Translate this page into:
Utilization, Predictors and Gaps in the Continuum of Care for Maternal and Newborn Health in Ghana
*Corresponding author email: efuaenos@gmail.com
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Background:
Continuum-of-care (CoC) throughout pregnancy, childbirth and the postnatal period is essential for the health and survival of mothers and their babies. This study assesses the utilization, predictors, and gaps in the continuum of maternal and newborn health (MNH) services in Eastern Ghana.
Methods:
A retrospective cross-sectional survey was conducted to assess utilization of MNH services and their determinants in the East Akim Municipality of Ghana. Three hundred and ten (310) mothers aged 15-49 years were sampled from 4 communities (3 rural; 1 urban) in the municipality using stratified sampling methodology. Logistic regression models were fitted to determine the likelihood of utilizing skilled birth attendance (SBA) and postnatal care (PNC) after antenatal care (ANC).
Results:
Sixty-six percent (66%) of mothers surveyed received the full complement of MNH services (ANC, SBA, PNC) for their most-recent birth. While 98% of mothers made at least one ANC visit with 83.5% receiving the World Health Organization-recommended 4+ visits, only 74% accessed SBA indicating a 24% attrition in the CoC from ANC to SBA, and an 8% attrition from SBA to PNC. About 86% of mothers accessed PNC within 42 days postpartum. Distance to health facility, urban residence, and exposure to media information were strong predictors of the full complement of MNH continuum-of-care utilization.
Conclusion and Global Health Implications:
The study found a remarkable utilization of MNH services in East Akim with significant attrition along the continuum-of-care. Efforts to enhance utilization of the MNH continuum-of-care should focus on increasing access to SBA in particular, through equitable distribution of MNH services in hard-to-reach areas and innovative communication approaches for reducing attrition at each level of the continuum-of-care. Evidence from this study can inform strategies for achieving universal access and utilization of the MNH continuum-of-care towards global goals and improved health outcomes in Ghana and other countries.
Keywords
Continuum-of-care
Antenatal care
Skilled birth attendance
Postnatal care
Maternal health services
Maternal health
Newborn health
Ghana
1. Introduction
Maternal and neonatal mortality remain high in developing countries, especially in sub-Saharan Africa. In 2017, sub-Saharan Africa alone accounted for approximately 66% of global maternal deaths.1 Furthermore, sub-Saharan Africa had the highest neonatal mortality rate estimated at 28 deaths per 1,000 live births in 2018.2 High rates of maternal and neonatal morbidity and mortality in developing countries are associated with poor access and quality of maternal and neonatal health care.3,4,5 The continuum-of-care (CoC) for maternal, newborn and child health (MNCH) approach is expected to address these challenges and improve the health and survival of mothers and children globally.4,6,7 The “continuum-of-care for MNH” is often narrowed to focus on pregnancy, childbirth and the postnatal period in the context of efforts to improve maternal and newborn health.8 In this context, the goal is to provide women with the full complement of interventions needed during pregnancy, childbirth and postnatal period in order to ensure good pregnancy outcomes and sustain the survival of newborns.9 An integrated approach to care at the various levels of the health system is also essential, with specific interventions outlined for facility- community- and home-based care.
