Translate this page into:
Barriers towards the Prevention and Treatment of Malaria among Pregnant Women at the Nkwen Health Center Bamenda, Cameroon
*Corresponding author email: ngwayuclaude1@gmail.com
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 4.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Malaria remains an important public health problem such that, assessing the challenges experienced among pregnant women (vulnerable) with the uptake of malaria prevention methods and treatment is pertinent. This hospital-based cross-sectional descriptive study that was carried out at a Medicalized Health Center in Nkwen, Cameroon, sought to assess the barriers to malaria prevention faced by 51 pregnant women who attended antenatal clinic (ANC). Over 88% of participants were 15-30 years old. All participants knew at least one symptom of malaria, with 20% of them confirmed to have taken intermittent preventive treatment in pregnancy (IPTp) and 53% reported using insecticide-treated bed net (ITN). Educating pregnant women and their spouses on the uptake of IPTp and the use of ITN is a key strategy to curb its high malaria morbidity and mortality rates.
Keywords
Barriers
Pregnant Women
Malaria Prevention
Treatment
Nkwen Health Center
Cameroon
1. Introduction
Despite the availability of different methods to prevent malaria,1 it remains an important public health problem in tropical regions around the world and especially in Sub-Saharan Africa. According to the World Health Organization (WHO), in 2017 approximately 219 million people were infected with the malaria parasite in 87 countries around the world.1 In the WHO African region, 435,000 people died from this infestation with 93% of these deaths occurring in African countries. Children below the age of 5 and pregnant women are the most vulnerable groups and are at higher risk of developing severe complications.2 Malaria prevention has been identified as a key strategy to curb its high morbidity and mortality especially in resource-poor communities around the world. Vector control and preventive therapies are available and widely used methods of prevention.3 WHO reported that household ownership of at least one Insecticide-Treated Nets (ITN) increased from 50% in 2010 to 80% in 2016 but the proportion of households with sufficient mosquito nets (one ITN for every two persons) is at 43% which is still inadequate.4 Though the coverage of eligible pregnant women with IPT increased from 13% in 2014 to 18% in 2017 in the 23 African countries that reported, it is however still not sufficient as more than 80% of pregnant women are still at risk of being infected with malaria4 and the rate of transmission is higher in areas with lower coverage.5 In Cameroon, malaria continues to be endemic and the first major cause of morbidity and mortality among pregnant women.4 Identifying the barriers that limit access to malaria prevention and treatment in pregnant women in malaria-endemic regions is pertinent to improving malaria prevention. This study, therefore, sought to assess the barriers (factors that hinder malaria prevention uptake) of malaria prevention faced by pregnant women who attend an antenatal clinic (ANC) at the Nkwen Health Center, Bamenda in the Northwest Region of Cameroon.
2. Methods
2.1. Study Data Collection
Data were collected from all consented participants in this hospital-based crossed sectional study in Nkwen Health Center Bamenda in the Northwest region of Cameroon, using a structured pretested questionnaire administered and filled by the healthcare provider. Socio-demographic characteristics of participants, data on ANC attendance, malaria treatment, prevention, and prescribers were captured with the questionnaire by the trained data collector. This study was made up of a total of 51 pregnant women attending ANC at Nkwen Health Center during the visiting hours and over three weeks.
2.2. Data Cleaning and Data Analysis
Data were entered, verified, and cleaned before analyses using Excel. Descriptive data analysis which is the basic virtual of any quantitative analysis was used. Thus, this simply a way to describe our data was done by calculating means, frequency distributions, and percentages. The summarized data was made in a meaningful way by presenting in tables and charts.
2.3. Ethical Approval
Ethical approval was obtained from the Institutional Review Board (IRB) of the Cameroon Baptist Convention Health Services (CBCHS).
3. Results
3.1. Sociodemographic Characteristics
The majority of our study participants (88%) were between the ages of 15-30 years while the remaining 12% were between 36- 40 years old. Over 58% of the women were in the 3rd trimester of their pregnancy and 41.7% were prima gravidae (Table 1).
