Translate this page into:
A Framework for Protecting Pregnant Women in the Era of COVID-19 Pandemic
*Corresponding author email: deepa.dongarwar@bcm.edu
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
The severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the causative agent for the coronavirus disease 2019 (COVID-19) pandemic, highlighted and compounded problems while posing new challenges for the pregnant population. Although individual organizations have provided disparate information, guidance, and updates on managing the pregnant population during the current COVID-19 pandemic, it is important to develop a collective model that highlights all the best practices needed to protect the pregnant population during the pandemic. To establish a standard for ensuring safety during the pandemic, we present a framework that describes best practices for the management of the pregnant population during the ongoing COVID-19 pandemic.
Keywords
COVID-19
Pregnant women
maternal and child health
program design and implementation
framework
professional associations
special considerations
1. Introduction
The coronavirus disease 2019 (COVID-19) pandemic, caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), was first identified in Wuhan, China in December 2019.1 The COVID-19 pandemic has significantly impacted social, occupational, and healthcare practices globally.2 For the pregnant women’s population, who naturally face special risks related to childbearing and overall development, the COVID-19 pandemic has imposed more challenges and put this population at greater risk.
During pregnancy and child development, immunologic changes occur that may induce a state of increased susceptibility to certain intracellular pathogens, including viruses, intracellular bacteria, and parasites.3 The World Health Organization (WHO) reports that the current basic reproduction number (R0) of SARS-CoV-2 is within the estimated range of 1.4-2.5; this value exceeds the previous R0 of the 2012 SARS-CoV-1 pandemic. The R0 value implies that human host infected with SARS-CoV-2 can spread the virus to about 1.4 – 2.5 extra hosts.4 Thus, we can assume extra precautions should be taken by pregnant women, children, and their families to prevent community spread of COVID-19.
Various organizations such as the American College of Obstetricians and Gynecologists (ACOG), and the Maternal and Child Health Bureau at the Health Resources and Services Administration (HRSA) of the U.S. Department of Health and Human Services have developed separate advisory guidance/ updates by constructing resources that will be useful in providing safe and high-quality care to mothers and babies during the COVID-19 pandemic.5,6 In addition, with the pandemic in place, some states have been able to redirect funds from Title V grants (the U.S. federal grant programs of support for promoting and improving the health and well-being of the nation’s mothers, children, and family) to assist in investigations, education/ information provision, emergency preparedness and infrastructure.7 Although stand-alone information and guidance on managing the pregnant population during the current COVID-19 pandemic are being created, it is important to develop a cohesive model that highlights all the best practices. In this study, we propose a framework for the health management of pregnant women during the ongoing COVID-19 pandemic.
2. Methods
This study was conducted by the participants of the Maternal and Child Health (MCH) Student Training Program at Texas Southern University and the Center of Excellence in Health Equity Training program at Baylor College of Medicine. Using Nominal Group Technique (NMT), we developed a unidirectional conceptual framework based on program-articulated tasks that could positively influence short- and long-term outcomes of program design and implementation for pregnant population during the COVID-19 pandemic. The senior author was the moderator of the NMT and conducted the survey to devise the components that should be considered in the program design. Then all participants prioritized and ranked the components; and the final components were included in the final framework.
When designing the program framework to best manage the pregnant patients during the COVID-19 pandemic, a variety of areas of focus were considered and finalized, including provider/patient planning and coordination, personnel, preventative measures, COVID-19 testing, community and physical distancing, telehealth, personal protective equipment, supplies, prioritization of care, ongoing assessment, patient communication, and disparities. We believe that activities and procedures targeting a pregnant woman in the era of COVID-19 pandemic will be best implemented across important milestones of the three main pregnancy and childbirth related periods. These are (1) the early prenatal period, (2) late prenatal period, and (3) the peripartum period. Our framework is analogous to the life course theory, a conceptual framework that has been extensively utilized to explain cumulative burden of disease and differential outcomes across different population groups over time. 7
3. Results
Figure 1 illustrates details of our framework for protecting pregnant women during the COVID-19 pandemic, which is divided into 5 sections. In this framework, we postulate that the perinatal period could be divided or classified into the early prenatal period, late prenatal period, and peripartum period, and the best practices to be followed for protection of pregnant women and their children include healthcare visits, supplements, safe breastfeeding practices, etc. During these periods, telecommunication and telemedicine are being used for prenatal/postnatal care and discharge/follow up visits for low risk patients.8 During the peripartum period, other grave concerns encompassing the spread of COVID-19 is the possibility of the mother passing the virus to the unborn child. According to the Centers for Disease Control and Prevention (CDC), there is no evidence at this time to support or contradict the claim that COVID-19 can be passed to an unborn child in utero.9 Therefore, recommended vaccinations such as the influenza and Tdap should be continued, to protect both the mother and infant.9 The environmental factors such as social behaviors of proper distancing, face covering, etc. and availability of resources, such as access to testing centers, medical assistance and insurance coverage; and household factors such as pandemic planning and preparedness, hygiene practices etc. are extremely important in maintaining good health for the pregnant women. Together with considerations at each stage of the pregnancy, environmental and household safety protocols, updated vaccination and medication records; and online resources provided by various organizations, pregnant population could be safeguarded and protected during this COVID-19 pandemic.
