Translate this page into:
COVID-19 Pandemic: Marked Global Disparities in Fatalities According to Geographic Location and Universal Health Care
✉Corresponding author email: deepa.dongarwar@bcm.edu
-
Received: ,
Accepted: ,
Abstract
Since its outbreak, COVID-19 pandemic has been the biggest global concern with exponentially increasing number of cases and associated deaths across all habitable continents. Various countries around the world with their diverse health care systems, have responded to the pandemic in very distinctive ways. In this paper, we: compared COVID-19 mortality rates across global geographic regions; and assessed differences in COVID-19-related case fatality rate (CFR) based on presence or absence of Universal Health Coverage (UHC). We found that as of May 6, 2020, Europe had experienced the highest CFR globally of 9.6%, followed by 5.9% in North America. Although the pandemic originated in Asia, the continent ranked second to the last in terms of CFR (3.5%). Countries with UHC had lower number of cases of 37.6%, but the CFR of countries with UHC was twice that of countries without UHC (10.5% versus 4.9%). In conclusion, UHC does not appear to protect against mortality in a pandemic environment such as with COVID-19.
Keywords
COVID-19
Global disparity
Universal Health Coverage
Case fatality rate
1. Background
Since the emergence of the coronavirus disease-19 (COVID-19) towards the end of 2019, the disease has gained extraordinary global attention due to the exponential increase in number of cases and fatalities associated with the disease within such a short period of time. The World Health Organization (WHO) declared the disease as a pandemic on March 11,2020 and it is the first such declaration since the 2009 H1N1 swine flu outbreak. As of May 6, 2020, there have been 3,780,513 cases, with a mortality rate of 6.9%, much higher than the initial estimates of 2% provided by the WHO.1 The disease has spread and affected several countries and territories in a variety of ways. The outbreak that began in China engulfed all the continents (except Antarctica) within three months of the first reported case;2 and so far, it has caused more than 261,000 deaths worldwide. Structural configurations within the health delivery systems in affected countries may play a vital role in mitigating deleterious outcome from the pandemic, but research or data supporting this are lacking3. We hypothesize that countries with universal health care (UHC) will perform better in mitigating COVID-19 related mortality.
2. Methods
The information used for our analysis was collected from Worldometer, which is a reference website reputed by the American Library Association as one of the best free online reference sources in the world.4 Worldometer gathers and compiles the information on COVID-19 from various sources, including governments' communication channels and reliable sources of local media; it has been providing live updates on COVID-19 related total cases, new cases, deaths, new deaths, recoveries and critical cases by country, territory or conveyance.
We classified the impacted countries into the following habitable geographic regions: (1) Asia, (2) Africa, (3) Australia (including countries belonging to Oceania), (4) Europe, (5) North America (including Central American countries) and (6) South America. We then calculated the total number of cases, deaths and case fatality rate (CFR) for these geographic regions. Countries with more than 5,000 cases of COVID-19, as of May 6, 2020, were classified as ‘high impact countries.’ Furthermore, we categorized the high impact countries based on whether or not they had UHC. 5 We calculated and compared the total number of COVID-19 cases, associated deaths and CFR of countries with UHC versus those without UHC.
3. Results
A total of 213 countries had been affected by the disease as of May 6, 2020. We found that the highest number of cases of COVID-19 were identified in Europe (1,520,412) accounting for 40.2% of all cases, followed by North America which claimed 35.9% of the total cases. Europe also had the highest proportion of all deaths (55.8%). When we compared the CFR across the different regions, we observed that although Asia had the third highest number of cases (601,748) in the world, its CFR ranked as the second lowest (3.5%) after Australia (1.4%); ranked lowest) (Figure 1). A total of 54 countries had more than 5,000 cases, out which 22 countries had a UHC system (40.7%). When these high impact countries were compared based on the presence of UHC or non-UHC, we found that countries with UHC had 13,789,891 cases, which was about 37.6% of all the cases reported globally. However, the countries with UHC experienced a much higher proportion of fatalities (56.4%). The CFR of countries with UHC (10.5%) was more than double that of countries without UHC (4.9%) (Figure 2).
