Translate this page into:
Pre-Exposure Prophylaxis and HIV Prevention Among Key Populations in Nigeria

*Corresponding author: Olaniyi Felix Sanni, Research and Development, Heartland Alliance, Abuja, Nigeria. Tel: +2348060085465 fescosofanalysis@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Sanni OF, Umoh P, Kalaiwo A, Abang R, Oguntonade A, Amechi P, et al. A cross-sectional study on pre-exposure prophylaxis and HIV prevention among key populations in Nigeria. Int J MCH AIDS. 2024;13:e013. doi: 10.25259/IJMA_6_2023
Abstract
Background and Objective
The discovery of innovative pharmacological preventative measures in Human Immunodeficiency Virus transmission has boosted optimism in the successful control of HIV/AIDS with the objective of eradication and the end of the epidemic. Hence, assessing the effect of pre-exposure prophylaxis (PrEP) on HIV prevention among key populations (KPs) is imperative in advancing the conversation on ending HIV/AIDs.
Methods
This was a cross-sectional study using data from KPs female sex workers (FSWs), men who have sex with men (MSM), and people who inject drugs (PWIDs) enrolled in Heartland Alliance Ltd/GTE One Stop Shops (OSS) between May 2019 and April 2023 in the six selected Nigerian states (Lagos, Bayelsa, Cross River, Akwa Ibom, Jigawa, and Niger). Data were cleaned in a spreadsheet and analyzed using IBM-SPSS version 28.0. Descriptive statistics, including frequency and percentage calculations, were conducted to analyze the dataset. Additionally, cross-tabulation analysis was performed, with a significance level set at 0.05, to explore relationships between variables.
Results
The study population comprised 13,580 participants, with 56.1% female. In all, 43.9% were aged 18–35 and 97.3% were single. Among the three KPs examined, FSW was the largest subgroup (50.8%), followed by MSM (28.1%) and PWID (21.1%). Most participants had been on PrEP for 0–3 months (87.8%), and PrEP was initiated for 81.6% due to high-risk sexual behaviors and 9.9% for serodiscordant relationship reasons. Most of them were enrolled in community healthcare settings (97.0%). The results showed that 99.9% remained HIV negative, while only two (0.01%) were seroconverted while on PrEP. The HIV-positive cases did not complete one-month PreP treatment, comprising an FSW and a PWID. Recent HIV contact or poor compliance with PrEP medication are two possible causes of seroconversion.
Conclusion and Global Health Implications
The findings underscore the significance of integrating PrEP into a comprehensive HIV prevention approach, including newer molecules that will improve adherence and the necessity of ongoing monitoring and support for PrEP users. With these insights, there can be an advocacy for promoting PrEP among the KPs as a vital component of Nigeria’s HIV prevention strategy.
Keywords
Pre-Exposure Prophylaxis (PrEP)
HIV Infections
Interventions
Population
AIDS
Sex Workers
INTRODUCTION
HIV/AIDS is a significant danger to global public health. According to the World Health Organization, there were 690,000 deaths from AIDS-related causes in 2019 and 1.7 million new HIV infections among people living with HIV (PLWHIV).[1,2] The discovery of innovative pharmacological preventative measures in HIV transmission has boosted optimism in the successful control of HIV/AIDS, with the objective of eradication and the end of the epidemic. Pre- and post-exposure prophylaxis (PrEP/PEP) is essential to any effective HIV preventive approach. PrEP, when used regularly and consistently, provides an extra layer of protection against disease transmission in high-risk groups.[3]
HIV transmission has been dramatically reduced, even among high-risk contacts/key populations (KPs), owing to the introduction of PEP as a 28-day prophylactic course for both occupational and nonoccupational HIV exposure in the 1990s and its more recent combination with PrEP.[4] They only function if patients take their medications as prescribed and continue to get therapy for their condition.[5] Long wait times, staff shortages, poorly planned clinics, and laboratory delays are potential patient flow issues that might jeopardize this method’s effectiveness.[6] To improve patient adherence to treatment and provide better service, there is an urgent need to develop an in-built system for assessing practice and service utilization by stakeholders such as clinicians, managers, and trialists that is unique in addressing patients’ interests within the clinical setting.
Nigeria is among the high-burden nations, with an estimated 1.9 million PLWHIV.[2] In Nigeria, serodiscordant couples who engaged in high-risk sexual practices accounted for more than half of all new HIV infections.[7] As a result, using PrEP would be a strategic step toward lowering HIV transmission. One of the primary strategic objectives of the Federal Ministry of Health in Nigeria is to effectively decrease the occurrence of new HIV infections by improving the availability and utilization of HIV prevention, intervention, and prophylactic measures by 90% among the general population.[8] While the National HIV and AIDS Strategic Framework (NASF) in Nigeria encompasses several thematic areas, including prevention, it does not explicitly address nonoccupational PrEP as a distinct component of its strategic approach.
The National Guideline for HIV Prevention, Treatment, and Care, established by the Federal Ministry of Health in Nigeria, offers a comprehensive framework for implementing PrEP.[8] Although some KPs have poor PrEP/PEP knowledge[9,10] and different studies have investigated awareness and predictors of PrEP/PEP usage, little is known regarding the impact of PrEP on HIV prevention. As a result, this paper assesses the effect of PrEP on HIV prevention among KPs in Nigeria.
