Translate this page into:
Birth Preparedness and Complication Readiness among Women Attending Antenatal Clinics in Ogbomoso, South West, Nigeria
✉Corresponding author email: samdeji3@hotmail.com
Abstract
Background:
Information on factors associated with birth preparedness and complication readiness (BP/CR) is central in designing cost effective programs for reducing maternal deaths among women. This study assessed factors influencing BP/CR among pregnant women attending antenatal clinic in Ogbomoso, South West Nigeria.
Methodology:
This is a cross-sectional study conducted between January and April, 2015. Systematic sampling technique was employed to recruit 400 women attending antenatal clinic at Bowen University Teaching Hospital, Ogbomoso, Nigeria. A pre-tested questionnaire was used for data collection and data analysis was done using SPSS version 21. Chi-square test was used for bivariate analysis while binary logistic regression was used for multivariate analysis. Statistical significance was set at p <0.05.
Results:
More than half (51.3%) of our respondents were in the 30-39 age category. Only 40.3% of these respondents were reported well prepared for births and were complication ready. The proportion of women who had BP/CR was significantly higher among those in the middle socio-economic group (51.6%, p<0.05), those who practiced Christianity (76.4%, p<0.05) and those from Yoruba ethnic group (80.1%, p<0.05). Respondents in lower socio-economic group were 42% less likely to have prepared for birth compared to women in the high socio-economic class (OR: 0.58, 95% CI: 0.34-0.99).
Conclusion and Global Health Implications:
The proportion of Nigerian women in our sample who were well-prepared for birth and its complication was below average. There is need for more awareness programs on BP/CR; such programs should target all women especially the vulnerable group.
Keywords
Birth Preparedness
Complication Readiness
Antenatal Care
Maternal Mortality
Nigeria
Focused Antenatal Care
Demographic and Health Survey
Introduction
Globally, maternal death has remained a public health concern especially in developing countries where 99% of these deaths occur.[1] The burden of maternal death is currently alarming; not less than 289,000 maternal deaths occurred globally in 2013.[2]; Sub-Saharan Africa (SSA) alone accounts for 62% (179,000 maternal deaths) of these globally estimated maternal deaths.[2] The region also has the highest regional Maternal Mortality Ratio (MMR) of 510 maternal deaths/100,000 live births among the developing regions.[2] Maternal death in Nigeria mirrors that of the entire SSA because of the country's large population. For instance, the Nigeria Demographic and Health Survey (NDHS) report for Nigeria in 2013 shows that Nigeria has MMR of 545 deaths/100,000 live births—estimated to be 13% of the global maternal deaths. MMR is equally unacceptably high in Oyo state, estimated to be as high as 143 maternal deaths/100,000 live births as at May, 2010.[3] Studies on birth-preparedness and complication readiness (BP/CR) are vital in trying to understand the underlying factors and subsequently in stemming the tide of MMR. Given the high burden of MMR in Oyo State, it is equally important to understand the factors associated with BP/CR among women in the state.
Birth-preparedness and complication readiness (BP/CR), developed to promote timely utilization of skilled maternal and neonatal care, refers to a process of planning for normal birth and anticipating actions needed in case of emergency.[4] BP/CR planning often includes identifying place of delivery, identifying mode of transportation to place of delivery, making arrangements for blood donors, and saving money for the delivery. The concept of BP/CR which is one of the key components of Focused Antenatal Care (FANC) encourages sharing the burden of childbirth between mothers, their families, and the community at large. It is a pragmatic approach designed to overcome the three delays causing most maternal deaths worldwide.[5] These delays are: delay in deciding to seek care, delay in getting to health facilities, and delay in obtaining care at the health facility.
Recognizing its crucial role in reducing maternal and neonatal deaths, the World Health Organization (WHO) in 2001 recommended and promoted BP/CR intervention as a fundamental component of antenatal program and the integrated management of pregnancy and childbirth.[6] The global Standard for Maternal and Neonatal Care issued by WHO in 2006 recommended that all pregnant women should have a written plan for birth and for dealing with unexpected adverse events in deliveries or immediately after birth. This plan should be discussed with skilled attendant at each antenatal visit or at least one month before delivery.[7] BP/CR intervention has therefore been embraced with varied implementation by many African countries including Nigeria, Burkina Faso and South Africa to mention but a few. Meanwhile, the Nigerian National Reproductive Health Policy of 2001 targeted 50% reduction in maternal mortality and 50% increased access to blood transfusion and emergency obstetric care services by 2006.[8] More than ten years after, Nigeria is still not able to achieve these reproductive goals not even with the adoption of the concept of BP/CR.
