Translate this page into:
Social Determinants of Depression: Social Cohesion, Negative Life Events, and Depression Among People Living with HIV/Aids in Nigeria, West Africa
✉Corresponding author email: oorelopehospital@gmail.com
-
Received: ,
Accepted: ,
Abstract
Background:
People Living with HIV/AIDS (PLWHA) continue to face persistent and deep rooted social barriers. Incidentally, studies in social determinants of depression are very limited, necessitating this study, which examined social determinants of depression and the impact of these determinants on depression.
Methods:
This was a hospital based, cross sectional descriptive study of three hundred adult HIV/AIDS patients, attending the HIV clinic of Kwara State Specialist Hospital, Sobi, Ilorin, Nigeria. Depressive symptoms were measured by the PHQ-9 rating scale. Three variables of social determinants of depression: socio-economic status (years of school and self-reported economic status of family), social cohesion, and negative life events were examined.
Results:
The self-reported economic status of the family varied from good 35(11.7%), average 162(54%), and poor among 103(34.3%) of the respondents. Social cohesion was low in 199(66.3%), fair in 65(21.7%) and high among 36(12%) of the respondents. There was significant association between social cohesion, negative life events, and depression.
Conclusion and Global Health Implications:
Income was the most significant socio-economic determinant. Majority had very low social cohesion and more negative life events, while those with below average years of schooling were more depressed. These are statistically significant. Social determinants of depression should be given a lot of emphasis, when addressing the issue of depression, if we are to meaningfully tackle this increasing scourge in our society.
Keywords
Depression
Social determinants
PLWHA
Social cohesion
Negative life events
Nigeria
People living with HIV/AIDS
Background and Introduction
Depression is the most frequently observed psy-chiatric disorders among HIV/AIDS patients, with prevalence of two to three times higher than in the general population.[1]
The Diagnostic and Statistical Manual of Mental Disorders (DSM IVTR) describes major depressive disorder as being accompanied by clinically significant distress or impairment in social, occupational or other important areas of functioning.[2]
More recent work on the social influences on depression, found a significant correlation between social factors and depression.[3] During the past few decades, the depth and breadth of our understanding of health issues has greatly increased because of the bio-psycho-social medical model. Important to this understanding is the concept of Social Determinants of Health (SDH). SDH focuses on the “causes of the causes”-the fundamental structures of social hierarchy and the socially determined conditions. SDH are primarily responsible for health inequities-the unfair and avoidable differences in health status. The concept of social determinants seeks to theoretically and empirically explain how social organization affects health.
Economic status or variables related to income or financial status is reported to be significant determinant of depression.[4] The socio demographic factors of age, gender, marital status, education and income are important factors, in explaining the variability in depression prevalence rates. Key North American Studies, particularly the Epidemiologic Catchment Area study,[5] and the Ontario Health Survey[6] found prevalence rates of 2.8% and 3% based on age and gender respectively.
Pattern and Colleagues found significant inter-action among age, sex, marital status and depression. Consistently, women have nearly double or triple prevalence rates than men. Several recent studies confirmed a strong inverse relationship between SES and mental disorder.[7] People in the lowest socio-economic class are more likely to suffer from psychiatric disorder, than those in the highest class.[8]
The social determinants of depression are social, economic and health condition people are born into and live. Poor social and economic circumstances affect health throughout life.[9] Social Support and Social Cohesion have been identified as playing major roles in the transmission and progression of HIV/AIDS and also depression.[9] While Social support enables people to negotiate life's crisis, social cohesion helps to stabilize health threatening situations by including and accepting people, and by enabling them to participate freely within the families, the committees and the society.
Though literature abounds in other parts of the world on social determinants of depression, there is paucity of data in Africa in general, and Nigeria in particular, among People Living with HIV/AIDS (PLWHA). This study explores social determinants of health and depression among HIV/AIDS patients, in North Central Nigeria.