METHODS
Study Design
This research adopted a comprehensive cross-sectional design to explore KPs vulnerable to HIV, specifically female sex workers (FSWs), men who have sex with men (MSM), and people who inject drugs (PWIDs). These groups are all participants in the Heartland Alliance Ltd/GTE Comprehensive Key Populations HIV prevention program from May 2019 to April 2023, which operates in six targeted states in Nigeria: Lagos, Bayelsa, Cross River, Akwa Ibom, Jigawa, and Niger. Data were extracted and analyzed in August 2023.
Unlike studies that use sampling techniques, this research included all individuals enrolled in the PrEP program under the HAL/GTE One Stop Shop initiative, which serves as a convenient location that offers a wide range of services that meet various KP needs. This approach provided a complete dataset, allowing for an exhaustive analysis of the KPs in these states. Data for the study were sourced from the HAL/GTE OSS databases in the six selected states, with the highest number of these KPs in Northern and Southern Nigeria; by incorporating all individuals enrolled in PrEP using tenofovir disoproxil fumarate (TDF) (300 mg) + 3(taxotere and cyclophosphamide) TC (150 mg), the study aimed to offer a comprehensive understanding of HIV-related factors among these groups. This inclusive methodology enabled an in-depth examination of HIV prevention and treatment factors among the KPs. It also allowed for a holistic understanding of the challenges and opportunities related to HIV management in the selected states. This study adheres to the STROBE guidelines for reporting cross-sectional studies, ensuring rigorous standards for reporting observational research.
Data Analysis
Before analysis, the dataset was cleaned using Microsoft Excel to ensure accuracy and completeness. This involved removing duplicates, handling missing values, and verifying the integrity of the data. The cleaned data were then imported into IBM Statistical Package for Social Sciences Version 28 (IBM Corp., Armonk, NY) for statistical analysis. Descriptive statistics were employed to summarize the sociodemographic characteristics of the study population; this included the frequencies and percentages for variables such as gender, age, marital status, KP groups, state of residence, education level, employment status, and duration of PrEP treatment. Chi-square tests examined the relationship between KPs and their HIV status PEP treatment. All statistical tests were two-sided, and a p-value of less than 0.05 was considered statistically significant.
Ethical Consideration
The project implementation study was conducted using the approved KP-CARE 1 ethical clearance from Heartland Alliance. This clearance was modified in compliance with Heartland Alliance Ltd Gte’s authorization to access KP’s data in order to uphold strict data security and protection guidelines. Strict procedures were put in place to anonymize and safely store the collected data in order to ensure participant privacy and confidentiality.
RESULTS
Sociodemographic
The study population comprised 13,580 respondents, and Table 1 displays their sociodemographic characteristics. The study population was constituted mainly of female respondents (56.1%), while the male population was 43.9%. The study population was youthful demographic background with a mean age of 28.14 years, a standard deviation of 6.90, with 45.1% aged 26–35 years while 40.7% belonged to the 18–25 age group. Also, notably, a vast majority of the respondents were single (97.3%). FSWs made up more than half of the study population (50.8%), followed by MSM (28.1%) and PWIDs (21.1%). The state highly represented in this study was Lagos (51.7%), followed by Bayelsa (16.9%). Approximately 84.3% of the participants attained senior secondary education as their highest level, followed by postsecondary (10.3%); this shows a high literacy level in the study. The percentage of the respondents employed was 51% compared to 37.7% who were unemployed. Last, the majority of the respondents have been on PrEP treatment for a period of 0–3 months (87.8%), followed by 4–12 months (11.5%) and over 12 months (0.7%).
| Variables |
Frequency (n = 13,580) |
Percentage (%) | |
|---|---|---|---|
| Gender | Male | 5956 | 43.9 |
| Female | 7624 | 56.1 | |
| Age (Years) | 18–25 | 5527 | 40.7 |
| 26–35 | 6123 | 45.1 | |
| 36–55 | 1884 | 13.9 | |
| 56 and above | 46 | 0.3 | |
| Marital Status | Single | 13,213 | 97.3 |
| Married | 367 | 2.7 | |
| Key Population | FSW | 6896 | 50.8 |
| MSM | 3818 | 28.1 | |
| PWID | 2866 | 21.1 | |
| State of Residence | Akwa Ibom | 2098 | 15.4 |
| Bayelsa | 2290 | 16.9 | |
| Cross River | 2174 | 16.0 | |
| Lagos | 7018 | 51.7 | |
| Education | Primary school | 485 | 3.6 |
| Junior Secondary | 138 | 1.0 | |
| Senior Secondary | 11,453 | 84.3 | |
| Postsecondary | 1396 | 10.3 | |
| No Education | 108 | 0.8 | |
| Employment status | Student | 1533 | 11.3 |
| Unemployed | 5125 | 37.7 | |
| Employed | 6922 | 51.0 | |
| Treatment period | 0–3 months | 11,925 | 87.8 |
| 4–12 months | 1562 | 11.5 | |
| >12 months | 93 | 0.7 | |
FSW: Female sex workers, MSM: Men who have sex with men, PWID: People who inject drugs.
Initiation of PrEP
Most respondents’ reasons for choosing PrEP are shown in Figure 1, and they are their engagement in high-risk sexual behaviors (81.6%), followed by serodiscordant relationships (9.9%). In comparison, the category labeled “Others,” which included unlisted reasons, accounted for 7.5%.