Different studies have reported low preparedness of women towards childbirths in developing countries. For example, only 47.8% of pregnant women in Indora city of India,[9] 17% in Ethiopia,[10] 23% in Ghana,[11] and 34.9% in Ile Ife, Nigeria[12] were birth-prepared as documented in various studies. Although similar studies have been conducted in different parts of Nigeria, [12-15] however, few of them had examined factors influencing preparation of women for birth and its complications. Moreover, only a few of these studies could be said to be recently conducted in the South Western part of the country where the most current study that is readily accessible was in 2011 in Ile-Ife.[12] The study was, however, restricted to health facilities in Osun State and did not cover all the communities in the South Western part of Nigeria. It is, therefore, imperative to assess the current practice gap regarding BP/CR among women in Oyo State particularly in Ogbomoso town where no such study has been conducted before. This study was aimed at providing baseline information for charting progress in this area, as well as for appropriate decision making by policy makers in the South West geopolitical zone of Nigeria. The study objectives were to assess practices and factors associated with BP/CR among pregnant women attending antenatal clinic in Ogbomoso, South West Nigeria.
Methodology
The study was conducted in a missionary tertiary health institution in Ogbomoso. The health institution is located in Ogbomoso North Local Government Area (LGA) of Oyo State Nigeria. Ogbomoso, an ancient city in the South Western part of Nigeria, has a population of 1.2 million people, according to the last population census conducted in Nigeria in 2006.[16] The inhabitants are predominantly of Yoruba ethnic group but other tribes such as Hausa and Igbo also reside in the town. The people are predominantly peasant farmers but a sizeable number of them are civil servants while others are involved in trading activities.
The study design was cross-sectional and hospital- based with the study population of women who were booked in the health facility whose gestational ages were at least 20 weeks. Women who were having certain pregnancy-related complications or who failed to give their consents for participation were excluded from the study. The minimum sample size was determined using the Leslie Kish formula for estimating single proportion.[17] Based on report of a similar study conducted in Nigeria, a proportion of 35% was used as percentage of pregnant women who had adequate birth preparedness and were complication ready.[12] A precision of 5% was used; correction for non-response was made and a total of 400 respondents participated in the study. The study participants were recruited using systematic sampling technique; sampling interval was calculated by dividing the sample size by average antenatal clinic attendance and the first participant was selected by balloting.
Data collection instrument and method
The quantitative data was collected over a period of four months (January to April 2015) using a facilitated, self-administered, semistructured questionnaire adapted from the safe motherhood questionnaire which was developed by the maternal and neonatal health program of JHPIEGO, an affiliate of John Hopkins University, Baltimore, Maryland, USA.[18] Data were collected on sociodemographic characteristics of the respondents, knowledge of the respondents on danger signs during pregnancy, and delivery, as well as on attitudes and practices of respondents regarding BP/CR. The adapted questionnaire was translated into local Yoruba language (for those who would find it easier to complete in Yoruba language) and back translated into English language to retain the original meaning of the questions. The questionnaire was pre-tested in another health facility to assess its internal validity. All ambiguous questions were either reframed or removed. Five research assistants were used for data collection. They were fresh Nigerian graduates and were trained on questionnaire administration for two days by the principal investigator. The training which took place at the department of community medicine, Bowen University Teaching Hospital, Ogbomoso, involved practical demonstrations.
Data analysis
The quantitative data were field-edited daily, entered using Epidata version 3.1[19] before exporting them into SPSS (version 21)[20] for analysis. Summary statistics were generated using frequencies and proportion. Associations between relevant variables were explored with Chi-square test. Where the number of cells was more than four, the likelihood chi-square test was used. The level of statistical significance was set at P<0.05. Binary logistic regression model was used to examine factors predicting BP/CR among pregnant women attending antenatal clinic. The independent variables imputed into the model were selected based on whether they had been reported as significant predictors of BP/CR by previous studies and based on whether they were significant at bi-variate level. Potential confounders such as respondents' ages and socio-economic status were controlled for and the adjusted odds ratios were obtained to identify factors that were significantly associated with BP/CR.
