Translate this page into:
Caffeine Intake During Pregnancy and Risk of Childhood Obesity: A Systematic Review
*Corresponding author email: kim7y@cmich.edu
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Objective:
This paper evaluates the association between caffeine consumption during pregnancy and overweight or obesity in the offspring.
Methods:
Following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines, a literature search was conducted using MedLine, PubMed, CINAHL-Plus and Google Scholar databases. Inclusion criteria were cohort studies on participants with live singleton births at ≥28 weeks gestation who had consumed caffeine during pregnancy. Included were studies reporting both measurement of maternal caffeine intake and offspring anthropometric measurements. Studies reporting serum paraxanthine, a measurement of caffeine intake, were also included.
Results:
After final elimination, there were eight studies meeting our inclusion criteria. From these studies, we deduced that caffeine intake during pregnancy between 50 mg and <150 mg/day was associated with increased risk of overweight and obesity by excess fat deposition or increased weight, and elevated BMI per International Obesity Task Force (IOTF) criteria using a reference population. The majority of studies reported the strongest association with maternal caffeine intake during pregnancy and overweight and obesity risk beginning at ≥300 mg/day.
Conclusions and Global Health Implication:
The risk of childhood overweight or obesity was associated with caffeine consumption at 50 mg/day during pregnancy with a stronger association at intakes ≥300 mg/day and higher. The current recommendation of <200 mg/day of caffeine during pregnancy is likely associated with lower risk of overweight or obesity in offspring but avoidance of the substance is recommended.
Keywords
Prenatal
Caffeine intake
Pregnancy
Childhood
Obesity
Overweight
Serum paraxanthine
Systematic review
1. Introduction
Starting in the 1980’s until 2004, the prevalence of childhood obesity in the United States was increasing at a rate of 0.4-0.7 percent points per year. By 2016, approximately 13.7 million children in the United States were classified as obese.1 Overweight or obese children have a 70% chance of being overweight or obese in adulthood2 along with higher risk for chronic diseases such as cardiovascular disease, cancer, or diabetes.3,4-7 This trend of growing obesity initiated the need for interventions such as food assistance programs and nutrition education which have led to some improvement3 however a large majority of Americans remain obese.
In children, body mass index (BMI)-for-age can serve as an indicator of health risks and uses a reference population to compare results.1 BMI-for-age does not measure body fat, and the numbers are adjusted for age and gender. The child’s height and weight are entered in the U.S. Centers for Disease Control and Prevention’s (CDC) growth charts. Children at or above the 85th percentile but less than 95th percentile are classified as overweight while those at or above the 95th percentile are classified as obese.2,8 Another measurement of childhood overweight and obesity involves cut-off points as designated by the International Obesity Task Force (IOTF). The IOTF links BMI at the age of 18 to child centiles based on data from six countries. This data does not translate into percentiles as with the CDC guidelines.9
If a child is obese by the age of 11 they are more likely to be obese in adulthood.5 The etiology behind childhood obesity is multifactorial with both genetic and environmental considerations. Specifically, for pediatrics, a more genetic component is thought to be at play involving DNA changes that occur as the fetus is developing or hormone alterations.2,7 During pregnancy, hormones change how caffeine metabolizing enzymes function.10,11 Due to the decreased enzyme function, caffeine ingestion during pregnancy may allow for the fetus to be exposed to glucocorticoids that the mother produces.11 These glucocorticoids potentially interrupt the development of the hypothalamic-pituitary-adrenal axis (HPA-axis), which is suggested to be the primary place of genetic changes to predispose the fetus to metabolic syndrome.11 Aside from genetic components, obesity for both children and adults can be a result of excess caloric intake or lack of physical activity.2,7
Maternal obesity prior to pregnancy or the development of gestational diabetes during pregnancy has been associated with offspring that have a high fat mass when compared to lean muscle mass.12 This disproportion in overall mass can predispose them to adult onset diseases indicating that a mother’s diet both during pregnancy and before pregnancy can affect the health of the child.12 Caffeine intake during pregnancy has been associated with unproportioned fat deposition such as abdominal subcutaneous fat,13 increased waist circumference,14 increased liver fat fraction,13 or increase in overall weight gain15 of the child.
1.2. Objectives of the Study
Research is inconclusive on whether appropriate caffeine intake can be included in the diet during pregnancy.14 Caffeine consumption of <400 mg per day outside of pregnancy has not been associated with negative health effects.16-18 In the U.S., a large prospective cohort study approximated that 75% of women consume caffeine during pregnancy.19 According to the American College of Obstetricians and Gynecologists (ACOG), <200 mg/day of caffeine is recommended20 but the World Health Organization (WHO) allows for <300 mg/day while pregnant.21 A typical 8oz cup of brewed coffee is approximately 137 mg of caffeine.20 The ACOG recommendation comes from an evaluation completed on large cohort populations that found no consistent risk of miscarriage, preterm birth, or intrauterine growth restriction associated with caffeine intakes <200 mg/day.20 Intakes of caffeine >200 mg/day have been associated with low birth weight, miscarriage, and small for gestation age (SGA) at birth.6,15,19,22,23 Evaluation of caffeine intake during pregnancy in relation to risk of childhood obesity was not considered while determining a recommendation for caffeine. Therefore, the objective of this systematic review was to determine if there is a specific amount of caffeine intake during pregnancy that is associated with childhood overweight or obesity as demonstrated in published literature.
1.3. Specific Aims and Hypothesis
Cohort studies indicate that maternal caffeine intake during pregnancy is associated with childhood overweight or obesity.13-15,22,24 Li et al.,24 found an 87% risk of obesity in the child when a mother consumed caffeine during pregnancy. Overweight status at ages six through 10 years old has also been associated with a mother’s caffeine consumption during pregnancy.13-15,22 The purpose of this systematic review was to summarize the current research that addresses an association between maternal caffeine consumption and risk of childhood overweight or obesity.
2. Methods
Using Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines, 25 a systematic literature review was conducted (Figure 1). The search strategy included utilizing several databases to identify peer-reviewed journal articles. Databases searched included Medline, PubMed, CINAHL- Plus and Google Scholar. Key words included in the search were “prenatal,” “caffeine,” “pregnancy,” “childhood,” “overweight,” “obesity,” and “serum paraxanthine.” By using these key words and finding articles to be included, reference list from these articles provided other studies that were available. Reviews were conducted and data were gathered in January 2020.