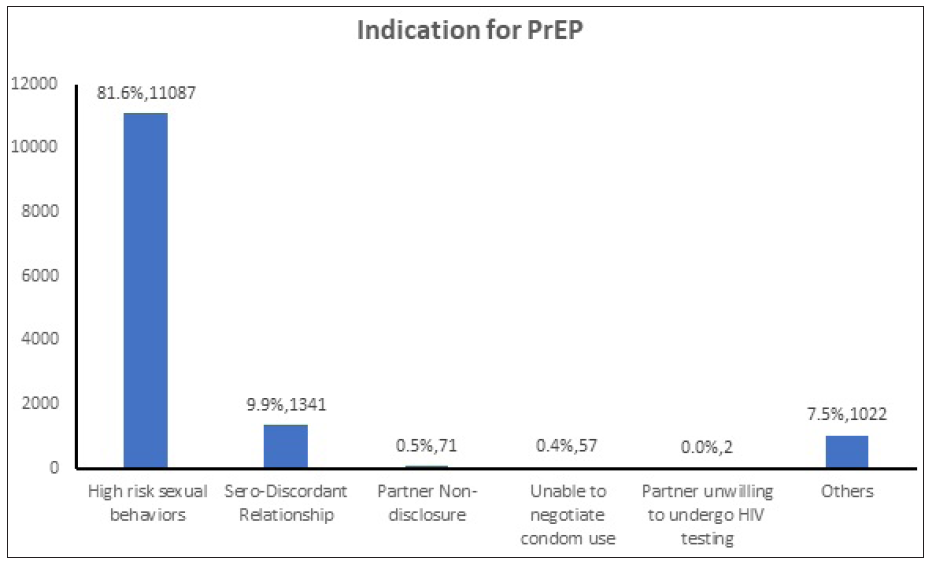
- Initiation of Pre-Exposure Prophylaxis (PrEP).
Pre-Exposure Prophylaxis Initiation Settings
The location of PrEP initiation is illustrated in Figure 2. The chart shows that most respondents started using PrEP in community healthcare (97.0%) settings such as outreach programs. In contrast, a smaller proportion (3.0%) started PrEP usage within clinical facilities, such as hospitals.
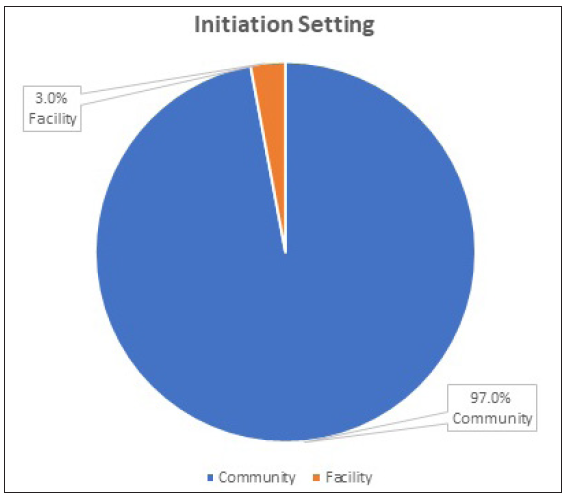
- Pre-Exposure Prophylaxis Initiation Settings
Duration of PrEP Medication Among Key Population
Notably, before initiating PrEP among the participants, none had a positive HIV diagnosis. The duration of PrEP medication among the KP is highlighted in Table 2. The result shows that the majority of the FSWs have been taking medication for a period of 0–3 months (90.1%), followed by those medicating for 4–12 months (9.4%) and those for 12 months and above (0.5%). Similarly, a significant proportion of MSM has been on PrEP medication for a period of 0–3 months (78.7%), followed by 4–12 months (20.3%) and 12 months and above (1.0%). Among PWID, a high proportion has utilized PrEP medication for 0–3 months (94.5%), followed by 4–12 months (4.8%) and over 12 months (0.7%). The association is statistically significant p<0.05.
| Variable | Duration of PrEP Medication | |||
|---|---|---|---|---|
| 0–3 Months | 4–12 Months | > 12 Months | X2 (P-value) | |
| FSW (%) | 6214 (90.1) | 648 (9.4) | 34 (0.5) |
458.507 (<0.001*) |
| MSM (%) | 3004 (78.7) | 775 (20.3) | 39 (1.0) | |
| PWID (%) | 2707 (94.5) | 139 (4.8) | 20 (0.7) | |
FSW: Female sex workers, MSM: Men who have sex with men, PWID: People who inject drugs.
HIV Status PEP Medication
The current HIV status of the respondents after undergoing PrEP medication is illustrated in Figure 3. The current HIV status shows that 99.9% of the respondents remained HIV-negative while 0.01% contracted the virus.
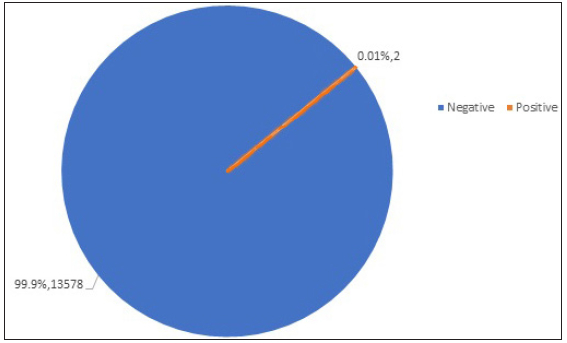
- HIV Status Post-Exposure Prophylaxis Medication.