Ethical consideration
Ethical approval for the study was obtained from Ethical Review Committee of Bowen University Teaching Hospital, Ogbomoso, Oyo State, Nigeria. Written consents were obtained from study participants before the start of the interview. Respondents who were discovered not to be adequately prepared for deliveries and those who were not complication-ready were appropriately counseled. Confidentiality was guaranteed by making the questionnaire anonymous and entering the data into a computer with a password known only to the principal investigator. Our respondents were not compensated for volunteering to participate in the study because the study did not involve any invasive procedure and no harm was recorded for participating in the study.
Key Study Variables and Measurements
Respondents’ knowledge on danger signs during pregnancy and delivery
Nine questions were asked on common danger signs during pregnancy and each correct answer was assigned a score of two points. Respondents were categorized based on their scores as having good knowledge (score of 13-18 points), fair knowledge (score of 7-12 points) and poor knowledge (score of 6 and below). Similarly, six questions were asked on common danger signs during delivery and each correct answer was assigned a score of two points. Respondents who had 0-4 points were classified as having poor knowledge; those who scored 5-9 points were classified as fair knowledge; and those who scored 10-12 points were classified as having good knowledge.
Respondents’ attitudes towards BP/CR
A five point likert scale was used to assess this variable and the answers ranged from “strongly agreed” to “don't know.” A set of eight questions were asked with each correct answer assigned a score of two points. Respondents with a score of 0-10 points were classified as having unfavorable attitude towards BP/CR while those who scored 11-16 points were classified as having favorable attitude towards BP/CR.
Respondents’ birth preparedness and complication readiness
Respondents were asked if they had decided on where to deliver their babies, their means of transportation to the identified place of delivery, whether they had been saving money towards delivery, if they had arranged for possible blood donor, and whether they had identified a skilled birth attendant to take their deliveries. Respondents were classified as being adequately birth prepared and complication-ready if they answered “yes” to at least three of the five questions.
Classification of respondents’ social class
Using Oyedeji's classification of Social Class,[21] respondents' socio-economic status was classified into three: Low, middle and high. This classification used a composite score of respondents' educational levels and occupational types of their spouses. Educational levels of respondents as well as occupational types of their spouses were scored. The score ranged from 1 to 5 for educational level. A score of 1 stood for respondents who could barely read or write or were illiterates while a score of 5 was for respondent who have attained university education or its equivalent. For spousal occupational types, the score also ranged from 1 to 5 with 1 for the unemployed, full-time housewives and students and 5 for professionals such as doctors, lawyers and engineers. Respondent's scores from each of the occupational and educational categories were added together and rated over 10. Those who scored less than 5 were grouped into lower social class; those who scored from 5 to 7 were grouped into middle- social class; while those who scored above 7 were grouped into high social-class.
Results
A total of 420 questionnaires were administered but 400 of them were completely filled giving a response rate of 95.0%. Majority (90.0%) of our respondents belonged to 20-29 age range and were married (86.0%). More than half (55.8%) of them were in the middle socio-economic class while majority (70.0%) of them practiced Christian religion. Almost three- quarter (70.8%) of the respondents belonged to Yoruba ethnic group and more than half of them (53.2%) had 2-4 children (Table 1).
| Variables | Frequency N=400 n (%) |
|---|---|
| Age (years) | |
| ≤19 | 5 (1.2) |
| 20-29 | 155 (39.0) |
| 30-39 | 205 (51.0) |
| ≥40 | 5 (8.8) |
| Marital status | |
| Married | 344 (86.0) |
| Separated | 17 (4.2) |
| Divorced | 10 (2.5) |
| Co-habiting | 24 (6.0) |
| Single | 5 (1.2) |
| Socio-economic status | |
| Low | 97 (24.2) |
| Middle | 223 (55.8) |
| High | 80 (20.0) |
| Religion | |
| Christianity | 280 (70.0) |
| Muslim | 107 (26.8) |
| Traditional | 13 (3.2) |
| Tribe | |
| Yoruba | 283 (70.8) |
| Hausa | 48 (12.0) |
| Igbo | 69 (17.2) |
| Number of children | |
| 1 | 169 (42.2) |
| 2-4 | 213 (53.2) |
| ≥5 | 18 (4.5) |
Most (65.0%) of the women interviewed demonstrated poor knowledge of danger signs during pregnancy while 50% of them demonstrated poor knowledge regarding danger signs during labor and delivery. Only 7% and 12% of the respondents had good knowledge of danger signs during pregnancy and delivery respectively (Figure 1). Figure 2 shows that more than half (53%) of our respondents were un-favorably disposed towards BP/CR.