- PRISMA flow diagram
2.1. Study Variables
Eligible studies included original articles. The study must have been available in English language with no restriction on the year of publication, as literature for this review was scarce. Included studies were prospective cohort populations with women who were pregnant ≥28 weeks with singleton live births. This ensured a level of uniformity while comparing literature throughout the review and helped to provide enough information from each cohort to evaluate the possibility of a significant association. We included only singleton births thus likely eliminating high risk pregnancy as a potential confounder. The elements of each study had to contain mothers that consumed caffeine during pregnancy, offspring with anthropometric measurements available, and measured caffeine intake from the mother during pregnancy to be included. No age limit for the mothers was set in these studies. Given that serum paraxanthine is a metabolite of caffeine that was used to identify maternal caffeine intake during pregnancy with childhood overweight or obesity outcomes, this measurement of caffeine was also included in the review. These criteria allowed for the review to have adequate evidence to compare results and identify an association.
Excluded studies were those with insufficient evidence such as missing childhood measurements, no caffeine measurements from mothers during pregnancy, and no protocol to evaluate caffeine measurements. As there have been other associations suggested with prenatal caffeine exposure and childhood outcomes, those articles that focused on outcomes other than childhood obesity, overweight, anthropometric measurements, or fat deposition were excluded.
The primary outcome was the association of maternal caffeine intake during pregnancy and childhood obesity status. Secondary outcomes include maternal caffeine intake and overweight status in childhood, altered fat deposition, or altered childhood anthropometrics causing similar health risk factors to obesity. For the selected studies, data were extracted including childhood overweight status, obesity, childhood fat deposition, or childhood anthropometrics with measurements and definitions. Demographics of the mothers and the source and amount of caffeine mothers consumed during pregnancy were evaluated. Study characteristics including place, time, and size of cohort were considered. Assumptions included basic knowledge of BMI and the association of altered fat deposition, and anthropometrics including skinfold measurements with childhood obesity or overweight status.
Risk of bias was assessed using the Newcastle-Ottawa scale for case control and cohort studies to determine the level of significance in regards to the data presented.26 The scale was used to evaluate selection bias, comparability bias, and outcome bias for each study by using eight categories. Once the assessment was completed, each study was evaluated with the set categories and was considered low risk (+), high risk (-), or unclear (?).
2.2. Statistical Analysis
The studies evaluated their data utilizing linear regression models of which the results were recorded by a standard deviation score with a 95% confidence interval (95% CI) and odds ratios (OR). Odds ratio with a 95% CI was utilized to compare mothers who consumed less amounts of caffeine (<50 mg/day,15 <150 mg/day,24 and <180 mg/day13) to those who consumed more (>50 mg/day,15≥150 mg/day,24 and ≥180 mg/day13). P-value or P for trend of <0.05 was used to establish significance for all of the studies except Barr and Streissguth.27 The study that utilized serum paraxanthine28 also evaluated the difference of BMI scores with serum paraxanthine levels using a Risk Ratio and 95% CI. Since each study presented different assessments of mothers’ caffeine sources during pregnancy, as well as varying anthropometrics and follow-up times, a meta-analysis was not possible and therefore a systematic review ensued.
To evaluate the quality of each study, the National Lung, Heart and Blood Institute Study Quality Assessment Tool for Observational Cohort and Cross-sectional studies was applied.29 When applying this tool, each study was evaluated through a series of 14 questions. Each question gave the study a point if they met the criteria and therefore the maximum score allocated was 14 points in total. Given the context of cohort studies, no additional analysis was needed. This is a systematic review, therefore this manuscript was exempt from seeking an institutional ethics approval before conducting the review.
3. Results
The original search yielded 24 articles to be included in the review. After duplicates were removed, 18 articles were available to be screened. Of the 18 articles available, only those with measurements of both maternal caffeine intake during pregnancy and childhood outcomes of overweight, altered fat deposition including anthropometric measurements indicating childhood overweight or obesity were included. This allowed for eight articles to be included in the final review (Figure 1).
Every study consisted of a prospective cohort population across multiple countries including Netherlands,13,22 Norway,15 United States,24,27,28 Ireland,14 and Brazil.10 Follow-up throughout the studies were significantly different. The shortest follow-up period measured infants at six months old as the endpoint of the study.10 The majority of studies had endpoint follow-ups between the ages of six to 10 years old for evaluation of the children.13-15,22,27,28 The longest study evaluated their cohort population up to 15 years.24 Eligible study characteristics are available in Table 1.
| Authors/Cohort | Time frame of follow- up | How Caffeine intake was obtained | Sources of Caffeine | Measurement of Caffeine (mg) | Main results (95% CI)* (mg/day of caffeine intake during pregnancy) |
|---|---|---|---|---|---|
| Voerman, et al, 2016.22 Generation R Study. 2001-2005, Netherlands | From birth to 6 years | Postal Questionnaires during 1st, 2nd and 3rd trimesters | Coffee, Tea | Each unit of caffeine based on 1 cup of caffeinated coffee ~90mg=1unit | 4-5.9 and ≥6 units/d= ↑ BMI: 0.9(-0.01, 0.19), 0.16 (-0.03,0.36)(P<0.001) and ↑total body mass at 6 yr old: 0.10 (0.01,0.20), 0.18 (0.01,0.37)(Ptrend 0.015) respectively. ≥6 units/day=↑risk of overweight 1.25(0.68,2.30).** |
| Voerman E, et al, 2019.13 Generation R Study. 2001-2005, Netherlands | 10 years old | Postal Questionnaires during 1st, 2nd and 3rd trimesters | Coffee, Tea | Each unit of caffeine based on 1 cup of caffeinated coffee ~90mg=1unit | 4-5.9 and ≥6 units/d=↑BMI: 0.12 (0.01,0.24) and 0.24 (0.01,0.47) respectively (Ptrend 0.048) and ↑ body fat mass 0.14(0.04, 0.25) and 0.22(0.02, 0.43) respectively (Ptrend 0.008). ≥6 units/d= ↑ risk of overweight at 10 yr old 1.59 (0.92,2.75).** |