Relationship Between KPs and HIV Status
The relationship between the KPs and their HIV status PEP is shown in Table 3. The result shows that the two positive cases were linked to FSW (0.01%) and PWID (0.01%). These two positive occurrences were associated with people on PrEP for 0–3 months (0.01%) and accessed care in community healthcare settings (0.01%). The two positive cases took PrEP treatment for less than one month, suggesting nonadherence to treatment: a false negative initial test result or a breakthrough infection.
| Variable | Duration of PrEP Medication | ||
|---|---|---|---|
|
HIV ‒ve (n = 13578) |
HIV +ve (n = 2) |
X2 (P-value) | |
| Group | |||
| FSW (%) | 6895 (99.9) | 1 (0.01) | 1.354 (0.508) |
| MSM (%) | 3818 (100.0) | 0 (0.0) | |
| PWID (%) | 2865 (99.1) | 1 (0.01) | |
| Treatment duration | |||
| 0–3 Months (%) | 11,923 (99.9) | 2 (0.01) |
0.278 (0.870) |
| 4–12 Months (%) | 1562 (100.0) | 0 (0.0) | |
| > 12 Months (%) | 93 (100.0) | 0 (0.0) | |
| Initiation setting | |||
| Community | 13,176 (99.9) | 2 (0.01) |
0.061 (0.805) |
| Facility | 402 (100.0) | 0 (0.0) | |
KP: Key population, PrEP: Pre-exposure prophylaxis, FSW: Female sex workers, MSM: Men who have sex with men, PWID: People who inject drugs.
DISCUSSION
This study examines the effect of PrEP on HIV prevention among KPs in Nigeria. The HIV PrEP is essential to HIV prevention.[11] The PrEP has emerged as an important strategy in the global fight against HIV/AIDS.
The study found that most respondents were female (56.1%), while males constituted 43.9% of the study population. This gender distribution might be attributed to the higher vulnerability of females to HIV infection in Nigeria and their higher engagement in sex work. Research has shown that FSWs are often disproportionately affected by HIV due to various socioeconomic factors, including limited access to healthcare and economic opportunities.[12,13] Therefore, the skewed gender distribution might reflect the higher prevalence of HIV among female KPs in Nigeria. From the study findings, the population is predominantly youthful, with 45.1% aged 26–35 and 40.7% belonging to the 18–25 age group. This youth-centric demographic is consistent with the overall age distribution of the Nigerian population. The implication is that targeting younger KPs for PrEP intervention could substantially and positively impact HIV prevention, given the higher HIV incidence rates among young people in Nigeria.[14] Also, most respondents reported being single (97.3%). This aligns with the characteristics of KPs, where individuals often face social stigmatization and discrimination, making it challenging to form stable relationships or marriages.[15,16] The implication is that PrEP programs should be designed to cater to a single individual’s specific needs and circumstances within KP communities.
Additionally, FSWs constituted the largest segment of the study population (50.8%), followed by MSM (28.1%) and PWIDs (21.1%). These findings align with the categorization of KPs.[17] The high representation of these groups underscores the importance of targeted PrEP interventions, as these populations are at heightened risk of HIV infection due to their behaviors and socioeconomic factors.[18,19] The study found that Lagos was the most highly represented (51.7%), followed by Bayelsa (16.9%). This geographic distribution may be due to variations in the availability and accessibility of PrEP services across different regions of Nigeria. Research has shown that urban areas often have better access to healthcare services, including HIV prevention.[20] Therefore, these findings highlight the need for equitable distribution of PrEP services to ensure broader coverage. In addition, most respondents had attained at least a senior secondary school level of education (84.3%), and more than half were employed (51.0%). This indicates a relatively high level of literacy and employment within the study population, which can be leveraged for effective PrEP awareness and adherence programs. Education and employment have been positively associated with better healthcare-seeking behaviors and adherence to HIV prevention strategies.[21,22]
Moreover, many respondents had been on PrEP treatment for 0–3 months (87.8%). This suggests a recent scale-up of PrEP programs in the study area. Longer durations of PrEP may be associated with improved outcomes and better HIV prevention effectiveness.[23] Therefore, the findings emphasize the need for continuous engagement and support for newly initiated individuals on PrEP.
Initiation of PrEP and Its Settings
From the findings, most respondents (81.6%) cited their engagement in high-risk sexual behaviors as the primary reason for choosing PrEP. This finding aligns with research on PrEP utilization among KPs globally and in Nigeria.[24] High-risk sexual behaviors, such as multiple sexual partners, inconsistent condom use, and transactional sex, have been identified as significant risk factors for HIV transmission.[25,26] Therefore, individuals who engage in these behaviors are more likely to perceive PrEP as a crucial preventive measure. In addition, the presence of serodiscordant relationships as the second most common reason (9.9%) for initiating PrEP corroborates previous studies highlighting the importance of PrEP in serodiscordant couples. In such partnerships, where one partner is HIV positive and the other is HIV negative, PrEP is a valuable tool for reducing the risk of HIV transmission.[27,28] These findings align with previous research conducted in different settings. For instance, a study by Pyra et al.,[29] conducted in East Africa demonstrated that PrEP was highly effective in reducing the risk of HIV transmission within serodiscordant couples, reinforcing the importance of PrEP for this population. Similarly, studies in various countries have consistently shown that individuals engaged in high-risk sexual behaviors are more likely to seek PrEP as a prevention strategy.[30,31]
These findings have several significant implications for HIV prevention strategies in Nigeria. First, the high percentage of respondents citing high-risk sexual behaviors as their reason for choosing PrEP underscores the need for targeted interventions among KPs engaging in such behaviors. These interventions may include comprehensive sexual education, condom distribution, and improved access to PrEP services.[32] Addressing the underlying factors contributing to high-risk behaviors, such as stigma and discrimination, is also critical. Second, recognizing serodiscordant relationships as a motivating factor for PrEP initiation highlights the importance of tailored counseling and support services for couples. Encouraging regular HIV testing and linkage to care for HIV positive partners is essential in serodiscordant relationships to ensure viral suppression and minimize transmission risk.[33,34]
The findings regarding the initiation settings for PrEP among KPs in Nigeria indicate a significant preference for community healthcare settings, with 97.0% of respondents choosing outreach programs for PrEP initiation. In comparison, only 3.0% opted for clinical facilities like the One Stop Shop/hospitals. The high prevalence of PrEP initiation in community healthcare settings can be attributed to several factors. First is the increased accessibility of outreach programs compared to clinical facilities. KPs, often facing stigma and discrimination, may feel more comfortable accessing PrEP services in community settings, receiving support from peers and community workers trained to address their unique needs.