1.1. Background of the Study
In Ghana, efforts at reducing maternal and neonatal morbidity and mortality focus on improving quality of care, promoting equity and ensuring a continuum of health care services for mothers and newborns by the Ghana Health Service (GHS). These include training more midwives and doctors and increasing the Midwives/Women in the Fertile Age (WIFA) ratio and the Doctor/Population ratio. 10 Other initiatives include adoption of the Community-based Health Planning and Services (CHPS) strategy to improve access to maternal and child health services; capacity building for improved client-service provider relationship; and Social and Behavior Change Communication (SBCC) to create awareness of the need for early and regular antenatal care attendance.10 The reproductive and pre-pregnancy health needs of adolescents are also addressed as part of the lifecycle approach to the CoC for MCNH, through the provision of iron and folate supplements within the School Health Education Program (SHEP).11 The program emphasizes health promotion and equips children and adolescents with basic life skills to enable them achieve optimum reproductive health. Despite these efforts, about 14% of adolescents (15-19 years) begin childbearing, which is often associated with an increased risk of complications during pregnancy and childbirth and poor neonatal health outcomes.12 Ghana’s National Health Insurance Scheme (NHIS) also enhances access to maternal health care by waiving the cost of maternity services for mothers and newborns and for children up to 18 years. The “Free” Maternal Health Care initiative of the NHIS covers the full range of MNH services including antenatal care (ANC), skilled birth attendance (SBA) and postnatal care (PNC).13
ANC services offer a platform for providing women with key interventions that provide significant health benefits for mothers and their babies.9,14 At least four (4+) ANC visits during pregnancy is recommended for all pregnant women.15These should, as a minimum, include all interventions outlined in the WHO Antenatal Care Model and Integrated Management of Pregnancy and Childbirth (IMPAC) guidelines.7,9 Though ANC service utilization in Ghana has improved over the years, reaching 89% for 4+ visits in 2017,12 much more needs to be done to achieve Universal Coverage and to improve quality of care. Skilled birth attendance (SBA), which refers to care provided by an accredited health professional such as a doctor, midwife or nurse during childbirth, is recognized as an effective intervention for reducing the risk of maternal death and is thus a critical intervention within the CoC. 16,17 In many developing countries, the proportion of pregnant women who obtain skilled care at birth, reduces compared to those receiving ANC.16
Several studies have investigated the demographic and background characteristics of women and their families, which influence their utilization of MNH services in various settings. However, only one study has investigated the factors associated with the completion of the continuum of MNH care in three districts of Ghana.18. The importance of ensuring the utilization of the full complement of MNH services at all levels of the health system warrants investigation to identify predictors and highlight the gaps that might exist in various contexts, even within the same country.
1.2. Objectives of the Study
This study aimed at assessing the level of utilization of the continuum of maternal and newborn health services in the East Akim Municipality and to determine factors that influence uptake of services, while documenting the gaps and attrition within the care continuum.
2. Methods
A retrospective cross-sectional study among women in their reproductive ages (15-49 years) was undertaken in the East Akim Municipality of the Eastern Region of Ghana from January to June 2017. The study was designed to assess women’s utilization of maternity services and to identify predictors of the completion of the CoC as well as attrition within the continuum.
The population of the East Akim Municipality, according to the 2010 Population and Housing Census is 167,896 representing 6.3% of the region’s total population. The female population constitutes 51.3% and the total fertility rate is 3.1 births per woman. Nearly 40% of the population is rural.19 Health resources in the district include two public and one private hospitals, four Health Centers, three private Maternity Clinics, eighteen functioning Community-based Health Planning and Services (CHPS) compounds (with 35 demarcated CHPS sites) and 120 Community Health Volunteers operating under the authority of the Ghana Health Service.19 According to the Ghana Maternal Health Survey (2017), 57.8% of women (15-49 years) in the Eastern region had NHIS coverage in 2017, compared to a national rate of 45.9%.12
The sample size was determined based on a population of women in their reproductive ages (15-49 years) of about 41,601 in the East Akim Municipality. Using Epi info sample size calculator, and assuming a margin of error of 5% at 95% confidence interval and 8% attrition rate, the estimated sample size was 310. A Stratified Sampling technique was used to select the required sample of respondents for the study. This method was chosen because of the need for representativeness of the two main strata in the chosen population, urban and rural communities, with varied demographic conditions. A simple random sampling method was used to select a total of four (4) communities comprising of three (3) rural and one (1) urban community. Three hundred and ten respondents (310) respondents were drawn from the 4 randomly selected communities according to their population proportion. A structured questionnaire was developed, guided by the objectives of the study and administered by trained Field Assistants to participants. Pre-testing of the questionnaire was done with 10 women from Fanteakwa, a nearby district in the East Akim municipality with similar socio-demographic characteristics as the target population. The questionnaire documented the respondents’ demographic and background characteristics and factors influencing their utilization of maternity services during pregnancy, childbirth and the postnatal period. Only women in their reproductive ages (15-49 years) residing within the selected communities in the East Akim Municipality, who had experienced pregnancy and childbirth in the past two years prior to the study and consented to participate in the study were interviewed. The interviews were conducted in English and the local dialect (Twi) for those who could neither speak nor understand English. Completed questionnaires were checked for completeness and errors at the point of data collection.
2.1. Study Variables
The key outcome variable for this study was utilization of the full complement of MNH services within the CoC. Related outcome variables explored in this study were ANC, SBA and PNC utilization along the MNH CoC. These variables were measured according to WHO definitions and recommended interventions. ANC refers to pregnancy-related check-ups that a pregnant woman obtained at a health facility or in the community. SBA is defined as delivery assistance provided by a doctor, midwife or nurse. PNC refers to check-ups by a health professional or other community health worker within 42 days or six weeks of childbirth.7 PNC data were gathered from women who gave birth at a health facility and those who delivered at a place other than a health facility. Independent variables included women’s sociodemographic and health system factors such as age, parity, residence, marital status, education, household income, health insurance coverage, exposure to mass media, pregnancy intention, place of receiving care, care provider and distance to health facility.