| Papadopoulou E, et al, 2018.15Norwegian Mother and Child Cohort Study. 1999-2008, Norway | 6, 18, 36 months and 5, 7 and 8 years. | FFQ during first 4-5 months of gestation | Coffee, black tea, caffeinated soft drinks, energy drinks, chocolate, chocolate milk and sandwich spreads, desserts, cakes and sweets with cocoa. | Caffeine in mg/d Low (0-49) Avg (50-199) High(200-299) Very High (≥300) | 50-199 mg/d=risk of ↑ BMI at 8 yr old:0.02 (-0.01,0.05) ≥300 mg/d= risk of ↑ BMI at 8 yr old: 0.31 (0.22,0.39), risk of excess growth by additional 480g in weight at 8yr old 1.29 (1.04,1.61). Risk of being overweight by 8 yr old 1.29 (1.04, 1.61).** |
| Li DK, et al, 2015.24 San Francisco: Kaiser Permanente Northern California: Integrated health-care delivery system. 1996-1998, United States | 15 years | In-person interview in first or very early second trimester. | Coffee (caffeinated or decaf) Tea (caffeinated or decaf), caffeinated soda, hot chocolate. | For every 150ml of a beverage ~5oz. Coffee:100mg Decaf Coffee: 2mg Tea: 39mg Decaf Tea: N/A Soda: 15mg Hot Choc: 2mg | Maternal caffeine intake overall during pregnancy has an 87% risk of their children having obesity using BMI-for-age criteria OR 1.87 (95% CI: 1.12, 3.12) (Ptrend <0.01). <150 mg/d alone had a 77% increased risk of the offspring being obese OR 2.37 (95% CI: 1.24, 4.52) (P<0.01). |
| Chen L, et al, 2019.14 The Lifeways Cross-Generation Cohort Study. 2001-2003, Ireland | 5 and 9 years old | FFQ in first trimester | Coffee, tea, soft drinks, chocolate containing food and beverages *tea is main source of caffeine in Ireland. | Caffeine divided into groups depending on intake reported in FFQ. All in mg/day <50, 50-<100, 100 to <200 and ≥200/day. | 50 mg/d = ↑ risk overweight at 9 yr old with every 100 mg/d increase 0.144 (1.10,1.88)(P<0.01). ↑ risk of increased central obesity at 9 yr old 1.62(1.12,2.34)(p<0.05). ≥200 mg/d=↑BMI z-score 0.17(0.04,0.29)(P<0.01). Caffeine from coffee only associated with ↑ risk of overweight or obesity at 9 yr old 2.81(1.14,6.90)(Ptrend 0.10) |
| Santos de Medeiros T, et al, 2017.10Impact of Perinatal Different Intrauterine Environments on Child Growth and Development in the First Six Months of Life Project. 2011-2015, Brazil | 3 and 6 months of age | FFQ 7 days post-partum | Caffeine from coffee only | Caffeine in mg by converting serving sizes as needed and using U.S nutritional tables. | Mothers who had caffeine during pregnancy had children with increased skinfold measurements at 3 months 0.0015 (0.000, 0.029) (p<0.047). No significant association with measurements at 6 months. |
| Barr and Streissguth, 1991.27 Seattle Longitudinal Study on Alcohol and Pregnancy. 1974-1975, United States | Birth to 7 years of age | Self-reported consumption using quantity-frequency-variability interview | Coffee, tea, cola, chocolate candy and chocolate milk | 27 mg for non-herbal tea, 112, 74 or 66 mg per cup of dripped, percolated or instant coffee, 10mg choc milk, 31mg soft drink and 20mg for 4oz chocolate bar | No association was found with prenatal caffeine exposure and birthweight, birth length, or head circumference. |
| Klebanoff and Keim, 2015.28 Collaborative Perinatal Project 1959-1965, United States | 4 and 7 years of age | Serum paraxanthine collected at registration and every 8 weeks during pregnancy, at delivery and 6 weeks post-partum | Caffeine intake in general – no specific source as the caffeine metabolite was being measured | n/a | No association between serum paraxanthine levels during pregnancy and childhood overweight or obesity. |
3.1. Sociodemographic Characteristics
The total number of mother-child pairs that had end point measurements of the child or adolescent at completion of the study was 34,443. The age of the participating mothers in four of the studies10,13,14,22 ranged from 26.2-36.5 years and a pre-pregnancy BMI range of 17.8-31.0. The other studies provided ages15,24,27,28 and BMI15,24 in separated groups and therefore could not be combined but are available in Table 2. Each cohort only allowed information on the mothers that had delivered a singleton, live birth and consumed caffeine during pregnancy.
| Authors, year, place of cohort. | Number of Subjects | Mean age (yr) | Pre-pregnancy BMI | Ethnicity | Education level | Smoked during pregnancy (yes) | Parity |
|---|---|---|---|---|---|---|---|
| Voerman, et al,22 2016 | 7,857 mothers in analysis. 5,562 children at follow-up | 30.4 | 22.6 | 58.5% of European descent | 5.9% primary 43.3% secondary 50.8% higher | 18.6% | 43.6% multiparous |
| Voerman E, et al,13 2019 | 4770 mothers with children at follow-up | 31.2 | 22.6 | 65.8% European descent | 7.4% primary 42.2% secondary 50.4% higher | 24.3% | 41.2% multiparous |
| Papadopoulou E, et al,152018 | 50,943 mother-child pairs | <20= < 1% 20-29=44.6% ≥30=54.5% | <18.5=2% 18.5-24.9=66.2% 25-29.9=21.7% ≥30=9% | n/a | < 13 years=29.2% 13-16 years=43.9% >16 years=26.7 | 7% | 46% multiparous |
| Li DK, et al,24 2015 | 661 children | *<25=14.3% 25-30=28.9% 30-35=34.9% 35+=21.7% | <25=67.9% ≥25=32% | White=34.4% Black=6% Hispanic=23.5% Asian/Pacific Islander=30.8% Other=4% | <College=56.7% College degree=28.6% Graduate School=14.4% | 9.9% | 57% multiparous |
| Chen L, et al,142019 | 558 mother-child pairs | 30.8±5.7 | 23.7±3.8 | n/a | Below tertiary=48% Tertiary or above=52% | 26% | 57% multiparous |
| Santos de Medeiros T, et al,102017 | 272 mother-child pairs | 26.2±6.7 | 24.4±6.6 | White=60.3% | Median: 10 years | 25% | 58.8% multiparous |
| Barr and Streissguth,271991 | 1529 mothers** | 13-16=2% 17-24=33% 25-32=59% 33-40=6% >40=<1% | n/a | White=86% Black=9% Other=5% | <High school=11% High School Grad=28% Some College=29% College Grad=25% Grad School=7% | n/a | 56% multiparous |
| Klebanoff and Keim,28 2015 | 1900 mothers*** | <20=14.5% 20-24=38.6% 25-29=23.8% 30-34=13.7% ≥35=9% | n/a | White=68.5 Other=31.4 | <12 years=40.9% 12 years=39.7% >12 years=19.2% | 41% | n/a |
Out of the participants, those who consumed the higher amounts of caffeine tended to be older (>30 years of age),13-15,24,28 have more than one child,13-15,24,27 be a smoker,10,13,15,24,27,28 and of European descent or white.13,22,24,28 Four of the studies found that mothers who had higher education also tended to consume more caffeine.13,14,22,23,24 Table 2 addresses demographic information of the included studies.