Additionally, outreach programs may offer a more discreet and confidential environment, which is essential for those concerned about privacy. This finding aligns with existing literature that emphasizes the importance of community-based interventions for KPs in addressing HIV prevention and care.[35,36] The preference for community-based PrEP initiation carries significant implications for HIV prevention efforts in Nigeria. One of the most notable implications is the potential to reach a larger portion of KPs. Outreach programs have a broader reach and can penetrate remote areas with limited access to clinical facilities. This expansion of PrEP services can contribute to reducing new HIV infections among KPs, aligning with global and national goals.[37]
Furthermore, the community-based approach fosters a sense of trust and engagement among KPs. When individuals feel comfortable and supported, they are more likely to adhere to PrEP regimens and engage in routine HIV testing, which is crucial for its effectiveness.[38] However, while the findings of this study predominantly found a preference for community healthcare settings, contrasting findings from other regions or countries may shed light on the importance of providing options. Some studies have shown that KPs may have varying preferences based on their circumstances, such as urban or rural residence, socioeconomic status, and HIV risk factors.[39,40] This highlights the need for a flexible approach to PrEP initiation and retention in care that caters to the diverse needs within the KPs.
Duration of PrEP Medication Among KPs
The findings indicated that the majority of FSWs, MSM, and PWIDs have been taking PrEP medication for a relatively short period of 0–3 months. It is crucial to consider the awareness and accessibility of PrEP among KPs. There might be limited knowledge about PrEP in many settings, and accessing it may present challenges. This could explain why many participants had only recently initiated PrEP. Studies by Bauermeister et al.,[41] Eaton et al.,[42] Shover et al.,[43] and Spinelli et al.,[44] have highlighted the importance of improving awareness and accessibility to PrEP for KPs. In addition, stigma and discrimination related to HIV and KPs can deter individuals from seeking PrEP. Fear of disclosure, discrimination from healthcare providers, or societal prejudice can contribute to delayed uptake. Research by Stahlman et al.,[45] has shown how stigma remains a barrier to HIV prevention among KPs.
However, while a large proportion of KPs initiate PrEP within the first three months, this suggests an opportunity for early intervention in HIV prevention. Timely initiation of PrEP is essential for its effectiveness, so healthcare providers should focus on reaching KPs as early as possible after assessing their risk. Spinelli et al.,[44] emphasize prompt initiation’s importance for maximum benefit. These findings underscore the need for targeted educational programs and support services tailored to KPs. By addressing stigma, providing accurate information, and offering counseling, it may be possible to encourage more individuals to start PrEP sooner. Although a smaller proportion, some participants have been on PrEP for longer (4–12 months or more). This suggests a subset of individuals who have successfully engaged with PrEP over time. Ensuring their continued access to PrEP and support is critical to sustaining HIV prevention efforts.