2.2. Statistical Analysis
The extent of maternity care utilization was assessed through descriptive statistics. Chi-square tests were performed to examine unadjusted associations between independent variables and utilization of maternal health services as an outcome. Variables significant at p<0.05 were included in multiple logistic regression models to assess strength of associations after adjusting for other variables. Predictors of the continuation of care from ANC to SBA and from SBA to PNC were determined through three sequential logistic regression models. To determine predictors of ANC use during pregnancy, the first model (1) was fitted to include all women in the study who had received ANC as the outcome. Code “1” was used if a woman received at least one ANC and “0” if no care was received. Among those who received ANC, some proceeded to access skilled care at birth whilst others did not. A second logistic regression model (2) was then fitted among women who received ANC to ascertain factors associated with proceeding to access skilled care at birth after receiving ANC. The outcome of interest for the second model was “1” for receiving ANC and SBA, and “0” for receiving ANC but no SBA. After childbirth, some mothers received PNC whilst others did not. Thus, a third model (3) was fitted among mothers who received ANC, SBA and PNC to explore predictors of completing the CoC. The outcome of interest for logistic model (3) were “1” for receiving ANC, SBA and PNC and “0” for receiving ANC and SBA but not PNC.
Variables in the logistic regression models included women’s sociodemographic factors, residence, household income, health insurance cover, mass media exposure and individual factors such as pregnancy intentions, number of ANC visits and place of delivery, among others. These variables have been reported in the literature to be associated with the utilization of maternity services.20,21
The data analysis was done using STATA statistical software (Stata Corp. 2007. Stata Statistical Software Release 14. Stata Corp LP, College Station, TX, USA).
2.3. Ethical Approval
Ethical approval was obtained from the Ghana Health Service through the East Akim Health Directorate. Informed consent was obtained from each participant before data collection. Respondents were assured of confidentiality and informed of their right to opt out of the study at any time they felt uncomfortable with the questions or felt physically and psychologically harmed during the course of data collection. Anonymity was assured by using assigned codes on the questionnaire instead of for respondents.
3. Results
3.1. Sociodemographic Characterisitcs
Table 1 shows socio-demographic characteristics of women interviewed for the study. A majority of the respondents (66.5%) were between the ages of 21 to 34 years, 18.7% were below 21 years and 14.8% were 35 years and above. Most women (74.8%) had primary/junior high schooling, 13.5% had secondary education and 11.6% had no education. The majority (63.2%) of respondents were rural residents and 53.9% reported having regular access to various types of mass media. Health insurance coverage was very high (96%). With regards to marital status, a high proportion of the respondents were co-habiting (42.3%), that is, staying together as spouses but without any formal or traditional marriage rites. Respondents’ income was assessed by how much money they made in a month from their trade or work. Majority of respondents (45.2%) reported an annual income level of between 500 -1,000 Ghana Cedis (GHC), followed by those who earned less than GHC 500 with only 13.6% having their income level above GHC 1,000. It was also observed that a majority of the respondents (56.5%) lived between 5 to 10 kilometers to the nearest health facility whilst another 34.2% lived less than 5 kilometers to a health facility. The remaining 9.4% of respondents lived at a distance of more than 10 kilometers to the nearest health facility.
| Characteristics (N=310) | n (%) |
|---|---|
| Age (Years) | |
| 16 – 20 | 58 (18.7) |
| 21 – 34 | 206 (66.5) |
| 35+ | 46 (14.8) |
| Educational status | |
| None | 36 (11.6) |
| Primary/JHS | 232 (74.8) |
| Secondary or higher | 42 (13.6) |
| Marital status | |
| Married | 110 (35.5) |
| Co-habiting | 131 (42.3) |
| Single | 69 (22.3) |
| Residence | |
| Rural | 196 (63.2) |
| Urban | 114 (36.8) |
| Income status | |
| < Ghc 500 | 128 (41.3) |
| Ghc 500 - 1000 | 140 (45.2) |
| > Ghc 1000 | 42 (13.6) |
| Distance to facility | |
| < 5 Kilometers | 106 (34.2) |
| 5 To 10 kilometers | 175 (56.5) |
| > 10 Kilometers | 29 (9.4) |
| Parity | |
| 1-2 | 185 (59.7) |
| >2 | 125 (40.3) |
| Health insurance | |
| Covered | 297 (95.8) |
| Not covered | 13 (4.2) |
| Exposure to mass media | |
| Yes | 167 (53.9) |
| No | 143 (46.1) |
3.2. Antenatal, Skilled Birth Attendance and Postnatal Care Utilization
Antenatal care utilization in East Akim was found to be high. Over 98% of women who had a birth in the two years preceding the study had at least one ANC visit during pregnancy and 83.5% had four or more visits as recommended by WHO (Table 2).
