Translate this page into:
Costs and Patterns of Financing Maternal Health Care Services in Rural Communities in Northern Nigeria: Evidence for Designing National Fee Exemption Policy
✉Corresponding author email: abukurfi@gmail.com
-
Received: ,
Accepted: ,
Abstract
Background:
As population and access to information increases, so does the demand for health services. Unfortunately, many people who genuinely require these services do not usually have access to them. To increase access, various financing options have been used. Despite this, maternal morbidity and mortality rates remain high and spending is still largely out of pocket. This study assesses maternal health problems, preferred sources of care and the pattern of financing in a semi-rural community in North Western part of Nigeria.
Methodology:
A cross-sectional descriptive study design was used. The study population consisted of women within the reproductive age group who had experienced childbirth 12 months or less prior to the study. A sample size of 240 was drawn using cluster and random sampling techniques. Interviewer administered questionnaires were used and the results were analyzed using Statistical Package for Social Sciences (SPSS).
Results:
The mean age of the respondents was 29 years and 49% had no personal income. Fever was the commonest problem. Although majority received antenatal care, those who lacked antenatal care mostly cited financial difficulties. Nearly half of the women delivered at home as opposed to a health facility. On average, women spent between Nigerian Naira (N) Nl, 350-NI4,850 (USD$9-99) for a total package of maternal health services. Out of pocket spending by the husbands or household heads and the women themselves accounted for 73.3% of expenses.
Conclusion and Public Health Implications:
In Nigeria, women are still vulnerable to common and preventable causes of maternal morbidity and mortality due to lack of access to antenatal health care. Out of pocket spending is still a popular method of financing. Harmonization of fee exemption policies can improve access to maternal healthcare.
Keywords
maternal health
maternal healthcare
financing
rural health care
Nigeria
health care financing
fee exemption
Introduction
More than two decades after the launch of the Safe Motherhood Campaign in 1987, over half a million women most of whom live in developing countries continue to die of maternal causes each year.[1] Nigeria accounts for approximately 2% of the world population; yet with an estimated 59,000 annual maternal deaths and a maternal mortality of 545 per 100,000, Nigeria is a leading contributor to the high maternal mortality rate in Sub-Saharan Africa.[2] Nigeria also accounts for almost 10% of the world's maternal deaths.[3] There are several reasons advanced for this high level of maternal mortality. According to the 2008 National Demographic Health Survey, only 35% of Nigerian women deliver in hospitals and the leading barrier to access is lack of finances for treatment. One in three women mentioned distance and transportation difficulties as the major problem while 41% of the respondents were concerned about lack of drugs.[4] Some other factors that prevent women from accessing maternal health services include indirect costs, women's lack of authority for decision-making and multiple demands on their time, as well as the attitude of healthcare workers.[5]
Many of the common causes of maternal mortality in Nigeria such as post-partum hemorrhage, sepsis and anemia are readily preventable, detectable and manageable. Key interventions such as ensuring antenatal care attendance and having a skilled attendant at delivery have also been identified and used to improve maternal health care in many countries. However, the use of such interventions has been found to be limited in developing countries like Nigeria.[6] One of the reasons for this is the level of health care financing, especially by the government. The introduction of user fees has been widely implemented in government health programs as a means of alleviating pressure on constrained budgets as demands for services increase. However, this has proved to be a significant barrier to access. As more people realize that health systems should not only be concerned with improving peoples' health but also protect them against the financial costs of illness, there has been growing calls world-wide for the removal of user fees (especially for basic health services at the primary health care level). This is important in view of the fact that currently, out-of-pocket expenditure represents 70% of health expenditure in Nigeria.[7] Apart from increasing access, it will also reduce morbidity and mortality, especially for the vulnerable groups such as young children and pregnant women. These exemptions may however not ensure universal access because informal fees and other costs associated with accessing healthcare are not affected; furthermore, exemption mechanisms may be poorly implemented.