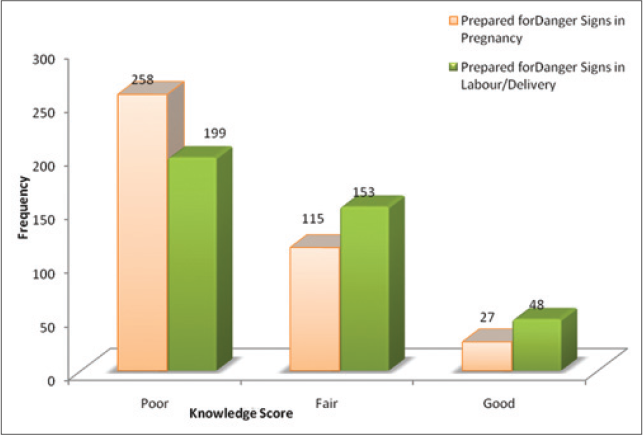
- Respondents’ Knowledge of Key Danger Signs.
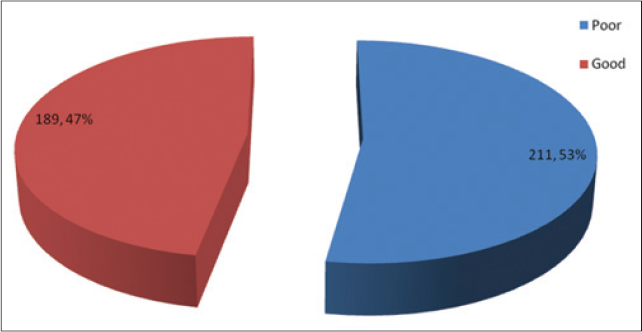
- Attitudes Towards Birth Preparedness and Complication Readiness among Respondents.
Only 161 (40.3%) of our respondents were adequately prepared for delivery and its complications (Figure 3). The proportion (51.6%) of women who were well prepared for birth and its complications was significantly higher among women in the middle socio-economic class compared to women in other socio-economic strata (p = 0.01). Similarly, the proportion (76.4%) was significantly higher among Christian women compared to women who practiced other religions (p = 0.02). Moreover, the proportion (80.1%) was significantly higher among respondents from Yoruba ethnic group compared to women from other tribes (p = 0.00). There was no significant relationship between respondents' BP/CR and other variables as shown in Table 2.
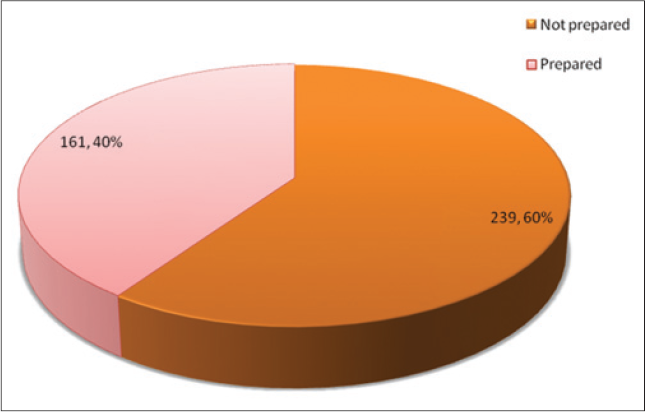
- Birth Preparedness and Complication Readiness among Respondents.