| Type of care | n (%) |
|---|---|
| Antenatal care | |
| At least one visit | |
| Yes | 305 (98.4) |
| No | 5 (1.6) |
| Number of visits | |
| <4 | 51 (16.5) |
| 4+ | 259 (83.5) |
| Skilled birth attendance | |
| Yes | 228 (74.0) |
| No | 82 (26.0) |
| Place of delivery | |
| Health facility | 231 (74.5) |
| Home and others | 79 (25.5) |
| Type of skilled attendant | |
| Doctor | 41 (18.0) |
| Midwife | 111 (48.7) |
| Nurse | 76 (33.3) |
| Non-skilled attendant | |
| Traditional birth attendant | 50 (61.0) |
| Family member | 20 (24.4) |
| Self-assisted delivery | 12 (14.6) |
| Postnatal care visit | |
| Within 42 days | 267 (86.1) |
| 0 – 2 Days | 43 (16.1) |
| 3 – 7 Days | 53 (19.8) |
| 8 – 21 Days | 88 (33.0) |
| 22 – 41 Days | 83 (31.1) |
| No visit | 43 (13.9) |
| Place of receiving care | |
| Hospital /clinic | 238 (89.1) |
| Health center | 26 (9.7) |
| Private facility | 3 (1.1) |
| Postnatal care provider | |
| Doctor | 17 (6.4) |
| Midwife | 94 (35.2) |
| Nurse | 156 (58.4) |
| Combinations of mnh services received | |
| Anc+sba+pnc | 203 (65.5) |
| Anc+pnc | 64 (20.6) |
| Anc+sba | 23 (7.4) |
| Anc only | 16 (5.1) |
| Pnc only | 2 (0.7) |
| Sba+pnc | 0 (0.0) |
| Sba only | 0 (0.0) |
| None | 2 (0.7) |
In the East Akim Municipality, 74.5% of respondents reported having institutional deliveries for their most recent births, and almost all women who delivered at a health facility were assisted by a skilled birth attendant (doctor, nurse or midwife) except for 1.7% who had self-assisted delivery because labor was instantaneous before any health worker could assist. In contrast, all women who gave birth at home (26%), were assisted by Traditional Birth Attendants (61.0%) and relatives (24.4%) or self-assisted (14.6%). Almost all institutional deliveries (99%) occurred in public health facilities with only 1% occurring at private health facilities.
A majority of the respondents (86.1%) had a postnatal visit within 42 days after birth in a health facility. Government hospitals, clinics and primary health care facilities were the predominant place of choice for postnatal care services (98.9%) and 1.1% visited private health facilities for their postnatal visits. With regards to care providers, Nurses were the predominant providers of postnatal care, attending to about half of all mothers (58.4%); followed by Midwives (35.2%) and Doctors (6.4%). With regards to the timing of postnatal care, the study found that only 36% of mothers who had a postnatal visit accessed care within the first 7 days after birth. Majority of the mothers reported to the health facility after the first week following birth - 33% accessed care within 8 to 21 days; and 31% reported between 22 to 41 days after birth.
3.3. Completion of Maternal and Newborn Health Continuum of Care
Figure 1 shows the proportion of women accessing antenatal, childbirth and postnatal care services and the attrition occurring along the CoC. While 98% of women received at least one antenatal care visit for their last pregnancy occurring within the last 24 months, only 74% continued to access skilled care at birth, indicating a 24% attrition in the CoC from ANC to childbirth. After delivery, 14% of mothers failed to access postnatal care. Cumulatively, only 66% of mothers accessed the full range of services within the MNH CoC.