Many sub-Saharan African countries have introduced “free” maternity services in a bid to eliminate poverty as an important barrier to maternal health service access and utilization. Some states in Northern Nigeria such as Kano, Katsina, Kaduna and the Federal Capital Territory, Abuja have also introduced similar schemes in public hospitals. One of the visible positive effects of such schemes has been the recorded increase in the number of women attending formal antenatal and delivery services. However, without adequate planning and financing, “free” maternity services could result in overstretched facilities, overworked staff and dissatisfied clients.
Objectives
This study was conducted in a community where ‘free’ maternal health services had been instituted in government owned health facilities, in order to assess the actual financial implications for the women and their families. Overall, we sought to provide evidence for proper planning and equitable allocation of resources, thereby increasing access to maternal health services. In general, the objectives of the study were to determine the cost of maternal health care in the designated community; and determine the pattern of financing of maternal healthcare in the community. Specifically, we sought to (1) identify the commonest maternal health problems in the community; and (2) identify the sources of maternal healthcare in the community.
Methods
Study area
Idon is one of the wards that constitute Kajuru Local Government Area (LGA) in the southern part of Kaduna state, North Western Nigeria. It is less than one hour's drive from the state capital and comprises 5 communities namely -Ayakun, Upinin, Akyagba, Ikawur and Idon gida -with a total population of 8,952. Idon is a densely populated semi-rural area and the major ethnic group is the Kadara who are mostly Hausa-speaking. Other tribes are the Hausa, Fulani, Yoruba and Igbo who are attracted by the agricultural and commercial activities as well as the proximity to a major road. The main occupations are subsistence farming, cattle rearing, trading, and some civil service. The commonest source of water is from shallow wells though the government has provided boreholes for the community. Waste disposal is by open dumping in specified areas and most houses have pit latrines. There is one general hospital and one primary health center that serve the entire ward; there is also one public primary school and a secondary school. Most girls get married in their teens and start child bearing soon after.
Study population
The study population comprised of women, resident in Idon, within the ages 15-49 years who had experienced childbirth within one year preceding the commencement of the study and was willing to participate. Girls below the age of 15 years, women above the age of 49 years, women who had not been pregnant and delivered within the preceding twelve months and those who refused to participate were excluded from the study.
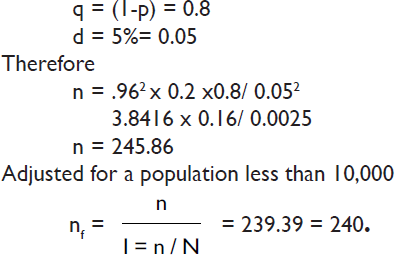
Sample size determination
The sample size for the study was determined using the formula n = z2 pq/d2 where
z = 1.96 at 95% confidence interval
p = 0.2 (this was the proportion of women who had been pregnant and delivered within the preceding one year estimated from a pilot study in the same area)
Study method
A cross sectional descriptive study was carried out between May and June 2010. A minimum sample size of 240 was estimated using a p value of 0.2 (which was obtained from a pilot study in the same LGA) and a significance level of 5%. A two-stage sampling method was used. First, the study area (ward) was divided into five clusters (communities) and Idon gida was randomly selected. Houses within the chosen cluster were numbered and then randomly selected to eliminate bias. Where there was more than one eligible respondent in a household, selection was made by balloting. The process was repeated until the minimum sample size was attained.
Study instrument
The questionnaires consisted of six sections covering the socio-demographic profile, the obstetric history / common maternal problems, the sources of maternal healthcare services, the cost of the services, the pattern of financing and recommendations for the improvement of the financing of maternal care. The pre-tested interviewer-administered questionnaires were used to interview women within the reproductive age group who had been pregnant and delivered within the last twelve months.
Data management
The interviewer-administered questionnaires were manually checked for completeness and consistency before data entry and analysis using the statistical package for social sciences (SPSS) version 16.0.