Methods
This study was conducted at HIV/AIDS treatment center in the Sobi Specialist Hospital, Ilorin, Kwara State, located in the North Central Nigeria. The HIV/AIDS treatment center started in the hospital in May, 2009. About 800 patients have been enrolled and over 600 are on Highly Active Antiretroviral Therapy (HAART). The center is currently being founded by an international Non-Governmental Organization (NGO), Friends for Global Health.
This is a descriptive, cross-sectional study carried out from March 1st to July 30th, 2013. The inclusion criteria were all concerted depressed HIV positive patients, who presented at the Clinic. The exclusion criteria were the critically-ill patients. The Patients Health Questionnaire -PHQ-9 was administered to screen for depression, until the estimated sample size of 300 was obtained. Respondents who scored one and more were assessed clinically for depression. The severity of the depression was further classified as minimal, mild-to-moderate and severe. The three keys of social determinants of depression (SDS) were assessed and the association with depression sought.
The sample size was estimated using the Fisher formula[10], using 21.3% from a previous study[11], as the best estimate of depressive disorders among People Living with HIV/AIDS (PLWHA). A minimum size of 218 was calculated using Fisher's formula but 300 was used to increase the power and reliability of the study. Pretesting was carried out at the Kwara State Civil Service Hospital, using 30 respondents (10% of the sample size).
Ethical approval was obtained from the Ethical Review Committee of the Kwara State Ministry of Health before commencement of the study. An interviewer administered questionnaire was used.
Based on existing research[12], we used three key SDH: socioeconomic status, social cohesion and negative life events. Socioeconomic status included two indicators: years of schooling and self-reported economic status of the family, in general, in the previous year. Categories for years of schooling were as follows: above average (7 years and above), average (1-6 years) and below average (0 year). Economic status of the family was self-reported as good, average or poor. Social cohesion was assessed from responses to two questions: (1) In the previous year, how often did you ask someone for help when you had problems? (Never = 1; Seldom = 2; Sometimes = 3; Often = 4), and when you had problems? (spouse or lover; parents, brothers, sisters or children; other relatives; people outside the family; organization or schools with whom you are affiliated; government, party or trade unions; religious or non-governmental organizations; other organizations) (no = 0; yes = 1). Negative life events were assessed using a 12-item scale (serious illness in oneself, serious illness in the family, financial difficulties, conflict with spouse, conflict with other family members, conflict with people in the village, conflict between family members, infertility issues, problems at work or school, problems in an intimate relationship, abuse, and other events).[13] For each life event that occurred in the last year, or that occurred earlier but continued to have a psychological effect during the past 12 months, the respondent indicated when the life event occurred, its effect (positive or negative) and the length of time over the last year that the psychological effect lasted. We used the sum of the number of life events with a negative effect as a measure of negative life events.
Age, gender, marital status, education level, self-rated financial status, social support and social cohesion, employment status and estimated monthly income were the socio-demographic variables and potential confounders. Marital status, educational level, and occupation were assessed. Monthly income was assessed using the minimum wage stipulated by the Federal Government of Nigeria, which is Twenty Thousand Naira (N20,000), which is about $133.
Completed questionnaire and measurements were entered into a computer data base. The data were analyzed using the epidemiological information (Epi-info) 2005 software package developed by the US Centers for Disease Control and Prevention (CDC). The 2 by 2 contingency tables were used to carry out Chi-square test and to find out the level of significance; p-values that are less than 0.05 were regarded as statistically significant.
Results
Table 1, shows the socio-demographic characteri-stics of the respondents. In all, 170 sero-positive respondents with depression were recruited into the study. The age range 36-40 years, had the highest number of respondents 50(29.4%). Females 139(81.8%) outnumbered males 31(18.2%) giving a male: female ratio of 1:4.5. Predominantly, 139(81.8%) were Muslims; Christians constituted 30(17.6%); with l(0.6) Traditional believers. Fourteen (8.2%) were married while the same number were single. One hundred and sixteen (68.3%) were separated/ divorce while 26(15.3) were widow/widower. The majority of the respondents 56(32.9%) had no formal education; 55(32.4%) had primary education; while 42(24.7%) had secondary education. Only 17(10.0%) attended tertiary institution. Majority, 9l(53.5%) were traders, while 14(8.2%) were unemployed and six (3.5%) were students.