| Variables | Birth prepared N=161 n (%) | χ2 | P-value |
|---|---|---|---|
| Age groups | |||
| ≤19 | 1 (0.6) | ||
| 20 - 29 | 58 (36.0) | ||
| 30 - 39 | 84 (52.2) | ||
| ≥ 40 | 18 (11.2) | 3.23 | 0.36 |
| Marital status | |||
| Married | 145 (90.1) | ||
| Separated | 5 (3.1) | ||
| Divorced | 1 (0.6) | ||
| Co habiting | 9 (5.6) | ||
| Single | 1 (0.6) | 6.08 | 0.19 |
| Socio-economic status | |||
| Low | 34 (21.1) | ||
| Middle | 83 (51.6) | ||
| High | 44 (27.3) | 9.18 | 0.01 |
| Religion | |||
| Christianity | 123 (76.4) | ||
| Muslim | 31 (19.3) | ||
| Traditional | 7 (4.3) | 8.23 | 0.02 |
| Tribe | |||
| Yoruba | 129 (80.1) | ||
| Hausa | 13 (8.1) | ||
| Igbo | 19 (11.8) | 18.29 | 0.00 |
| Attitude towards birth preparedness | |||
| Good | 71 (44.1) | ||
| Bad | 90 (55.9) | 1.07 | 0.30 |
| Knowledge on danger signs during pregnancy | |||
| Good | 10 (6.2) | ||
| Fair | 48 (29.8) | ||
| Poor | 103 (64.0) | 0.23 | 0.89 |
| Knowledge on danger signs during labor/ delivery | |||
| Good | 15 (9.3) | ||
| Fair | 59 (36.7) | ||
| Poor | 87 (54.0) | 2.79 | 0.25 |
| Number of children | |||
| 1 63 (39.1) | |||
| 2 - 4 | 93 (57.8) | ||
| ≥5 | 5 (3.1) | 2.82 | 0.25 |
At the multi-variate level (Table 3), only socioeconomic class of respondents was found to be significantly associated with BP/CR. Respondents in the lower socio-economic classes were 42% less likely to be well prepared for birth and its complications compared to those in high socioeconomic class.
| Selected variables | Adjusted odds ratio | P-value | 95% C.I | |
|---|---|---|---|---|
| Lower | Upper | |||
| Age | ||||
| ≤ 19 (reference) | ||||
| 20-29 | 0.33 | 0.32 | 0.03 | 3.75 |
| 30-39 | 0.59 | 0.17 | 0.28 | 1.25 |
| ≥40 | 0.70 | 0.33 | 0.33 | 1.44 |
| Socio-economic status | ||||
| High (reference) | 0.58 | |||
| Middle | 0.58* | 0.12 | 0.29 | 1.15 |
| Low | 0.04 | 0.34 | 0.99 | |
| Knowledge of danger signs during pregnancy | ||||
| Good (reference) | ||||
| Fair | 1.14 | 0.76 | 0.49 | 2.69 |
| Poor | 1.19 | 0.70 | 0.49 | 2.92 |
| Knowledge of danger signs at delivery | ||||
| Good (reference) | ||||
| Fair | 1.77 | 0.10 | 0.89 | 3.52 |
| Poor | 1.42 | 0.33 | 0.70 | 2.89 |
Ref=Reference category *significant at p<0.05
Discussion
The current study revealed that only 40.3% of our respondents were adequately prepared for delivery and its complications. This result is similar to what has been reported in other studies. For instance, in a study published in 2010 on BP/CR among slum dwellers in Indore city of India, Agarwal et al. reported only 47.8% of the women interviewed were adequately prepared for birth and it complications.[9] Some studies even reported lower figures as the proportion of women who were adequately prepared for birth and its complications. In 2014, Gurmesa et al. found out that only 23% of the women in Jima zone, South West Ethiopia was well-prepared for birth and its complications.[22] Another study in Ethiopia reported that only 29.9% of the women surveyed were well-prepared for birth and its complications.[23] A figure of 23% was also reported among Ghanaian women.[11] In Nigeria, a 2011 study reported that only 35% of the pregnant women in Ile-Ife met the criteria of being well-prepared for birth.[12] Illiyasu et al, in 2010 reported that only 6.2% and 19.5% of the women interviewed in Northern Nigeria had preparations for skill birth attendants and had savings for emergencies respectively.[13] Moreover, Onayade et al in a study conducted in Ile-Ife in 2010 showed that only 11.3% of the respondents had identified possible blood donors.[14]
In contrast, some studies had reported higher proportions for women who were adequately- prepared for birth and its complications. Bintabara et al in a study conducted among women in Chamwino district of Tanzania reported that 58.2% of the respondents were well-prepared for birth.[24] Moreover, Karkee et al, in 2013, reported that 65% of the women interviewed were well-prepared for birth and its complications in Nepal.[25] The reason for higher figure reported by the Nepal study could have been due to the study setting used. The study was conducted in Kaski district of the western development region of India, an area reputed for being one of the most developed districts in India, ranking third in Human Development Index of the 75 districts in India. This laudable quality of the district could have positively affected the women's economic status thereby improving their access to health-related information sufficient to make them to be adequately-prepared for birth during antenatal visits. Tobin et al in a study conducted among pregnant women attending antenatal clinics in Edo State, Nigeria revealed that 87.4% of the respondents were adequately prepared for birth.[15] Again this study was conducted in an urban Local Government area of Edo State where the socioeconomic condition of the people is expected to have influenced their health seeking behavior positively.