Ethical Approval
Ethical clearance was obtained from the Department of Community Medicine, Ahmadu Bello University, Zaria. Permission was sought and obtained from the local government and from the community head before the commencement of the study. In addition, before the administration of questionnaires, the aim of the study was explained to participants. Their verbal consent was obtained and their privacy and confidentiality ensured.
Results
Socio-demographic characteristics
The minimum age of the respondents was 16 and the maximum age was 45, with a mean age of 29 years (+2SD). Most of them were Kadara and Hausa by ethnicity (n=128 and 34 respectively), and Christians by religion (n=192). 220 women were married. Forty-five respondents were full time housewives (totally reliant on their spouses) but the majority were farmers (n=87). The majority of the husbands were also farmers (n=104). Fifty three women had no formal education. Compared with the husbands, fewer respondents (n=34, n=39) had post-secondary education. The average monthly income for the respondents in this study was N2,196. At the rate of N150 to a dollar, this equals US$14.6 per month or about US$0.5 per day. Most of the respondents (n=1 17) had no income. Only 3 of them earned more than US$66.70 monthly. In stark contrast to the income levels, the average household consisted of eight individuals.
| Characteristics | Categories | Frequency | Percent |
|---|---|---|---|
| Age (years) | 15-19 | 12 | 5.0 |
| 20-24 | 53 | 22.1 | |
| 25-29 | 78 | 32.5 | |
| 30-34 | 40 | 16.7 | |
| 35-40 | 49 | 20.4 | |
| 40- 45 | 8 | 3.3 | |
| Tribe | Kadara | 128 | 53.3 |
| Hausa/Fulani | 34 | 14.2 | |
| Igbo | 21 | 8.8 | |
| Yoruba | 4 | 1.7 | |
| Others | 53 | 22.0 | |
| Religion | Christianity | 192 | 80.0 |
| Islam | 48 | 20.0 | |
| Marital status | Married | 220 | 91.7 |
| Divorced | 11 | 4.6 | |
| Single | 9 | 3.8 | |
| Educational level | None | 53 | 22.1 |
| Primary | 64 | 26.7 | |
| Secondary | 89 | 37.1 | |
| Post-secondary | 34 | 14.2 | |
| Occupational status | Farming | 87 | 36.2 |
| Business/trading | 53 | 22.1 | |
| Civil servant | 48 | 20.0 | |
| Private employee | 45 | 18.8 | |
| Unemployed | 7 | 2.9 | |
Maternal Health problems
Nearly half (n=117) had had one or more previous abortions-either spontaneous or induced. Ninety one of the respondents had medical problems that necessitated treatment in their last pregnancy. Fever, which could be characteristic of malaria or other infections, was the commonest health problem that made women seek treatment during their last pregnancy (n= 27). Hemorrhage (n=16) and anemia (n=15) were also mentioned (see table 2).
| Health problem | Frequency | Percent |
|---|---|---|
| Fever | 27 | 29.6 |
| Hemorrhage | 16 | 17.6 |
| Anemia | 15 | 16.5 |
| Severe vomiting Prolonged obstructed | 14 | 15.4 |
| labor | 6 | 6.6 |
| Hypertension | 5 | 5.5 |
| Others | 8 | 8.8 |
| Total | 91 | 100 |
Sources of maternal healthcare
209 of the respondents received ante-natal care from a variety of sources-public and private. One hundred and four women received ante-natal care from the primary health center, their main reasons being close proximity to the center (n=76) and the time saved (n=16). Eighty-five women received ante-natal care from the general hospital which was further away; for them, the experience of the health workers (n=41) and distance (n=27) as well as cost (n=12) were the main factors that influenced their choice. Only 20 women attended antenatal care at a private healthcare facility. Of the 31 women who did not receive ante-natal care, 18 cited financial difficulties as the main reason. Others mentioned geographical distance (n=6) and cultural/ religious reasons (n=7). In addition, 101 women -nearly half -delivered their babies at home. Only 40 out of the 240 respondents (one-sixth) received all three aspects of maternal healthcare (antenatal, delivery and post-natal care).