| Variable | N = 170 | (%) |
|---|---|---|
| Age group (years) | ||
| < 26 | 19 | 11.2 |
| 26 - 30 | 27 | 15.9 |
| 31 - 35 | 20 | 11.8 |
| 36 - 40 | 50 | 29.4 |
| 41 - 45 | 11 | 6.5 |
| 46 - 50 | 19 | 11.1 |
| 51 - 55 | 6 | 3.5 |
| 56 - 60 | 11 | 6.5 |
| >60 | 7 | 4.1 |
| Gender | ||
| Male | 31 | 18.2 |
| Female | 139 | 81.8 |
| Ethnicity | ||
| Hausa | 39 | 22.9 |
| Yoruba | 92 | 54.1 |
| Igbo | 28 | 16.5 |
| Others | 11 | 6.5 |
| Religion | ||
| Christianity | 30 | 17.6 |
| Islam | 139 | 81.8 |
| Traditional | 1 | 0.6 |
| Marital Status | ||
| Single | 14 | 8.2 |
| Married | 14 | 8.2 |
| Separated/Divorced | 116 | 68.3 |
| Widowed/Widower | 26 | 15.3 |
| Educational level | ||
| Non-Formal | 56 | 32.9 |
| Primary | 55 | 32.4 |
| Secondary | 42 | 24.7 |
| Tertiary | 17 | 10.0 |
| Occupation | ||
| Trader | 91 | 53.5 |
| Civil servant | 16 | 9.4 |
| Self employed | 43 | 25.4 |
| Unemployed | 14 | 8.2 |
| Students | 6 | 3.5 |
| Monthly Income (N) | ||
| No Income | 20 | 11.8 |
| ≤20000 | 129 | 75.9 |
| 20001-30000 | 10 | 5.8 |
| 30001-40000 | 6 | 3.5 |
| 40001-50000 | 3 | 1.8 |
| >50000 | 2 | 1.2 |
Table 2 displays the variations according to self-reported economic status of the family, years of schooling, social cohesion in the previous year and negative life events. Eighty-eight (5l.8%) had poor, 62 (36.5%), had average, while 20 (11.7%) had good self-reported economic status. Those with below average year of schooling or about 80 (47.0%) respondents were more depressed than those with above average year of schooling 45 (26.5%). This is statistically significant (p-value = 0.03). Negative life events were associated with depression. Nine (29.1%) males and 45 (32.3%) female's respondents had more than three negative life events. This was of statistical importance (p-value = .004).
| Indicator | Levels of Depression | |||
|---|---|---|---|---|
| Low Depression | Mild Depression | High Depression | p-value | |
| Economic Status | 0.64 | |||
| Good | 20 (11.7) | 15 (8.8) | 22 (12.9) | |
| Average | 62 (36.5) | 56 (33.0) | 44 (25.9) | |
| Poor | 88 (51.8) | 99 (58.2) | 104 (61.2) | |
| Total | 170 (100) | 170 (100) | 170 (100) | |
| Years of Schooling | 0.03 | |||
| Below average | 80 (47.0) | 55 (32.4) | 73 (42.9) | |
| Average | 45 (26.5) | 72 (42.4) | 60 (35.3) | |
| Above average | 45 (26.5) | 43 (25.2) | 37 (21.8) | |
| Total | 170 (100) | 170 (100) | 170 (100) | |
Figure 1, shows that 130 (43.3%) of the respon-dents were not depressed; 170 (56.7%) satisfied the criteria for a depressive disorder using the PHQ-9. Among the respondents, 109 (36.3%) had minimal depression, while 4 (13%) were severely depressed.