| Variable | Frequency (N) | Percentage (%) |
|---|---|---|
| Age Range (in years) | ||
| 15-20 | 15 | 29.4 |
| 21-25 | 18 | 35.2 |
| 26-30 | 12 | 23.4 |
| 31-35 | 3 | 5.88 |
| 36-40 | 3 | 5.88 |
| Total | 51 | 100 |
| Marital Status | ||
| Married | 33 | 64.7 |
| Single | 6 | 11.7 |
| Separated | 6 | 11.7 |
| Divorce | 3 | 5.5 |
| Widow | 3 | 5.5 |
| Total | 51 | 100 |
| Gestational Age (in months) | ||
| 0-3 | 6 | 11.7 |
| 4-6 | 15 | 39.4 |
| 7-9 | 30 | 58.2 |
| Total | 51 | 100 |
| Gravidity | ||
| 1st pregnancy | 24 | 47.1 |
| 2nd pregnancy | 12 | 23 |
| More than 2 | 15 | 29 |
| Total | 51 | 100 |
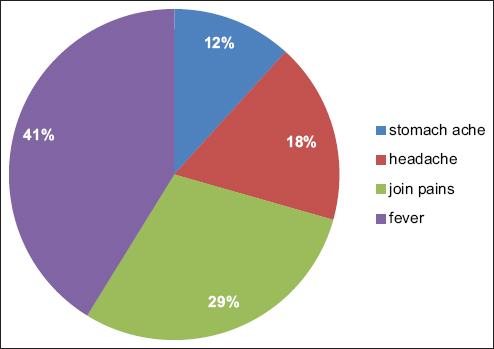
All the women knew at least one or more symptoms of malaria in pregnancy with the most common reported symptoms being fever (41%) and joint pains (29%) (Figure 1).
- Knowledge of symptoms of malaria
3.2. Health Seeking Behavior and Intermittent Preventive Treatment of Malaria (IPTp) Use During Pregnancy
Only 19.6% of the women reported having used Intermittent Preventive Treatment of Malaria (IPTp) during the pregnancy; 15.6% (8) were not sure if they received it or not while the remaining 64.7% indicated not to have used it. Over 29.4% of our study participants reported that they seek formal health care every time they present with symptoms of malaria such as fever; another 29.4% seek formal care occasionally; while the remaining 41.1% indulged in self-medication. The majority of the women (64.1%) were not on malaria treatment as at the time of the interview, while those on treatment 10 (19.6%) consulted with either a doctor, 38 (75%) or a nurse 3 (4.4%). A greater proportion of the women attended the clinics only when they had a chance and this could be one of the reasons for the barriers (Table 2).
| Variable | Frequency (N) | Percentage (%) |
|---|---|---|
| Those on malaria treatment | ||
| Yes | 10 | 19.6 |
| No | 33 | 64.7 |
| Do not think so | 8 | 15.6 |
| Total | 51 | 100 |
| Prescription of malaria treatment | ||
| Doctor | 7 | 70 |
| Nurse | 3 | 30 |
| Total | 10 | 100 |
| ANC attendance | ||
| Always | 15 | 29.5 |
| Sometimes | 12 | 23.5 |
| Once | 6 | 11.7 |
| When available or chanced | 18 | 35.2 |
| Total | 51 | 100 |
3.3. Use of Insecticide-Treated Bed Nets (ITN)
Fifty-three percent of the women reported using ITN frequently as a means of vector control; 17.6% use it occasionally; while 29.4% did not use it at all. Among those who reported not using ITNs, 40% of them did not see the need while the remaining 60% gave reasons such as their partners did not like it and that it made them feel a lot of heat at night (Table 3).
| Variables | Frequency (N) | Percentage (%) |
|---|---|---|
| Consultations when having fever | ||
| Yes | 15 | 29.4 |
| No | 21 | 41.1 |
| Sometimes | 15 | 29.4 |
| Total | 51 | 100 |
| Use of ITN | ||
| Yes | 27 | 52.9 |
| No | 15 | 29.4 |
| Sometimes | 9 | 17.6 |
| Total | 51 | 100 |
4. Discussion, Conclusion, and Global Health Implications
In this study, we examined the barriers to malaria prevention and treatment faced by pregnant women who attend ANC at the Nkwen Medicalized Health Center Bamenda, Cameroon. Eighty-eight percent of our study participants were within the age range of 15-30 years. This finding is as expected given that these are women of reproductive age and the age during which the majority of women go for marriage in the African setting. We found that the majority of the women at ANC were in the 3rd trimester and this finding could be attributed to the fact that a greater number of pregnant women in developing regions begin ANC late as shown in some studies.6,7
Fever is known to be one of the most common symptoms8 of malaria and the majority of the women could recognize fever (41%) and joint pains (29%) as symptoms of malaria. In all 19.6% (10) of the women were on malaria treatment at the time of the interview, and 70% of them said their malaria was diagnosed and being treated by a doctor while the remaining 30% reported that they were treated by nurses. This finding may just be a depiction of the fact that many cases of malaria in pregnancy are missed as the majority of healthcare providers attending to women at ANC are nurses and midwives who may not pay as much attention to minute details as medical doctors would. The majority of our respondents acknowledged owning at least one ITN in their home and this results from the fact that Cameroon’s Ministry of Public Health distributes ITNs to homes regularly. However, 70% (of them use these nets, and a quarter of them do not use them frequently). The majority in the remaining 30% who do not use ITN said they do not see the importance while some reported that their spouses were not comfortable sleeping under the ITN. This differs slightly from what was obtained in a qualitative study in Ethiopia where the respondents said they do not use ITN because they did not see a lot of mosquitoes around and did not view malaria as a big problem.9
Only about 20% of our study participants could confirm that they had received IPTp (sulfadoxine-pyrimethamine) and 16% were not sure if they received it or not. This finding was, however, contradictory to a similar study carried out in Cameroon which showed that more than 80% of women at ANC received IPTp against malaria.10 This difference may be explained by the fact that our sample was smaller and may not fully reflect the overall reality. In addition, we did not exclude women who were not eligible for IPTp such as those who are were still in the first trimester of pregnancy. Close to 20% of women in the study were diagnosed and being treated for malaria which is not very different from the prevalence of malaria in pregnancy as reported in a study carried out in Uganda.11
Study Limitations
This study had a small sample size and was hospital-based which may have limited the scope and impacted the results we see. We relied on self-reported knowledge by the study participants and some of them were not literate. This may have brought about bias in the information we obtained and reported in the results.