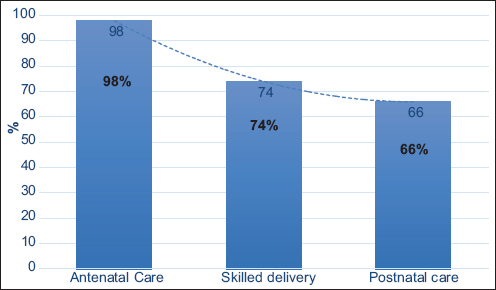
- Proportion of mothers who utilized the full complement of antenatal, skilled birth attendance and postnatal care services and the attrition occurring along the continuum of care
The proportion of women who received various combinations of maternity services are presented in Table 2. The results indicate that 65.5% of women received all three services within the MNH CoC, while 20.6% of women had at least one ANC visit and PNC but did not access SBA. A few mothers (7.4%) received ANC and SBA but did not receive PNC; 5% received only ANC; 0.7% received PNC alone; and 0.7% did not receive any of the services within the CoC. However, none of the respondents received SBA alone without ANC or PNC.
3.4. Factors Influencing Utilization of Maternal and Newborn Health Continuum of Care
Three logistic regression models were fitted to determine factors influencing utilization of maternity services along the CoC. Table 3 presents the results. In each model, variables which were significant at p-value<0.05 in the bivariate analysis were included. The odds ratios reported are all adjusted for confounding effect.
| Variables | Model 1 ANC | Model 2 ANC + SBA | Model 3 ANC+SBA+PNC | |||
|---|---|---|---|---|---|---|
| AOR 95%CI | AOR 95%CI | AOR 95%CI | ||||
| Age in years (ref <21) | ||||||
| 21-34 | 2.0 | 0.95 - 4.06 | 0.6 | 0.26 - 1.61 | 0.8 | 0.19 - 3.20 |
| 35+ | 2.1 | 0.69 - 6.36 | 0.8 | 0.20 - 3.01 | 2.0 | 0.13 - 30.87 |
| Education (ref=No education) | ||||||
| Primary/JHS | 0.7 | 0.30 - 1.62 | 3.7* | 1.52 - 8.94 | --- | --- |
| Secondary or Higher | 1.3 | 0.37 - 4.62 | 19.8* | 2.18 -178.80 | ||
| Residence (ref=Rural) | ||||||
| Urban | 1.6 | 0.89 - 3.00 | 8.6* | 3.33 - 22.08 | 4.8* | 1.21 - 19.28 |
| Distance to Facility (ref=>10 km) | ||||||
| < 5 kilometers | 2.0 | 0.41 - 2.75 | 0.8 | 0.28 - 2.16 | 7.5* | 1.54 - 36.52 |
| 5 to 10 kilometers | 1.4 | 0.80 - 2.64 | 0.9 | 0.32 - 2.74 | 6.2* | 1.27 - 30.12 |
| Income status (ref=No income) | ||||||
| High income | 1.1 | 0.41 - 2.75 | 1.3 | 0.37 - 4.48 | 1.5 | 0.15 - 14.33 |
| Low to medium | 1.5 | 0.80 - 2.64 | 1.2 | 0.61 - 2.35 | 2.0 | 0.61 - 6.38 |
| Health Insurance (ref=No) | ||||||
| Yes | 1.1 | 0.25 - 4.92 | 3.4 | 0.62 - 18.48 | --- | --- |
| Parity (ref= >2) | ||||||
| 1-2 | 1.1 | 0.63 - 2.23 | 2.0 | 0.96 - 4.01 | 1.6 | 0.46 - 5.5 |
| Exposed to media (ref=No) | ||||||
| Yes | 1.3 | 0.75 - 2.25 | 0.8 | 0.44 - 1.56 | 6.0* | 1.72 - 21.01 |
| Intended Pregnancy (ref=No) | ||||||
| Yes | 2.0* | 1.11 - 3.73 | 1.1 | 0.56 - 2.34 | 2.1 | 0.60 - 7.73 |
| Had 4+ ANC visits (ref=No) | ||||||
| Yes | 2.5* | 1.31 - 4.80 | 1.0 | 0.32 - 2.90 | ||
| Delivery at a facility (ref=No) | ||||||
| Yes | 9.5* | 2.49- 98.59 | ||||
| Number of women (N) | 310 | 305 | 267 | |||
The first model (1) analyzes predictors of ANC utilization in the East Akim municipality. The results show that ANC use was significantly associated with intended pregnancy after adjusting for confounding. Variables such as age, distance to health facility, educational level, residence, income status, health insurance and parity were not significant predictors of ANC utilization in the multi-logistic regression model.