Sources of caffeine included were coffee,13-15,22,24,27 tea,13-15, 22,24,27 soft drinks,14,15,24,27 chocolate,14,15,27 chocolate milk,14,15,27 hot chocolate,14,24 sandwich spreads,15 and desserts or sweets with cocoa.14,15 Energy drinks were excluded due to limited consumption of these during pregnancy.15
Caffeine content was measured differently throughout the studies. Two of the studies estimated an average coffee serving to be approximately 90 mg of caffeine13,22 and then characterized caffeine content into units (1 unit=90 mg of caffeine). One study that utilized in person interviews,24 used 150 ml to be approximately 100 mg of caffeine as a standard serving. Three of the studies10,14,15 evaluated caffeine content using mg/day based on the responses received from the food frequency questionnaire (FFQ) data. Only one study provided the differences of caffeine content depending on preparation of the coffee i.e. dripped, percolated or instant coffee.27 In the Collaborative Perinatal Project conducted by Klebanoff and Keim,28 caffeine consumption was measured by serum paraxanthine levels, which have been shown to correlate with 24 hour caffeine consumption. Serum was collected every eight weeks during pregnancy but only two serum samples were used; one for <20 weeks and one from >26 weeks gestation.
Every study was able to control for confounders and had adequate length of follow up time to assess outcomes. The outcome of interest was an area of low bias for all the studies due to the nature of selecting a cohort that is known to be pregnant. Aside from the outcome of interest being known, Barr and Streissguth27 and Klebanoff and Keim28 had the lowest risk of bias. Li et al.24 overall had a low bias assessment; however, participants provided their own caffeine information despite having an interviewer present therefore introducing a potential for bias. Every study had a similar selection process of obtaining their participants from a cohort population voluntarily. The pregnant women that did not consume caffeine during pregnancy were selected from the same cohort. Santos de Medieros et al.10 presented the highest risk of bias from the studies. Part of this was due to their inability to get the sample size they needed from the cohort and therefore selected their own convenience sample out of the cohort available to them.10 The assessment of outcomes was unclear in half of the studies10,13,15,22 due to lack of statements identifying if the researchers were blinded, who was doing the measurements they provided, and lack of comparison to secure records. The majority of studies had adequate follow-up retention however three of them10,13,14 had > 20% loss to follow up. Details for the risk of bias are summarized in Figure 2.
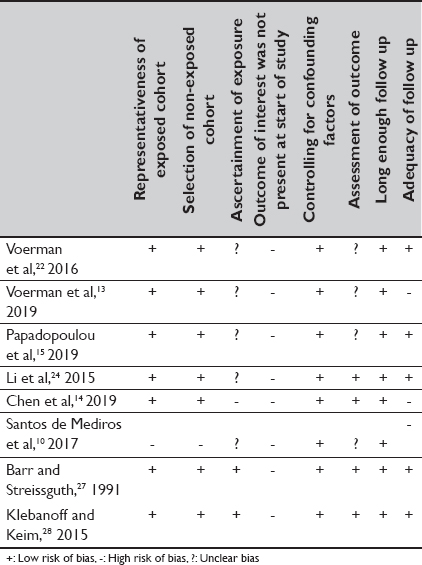
- Risk of Bias in Individual Studies26
3.2. Main Variable Results
The Generation R cohort in the Netherlands produced two studies of which caffeine was categorized into units, each unit equaled 90 mg of caffeine.13,22 For the first study22 when comparing results between pregnant mothers who consumed <2 units of caffeine to those that consumed 4-5.9 units and ≥6 units, the offspring had increased childhood BMI using IOTF criteria, 0.9 standard deviation (SD) (95% confidence interval (CI): -0.01, 0.19) for 4-5.9 units and 0.16 SD (95% CI:-0.03, 0.36) for ≥6 units, (P<0.001). Using the same caffeine amounts, elevated total body mass at six years old was also observed 0.10 SD (95% CI: 0.01, 0.20) and 0.18 SD (95% CI: -0.01, 0.37) respectively (Ptrend 0.015). Mothers who consumed ≥6 units per day during pregnancy had children with an increased android/gynoid fat ratio 0.27 SD (95% CI: 0.05, 0.49). This same group of mothers that consumed ≥6 units caffeine per day also showed children at age six with an increased risk of being overweight when compared to mother’s who consumed <2 units per day. OR 1.25 (95% CI: 0.68, 2.30).
The second Generation R cohort study13 evaluated offspring up to 10 years of age and found congruent results. For those who had maternal caffeine consumption during pregnancy of 4-5.9 units or ≥6 units of caffeine per day compared to <2 units per day, offspring were found to have increased BMI per IOTF criteria 0.12 SD (95% CI: 0.01, 0.24) and 0.24 SD (95% CI: 0.01, 0.47) respectively (Ptrend 0.048). Elevated body fat mass index at both 4-5.9 and 6 units was also observed 0.14 SD (95% CI: 0.04, 0.25) and 0.22 (95% CI: 0.02, 0.43) respectively (Ptrend 0.008), and an elevated android/gynoid fat mass ratio was found with the same amount of caffeine 0.16 SD (95% CI: 0.05, 0.27) and 0.22 SD (95% CI: 0.01, 0.44) respectively (Ptrend 0.003). Mothers who consumed ≥6 units caffeine per day compared to those who have <2 units per day during pregnancy had increased risk of their child being overweight at 10 years of age OR 1.59 (95% CI: 0.92, 2.75). Similarly, mothers who had 4-5.9 or ≥6 units of caffeine per day had offspring with associated increased abdominal subcutaneous fat mass index 0.15 SD (95% CI: -0.01, 0.30) for the 4-5.9 units and 0.35 SD (95% CI: 0.04, 0.65) for ≥6 units (Ptrend 0.023). With the same units of caffeine, elevated abdominal visceral fat mass index was also observed with 0.14 SD (95% CI: -0.03, 0.30) and 0.43 SD (95% CI: 0.11, 0.76) respectively (Ptrend 0.003). Finally, liver fat fraction was also high in these children with 4-5.9 units of caffeine consumed per day when compared to <2 units per day 0.2 SD (95% CI: 0.04, 0.36) (Ptrend 0.004).