Future studies with mixed designs involving explanatory and exploratory approaches with significant sample sizes should be carried out to establish how to increase access to IPTp-SP in all areas with moderate to high malaria transmission in Africa, including Cameroon as part of antenatal care services. WHO recommends a schedule of at least four antenatal care visits during pregnancy.
The majority of pregnant women attending ANC at the Health Center Nkwen can identify fever and joint pains as common symptoms of malaria. The utilization of malaria prevention methods is still very low among pregnant women attending ANC at CMA Nkwen, Bamenda. The vector control method (mainly the use of ITN) is the most commonly used malaria prevention method compared to IPTp. The majority of the women and their spouses do not see the need to sleep under ITN. More efforts are therefore needed to sensitize the population as a whole on the importance of malaria prevention and more prevention methods should be made available to them.
Acknowledgments:
We are grateful to the women who took part in this study.
Compliance with Ethical Standards
Conflicts of Interest: The authors declare that they have no competing interests.
Financial Disclosure: Nothing to Declare.
Funding/Support: There was no funding for this study.
Ethics Approval: Ethical clearance was obtained from the Institutional Review Board (IRB) of the Cameroon Baptist Convention Health Services.
Disclaimer: The authors are responsible for the views expressed in this article, which do not necessarily represent the views, decisions, or policies of the institutions with which they are affiliated. Publication Support: The publication of this article was fully supported by the Global Health and Education Projects, Inc. (GHEP) through the Emerging Scholar’s Grant Program (ESGP). The information, contents, and conclusions are those of the authors and should not be construed as the official position or policy of, nor should any endorsements be inferred by ESGP or GHEP.
References
- Malaria eradication within a generation:ambitious, achievable, and necessary. Lancet. 2019;394(10203):1056-112. doi:10.1016/S0140-6736(19)31139-0
- [Google Scholar]
- Malaria in pregnancy:a passive surveillance study of pregnant women in low transmission areas of Colombia, Latin America. Malar J. 2016;15(1):66. doi:10.1186/s12936-016-1125-9
- [Google Scholar]
- Prevention efforts for malaria. Curr Trop Med Rep. 2018;5(1):41-50. doi:10.1007/s40475-018-0133-y
- [Google Scholar]
- Assessment of malaria as a public health problem in and around Arjo Didhessa sugar cane plantation area, Western Ethiopia. BMC Public Health. 2020;20(1):655. doi:10.1186/s12889-020-08784-5
- [Google Scholar]
- Coverage of malaria protection in pregnant women in sub-Saharan Africa:a synthesis and analysis of national survey data. Lancet Infect Dis. 2011;11(3):190-207. doi:10.1016/S1473-3099(10)70295-4
- [Google Scholar]
- Early antenatal care visits:a systematic analysis of regional and global levels and trends of coverage from 1990 to 2013. Lancet Glob Health. 2017;5(10):e977-83. doi:10.1016/S2214-109X(17)30325-X
- [Google Scholar]
- Gestational age at booking for antenatal care in a tertiary health facility in north-central, Nigeria. Niger Med J. 2012;53(4):236-9. doi:10.4103/0300-1652.107602
- [Google Scholar]
- Clinical manifestations of Plasmodium falciparum malaria experimentally induced by mosquito challenge. J Infect Dis. 1997;175(4):915-20. doi:10.1086/513990
- [Google Scholar]
- Factors associated with use and non-use of mosquito nets owned in Oromia and Amhara Regional States, Ethiopia. Malar J. 2009;8(1):264. doi:10.1186/1475-2875-8-264
- [Google Scholar]
- Factors associated to the use of insecticide-treated nets and intermittent preventive treatment for malaria control during pregnancy in Cameroon. Arch Public Health. 2016;74(1):5. doi:10.1186/s13690-016-0116-1
- [Google Scholar]
- Impact of malaria during pregnancy-on-pregnancy outcomes in a Ugandan prospective cohort with intensive malaria screening and prompt treatment. Malar J. 2013;12(1):139. doi:10.1186/1475-2875-12-139
- [Google Scholar]