The second model (2) analyzes the predictors of SBA utilization among women who received ANC. Factors related to ANC utilization such as number of visits are introduced into this logistic model and in addition to variables included in first model (1). The results showed that use of SBA was significantly associated with educational level, urban residence and number of ANC visits. Educational level was the strongest predictor of SBA utilization. The odds of using SBA were almost 20 times higher for women with secondary or tertiary education than for women with no formal education. Residence was also found to be a significant predictor of SBA utilization. The odds of skilled delivery were almost 9 times higher for women who live in urban areas than those who live in rural areas. Women who had four or more ANC visits had 2.5 times higher odds of accessing SBA compared with women who had less than four visits.
The third Model (3) estimates the predictors of postnatal care utilization among mothers who received both ANC and SBA. All the variables in the second Model (2) were retained in the third Model (3) except for educational level and health insurance coverage because they were found to have no significant association in the bivariate analysis; and place of delivery is also added to the third Model (3). Four variables appeared to be significant predictors of postnatal care utilization among women who received ANC and SBA - residence, distance to health facility, place of delivery and exposure to media information. Mothers resident in urban areas were 4.8 times more likely to go for postnatal checks than those in the rural areas (AOR:4.8; 95% CI: 1.21-19.28). With regards to distance, mothers who lived less than 5 kilometers to a health facility had 7.5 times higher odds of accessing postnatal care than those who lived more than 10 kilometers to the nearest health facility (AOR: 7.5; 95% CI:1.54-36.52), and 6 times more likely to access postnatal care than those who lived 5 to 10 km from a health facility (AOR: 6; 95% CI:1.27-30.12). Mothers exposed to media were 6 times more likely to access postnatal care (AOR: 6; 95% CI:1.72-21.01). Delivery at a health facility was found to be a very strong predictor of postnatal care utilization within 42 days following childbirth. Mothers who delivered in a health facility were almost 10 times more likely to access postnatal care (AOR: 9.5; 95% CI:2.49-98.59).
4. Discussion
Maternal and newborn health interventions are most effective when they are based on the continuum-of-care approach. The approach calls for a service delivery system which brings together all the three components of maternal and newborn health services, namely antenatal, childbirth and postnatal care with high quality services at all levels. To ensure effectiveness of the CoC approach for improving the health and survival of women and their newborns, it is imperative to understand the factors influencing utilization of these services in various settings, the gaps as well as reasons for attrition along the pathway of the CoC for improvement.
4.1. Discussion of Results
In this study, we found that despite almost universal ANC attendance for at least one visit (98.4%), a significant proportion of mothers did not access SBA after ANC. Only 74% continued to access SBA, indicating a 24% attrition in the CoC from pregnancy to childbirth. After childbirth, 14% of mothers failed to access postnatal care. Consequently, only 66% of mothers accessed the full complement of maternity services within the continuum-of-care, with attrition rates being higher between ANC and SBA (24%) than between SBA and PNC (8%). The results for ANC and SBA compare well with those from a similar study by Yeji et al. (2015) in three districts of Ghana, which reported utilization rates of 86.1% for ANC4+ and 75.6% for SBA.18 They also recorded PNC utilization rates of 25.4% within 48 hours after childbirth, 52.4% at 2 weeks and 90.6% at 6 weeks, resulting in a continuum-of-care (CoC) completion rate of only 8%, using the PNC utilization rate within 48 hours after delivery as the CoC completion criteria. In our study, 16% of PNC attendees reported within 48 hours; 20% reported within 3 to 7 days; 33% within 8 and 21 days; and 31% reported within 22 to 41 days after childbirth. Although 86.1% of mothers had a postnatal visit within 42 days after childbirth in a health facility only 66% received all three services (ANC, SBA, PNC) within the MNH CoC resulting in a 66% CoC completion rate. The observations from our study also compare well with those from a population-based survey in Cambodia by Wang and Hong,8 which reported that 71% of women were able to access the full complement of MNH services from pregnancy through childbirth to postnatal care.
Receiving four or more ANC visits and residence were found to be significant predictors of subsequent use of SBA (p-value 0.005 and <0.001 respectively). A similar finding was reported by Jacobs et al. in a study among remote and poor rural communities of Zambia, where adequate ANC utilization in previous pregnancies was found to be a significant predictor of SBA utilization (OR, 4.48; 95% CI, 2.38–8.43).22 Compared to women who lived in remote areas, women in rural communities were 2.72 (OR 2.57; 95% CI: 1.37–6.82) times more likely to access SBA. Results from Cambodia also demonstrated a significant association between four or more antenatal visits and subsequent use of SBA. Thus, women who had four or more ANC visits had two times the odds of accessing SBA (AOR:2.0; 95% CI: 1.7-2.4).8 These observations compare well with the findings of this study. When women receive quality ANC, they become well informed about pregnancy and childbirth and are more likely to appreciate the benefits of skilled care at birth.