Antenatal Care costs
As depicted in table 3, most of the respondents (n=127) spent nothing on transportation costs for antenatal care because they walked to the facility of their choice. Ultrasound scans were responsible for 62.8% N110,805 or (US$738.70) of total antenatal care costs for all the respondents while medications and laboratory tests accounted for 11.6% N20,430 or (US$136.20) and 8.4% N14,869.5 or (US$99.13) respectively. Transportation costs amounted to only N6640.5 or (US$44.27). The average amount spent on antenatal care per woman was N735 or (US$4.90).
| Category | Services | Cost (Naira) | Percent |
|---|---|---|---|
| Antenatal care | Ultrasound scan | 110800 | 62.8 |
| Medications | 20430 | 11.6 | |
| Laboratory investigations | 14870 | 8.4 | |
| Administration | 9440 | 5.3 | |
| Transportation | 6640 | 3.9 | |
| Hospital admission | 5250 | 3.0 | |
| Other treatment | 8910 | 5.0 | |
| Total | 176340 | 100 | |
| Delivery care | Caesarean section | 167000 | 65.7 |
| Normal Delivery | 49000 | 19.3 | |
| Delivery materials | 14180 | 5.6 | |
| Medications | 11900 | 4.7 | |
| Transportation | 11260 | 4.4 | |
| Other treatment | 840 | 0.3 | |
| Total | 254180 | 100 | |
| Postnatal care | Family planning | 6650 | 45.5 |
| Drugs | 6020 | 41.2 | |
| Transport | 1950 | 13.3 | |
| Total | 14620 | 100 | |
| Outcome of delay in treatment | Inability to pay immediately | ||
| Yes (%) | No (%) | Total frequency (%) | |
| No difference | 11(37.9) | 26 (100.0) | 37(67.3) |
| Complications | 12(41.4) | 0(0.0) | 12(21.8) |
| Loss of pregnancy | 6(20.7) | 0(0.0) | 6(10.9) |
| Total | 29(100.0) | 26(100.0) | 55(100.0) |
| X2= 23.989, df = 2, p=0.000 | |||
Delivery care costs
The cost of delivery ranged from free to N5650.5 or (US$376.70) with an average cost of N450 or (US$3) for normal deliveries as against N13950 or (US$93) for complicated deliveries requiring Caesarean sections. The cost of caesarean sections accounted for 65.7 % N166,995 or (US$1,113.30) of total delivery costs for all the respondents while normal delivery accounted for only 19.3% N49005 or (US$326.70). Medications and transportation were responsible for N11895 US$79.30 and N11260.7 US$75.07 respectively.
Post-natal care costs
Less than 50% of the women in this study had postnatal care (n=106) compared to number that received antenatal care (n=209). The average cost of post-natal care per woman was less than N288 or US$1.92.
Total maternal care costs
The average cost of total maternal care therefore came to approximately N1350 or US$9 for normal delivery and N14850 or US$99 for caesarean sections per woman.
Pattern of financing
Sixty women confirmed that the maternal services they received were ‘free’ or paid for by the government. In most cases however, the husband or household head paid (n=134), while in 42 cases, the women themselves had to pay for the services. In four cases, a religious or charity organization paid for the women. Furthermore, 63 of the respondents had at one time or the other had difficulties in paying for maternal health services. Of this number, 46 decided to manage without treatment, while 16 decided to sell an asset and one took a loan from friends. Twelve out of the 29 cases that were delayed resulted in avoidable complications and in 6 cases there were miscarriages. In response to how they felt the government could assist them in the financing of maternal healthcare, 53 of the respondents felt it was not in their place to recommend for the government and thus refused to answer this question. Fifty-one women reported that they were satisfied with the current state of affairs, and that the government should continue with the free maternal and child health scheme. Six respondents felt that women also needed to be empowered financially.
