africa regarding the Pap smear. International Journal of Gynecology & Obstetrics. 2003;83(3):315-316.
- [Google Scholar]
- Pap screening and knowledge of risk factors for cervical cancer in Chinese women in British Columbia, Canada. Ethnicity & Health. 2004;9(3):267-281.
- [Google Scholar]
- Cervical cancer knowledge and screening in Accra, Ghana. Journal of Women's Health and Gender-based Medicine. 2002;11(6):487-488.
- [Google Scholar]
- Use of Pap test among Hispanics and non-Hispanic whites in a rural setting. Preventive Medicine. 2004;38(6):713-722.
- [Google Scholar]
- Factors that influence cancer screening in older African American men and women:focus group findings. Family and Community Health. 2001;24(3):27-33.
- [Google Scholar]
- Cervical cancer and Pap smear screening in Botswana:knowledge and perceptions. International Nursing Review. 2003;50(3):167-175.
- [Google Scholar]
- Utilization of cervical cancer screening services and trends in screening positivity rates in a 'Screen-And-Treat'program integrated with HIV/AIDS care in Zambia. PLoS ONE. 2013;8(9):e74607.
- [Google Scholar]
- Implementation of cervical cancer prevention services for HIV-infected women in Zambia:measuring program effectiveness. HIV Therapy. 2010;4(6):713-722.
- [Google Scholar]
- Epi Info, Version 6:a word processing, database, and statistics program for public health on IBM compatible microcomputers. Atlanta, Georgia, U.S.A: Centers for Disease Control and Prevention; 1996.
- SPSS for Windows, Version 16.0. Chicago: SPSS Inc; 2007.