HIV Status PEP Medication and Relationship Between KPs
As found in the study, the substantial majority (99.9%) of respondents remaining HIV negative after undergoing PrEP medication can be attributed to the effectiveness of PrEP in preventing HIV transmission. PrEP, consisting of antiretroviral drugs taken by HIV negative individuals, has been widely recognized as an efficacious preventive measure, particularly among KPs such as MSM, sex workers, and PWID.[46] This result aligns with previous research indicating that PrEP significantly reduces the risk of HIV infection when taken consistently and correctly.[47–49] Also, the 0.01% of respondents contracting HIV PEP highlights that PrEP is not infallible. This small percentage may be due to several factors, including inconsistent PrEP adherence or seroconversion occurring during the initial stages of PrEP usage when the protective effect is not fully established. This underscores the importance of adherence counseling and regular testing among PrEP users. It also emphasizes the significance of risk-reduction strategies, such as condom use, in addition to PrEP.[38]
Furthermore, the overwhelmingly high percentage of respondents remaining HIV negative suggests that PrEP has the potential to play a pivotal role in reducing HIV transmission among KPs in Nigeria. It provides an encouraging avenue for HIV prevention programs and policymakers to prioritize the promotion and accessibility of PrEP as an integral component of the national HIV prevention strategy. In addition, the small number of individuals contracting HIV PEP indicates that further attention is needed to understand the circumstances under which PrEP effectiveness might be compromised. This underscores the importance of ongoing monitoring, support, and education for PrEP users to ensure consistent and correct usage. It also emphasizes the necessity of integrating PrEP into a comprehensive prevention approach, considering the limitations of any single prevention method.[50]
Moreover, the exceptionally low HIV incidence rate among KPs, as indicated by the 0.01% prevalence for FSWs and PWIDs, is noteworthy. This can be attributed to several factors. First, it may reflect the success of PrEP as an effective preventive measure against HIV transmission. Previous research has demonstrated that PrEP is highly effective when taken consistently, and this could explain the low infection rates among individuals who adhered to the regimen.[49,51] Studies such as the HPTN 067/ADAPT trial have shown that PrEP can significantly reduce the risk of HIV acquisition among high-risk populations, which aligns with the observed low HIV prevalence among KPs PEP use.[52] The finding that these two positive cases occurred among individuals on PrEP for 0–3 months is significant. It suggests there may be a delay in the full protective effect of PrEP. It is essential to delve into why individuals who have been on PrEP for a shorter duration seem to have a slightly higher risk of HIV infection. This could be due to suboptimal adherence, misconceptions about the rapid onset of PrEP efficacy, or late initiation. Research studies have indicated that PrEP efficacy may take some time to reach maximum protection. For instance, the PrEP trial reported that participants who adhered to the medication had greater protection, but it took time to build up to maximum effectiveness.[53]
These findings underscore the critical importance of sustained adherence to PrEP. It is essential to emphasize the need for individuals to continue taking PrEP consistently, even if they perceive themselves to be at low risk. Studies like the TDF 2 trial have highlighted that PrEP efficacy is highly correlated with adherence. Suboptimal adherence can result in reduced protection against HIV.[54] The observation that the two positive cases accessed care in community healthcare settings suggests there may be gaps in the quality of care and education provided. These settings should be equipped to offer comprehensive information about PrEP, including the importance of adherence and the time it takes for the medication to reach its maximum effectiveness. The success of PrEP programs often relies on robust education and counseling. Studies such as the Partners PrEP Study have shown that thorough education and support can improve adherence and reduce HIV risk.[55]
Limitations
One limitation of this study is the reliance on secondary data obtained from Heartland Alliance International (HA LTD/GTE) baseline data. This may introduce potential biases and data quality issues related to data collection methods, completeness, and accuracy, as the study did not have control over the original data collection process. Additionally, the cross-sectional observational study design employed in this research limits the establishment of causal relationships between PrEP and HIV prevention outcomes among KPs. Longitudinal or experimental designs would provide stronger evidence of PrEP effectiveness. Finally, the study’s focus on six specific Nigerian states may not fully represent the diversity of the entire nation, potentially limiting the generalization of the findings to other regions within Nigeria.
CONCLUSION AND GLOBAL HEALTH IMPLICATIONS
This study delved into the impact of PrEP on HIV prevention among KPs in Nigeria. The findings underscore the prevalence of PrEP as a critical tool in reducing HIV transmission within this vulnerable demographic. A substantial proportion of respondents remained HIV negative PEP, emphasizing the pivotal role that PrEP can play in the national HIV prevention strategy. The gender distribution, with a majority being female, mirrors the heightened vulnerability of females to HIV in Nigeria, highlighting the urgent need for targeted interventions. The youth-centric demographic underscores the importance of early PrEP initiation, given higher HIV incidence rates among young people.
Additionally, the predominance of single individuals among KPs calls for tailored PrEP programs to address their unique needs. This study illuminates the preference for community healthcare settings for PrEP initiation, offering insights into accessibility and comfort factors. This finding can guide the expansion of PrEP services to remote areas and foster trust among KPs.
While most participants had recently initiated PrEP, emphasizing the importance of awareness and early intervention, this study also revealed the need for sustained adherence to maximize PrEP effectiveness. The two positive cases occurring within the first 0–3 months of PrEP use highlight the importance of consistent adherence and education on PrEP’s delayed onset of efficacy. The findings underscore the significance of integrating PrEP into a comprehensive prevention approach and the necessity of ongoing monitoring and support for PrEP users. With these insights, there can be an advocacy for the promotion and accessibility of PrEP as a vital component of Nigeria’s HIV prevention strategy, focusing on addressing the unique needs of KPs and ensuring sustained adherence for optimal impact on HIV transmission. This study promotes global PrEP education, promotion, and access, addressing the requirements of critical populations, promoting optimal adherence, and providing an appropriate example for other nations facing similar HIV prevention issues.
Key Messages
-
The study emphasizes the potential of pre-exposure prophylaxis (PrEP) to reduce HIV transmission among critical populations in Nigeria.
-
The gender distribution, especially the majority being female, highlights the heightened sensitivity of Nigerian women to HIV.
-
Targeted interventions are needed to address and ease this vulnerability. Furthermore, the prevalence of single people in KPs requires personalized PrEP programs to meet their unique needs, underscoring the importance of tailored interventions for certain subgroups.
-
This study sheds light on the preference for PrEP start in community healthcare settings.
Acknowledgments
The authors would like to express our heartfelt gratitude to Heartland Alliance LTD/GTE (HALG) for their critical participation in enriching this manuscript. The data provided by HALG considerably improved the robustness of our research. We appreciate their collaborative spirit and dedication to furthering our expertise in this subject.
COMPLIANCE WITH ETHICAL STANDARDS
Conflicts of Interest
Dr. Bartholomew Boniface Ochonye is the CEO of Heartland Alliance.
Financial Disclosure
Funding for this study was made possible by USAID/PEPFAR.