The Norwegian Mother and Child Cohort study15 separated maternal caffeine consumption into different groups, low (<50 mg), average (50-199 mg), high (200-299 mg), and very high (≥300 mg). Follow-up on the children was completed at six months old up to eight years of age. When compared to the low caffeine intake, children who had mothers with very high caffeine intake during pregnancy had an increased likelihood of excess growth, defined as an excess of 480 grams, by eight years old (adjusted odds ratio aOR) 1.29 (95% CI: 1.04, 1.61). When compared to low caffeine consumers, risk of being overweight by age eight was only found in the very high caffeine group odds ratio (OR) 1.29 (95% CI: 1.04, 1.61). This study evaluated BMI for children at eight years old by using Jenss-Bayley growth curve model and cut off points for overweight or obesity were determined using the IOTF criteria. Increased BMI was found in offspring of pregnant mothers who consumed 50-199 mg/day in all age groups including infancy at three months β coefficients (β) 0.03 (95% CI: 0.01, 0.05), toddlerhood at 18 months β 0.04 (95% CI: 0.02, 0.06), preschool at five years β 0.03 (95% CI: 0.01, 0.06), and school age at eight years β 0.02 (95% CI: -0.01, 0.05). Risk of elevated BMI by age eight in the very high caffeine group when compared to the low group was β 0.31 (95% CI: 0.22, 0.39).
The longest study had a 15 year follow-up period in which caffeine intake was divided into three groups: no caffeine, <150 mg/day, and ≥150 mg/day.24 Compared to the no caffeine group, caffeine intake overall from the mother during pregnancy showed an 87% increased risk of their children having obesity using BMI-for-age criteria OR 1.87 (95% CI: 1.12, 3.12) (Ptrend <0.01). The group that had <150 mg caffeine per day alone had a 77% increased risk of the offspring being obese aOR 1.77 (95% CI: 1.05, 3.00).. The offspring from those who consumed ≥150 mg/day were more than twice as likely to have obesity 2.37 (95% CI: 1.24, 4.52). P-value for trend for the dose response groups was P<0.01. The researchers found that the source of caffeine did not seem to impact the overall outcomes. Additionally, this is the only study that separated genders of children, finding that girls were at higher risk of obesity than boys (<150 mg/day OR 1.24 (95% CI: 0.61, 2.50)) and (≥150 mg OR 3.32 (95% CI: 1.49, 7.41)) (Ptrend 0.007) when their mothers consumed caffeine during pregnancy.
Chen et al.14 found that compared to those who did not drink caffeine during pregnancy, mothers with caffeine intake starting at 50 mg/day during pregnancy had an increased risk of offspring with childhood overweight or obese status at age nine with every 100 mg/day increase of caffeine OR 1.44 (95% CI:1.10, 1.88) (P <0.01). This same increase in caffeine was also associated with an elevation in central obesity, measured as a waist circumference >90th percentile in nine year olds OR 1.62 (95% CI: 1.12, 2.34) (P <0.05). BMI z-scores, which are age and sex specific, were elevated with caffeine consumption ≥200 mg/day 0.17 (95% CI: 0.04, 0.29) (P <0.01) when compared to those mothers who consumed <50 mg caffeine per day. When comparing low caffeine intake of <50 mg/day to highest intake ≥200 mg/day, caffeine from coffee alone had an association with overweight and obese status at nine years old OR 2.81 (95% CI: 1.14, 6.90) (Ptrend 0.10) and central obesity OR 4.57 (95% CI: 1.14, 18.24) (Ptrend 0.046).
3.3. Other Variable Results
Following studies that found a positive association with caffeine intake during pregnancy and adverse childhood outcomes, Santos de Medieros et al.10 utilized a cohort group but then stratified participants into smaller groups based on the pregnant mother’s characteristics. These groups included diabetic mothers, those with hypertension, those with SGA children, mothers that smoked, and the control group of no caffeine consumption during pregnancy. Caffeine intake was evaluated by group and then body fat recorded as skinfold measurements were taken on infants at three and six months. For the women that consumed caffeine during pregnancy, their offspring did show an increase in skinfold thickness measurements at three months in a multiple linear regression β 0.0015 (95% CI: 0.000, 0.029) (P<0.047). The sum of skinfold thickness was high and was found to have significance when compared to the control group (P=0.034). When these measurements were repeated at six months, no significant association was found between the maternal caffeine intake during pregnancy and skinfold measurements. It is interesting to note that mothers with diabetes were more likely to consume caffeine compared to the other groups (P<0.05) and those who smoked had a higher caffeine intake overall when compared with the control group (P=0.01).
The Seattle Longitudinal Study on Alcohol and Pregnancy cohort27 determined if an association exists between maternal caffeine consumption and infants’ anthropometric measurements at birth. No association was found between caffeine intake and birthweight, birth length, or head circumference. Offspring were followed for seven years at which time still no significant association was found.
Finally, serum paraxanthine levels were measured to identify caffeine intake of pregnant mothers instead of milligrams of caffeine consumed.28 Serum paraxanthine is a metabolite of caffeine and evaluates both caffeine intake and metabolism; elevated levels correspond to recent caffeine consumption typically for a 24 hour period. Serum paraxanthine levels were collected at <20 weeks and ≥26 weeks gestation. A trend was observed of elevated child BMI-for-age with increasing risk of overweight or obesity as serum paraxanthine levels increased up to 1,000 μg/liter. For serum paraxanthine levels >1000 μg/liter BMI-for-age plateaued or decreased with increased concentration. Therefore, no association between serum paraxanthine levels in a pregnant mother and risk of overweight or obesity in offspring was identified.
An association was found between maternal caffeine consumption as low as 50 mg/day during pregnancy with increased risk of elevated BMI,15 overweight or obese status,14 and increased waist circumference.14 Increased risk of obesity was also found in amounts <150 mg/day.24 Other studies did not find an association with risk of overweight until ≥200 mg/day14 or ≥300 mg/day of caffeine consumption.15 Furthermore, two of the studies did not associate overweight status of the child with caffeine intake until amounts were ≥540 mg/day.13,22 Those that found an association when caffeine was 50 mg/day did find that with increasing amounts of caffeine intake, risk of these outcomes increased.14,15,24
Additional findings throughout the studies included increased total body fat mass, 13,22 and higher liver fat fraction13 at ≥360 mg of caffeine per day during pregnancy. Increased android/gynoid fat ratio was also observed both at ≥360 mg13 and ≥540 mg13,22 of caffeine per day. Excess growth15 was identified at ≥300 mg/day and central obesity14 was found with caffeine at 50 mg/day. Altered anthropometrics including skin fold test at six months10 or height, length, and head circumference at seven years27 were not found to be associated with a mother’s caffeine consumption during pregnancy. No relationship was found between serum paraxanthine levels during pregnancy and BMI-for-age by seven years old.28
All studies in this review were ≥10 out of 14 in quality. The highest rated study was Klebanoff and Keim28 had a study quality score of 12 out of 14. By evaluating serum paraxanthine levels, areas of potential error such as error of self-report of caffeine intake were eliminated. In order to have a sufficient sample size and due to the nature of the cohort study design the majority of studies13-15,22,24,27,28 were unable to justify their sample size. The one exception to this was Santos de Medieros et al.10 who selected a convenience sample out of the cohort. The statistical power of the study was evaluated due to the use of the convenience sample. Every study did not make it clear if those who were evaluating the childhood anthropometric outcomes were aware of the caffeine consumption of the mothers during pregnancy. Chen et al.14 and Papdopoulou et al.15 had the lowest quality with a score of 10 out of 14 due to caffeine intake assessment only being completed once in their evaluation of the mother’s intake. The summary of the quality assessment of studies in this review can be seen in Table 3. As a meta-analysis was unable to be completed due to the differing results and measurements of each study, no additional analysis was needed.