In addition, there were statistically significant associations between the monthly income of the women and difficulty in payment for maternal health services (p=0.000, p<0.05); as well as between delay in treatment due to difficulty in payment and the outcomes of the delay (p=0.000, p<0.05).
Limitations
Many respondents could not accurately determine the income of their spouses so this information was not requested. Determining their own income was also a challenge for some women as their income varied from day to day or week to week; estimates were therefore used. In addition, the findings of the study cannot be generalized for other communities except those with similar characteristics.
Discussion
In this study, 53 of the women did not have any formal education. This finding is not unusual in the North Western part of Nigeria although there is increasing focus on girl child education. Female education is also a critical factor in maternal and child mortality reduction because the woman's income is more likely to be used for household needs such as food, education, medicine and other family needs.[8] Educated women are also more likely to make important family decisions about nutrition, healthcare and the use of resources.
The average monthly income for the respondents in this study was N2,196. At the rate of N150 to a dollar, this equals US$14.6 per month or about US$0.5 per day. These findings highlight the socioeconomic status of women living in the area. Seventy-one households consisted of 10 to 14 people. The more individuals who need to be cared for may mean less money is available for women's maternal healthcare needs.
Fever, which could be characteristic of malaria or other infections, was the commonest health problem; it was followed by hemorrhage. This is worth noting in view of the fact that antimalarial and antibiotics are part of the essential drug list in Nigeria; misoprostol has also been recently added. Similar studies done in Maiduguri in Northern Nigeria and the Ejisu district in Ghana found hemorrhage, obstructed labour, hypertensive diseases in pregnancy and sepsis to be important contributors to maternal morbidity and mortality.[2,10]
Many factors limit the utilization of maternal health services in the rural areas in developing countries including Nigeria. These factors include the availability, accessibility and quality of services as well as the social characteristics of the users and their communities. In this study, the majority of the women who did not receive ante-natal care cited financial difficulty as the main reason. In another study in Bangladesh which reviewed findings from a national survey, almost half of the women were found to have had complications during pregnancy however only one in three sought treatment from a trained provider, the principal reason being the cost of care.[8]
While most respondents who received ante-natal care considered distance to be the major factor that influenced their choice of source of care, only 16 mentioned financial costs or affordability. This was most likely due to the state government's free maternal and child health package was offered at both public facilities in the community-the primary health center and the general hospital-which catered for the needs of over 90% of the women in this study. The package was not offered at private health facilities and accordingly, affordability was not a factor in the choice of private hospitals. Other studies have also shown that the cost of seeking institutionalized care can act as a deterrent in the case of poor households.[9] Additionally, there is evidence that medical expenses can push even non-poor households below the poverty line.[11]
Health workers in the general hospital were considered to be most experienced; in addition to being the most geographically accessible, primary health centers were considered to have the least waiting times to service. It must be noted that despite the high rates of antenatal care attendance (only 31 did not attend at all), 101 women-nearly half-delivered their babies at home. This supports the 2008 National Demographic Health Survey findings that states that of the 70% of births that occur in rural areas only 27% are assisted by skilled birth attendants. [4]
Nearly every woman who attended antenatal care at the general hospital delivered at those hospitals whereas of the 104 women who utilized the primary health center, only 31 deliveries were taken. The reasons are not farfetched. Culturally, many women in the area prefer to deliver at home and usually have a female relative/ neighbor/ friend who double as a local midwife or traditional birth attendant to assist them. Indeed, some studies show that Nigerian women rate the services of traditional birth attendants as being better than that of medical healthcare practitioners especially with regards to interpersonal relationships and flexibility of payment options.