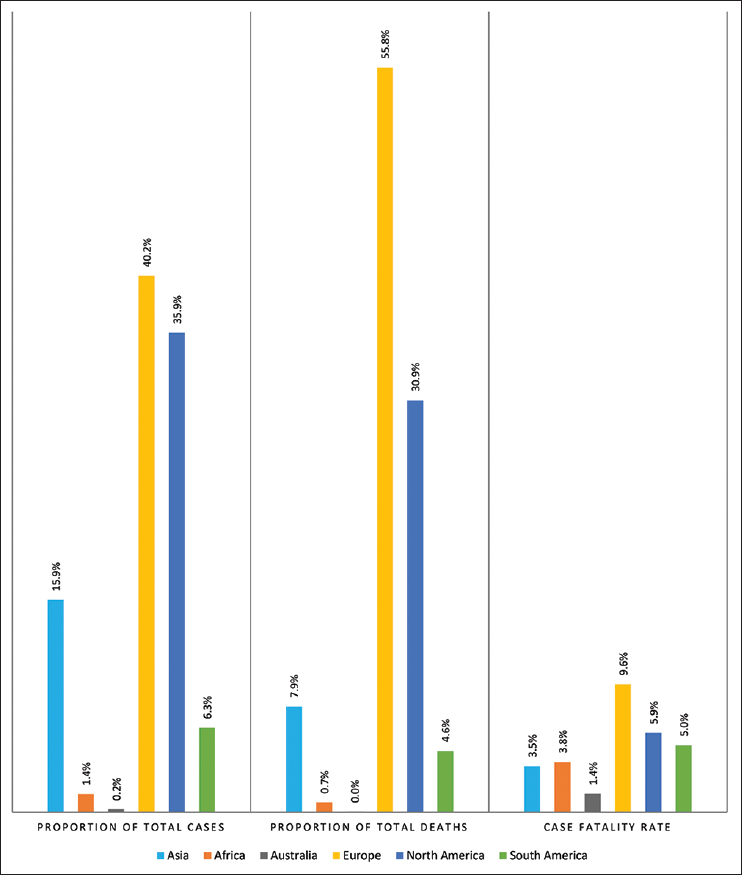
- COVID-19 cases, deaths and case fatality rate by continents
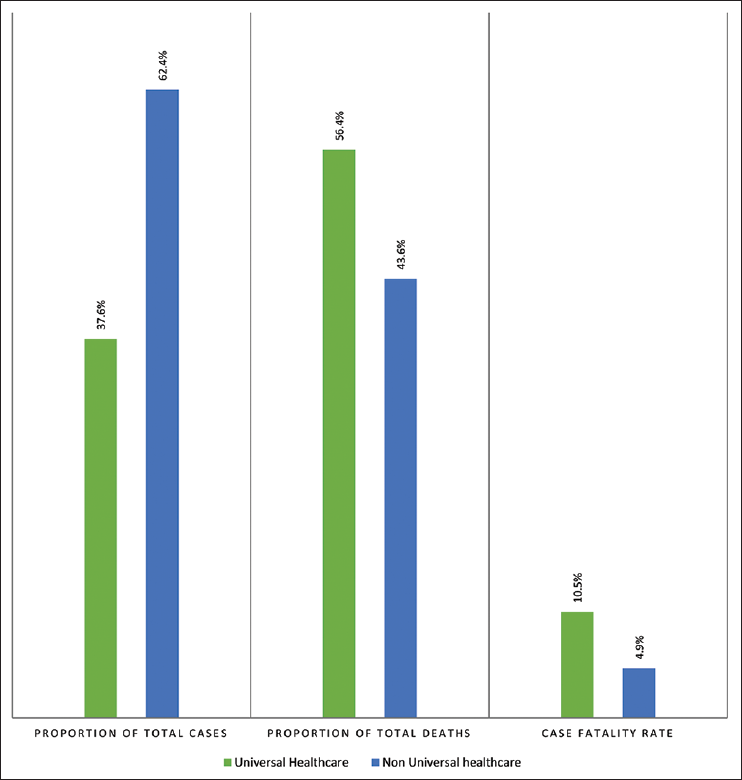
- COVID-19 cases, deaths and case fatality rate by Universal Health Coverage (UHC) among high impact countries
4. Discussion, Conclusion and Global Health Implications
Since the outbreak of the disease, Asia, Europe and now the United States are under the global microscope because of the enormous number of cases and deaths reported in these regions. From our study, we found that, in spite of the fact that the disease originated in Asia and the continent had the highest number of cases before the disease spread more rapidly in other continents, Asian countries have been able to contain the virus much more effectively than the other regions.
This could be because of the immediate stern measures taken by Asian countries which helped in faster containment of the outbreak or because the countries in the west seem to have been more complacent, despite getting a head start to prepare.6 Among the 32 countries worldwide that have a universal healthcare system, 22 were highly impacted by the disease so far. Italy, Spain, UK, Germany and France were the countries with the highest number of recorded COVID-19 cases among those with a UHC. Globally; more than 145,000 fatalities were attributed to high impact countries with UHC. There are various benefits of UHC, such as equitable health coverage for the entire population,7 lower cost of healthcare to the economy, reduced administrative costs, etc. Germany has had the lowest CFR among the most impacted countries since the beginning of the pandemic,8 and their success could be attributed to large-scale testing and early detection of the outbreak. Germany also has a much higher number of beds per capita as compared to Italy or Spain, which have a CFR of 13.8% and 10.2% respectively.9
There are few inherent limitations of UHC, including long wait times and limited usage of new healthcare technology because of restricted budget. Spanish patients have been reported of dying in waiting rooms before they could be admitted.10 COVID-19 pandemic has highlighted that ‘equitable distribution of healthcare resources’ may not necessarily be protective of death associated from COVID-19 pandemic, especially in countries with a high number of COVID-19 cases and limited healthcare resources like Italy and Spain.11-13 Italian healthcare professionals have specifically been in the news for the tough utilitarian decisions they have been making in the allocation of limited resources to maximize societal benefits in these trying times.11,12 Patients with existing comorbidities, those who are too old to recover or those who have lesser remaining life- years are allowed to die in order to accommodate for the aggressively-increasing number of patients showing up to the hospitals in a setting challenged by limited resources.11 Due to the dynamic nature of the ongoing pandemic, with numbers constantly changing, it is possible that the final results will only be available by the end of the pandemic, whenever that is.
References
- Update on the situation regarding the new coronavirus [transcript] - January 29, 2020.
- [Google Scholar]
- As coronavirus spread through Asia, the West had a head start to prepare. Why wasn't it used? (accessed )
- [Google Scholar]
- Global Ranking of COVID-19-Related Mortality by Country using a Novel Pandemic Efficiency Index (PEI) International Journal of Maternal and Child Health and AIDS. . 2020;9(2):182-185.
- [CrossRef] [PubMed] [Google Scholar]
- Germany has a remarkably low coronavirus death rate — thanks largely to mass testing, but also culture, luck, and an impressive healthcare system. (accessed )
- [Google Scholar]
- ‘We are making difficult choices’: Italian doctor tells of struggle against coronavirus. (accessed )
- [Google Scholar]