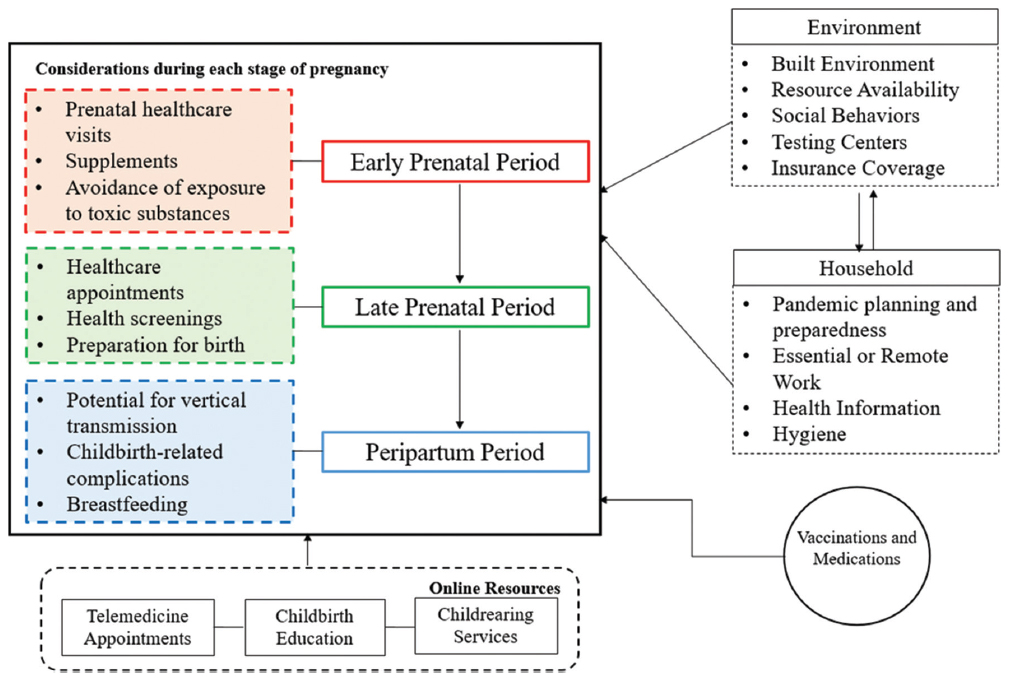
- Framework for Protecting Pregnant Women During the COVID-19 Pandemic
4. Discussion And Global Health Implications
Ensuring the health of mothers, infants, and children is important because it mirrors the health of the next generation. Naturally, many factors can affect pregnancy and childbirth, and the addition of a novel and rapidly evolving virus like COVID-19 drastically shifts how the Maternal and Child Health (MCH) population should be managed-requiring more safety precautions, special considerations, and new program implementation. The social determinants of health (SDOH) are known to contribute to worse outcomes in the maternal population.10 Therefore, surveillance system to protect the MCH population is extremely important during the current COVID-19 pandemic.11
The COVID-19 pandemic underscores the necessity for special considerations for pregnant women and family engagement. Special considerations for the pregnant population should include review of insurance availability. About 49% of Americans have employer provided health insurance.12 Loss of health insurance due to unemployment has increased during the pandemic as a result of stay-at-home orders and business closures. The potential impact of increased uninsured MCH patients infected with COVID-19 poses another public health emergency.
For the pregnant population, the COVID-19 pandemic has highlighted and complicated already occurring problems while posing new public health emergencies. To continue working towards improved MCH equity, special considerations, direct support, adequate resources, and best practice program implementation should be driven by policy makers, healthcare systems, and MCH focused non-profit organizations. This framework has been developed by the research team and remains untested at this point. Future researchers and policy makers should utilize this framework to validate and implement programs for protection of pregnant women’s population during the pandemic.
Acknowledgements:
Not applicable.
Compliance with Ethical Standards
Conflicts of Interest: None from all authors and co-authors.
Financial Disclosure: None.
Funding/Support: This work was funded by the Health Resources and Services Administration’s Maternal and Child Health Student Training Program (HRSA-MCH; T16MC29831) and U.S. Department of Health and Human Services and Health Resources and Services Administration for Baylor College of Medicine Center of Excellence in Health Equity, Training, and Research (Grant No: D34HP31024).
Ethics Approval: Not applicable.
Disclaimer: None.
References
- Coronavirus (COVID-19) frequently asked questions. https://www.cdc.gov/coronavirus/2019-ncov/faq.html#In-Case-of-an-Outbreak-in-Your-Community Published June 17, 2020
- Johns Hopkins Coronavirus Resource Center. https://coronavirus.jhu.edu/. Published 2021
- Emerging infections and pregnancy. Emerg Infect Dis. 2006;12(11):1638-1643. doi:10.3201/eid1211.060152
- [Google Scholar]
- China coronavirus:what do we know so far? BMJ. 2020;368:m308. doi:10.1136/bmj.m308 Published January 24, 2020
- [Google Scholar]
- Coronavirus (COVID-19) Information. https://www.hrsa.gov/coronavirus. Published 2021
- Racial and Ethnic Disparities in Birth Outcomes:A Life-Course Perspective. Matern Child Health J. 2003;7(1):13-30. doi:10.1023/a:1022537516969
- [Google Scholar]
- 2020. Maternal and Child Health During COVID-19. https://www.aha.org/system/files/media/file/2020/05/COVID-19-Maternal-Guidelines_rev6.pdf
- If You Are Pregnant, Breastfeeding, or Caring for Young Children. https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/pregnancy-breastfeeding.html Published June 9, 2020
- Role of Social Determinants of Health in Widening Maternal and Child Health Disparities in the Era of Covid-19 Pandemic. Int J MCH AIDS. 2020;9(3):316-319. doi:10.21106/ijma.398
- [Google Scholar]
- A Surveillance System for the Maternal and Child Health (MCH) Population During the COVID-19 Pandemic. Int J MCH AIDS. 2020;9(3):350-353. doi:10.21106/ijma.411
- [Google Scholar]
- Health Insurance Coverage of the Total Population Data (2008-2018). https://www.kff.org/other/state-indicator/total-population/