Some of the health workers, especially from public health facilities, were also said to assist at home deliveries. Apart from this, the primary health facility in the study area lacked adequate facilities to effectively manage obstetric emergencies. For example, there was no electricity or running water in the facility. It was manned by Community Health Extension Workers and a few nurses who gave health talks, routine antenatal services, immunization and the treatment of common diseases such as malaria. Cases that appeared difficult to handle or occurred at night were usually referred to the general hospital. Many women were aware of the need for specialized care during the antenatal and delivery periods but not during postnatal period. For many of them, the essence of being pregnant and cared for during that period is to have a safe delivery.
Several studies on out-of-pocket costs of maternity care in low income countries in sub-Saharan Africa and Asia have consistently shown that out-of-pocket costs of maternity care vary considerably depending on the type of delivery (normal or complicated), as well as the type of health facility (public vs. private) and the level of the health system.[11] In Uganda, Malawi and Ghana, for example, out-of-pocket costs for normal delivery (including user fees, travel costs and accommodation costs) ranged from US$2.30-22.80 in Uganda, US$0.40-7.90 in Malawi, and US$12.60-20.70 in Ghana. Fees for complicated deliveries were higher, ranging from US$13-59 in Uganda to US$68-140 in Ghana.[12] With respect to the mean cost of delivery by place of delivery, it is by far much cheaper for the women to deliver at home N332.92 or (USD2.12) than in the private health facilities N12,638.57 or (USD84.25) in the community.
In other studies in Kenya and Tanzania, costs of normal delivery were significantly higher at private facilities than at government facilities. In Kenya, costs at private/mission facilities were twice as high as those incurred at government facilities, and in Tanzania, these costs were almost four times as high. In contrast, mean costs at mission health centers in Burkina Faso (US$3.1) were lower than those incurred at government health centers because such sites subsidized the costs of drugs and supplies.[11] Although only 18 of the respondents in this study paid unofficial or extra fees, these fees have been found to be quite substantial in some studies. For instance, in a study in Bangladesh, unofficial fees were on average 12 times higher than official fees. [13] Another study in India reported that such fees were five times the formal fees, and represented 80% of total out-of-pocket expenses.[14] A Tanzanian study also found that 73.3% of spending was actually out of pocket which is in line with the over 70% estimated for Sub-Saharan Africa.[15] Notably, none of the respondents was covered by any form of health insurance whatsoever. Considering the fact that there is a National Health Insurance Scheme in place, which can help to prevent the catastrophic effects of healthcare financing and efforts, are being made to expand the scheme to rural areas, opportunities exist for intervention in the community. It might also be interesting to compare the pattern of maternal healthcare financing in the study area prior to the commencement of the free maternal health scheme and after.
It is worthy of note that treatment was only delayed in less than half of the cases that reported difficulties in paying for maternal health services. This was due mostly to familiarity with the health workers and in some instances, compassion. This brings to the fore the importance of the attitudes of health workers in maternal healthcare. However, six women still ended up with miscarriages.
Most women in the study felt it was improper for them to recommend for the government or that things should be left as they were as far as maternal healthcare financing and services were concerned. Interestingly, this highlights the social status of many women who cannot picture themselves as voices to be heard or as agents of change. Many of them were among the 60 who did not pay for the services. Others were concerned about the extension of the programmer to more rural areas, private hospitals and the less privileged. Adequate free drugs and the financial empowerment of women were also mentioned; the latter they said could be done through loans and setting up of small scale industries and government-assisted local cooperative groups. Very few women felt that more awareness needed to be created among the husbands and household heads on the importance of maternal healthcare for women. They felt the men could be reached at social gatherings and places of worship in the community.