Funding/Support
Funding for this study was made possible by USAID/PEPFAR.
Ethics Approval
The project implementation study was conducted using the approved KP-CARE 1 ethical clearance from Heartland Alliance. This clearance was modified in compliance with Heartland Alliance Ltd Gte’s authorization to access KP’s data in order to uphold strict data security and protection guidelines. Approval number UUTH/AD/S/96/VOL.XXI/554, dated May 10, 2021.
Declaration of Patient Consent
Patient’s consent not required as patient’s identity is not disclosed or compromised.
Use of Artificial Intelligence (AI)-Assisted Technology for Manuscript Preparation
The authors confirm that there was no use of AI-Assisted Technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
This manuscript’s results and conclusions are based on information available at the time of publication. Subsequent events may have an impact on the validity or practicality of the study’s findings.
REFERENCES
- Nigeria Prevalence Rate. Fed Minist Heal 2019:1-7. [Accessed 2020 Aug 20 ]. Available from: https://naca.gov.ng/nigeria-prevalence-rate/
- [Google Scholar]
- HIV and AIDS. World Health Organization; 2020.
- Awareness and use of pre-exposure and postexposure prophylaxes among Nigerian university students: Findings from a cross-sectional survey. Medicine (Baltimore). 2018;97(36):e12226.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Perspectives on HIV pre-and postexposure prophylaxes (prep and pep) among female and male sex workers in Mombasa, Kenya: Implications for integrating biomedical prevention into sexual health services. AIDS Educ Prev. 2017;29(2):141-53.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Predictors of disengagement in care for individuals receiving pre-exposure prophylaxis (PrEP) J Acquir Immune Defic Syndr. 2019;81(4):E104-8.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Clinic flow for STI, HIV, and TB patients in an urban infectious disease clinic offering point-of-care testing services in Durban, South Africa. BMC Health Serv Res. 2018;18(1):363.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- HIV epidemiology in Nigeria. Saudi J Biol Sci. 2018;25(4):697-703.
- [CrossRef] [PubMed] [Google Scholar]
- HIV non-occupational post exposure prophylaxis in Nigeria: A review of research evidence and practice. Int J Matern Child Heal AIDS. 2019;8(2):101-19.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Differences in awareness of pre-exposure prophylaxis and post-exposure prophylaxis among groups at-risk for HIV in New York State: New York City and Long Island, NY, 2011–2013. J Acquir Immune Defic Syndr. 2017;75(3):S383-91.
- [CrossRef] [PubMed] [Google Scholar]
- Disparities in awareness of HIV postexposure and preexposure prophylaxis among notified partners of HIV-positive individuals, New York City 2015–2017. J Acquir Immune Defic Syndr. 2017;76(2):132-40.
- [CrossRef] [PubMed] [Google Scholar]
- Intersectional discrimination and PrEP use among young black sexual minority individuals: The importance of black LGBTQ communities and social support. AIDS Behav. 2023;27(1):290-302.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Gender inequality and HIV transmission: A global analysis. J Int AIDS Soc. 2014;17(1):19035.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Socio-demographic characteristics and behavioral risk factors of female sex workers in sub-Saharan Africa: A systematic review. AIDS Behav. 2012;16(4):920-33.
- [CrossRef] [PubMed] [Google Scholar]
- Low coverage of HIV testing among adolescents and young adults in Nigeria: Implication for achieving the UNAIDS first 95. PLoS One. 2020;15(5):e0233368.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Similar, but different: Drivers of the disproportionate HIV and sexually transmitted infection burden of key populations. J Int AIDS Soc. 2019;22(Suppl 6):e25344.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Relationship stigma and relationship outcomes in interracial and same-sex relationships: Examination of sources and buffers. J Fam Psychol. 2015;29(6):818-30.
- [CrossRef] [PubMed] [Google Scholar]
- Key Populations Atlas. UNAIDS; 2018. [Accessed 2020 Aug 20]. Available from: https://www.unaids.org/en/topic/key-populations.
- Proactive strategies to optimize engagement of Black, Hispanic/Latinx, transgender, and nonbinary individuals in a trial of a novel agent for HIV pre-exposure prophylaxis (PrEP) PLoS One. 2022;17(6):e0267780.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Tailored combination prevention packages and PrEP for young key populations. J Int AIDS Soc. 2015;18(2):8-22.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Strategies to improve linkage to HIV care in urban areas of sub-Saharan Africa: A systematic review. HIV/AIDS—Res Palliat Care. 2019;11:321-32.
- [PubMed] [Google Scholar]
- Employment as a social determinant of HIV care and prevention outcomes. AIDS Updates—Recent Advances and New Perspectives 2021
- [PubMed] [Google Scholar]
- Do the more educated know more about health? Evidence from schooling and HIV knowledge in Zimbabwe. Econ Dev Cult Change. 2014;62(3):489-517.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Scaling-up PrEP delivery in sub-Saharan Africa: What can we learn from the scale-up of ART? Curr HIV/AIDS Rep. 2019. ;16(2):141-50.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Communication needs for improved uptake of PrEP and HIVST services among key populations in Nigeria: A mixed-method study. AIDS Res Ther. 2021;18(1):88.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- 844 high risk behaviors, suboptimal HIV viral suppression, and limited PrEP use among people who engage in transactional sex. Open Forum Infect Dis. 2021;8(Supplement_1):S512-3.