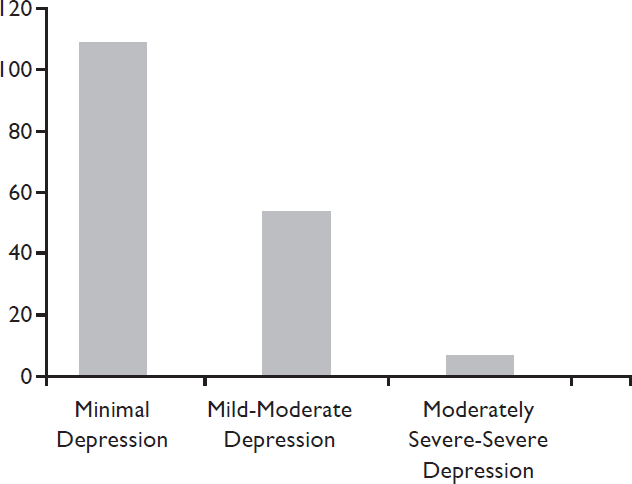
- Levels of Depression among Respon-dents, Using the Patients Health Questionnaires (PHQ-9) Scale
Discussion
The prevalence of depressive disorders among HIV/ AIDS patients attending the HAART, at the Kwara State Specialist Hospital Sobi, was 56.7%. Our finding was similar to the previous studies. It also falls within the prevalence rates seen internationally.[14] It also agrees with most local studies.
The socio demographic factors of age, gender, marital status, education, and income have consis-tently been identified as important factors in ex-plaining the variability in the prevalence of depression. Key North American studies, particularly the Epidemiologic Catchment Area Study, the National Co-morbidity Survey, the Canadian Health Population Health Survey pointed out this fact. Similarly, economic status or variables related to income or financial status were reported to be significant in Hong Kong[15] and Beijing.[16] O'Sullivan[17] while stud-ying the psychosocial determinants of depression found social factors as a risk factor for depression.
Similar to other findings, there was female pre-ponderance in prevalence of depressive disorders.[18] Prevalence of depression had been found to vary considerably based on gender.[19] Women (68.7%) reported significant higher prevalence of depression than men (32.3%) in a study in Russia.[20] The above findings are in consonant to our study.[21] On the contrary, a South-African study[22] found that the prevalence rate of depressive symptomatology to be almost equal in both sexes. The result of our study negates one previous finding that, in Africa, there are higher rates of depression among men than women in psychiatric institution.[23] Marital status had been found to interact with gender in accounting for variance in the prevalence rate of depression. In Australia,[24] for example, those who were separated or divorced PLWAs had a higher rate of depression. Similarly, another South-African Stress and Health Study (SASH),[25] found that mood disorders were more frequent among separated, widowed and divorced individuals and among people with only an elementary school level of education. This is similar to our findings. Women are more likely to experience negative social determinants than men because they carry the double burden of raising children and household work. Gender inequity in the spousal relationship, was related to depressive mood, hence there is need to pay more attention to gender relations in future research on social determinants of depressive mood.
Fifty (29.4%) respondents were in the 36 -40 age range. Previous research had found that age was one of the demographic characteristics that accounted for much of the variance in the prevalence of depression. In a study in Nigeria,[26] there was no significant association between depression and age. Similarly in Bongongo study,[27] no relationship was found between age and depressive features among patients receiving HAART. One study reported that depression could occur at any age, and that individuals, may experience depression at different times of their lives for different reasons.[28] There were no significant differences between age group and depression. This was similar to the finding of Bongongo and colleagues[27] in South-Africa, where age group was not significant.
Among the depressed respondents, the edu-cational level was less than secondary school level in 55 (32.4%), while the lowest depression prevalence rate was found among respondents with tertiary education 17 (10.0%). This contrasts with the findings in Canada, where respondents, whose educational level were less than secondary education, had the lowest rate of depression and the highest prevalence rate of depression (13.4%), was seen among those with tertiary education. Education is a critical social determinant of health because, people with higher levels of education are often healthier than people with lower levels of educational attainment. There are three main reasons why education is important as a social determinant. Firstly, education leads to better health outcome because one's level of education is highly correlated with other social determinants such as level of income, employment, security, and working conditions. Education enhan-ces one's socio-economic condition by creating opportunities for advancement in the workforce. Secondly, education protects people from the instability of the current job market by increasing their ability to access new training opportunities and career. Thirdly, education increases one's ability to monitor their unhealthy living and eating habits, and creates alternative lifestyles that are more beneficial to their health status in the long-run, it is important that governments ensure that the public education system, and particularly post-secondary institutions are relatively affordable and accessible to the entire population -not just the privileged class.