Conclusion and Public Health Implications
From the research findings, the commonest maternal health problems identified by the women were fever, hemorrhage and anemia. The sources of maternal healthcare available to the women in the community were the traditional birth attendants, the private hospitals, the primary health center and the general hospital. A lot of women in the community still delivered in their homes as opposed to health facilities where there was a higher chance of having a skilled attendant at delivery and thus preventing maternal and infant mortality. The problems encountered in seeking maternal healthcareinclude financial difficulties, socio-cultural factors and distance. Most of the spending was still out of pocket. On the average, the women lived in households of 5-9 individuals and the majority (n=117) had no income; but average earnings were less than half a dollar a day which translates to N2190 or (US$14.6) a month or N26280 or (US$175.2) annually. On the other hand, the average total cost of maternal care was NI, 323 or (US$9) for normal delivery which is almost month's earnings. Where Caesarean sections were involved, the average total cost of maternal care was NI4,873 or (US$99), almost equivalent to seven months (untouched) earnings.
Recommendations
The registration and training of traditional birth attendants in the community.
The institution of regular home visits by the health workers to pregnant and recently delivered women.
Increased advocacy to the husbands, traditional and religious leaders to increase support for health facility utilization.
Improvement of health facilities as well as retraining of staff.
The introduction of a harmonized fee exemption policy (including the private sector) or community health insurance scheme.
Competing interests:
The authors declare that they have no competing interests.
Acknowledgements:
The authors would like to acknowledge the assistance of the Kaduna State Ministry of Health and the Kajuru Local Government Secretariat.
References
- Cost effectiveness strategies for maternal and neonatal health in developing countries. British Medical Journal. 2002;331:1107.
- [CrossRef] [PubMed] [Google Scholar]
- Trends in maternal mortality at the University of Maiduguri teaching hospital, Maiduguri, Nigeria- a five year review. Nigerian Medical Journal. 2010;51:147-51.
- [Google Scholar]
- Curbing maternal and child mortality: The Nigerian experience. International Journal of Nursing and Midwifery. 2012;4(3):33-39.
- [CrossRef] [Google Scholar]
- National Population Commission (NPC) Nigeria and ORC Macro. In: Nigerian National Demographic and Health Survey. Calverton Maryland: NPC and ORC Macro; 2008.
- [Google Scholar]
- Costs of near miss obstetric complications for women and their families in Benin and Ghana. Health Policy and Planning. 2003;18:383-90.
- [CrossRef] [PubMed] [Google Scholar]
- Safe Motherhood interventions in low income countries: an economic justification and evidence of cost-effectiveness. Health Policy. 2000;53(3):201-28.
- [CrossRef] [PubMed] [Google Scholar]
- Health expenditure and health status in Northern and Southern Nigeria: a comparative analysis using NHA framework. Paper presented at CSAE conference, Oxford University, UK 2010. (accessed )
- [Google Scholar]
- Maternal Healthcare seeking behaviour in Bangladesh: findings from a national survey. International Family Planning Perspectives,. 2007;33(2):75-82.
- [CrossRef] [PubMed] [Google Scholar]
- Can mothers afford maternal health care costs? User costs of maternity services in rural Tanzania. African Journal of Reproductive Health. 2002;6:66-73.
- [CrossRef] [PubMed] [Google Scholar]
- Maternal mortality and related factors in Ejisu district, Ghana. East African Medical Journal. 1994;71(10):656-60.
- [Google Scholar]
- Out of pocket costs for facility based maternity care in three African countries. Health Policy and Planning. 2009;24(4):289-300.
- [CrossRef] [PubMed] [Google Scholar]
- Cost of maternal healthcare services in three Anglophone African countries. International Journal of Health Planning and Management. 2003;18:3-22.
- [CrossRef] [PubMed] [Google Scholar]
- What are the economic consequences for households of illness and paying for healthcare in low and middle income country contexts? Social Science and Medicine. 2005;62:858-65.
- [CrossRef] [PubMed] [Google Scholar]
- Formal and informal fees for maternal health services in five countries; policies, practices and perspectives. 2005. POLICY Working Paper Series. :16. (accessed )
- [Google Scholar]
- User fee exemptions are not enough: out of pocket payments for free delivery services in rural Tanzania. Tropical Medicine and International Health. 2008;13(12):1442-1451.
- [CrossRef] [PubMed] [Google Scholar]