In our study, we found that socio-economic class of the respondents was a strong determinant of their birth preparedness and complication readiness. Gurmesa et al reported that wealth index was one of the factors that were significantly associated with BP/CR among the women interviewed in Ethiopia.[22] Also, Robert et al identified wealth index and respondents' level of education as some of the associated factors of BP/ CR among Ghanaian women.[11] In Nigeria, Ekaete et al identified respondents' level of education as one of the factors that was significantly associated with BP/CR.[26] Socio-economic status as classified in the current study comprised of respondents' level of education and the occupational type of their spouses. Most of our respondents were in the middle socio-economic class hence they had certain degree of education and most of their spouses were employed. These two factors could have positively influenced the rate of utilization of antenatal care services among our study respondents. Antenatal care attendance increases the chances of women to access information required to make decisions relating to BP/CR. Meanwhile, factors such as knowledge of danger signs, age of respondents and their marital status, which had been reported in the literature as strong predictors of BP/CR, were found not to be significantly associated with BP/CR in the current study.
Study limitation
Due to financial and time constraints, this study was conducted among women attending antenatal clinic; the result may, therefore, not be generalizable to all women in the state or in the Nigeria at large. In order to minimize this challenge and increase the external validity of the study, the number of study participants was marginally increased above the calculated sample size. Our assumption for this was that the higher the sample size, the greater the external validity and the precision of our study.
Conclusion and Global Health Implications
According to the WHO's standards for maternal and neonatal care, all pregnant women are expected to have a written BP/CR plan. Yet, less than half of our respondents could be said to have been adequately-prepared for birth and its complications. This implies that most of the women had no arrangement for where to deliver their babies, had no concrete arrangement for means of transportation to places of delivery, had not arranged for possible blood donors, and had not identified skilled birth attendants as at the time of the survey. Studies have shown that women who take at least one of these steps were more likely to deliver with skilled birth attendants. Moreover, it has been shown that women who saved money for delivery or who had transport arrangement had higher chances of being attended by skilled birth attendants. This in-adequacy in birth preparedness could mean that majority of deliveries among our respondents will not be attended by skilled birth attendants. With such staggering figure as this, the possibility of reducing the currently high Nigerian maternal mortality ratio may be slim thus the chances of meeting the Millennium Development Goal (MDG) target appears implausible. There is an urgent need for policy re-structuring to increase the proportion of Nigerian women who would be adequately prepared for births when pregnant. First, health workers should ensure that every pregnant woman attending antenatal clinics in Nigeria have a written birth preparedness plan that will be jointly reviewed by the health workers and the women at each antenatal visit. Secondly, there is need to increase awareness on the importance of BP/CR in reducing maternal deaths; such awareness program should target all pregnant women particularly those in the lower socio-economic class in order to have profound effects. This could involve partnerships with media houses and the use of information, education and communication materials on information dissemination in Nigerian local languages. Thirdly, government may consider partnering with road transport workers in every community to ensure that all pregnant women are adequately linked to a transporter who would be willing and ready to transport them to the health facilities during labor. Lastly, there is need for improved family support for all pregnant women. Spouses should assist their wives in saving money for deliveries, and to arrange for possible blood donors should these be needed during delivery.
Financial Disclosure:
None to report.
Conflict of interest:
The authors declare that they have no conflict of interest relevant to this study.
Funding/Support:
The authors received no financial support for the research, and/or authorship of this article.