| Reference | Possible conflict of interest reported | Total quality score* | Criteria not met |
|---|---|---|---|
| Voerman, et al,22 2016 | No | 11 | Was a sample size justification, power description, or variance and effect estimates provided? Not recorded. Were the outcome assessors blinded to the exposure status of participants?: Not recorded Was loss to follow-up after baseline 20% or less? 30% loss to follow up. |
| Voerman E, et al,13 2019 | No | 11 | Was a sample size justification, power description, or variance and effect estimates provided? Not recorded. Were the outcome assessors blinded to the exposure status of participants?: Not recorded Was loss to follow-up after baseline 20% or less? 39.6% loss to follow up |
| Papadopoulou E, et al,152018 | No | 10 | Was a sample size justification, power description, or variance and effect estimates provided? Not recorded. Was the exposure assessed more than once over time?: No Were the outcome assessors blinded to the exposure status of participants?: Not recorded Was loss to follow-up after baseline 20% or less? 77% loss to follow up. |
| Li DK, et al,24 2015 | No | 11 | Was a sample size justification, power description, or variance and effect estimates provided? Not recorded. Was the exposure assessed more than once over time?: No Were the outcome assessors blinded to the exposure status of participants?: Not recorded |
| Chen L, et al,142019 | No | 10 | Was a sample size justification, power description, or variance and effect estimates provided? Not recorded. Was the exposure assessed more than once over time?: No Were the outcome assessors blinded to the exposure status of participants?: Not recorded Was loss to follow-up after baseline 20% or less? No |
| Santos de Medeiros T, et al,102017 | No | 11 | Was the timeframe sufficient so that one could reasonably expect to see an association between exposure and outcome? No For exposures that can vary in amount or level, did the study examine different levels of the exposure as related to the outcome? No Were the outcome assessors blinded to the exposure status of participants?: Not recorded |
| Barr and Streissguth,271991 | Not stated | 11 | Was a sample size justification, power description, or variance and effect estimates provided? Not recorded. Was the exposure assessed more than once over time?: No Were the outcome assessors blinded to the exposure status of participants?: Not recorded |
| Klebanoff and Keim,28 2015 | Not stated | 12 | Was a sample size justification, power description, or variance and effect estimates provided? Not recorded. Were the outcome assessors blinded to the exposure status of participants?: Not recorded |
4. Discussion
Of the eight studies available, five of them found an association between maternal caffeine consumption of 50 mg/day to >540 mg/day and offspring obesity with either elevated BMI-for-age13,22,24 or elevated BMI per IOTF criteria.14,15 The likelihood of these outcomes increased as caffeine intake increased.14,15 Secondary outcomes that were associated with caffeine intake during pregnancy included risk of overweight starting at ≥50 mg/day14 to ≥540 mg/day,13,15,22,24 excess growth or increase in total body weight at ≥300 mg/day,15 increased central obesity or high waist circumference at ≥50 mg/day,14 elevated android/gynoid fat ratio at ≥360 mg/day,13,22 elevated liver fat fraction at ≥360 mg/day,13 and an increase in both total body mass22 and body fat mass at ≥360 mg/day.13 Three of the studies were unable to find a relationship between caffeine consumption and a child’s anthropometrics including skin fold measurements,10 height, length, and head circumference,27 and BMI-for-age using serum paraxanthine levels.28
4.1. Discussion
The large size of the cohort groups available allowed researchers to draw conclusions in regards to adverse risk factors of caffeine intake during pregnancy. By evaluating possible health outcomes beyond the first couple months after birth, these studies support previous evidence that nutrient intake during pregnancy plays a large role in health outcomes for life. Only 25% of women do not consume caffeine while pregnant.19 Research has shown that women do decrease their caffeine intake during pregnancy27 but the loss of the beneficial side effects of caffeine such as mental alertness and decreased fatigue16 can be challenging.
These cohorts were from countries around the world eliminating location as a factor and allowing researchers to focus in on individual maternal intakes. The size of the cohorts was beneficial as researchers were able to draw conclusions from a large offspring population and have enough anthropometric data to evaluate obesity trends. The researchers also included measurements on other weight related health factors including overall body fat mass, 13 waist circumference,14 and liver fat fraction.13 Elevations in these measurements has similar health risk as being overweight or obese and may help determine the primary etiology of adipose changes with caffeine intake. Klebanoff and Keim28 used serum paraxanthine to identify the amount of caffeine consumed than only using serum caffeine level. Measurements of serum paraxanthine have been found to correlate with self-reported caffeine consumption and may be a useful tool to clarify caffeine intake.30
In regards to quality, the strengths of the studies included clarity and specificity of which the authors discussed their objectives and appropriate populations, exposure measures were clearly defined, and sufficient time frames were provided.
4.2. Limitations
Information on maternal caffeine consumption during pregnancy was derived from food frequency questionnaires,10,14,15 postal questionnaires,13,22 and in person interviews.24,27 While the FFQ method is preferred in large cohorts,31 self-reporting errors may occur.32 For the studies utilizing the food frequency questionnaire and postal questionnaires, information was gathered at different time points throughout the pregnancy including first trimester,15 22 weeks,14 and at each trimester.10,13,22 Two studies24,27 used in-person interviews which may have contributed to a better estimation of actual consumption thus aiding in the significant finding however in-person interviewing could also contribute to misinformation if the participant was not comfortable sharing true caffeine intake. In person interviews were obtained during the first trimester or early second trimester24 and the quantity frequency index was completed during the 5th month of pregnancy.27 As caffeine intakes may change as pregnancy continues,27 in the future it may be helpful to collect serum at different points throughout the pregnancy.
The types and sources of caffeine recorded varied across all studies. Most agreed that coffee was a major contributor to caffeine intake, many of them pointed out that caffeine levels in both coffee and tea can vary depending on preparation method.10,13-15,22,24,27 Two studies identified coffee as their main caffeine source10,14 of which they were able to find a relationship with obesity of overweight status in offspring. However, other studies15,24 found that overweight or obesity risk was associated with any source of caffeine including coffee, soda and tea. Only two of the studies considered added sugar intake from soda or if the mother had sugar or cream added to their caffeinated beverages.14,24 This is important not only for the excess calories these additives could provide, but also for the component of pure sugar to the infant potentially affecting the outcomes of the study. These additives should be addressed in the questionnaire used to evaluate caffeine intake.