| Social Cohesion | |||||
|---|---|---|---|---|---|
| Low 0 - 2 | Fair 3 - 5 | High 6 - 9 | Total (%) | P-value | |
| Depressed Male | 21 (67.7) | 8 (25.9) | 2 (6.5) | 31 (100) | 0.05 |
| Depressed Female | 112 (80.6) | 27 (19.4) | 0 (0.0) | 139 (100) | |
About 25 (8.3%) were unemployed. Unemploy-ment leads to poor physical mental health in a number of ways. When patients become unemployed, it is a stressful event that affects their self-esteems. Since employment generates income, a positive identity and the ability to live healthy lifestyles, unemployment leads to impoverishment, psychological stress and participate in health-threatening coping behaviors such as tobacco consumption, alcohol abuse, pro-miscuity. This is similar to another study, where depressive features were more common among the unemployed. Depression resulting from unem-ployment has increased over the years.[28] Six (2.0%) were students. The implication of this age group is that, youth, the future of Nigeria, should be targeted for HIV interventions. Unemployment is also responsible for mental health problems such as depression.
The highest prevalence rate of depression 129 (75.9%) was seen in patients with an income level of less than twenty thousand Naira (N20,000), which is the minimum recommended income by the Federal Government of Nigeria. This is similar to the findings in the province of Ontario, in Canadian Health Survey, where the highest prevalence of depression (18.4%), was seen in household, with an income level of less than $10,000 per year.[11] Income is the most significant social determinants of health, because it determines one's overall living conditions, affect one's psychological condition, and help shape one's diet and eating habits. Low-income people living in poverty, cannot afford healthy food, sufficient clothing and good housing all of which are necessary preconditions of good health.
Social cohesion occurs when specific marginalized groups are not able to participate in their identity and social location. Social cohesion is based on four differences viz: denial of participation in civil affairs, denial of social funds, exclusion for social production and economic exclusion. In this study, Social Cohesion was very low in both males and females, 2l (67.7%) and 112 (80.6%) respectively among the depressed HIV patients. Only 2 (6.5%) males had high social cohesion. This is statistically significant (p -value = 0.005). Deprivation causes social exclusion when people are unable to participate in cultural, educational and recreational activities due to their poor social-economic conditions. In the long term social exclusion, negatively impacts on one's physical and mental health. Income inequality is a key public health issue that must be addressed by governments and policy makers by increasing minimum wage and social assistance levels.
Social support and good social relationship makes an important contribution to health and prevent the depression. Social support also helps to give people the emotional and practical resources they need.
Belonging to a social network of communication and mutual obligatory makes people feel cared for, loved, esteemed and valued. This has a powerful protective effect on health. Therefore, good social relationship can reduce depression. On the other hand, low social support causes more stress and can accelerate or worsen the progression from HIV to AIDS.29
Limitations
The relatively small sample may be a potential limitation. Self-reported measures to assess econo-mic status and depressive symptoms were used. These were prone to participant response bias, such as low reported symptoms due to stigma. Moreover, like all cross-sectional studies, it is difficult to establish causal association between independent and dependent variables. Furthermore, a cultural measure was lacking in this study.
Conclusion and Global Health Implications
The social determinants of depression are social, economic and health condition people are born into and live. Poor social and economic circumstances affect health throughout life.[9] Some socio-economic conditions refer to the relationship between income level and educational attainment. Socio-economic variations among the studied patients are strongly and positively associated with depression. The recognition that the disempowerment of women is in part responsible for the increased rate of depre-ssion call for more focus in gendered social deter-minant of depression. Unemployment puts health at risk and the risk is higher in patients with depression. Poverty, relative deprivation and social exclusion have a major impact on depression. This study calls for improved public health education and awareness, to highlighting the health impact of depressive symptoms and the role of social determinants of depression on the sample of HIV/AIDS patient in Nigeria. It also provides initial evidence on the importance of SDH in depression. Social inequity should be given high priorities when addressing the issue of depression.