- [Google Scholar]
- Estimating HIV prevalence and risk behaviors among high-risk heterosexual men with multiple sex partners: Use of respondent-driven sampling. J Acquir Immune Defic Syndr. 2009;51(1):72-7.
- [CrossRef] [PubMed] [Google Scholar]
- HIV-negative male couples’ attitudes about pre-exposure prophylaxis (PrEP) and using PrEP with a sexual agreement. AIDS Care. 2016;28(8):994-9.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- PrEP discontinuation and prevention-effective adherence: Experiences of PrEP users in Ugandan HIV serodiscordant couples. J Acquir Immune Defic Syndr. 2019;82(3):265-74.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- PrEP use during periods of HIV risk among East African women in serodiscordant relationships. J Acquir Immune Defic Syndr. 2018;77(1):41-5.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- HIV providers’ likelihood to prescribe pre-exposure prophylaxis (PrEP) for HIV prevention differs by patient type: A short report. AIDS Care. 2016;28(9):1154-8.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Sexual behavior, risk compensation, and HIV prevention strategies among participants in the San Francisco PrEP demonstration project: A qualitative analysis of counseling notes. AIDS Behav. 2016;20(7):1461-9.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- The role of sexual risk behaviors on PrEP awareness and interest among men who have sex with men in Latin America. Int J STD AIDS. 2019;30(6):542-9.
- [CrossRef] [PubMed] [Google Scholar]
- “I have it just like you do”: Voices of HIV-negative partners in serodifferent relationships receiving primary care at a public clinic in San Francisco. AIDS Care. 2015;27(3):401-8.
- [CrossRef] [PubMed] [Google Scholar]
- HIV-1 prevention for HIV-1 serodiscordant couples. Curr HIV/AIDS Rep. 2012;9(2):160-70.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Adequate funding of comprehensive community-based programs for key populations needed now more than ever to reach and sustain HIV targets. J Int AIDS Soc. 2022;25(7):e25967.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Enhancing benefits or increasing harms: Community responses for HIV among men who have sex with men, transgender women, female sex workers, and people who inject drugs. J Acquir Immune Defic Syndr. 2014;66(Suppl 3):S319-28.
- [CrossRef] [PubMed] [Google Scholar]
- The Global AIDS Strategy 2021–2026. WHO; 2020. p. :10-2.
- Helping our patients take HIV pre-exposure prophylaxis (PrEP): A systematic review of adherence interventions. HIV Med. 2014;15(7):385-95.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Heterogeneous HIV testing preferences in an urban setting in Tanzania: Results from a discrete choice experiment. PLoS One. 2014;9(3):e92100.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Heterogeneity in individual preferences for HIV testing: A systematic literature review of discrete choice experiments. EClinicalMedicine. 2020;29-30:100653.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- PrEP awareness and perceived barriers among single young men who have sex with men. Curr HIV Res. 2014;11(7):520-7.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Minimal awareness and stalled uptake of pre-exposure prophylaxis (PrEP) among at risk, HIV-negative, black men who have sex with men. AIDS Patient Care STDS. 2015;29(8):423-30.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- HIV preexposure prophylaxis initiation at a large community clinic: Differences between eligibility, awareness, and uptake. Am J Public Health. 2018;108(10):1408-17.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- A panel management and patient navigation intervention is associated with earlier prep initiation in a safety-net primary care health system. J Acquir Immune Defic Syndr. 2018;79(3):347-51.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Measuring sexual behavior stigma to inform effective HIV prevention and treatment programs for key populations. JMIR Public Heal Surveill. 2017;3(2):e23.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Oral pre-exposure prophylaxis (PrEP) to prevent HIV: A systematic review and meta-analysis of clinical effectiveness, safety, adherence and risk compensation in all populations. BMJ Open. 2022;12(5):e048478.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- HIV pre-exposure prophylaxis (PrEP): A review of current knowledge of oral systemic HIV PrEP in humans. Infection. 2016;44(2):151-8.
- [CrossRef] [PubMed] [Google Scholar]
- 1963. PrEP significantly reduces the rate of new HIV diagnoses in US metropolitan statistical areas independent of treatment as prevention (2012–2017) Open Forum Infect Dis. 2019;6(Supplement_2):S64-5.
- [Google Scholar]
- Effectiveness and safety of oral HIV preexposure prophylaxis for all populations. AIDS. 2016;30(12):1973-83.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- A review of approaches used to increase awareness of pre-exposure prophylaxis (PrEP) in the United States. AIDS Behav. 2019;23(7):1749-70.
- [CrossRef] [PubMed] [Google Scholar]
- PrEP adherence patterns strongly affect individual HIV risk and observed efficacy in randomized clinical trials. J Acquir Immune Defic Syndr. 2016;72(4):444-51.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Low disclosure of PrEP nonadherence and HIV-risk behaviors associated with poor HIV PrEP adherence in the HPTN 067/ADAPT Study. J Acquir Immune Defic Syndr. 2019;82(1):34-40.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Symptoms, side effects and adherence in the iPrEx open-label extension. Clin Infect Dis. 2016;62(9):1172-7.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- FEM-PrEP: Adherence patterns and factors associated with adherence to a daily oral study product for pre-exposure prophylaxis. J Acquir Immune Defic Syndr. 2014;66(3):324-31.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Clinical treatment options infectious diseases: Update on PrEP implementation, adherence, and advances in delivery. Curr Treat Options Infect Dis. 2015;7(2):101-12.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]