The studies evaluated caffeine in milligrams per day then grouped caffeine amounts into different categories to identify what low versus high caffeine intake definitions were. The categories often had a large range of caffeine amounts consumed. This range prevents mothers from knowing the exact amount of caffeine that can be consumed without associations with childhood overweight or obesity. The studies by Voerman et al.13,22 from 2016 and 2019 had the most divisions of caffeine intakes allowing for little range, however Chen et al14 had wide ranges such as 50-199 mg/day for average caffeine intake and therefore were conclusively able to report an association with caffeine as low as 50 mg/day when it may have been found only in those who consumed >50-199 mg/day. The five studies with a positive association between caffeine intake during pregnancy and childhood obesity by age appropriate BMI found this association at 50-199 mg/day,15 <150 mg/day,24 ≥200 mg/day,14 and ≥360 mg/day.13,22 This large difference shows the importance of providing smaller ranges of caffeine measurements.
Only one study24 found a significant difference between genders. As this study had a 15-year follow-up period, it was the only study to evaluate offspring beyond 10 years of age. Girls who were born to mothers that consumed any amount of caffeine (< 150 mg or ≥150 mg/day) during pregnancy were more likely to be persistently obese. With the advancing age of the offspring, gender differences at puberty need to be considered while evaluating anthropometrics. In general, during puberty, girls accumulate more fat than their male counterparts, while males develop more lean body mass.33 Therefore, puberty changes may contribute to the gender differences observed.
Potential mechanisms between caffeine consumption in pregnancy and childhood obesity or overweight status were discussed throughout the studies. The enzyme CYP1A2 decreases throughout pregnancy due to hormone changes.13-15,22,34 The decreasing function of the enzyme, in addition to caffeine being able to cross the placental barrier, results in the fetus having caffeine in their system for a longer period of time potentially affecting growth and development.20,22,35 Hormone changes are also thought to be responsible for elevated glucocorticoid levels that occur when caffeine is consumed.11,36,37 This increase in glucocorticoid levels have been associated with childhood obesity and higher visceral adipose tissue deposition.11,36,37 Some studies have suggested that continuous fetal exposure to glucocorticoids could alter the development of the hypothalamic-pituitary-adrenal axis (HPA-axis),10,24,36,37 limit fetal growth, alter the growth of the pancreas, change insulin targeted tissues, and affect adipose deposition.10,13,22 The HPA-axis regulates homeostatic functions throughout the body including glucose and lipid metabolism.10,11,37 Another mechanism involves the association of caffeine intake during pregnancy with SGA infants.38,39 These children go through a period of catch-up growth which has been associated with increased body and abdominal fat, particularly central adiposity.6,23 Insulin resistance and elevated insulin-like-growth factor-1 (IGF-1) levels have also been observed to be possibly creating excess fat deposition over lean muscle mass developement.6,11,22,23 Due to the difficulty of experimenting on a pregnant population, these potential etiologies were developed from rodent studies and therefore are difficult to find the same pathways in humans.36,37,40 Emerging research has found a way to utilize “organ-on-a-chip technology”.41 Placental organ tissue has been difficult to obtain due to it only being present during pregnancy. Having this available can help determine amounts of caffeine pass through the placental barrier potentially allowing for more research for caffeine alternatives during pregnany.41
4.3. Recommendations for Further Studies
Ideally future research will continue utilizing large cohort populations. Financially a more specific food frequency questionnaire that delineates specific beverage consumption, including preparation method, and consideration of add-ins such as sugar or cream to beverages would likely yield truer consumption. In-person interviews may improve the quality of the diet being evaluated by having the interviewer define and explain questions along with providing visualization of portion sizes, but this can be time consuming and costly if trained researchers are the ones interviewing. Finding a way to reduce confounders such as separating those who drink coffee versus those who drink tea may also be helpful in determining outcomes with caffeine intake. Determining an appropriate time for follow-up is needed to identify childhood or adolescent age cut off points. As children age into puberty body composition changes can alter results and therefore needs to be addressed.
5. Conclusion and Global Health Implications
From the studies reviewed, caffeine intake as low as 50 mg/day14,15 during pregnancy has an association with increased risk of childhood overweight or obesity measured by either BMI per IOTF criteria15 or central obesity.14 One study found increased risk of obesity when any caffeine intake during pregnancy was considered, but the risk doubled when caffeine amounts were ≥150 mg/day.24 The remaining two studies with a positive association didn’t observe a risk of overweight or obesity until caffeine intake was ≥360 mg/day.13,22 As only two studies found associations at 50 mg/day but did identify that the risk increased as the amount of caffeine increased,14,15 the current recommendation of <200 mg/day presents with a lower risk of offspring overweight or obesity, but complete avoidance of caffeine would be recommended during pregnancy to eliminate any risk of these characteristics in children.
Acknowledgements:
None.
Compliance with Ethical Standards
Conflicts of Interest: The authors declare no conflicts of interest.
Financial Disclosure: This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Funding/Support: There was no source of funding or sponsors for this study.
Ethics Approval:This is a systematic review, therefore it was not necessary to obtain an institutional ethics approval before conducting the review.
References
- Prevalence of obesity among adults and youth: United States, 2015-2016. In: NCHS Data Brief. Vol 288. Hyattsville, MD: National Center for Health Statistics; 2017.
- [Google Scholar]
- Overweight and obesity in children and adolescents. J Clin Res Pediatr Endocrinol. 2014;6(3):129-143.43.