In this study, 89.6% of the mothers who accessed skilled birth attendance proceeded to access postnatal care. Although this shows the influence of skilled delivery on postnatal visits, the study also revealed that about 76% of the women who did not access SBA visited the health facility for PNC. This observation demonstrates that some women choose to utilize PNC services after having home deliveries. However, none of the respondents in this study received SBA without ANC, thus underscoring the importance of ANC as a catalyst for SBA.
The study found significant socio-demographic inequalities in the use of maternity services in the East Akim municipality. Women from urban communities were 1.6 times as likely to use ANC and 8.6 and 4.8 times as likely to use SBA and PNC respectively, compared with women from the rural communities. Over 90% of women who received ANC and over 70% of women who gave birth at health facilities reported receiving these services in public hospitals. This may be due to the availability of very few private health facilities in the municipality, which are perceived to be expensive and therefore patronized by the few women who can afford their services. Private health services are an important component of Ghana’s health system as they contribute significantly to healthcare provision across the country. Thus, the government may need to proactively engage private providers in developing a public-private partnership to provide quality and affordable maternal health services.
Regarding the use of skilled birth attendance, the study found significant associations with educational level, residential status and four or more ANC visits. These factors have been reported by several studies as predictors of SBA utilization.8,23 Among women who received ANC and SBA, predictors of continuation to PNC and completion of the continuum-of-care included residence, distance to health facility, delivery at a health facility and exposure to mass media (television, radio, internet, newspaper). In Bangladesh, women living in rural areas were less likely to complete the continuum-of-care compared to those from urban settings.24 Nepalese women with higher wealth status and access to media had higher odds of accessing the continuum-of-care from pregnancy, through childbirth to the postnatal period.25 In Ghana, geographical location, level of education and religion have been found to be significantly associated with completion of the CoC for MNH.18
Ghana has been fairly successful at expanding coverage of maternal health services across the country, as demonstrated by the current study in East Akim where 66% of mothers surveyed patronized the full complement of maternal and newborn health services from pregnancy, through childbirth to postnatal care. However, efforts are still needed to increase the proportion of women who receive the full complement of maternal and newborn health services from antenatal care during pregnancy through skilled birth attendance to postnatal care. The outcome of this and other studies can inform the development of effective strategies for improving utilization of the MNH continuum-of-care to achieve desired MNH outcomes.
4.2. Limitations
This study provides useful data on the prevailing pattern of maternal health services utilization in the East Akim Municipality of Ghana, and a basis for strengthening the health system to ensure equitable access to effective interventions for improving MNH outcomes. However, the study relied on self-report from respondents, thereby enhancing the potential for information error. This potential bias was minimized by verifying the authenticity of information provided in the respondents’ health cards and records.
4.3. Recommendation for Further Studies
Similar studies on the level and determinants of the MNH continuum-of-care utlization, especially in developing country contexts and deprived communities are needed, given the dearth of information on factors influencing utilization of the full complement of MNH services in different settings.
5. Conclusion and Global Health Implications
The study finds a remarkable utilization of maternal health care services in the East Akim Municipality of Ghana. Two-thirds (66%) of mothers utilized the full complement of the continuum of MNH services. Distance from a health facility, urban residence and exposure to mass media were found to be strong predictors of the full complement of continuum of MNH care utilization. These findings are salient to national and global efforts at improving maternal and newborn health and survival. Understanding the factors which influence the uptake of MNH interventions in various contexts is essential for the development of national strategies that are aligned to national needs and resources.
At the local level, efforts should focus on extending outreach services to rural and hard-to-reach areas of the municipality where utilization of MNH services was found to be relatively low. Whereas outreach services can be effective in improving access and utilization of ANC and PNC services, SBA utilization will require access to health facilities with obstetric care capabilities. This can be achieved through equitable allocation of national resources, including the distribution of health facilities and strengthening of health systems to deliver the full complement of quality maternal and newborn health services. Evidence from this study and similar studies from other countries can enhance our understanding of the determinants of MNH services utilization and inform a comprehensive strategy for achieving universal access and utilization of MNH services as part of global efforts to improve MNH outcomes.