References
- Maternal Mortality: Fact Sheet 348. Geneva, Switzerland. World Health Organization 2014
- [Google Scholar]
- Estimates by WHO, UNICEF, UNFPA, the World Bank and the United Nations Population Division. Geneva, Switzerland, Department of Reproductive Health and Research World Health Organization 2014
- [Google Scholar]
- Federal Republic of Nigeria, Abuja. Nigeria Demographic and Health Survey (NDHS) 2013 Available at http://dhsprogram.com/what-we-do/survey/survey-display-438.cfm
- [Google Scholar]
- Neonatal Health Programme. Birth preparedness and complication readiness: a matrix of shared responsibilities. Original BP/CR Matrix poster published in 2001. English introductory text revised in 2004
- [Google Scholar]
- Too far to walk: Maternal mortality in context. Social Science and Medicine. 1994;38:1091.
- [CrossRef] [PubMed] [Google Scholar]
- Manual for the implementation of the new model. Geneva, Switzerland, World Health Organization 2002 (document WHO/RHR/01.30). Available at http://apps.who.int/iris/bitstream/10665/42513/1/WHO_RHR_01.30.pdf
- [Google Scholar]
- Birth and emergency preparedness in antenatal care. In: Standards for maternal and neonatal care. Geneva, Switzerland, World Health Organization 2006:1-6.
- [Google Scholar]
- Abuja, Federal Ministry of Health Nigeria 2001 Available at http://www.policyproject.com/pubs/countryreports/nig_rhstrat.pdf
- Birth preparedness and complication readiness among slum women in Indore city, India. Journal of Health, Population and Nutrition. 2010;28(4):383-91.
- [CrossRef] [PubMed] [Google Scholar]
- Birth Preparedness and Complication Readiness among Pregnant Women in Southern Ethiopia. PLoS ONE. 2011;6(6):e21432.
- [CrossRef] [PubMed] [Google Scholar]
- Birth preparedness and complication readiness: A study of post partum women in a rural district of Ghana. Public Health Research. 2014;4(6):225-233.
- [Google Scholar]
- Birth preparedness and complication readiness of pregnant women attending the three levels of health facilities Ife Central Local Government Area, Nigeria. Journal of Community Medicine and Primary Health Care. 2011;23:1-2.
- [Google Scholar]
- Birth preparedness, complication readines. and fathers' participation in maternity care in a northern Nigeria Community. African Journal of Reproductive Health. 2010;14(1):21-32.
- [Google Scholar]
- Birth preparedness and complication readiness plans of antenatal attendees in Ile-Ife, Nigeria. Nigeria Postgraduate Medical Journal. 2010;17(1):30-39.
- [CrossRef] [PubMed] [Google Scholar]
- Assessment of Birth preparedness and complication readiness among pregnant women attending Primary Health Centres in Edo State, Nigeria. Annals of Nigeria Medicine. 2014;8:76-81.
- [CrossRef] [Google Scholar]
- Monitoring Birth preparedness and complication readiness tool and indicators for maternal and newborn health. Baltimore, MD: JHPIEGO; 2004. p. :1-29.
- [Google Scholar]
- EpiData (Version 3.1). A comprehensive tool for validated entry and documentation of data. The EpiData Association, Odense Denmark 2004
- [Google Scholar]
- Socio-economic and cultural background of hospitalized children in Ilesha. Nigerian Medical Practitioner. 1985;12:111-117.
- [Google Scholar]
- Factors affecting birth preparedness and complication readiness in Jimma Zone, Southwest Ethiopia. a multilevel analysis. The Pan African Medical Journal. 2014;19:272.
- [CrossRef] [PubMed] [Google Scholar]
- Birth preparedness and complication readiness among women of child bearing age group in Goba Woreda, Oromia region, Ethiopia. BMC Pregnancy and Childbirth. 2014;14:282.
- [CrossRef] [PubMed] [Google Scholar]
- Birth preparedness and complication readiness among recently delivered women in Chamwino district, central Tanzania. a cross-sectional study. Reproductive Health. 2015;16:12(1):44.
- [CrossRef] [PubMed] [Google Scholar]
- Birth preparedness and skilled attendance at birth in Nepal: Implication for achieving Millenium Development Goal 5. Midwifery. 2013;29(10):1206-1210.
- [CrossRef] [PubMed] [Google Scholar]
- Assessment of birth preparedness and complication readiness among pregnant women attending Primary Health Care Centers in Edo State, Nigeria. Annals of Nigerian Medicine. 2014;8(2):76-81.
- [CrossRef] [Google Scholar]