- [Google Scholar]
- Understanding recent trends in childhood obesity in the United States. 2019. Econ Hum Biol. 34:16-25. https://doi.org/ 10.1016/j.ehb.2019.02.002
- [Google Scholar]
- 2020. Overweight and Obesity: Childhood obesity causes and consequences. https://www.cdc.gov/obesity/childhood/causes.html
- Early development of adiposity and insulin resistance after catch-up weight gain in small-for-gestational-age children. J Clin Endocrinol Metab. 2006;91(6):2153-2158. doi:10.1210/jc.2005-2778
- [Google Scholar]
- ASPE Research brief:Childhood obesity. 2005. U.S. Department of Health and Human Services. https://aspe.hhs.gov/ basic-report/aspe-childhood-obesity-white-paper
- [Google Scholar]
- Overweight and Obesity:Defining childhood obesity. https://www.cdc.gov/obesity/childhood/defining.html
- Extended international (IOTF ) body mass index cut-offs for thinness, overweight and obesity. Pediatr Obes. 2012;7(4):284-294. doi:10.1111/j.2047-6310.2012.00064.x
- [Google Scholar]
- Caffeine intake during pregnancy in different intrauterine environments and its association with infant anthropometric measurements at 3 and 6 months of age. Matern Child Health J. 2017;21:1297-1307. doi:10.1007/210995-016-2230-7
- [Google Scholar]
- Fetal rat metabonome alteration by prenatal caffeine ingestion probably due to the increased circulatory glucocorticoid level and altered peripheral glucose and lipid metabolic pathways. Toxicol Appl Pharmacol. 2012;262:205-216. doi:10.1016/j.taap.2012.05.002
- [Google Scholar]
- Impact of maternal nutrition and metabolism on health of the offspring. Semin Fetal Neonatal Med. 2007;12:71-77. doi:10.1016/j.siny.2006.10.010
- [Google Scholar]
- Associations of maternal caffeine intake during pregnancy with abdominal and liver fat deposition in childhood. Pediatr Obes 2019:e12607. doi:10.1111/ijpo.12607
- [Google Scholar]
- Maternal, but not paternal or grandparental, caffeine intake is associated with childhood obesity and adiposity:The lifeways cross-generation cohort study. Am J Clin Nutr. 2019;109:1648-1655. doi:10.1093/ajcn/nqz019
- [Google Scholar]
- Maternal caffeine intake during pregnancy and childhood growth and overweight:results from a large Norwegian prospective observational cohort study. BMJ Open. 2018;8:e018895. doi:10.1136/bmjopen-2017-018895
- [Google Scholar]
- Beverage caffeine intakes in the U.S. Food Chem. Toxicol. 2014;63:136-142. doi:10.1016/j.fct.2013.10.042
- [Google Scholar]
- Key elements of healthy eating patterns. A closer look inside healthy eating. https://health.gov/our-work/food-nutrition/2015-2020-dietary-guidelines/guidelines/chapter-1/a-closer-look-inside-healthy-eating-patterns/#callout-caffeine
- [Google Scholar]
- The impact of coffee on health. Planta Med. 2017;83:1256-1263. doi:10.1055/s-0043-115007
- [Google Scholar]
- Maternal caffeine consumption during pregnancy and the risk of miscarriage:a prospective cohort study. Am J Obstet Gynecol. 2008;198:279e.1-279.e8. doi:10.1016/j.ajog.2007.10.03
- [Google Scholar]
- caffeine consumption during pregnancy. Committee Opinion No.462. ACOG Comm Opin. 2010;116:467-468.
- [Google Scholar]
- World Health Organization Web site. https://www.who.int/elena/titles/caffeine-pregnancy/en/
- Maternal caffeine intake during pregnancy, early growth, and body fat distribution at school age. Obesity. 2016;24(5):1170-1177. doi:10.1002/oby.21466
- [Google Scholar]
- Association between postnatal catch-up growth and obesity in childhood: prospective cohort study. BMJ. 2000;320:97-971.
- [Google Scholar]
- Maternal caffeine intake during pregnancy and risk of obesity in offspring:a prospective cohort study. Int J Obes. 2015;39:658-664. doi:10.1038/ijo.2014.196
- [Google Scholar]
- The PRISMA statement for reporting systematic review and meta-analyses of studies that evaluate health care interventions:Explanation and elaboration. PLoS Med. 2009;6(7):e1000100. doi:10.1371/journal.pmed.1000100
- [Google Scholar]
- The Newcastle-Ottawa Score (NOS) for assessing the quality of nonrandomized studies in a meta-analyses. The Ottawa Hospital Research Institute Web site. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp
- [Google Scholar]
- Caffeine use during pregnancy and child outcome: A 7-Year prospective study. Neurotoxicol Teratol. 1991;13(4):441-448.
- [Google Scholar]
- Maternal serum paraxanthine during pregnancy and offspring body mass index at ages 4 and 7 years. Epidemiology. 2015;26(2):185-191. doi:10.1097/EDE.0000000000000220
- [Google Scholar]
- Study quality assessment tools. https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools
- Serum caffeine and paraxanthine as markers for reported caffeine intake in pregnancy. Ann Epidemiol. 2008;8:107-111.
- [Google Scholar]
- Prenatal caffeine assessment: Fetal and maternal biomarkers or self-reported intake? Ann Epidemiol. 2008;18:172-178. doi:10.1016/j.annepidem.2007.11.005
- [Google Scholar]
- No. 4: Applying Dietary Assessment Methods for Food Fortification and Other Nutrition Programs;Global Alliance for Improved Nutrition (GAIN) Tufts University, HarvestPlus/International Food Policy Research Institute. Program and project documents. 2012. Geneva, Switzerland; https://www.gainhealth.org/resources/ reports-and-publications/applying-dietary-assessment-methods-food-fortification-and-other
- [Google Scholar]
- Pregnancy-induced changes in the pharmacokinetics of caffeine and its metabolites. J Clin Pharmacol. 2016;56(5):590-596. doi:10.1002/jcph.632
- [Google Scholar]
- Passage of caffeine into human gonadal and fetal tissues. Biochem Pharmacol. 1962;11:166-168.
- [Google Scholar]
- A hypothalamic-pituitary-adrenal axis-associated neuroendocrine metabolic programmed alteration in offspring rats of IUGR induced by prenatal caffeine ingestion. Toxicol Appl Pharmacol. 2012;264:395-403. doi:10.1016/j.taap.2012.08.016
- [Google Scholar]
- Caffeine-induced activated glucocorticoid metabolism in the hippocampus causes hypothalamic-pituitary adrenal axis inhibition in fetal rats. PLoS One. 2012;7(9):e44497. doi:10.1371/journal.pone.0044497
- [Google Scholar]
- Maternal caffeine consumption and small for gestational age births:Results from a population-based case-control study. Matern Child Health J. 2014;18(6):1540-1551. doi:10.1007/ s10995-013-1397-4
- [Google Scholar]
- Maternal caffeine intake during pregnancy is association with birth weight but not with gestational length:results from a large prospective observational cohort study. BMC Med. 2013;11:42. doi:10.1186/1741-7015-11-42
- [Google Scholar]
- Caffeine-induced fetal rat over-exposure to maternal glucocorticoid and histone methylation of liver IGF-1 might cause skeletal growth retardation. Toxicol Lett. 2012;214:279-287.
- [Google Scholar]
- Placenta-on-a-chip:In vitro study of caffeine transport across placental barrier using liquid chromatography mass spectrometry. Glob Chall. 2019;3:1800112. doi:10.1002/gch2.20180011
- [Google Scholar]