Acknowledgements:
We express our gratitude to the leadership of the Municipal Health Directorate of East Akim, Eastern Region for their support and cooperation. We thank Dr. Keitum from Kyebi Government Hospital for providing technical support to the team. The authors are grateful to the traditional leaders, Community Health Volunteers and study participants for their support and participation in this study.
Compliance with Ethical Standards
Conflicts of Interest: The authors declare that they have no conflicts of interest.
Funding/Support: The study was supported by the authors with no external funding.
Ethical approval: Ethical approval was obtained from the Ethics Review Board of the Ghana Health Service through the East Akim Health Directorate.
Disclaimer: None.
References
- Bank Group and the United Nations Population Division. Washington, DC: World Bank Group; 2019. p. :2.
- Levels and Trends in Child Mortality 2019:Estimates Developed by the UN Inter-agency Group for Child Mortality Estimation. New York: United Nations Children's Fund; 2019.
- Disease and mortality in sub-Saharan Africa (2nd ed). Washington DC: The International Bank for Reconstruction and Development / The World Bank; 2006.
- Continuum of care for maternal newborn, and child health:from slogan to service delivery. Lancet. 2007;370(9595):1358-1369.
- [Google Scholar]
- Mortality due to low-quality health systems in the universal health coverage era:a systematic analysis of amenable deaths in 137 countries. Lancet. 2018;392(10160):2203-2212.
- [Google Scholar]
- Opportunities for Africa's Newborns:Practical data policy and programmatic support for newborn care in Africa. (authors/editors:J Lawn &K. Kerber). Geneva, Switzerland: WHO on Behalf of the Partnership for Maternal Newborn and Child Health; 2006.
- Pregnancy Chilbirth, Postpartum and Newborn Care:a Guide for Essential Practice (3rd ed). Geneva, Switzerland: World Health Organization; 2015.
- Levels and determinants of continuum of care for maternal and newborn health in Cambodia-evidence from a population-based survey. BMC Pregnancy Childbirth. 2015;15(62):1-9.
- [Google Scholar]
- Standards for improving quality of maternal and newborn care in health facilities. Geneva, Switzerland: World Health Organization; 2016.
- 2016 Annual Report. Accra: Ghana Health Service; 2017. p. :1.
- Accra. Ghana: UNICEF-Ghana; 2019.
- Accra. Ghana: GSS, GHS and ICF; 2018.
- Adequacy of prenatal care and neonatal mortality in infants born to mothers with and without antenatal high-risk conditions. Aust N Z J Obstet Gynaecol. 2007;47(2):122-127.
- [Google Scholar]
- 2002. WHO Antenatal Care Randomized Trial:Manual for Implementation of the New Model. Geneva, Switzerland: World Health Organization; https://apps.who.int/iris/handle/10665/42513
- The World Health Report 2005:Make Every Mother and Child Count. Geneva, Switzerland: World Health Organization; 2005.
- Strategies for reducing maternal mortality in developing countries:What can we learn from the history of the industrialized West? Trop Med Int Health. 1998;3(10):771-782.
- [Google Scholar]
- Continuum of care in a maternal, newborn and child health program in Ghana:Low completion rate and multiple obstacle factors. PLoS One. 2015;10(12):1-23.
- [Google Scholar]
- East Akim Municipal October 2014
- Determinants of skilled birth attendants for delivery in Nepal. Kathmandu Univ Med J. (KUMJ). 2010;8(31):325-332.
- [Google Scholar]
- Determinants of maternal health services utilization in urban settings of the Democratic Republic of Congo--a case study of Lubumbashi City. BMC Pregnancy Childbirth. 2012;12:66.
- [Google Scholar]
- Predictors of antenatal care skilled birth attendance and postnatal care utilization among the remote and poorest rural communities of Zambia:A multilevel analysis. Frontiers in Public Health. 2017;5:11.
- [Google Scholar]
- Factors associated with postnatal care for newborns in Zambia:Analysis of the 2013-14 Zambia demographic and health survey. BMC Pregnancy Childbirth. 2017;17(1):418.
- [Google Scholar]
- Practices and determinants of delivery by skilled birth attendants in Bangladesh. Reproductive Health. 2014;11(1):1-7.
- [Google Scholar]
- Correlates of continuum of maternal health services among Nepalese women:Evidence from Nepal multiple indicator cluster survey. PLoS One. 2019;14(4):1-11.
- [Google Scholar]