Conflict of interest:
None Declared
References
- Depression is a risk factor for suboptimal adherence to highly active antiretroviral therapy. Journal Acquired Immune Deficiency Syndrome. 2002;31(3):136-39.
- [CrossRef] [PubMed] [Google Scholar]
- Diagnostic and Statistical Manual of Mental Disorders DSM-IV-TR. Arlington, VA: American Psychi-atric Publishing; 2000.
- [Google Scholar]
- Life stress, social support and clinical depression; a reanalysis of the literature. Social Science and Medicine. 1993;37:331-342.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison of social status determinants of depressive symptoms among elderly Chinese in Guangzhou, Hong King, Asian Journal. Gerontology Geriatric. 2009;4:58-65.
- [Google Scholar]
- Psychiatric disorders in America: The Epidemiologic Catchment Area Study New York: The Free Press. 1991
- [Google Scholar]
- One year prevalence of psychiatric disorder in Ontarians 15 to 64 years of age. Canadian Journal of Psychiatry. 1996;41:559-563.
- [CrossRef] [PubMed] [Google Scholar]
- Socio economical inequ-alities in depression: A meta- analysis. American Journal of Epidemiology. 2003;157:98-112.
- [CrossRef] [PubMed] [Google Scholar]
- Data collection in: Research Methodology with Statistics for Health and Social Sciences. Nathadex publishers, Ilorin. 2003;130:159.
- [Google Scholar]
- Pre-valence of depression and role of support group in its management: A study of Adult HIV/AIDS patients attending HIV/AIDS Clinic in a tertiary health facility in South-eastern Nigeria; Journal of Public Health and Epide-miology. . 2011;3(4):182-86.
- [Google Scholar]
- Closing the gap in a generation: health equity through action of on the social determinants of health (2008) Available: http://www.searo.who.int/LinkFiles/SDH_SDH_FinalReport.pdf (accessed )
- [Google Scholar]
- Risk factors for suicide in China: a national case-control psychological autopsy study. Lancet. 2002;360:1728-36.
- [CrossRef] [PubMed] [Google Scholar]
- Minorities, the poor and survivors of abuse: HIV-infected patients in the US. Deep South. South Medical. Journal. 2007;100:1114-1122.
- [CrossRef] [PubMed] [Google Scholar]
- Family and cultural correlates of depression among Chinese elderly. Inter-national Journal of social Psychiatry. 1999;43:199-212.
- [CrossRef] [PubMed] [Google Scholar]
- The psychosocial determinants of depression: a lifespan perspective. Journal of Nervous and Mental Disorder. 2004;192(9):585-94.
- [CrossRef] [PubMed] [Google Scholar]
- Gender differences in depression. The British Journal of Psychiatry,. 2000;177:486-492.
- [CrossRef] [PubMed] [Google Scholar]
- Emergence of gender differences in depression during adolescence: National panel results from three countries. Journal of America. Academy. Child Adolescence. Psychiatry. 2002;41:190-198.
- [CrossRef] [PubMed] [Google Scholar]
- Social and lifestyle determinants of depression, anxiety, sleeping disorders and self-evaluated quality of life in Russia population based study in Arkhangelsk. Social Psychiatry and Psychiatric Epidemiology. 2005;40(7):511-8.
- [CrossRef] [PubMed] [Google Scholar]
- Socio-demo-graphic characteristics of depressive illness among Nigerians. Acta Psychiatry Scand-inavian. 1986;73(2):128-132.
- [CrossRef] [PubMed] [Google Scholar]
- Treating depression in HIV/AIDS. South-African Journal of Psychiatry. 2007;13(3):86-88.
- [CrossRef] [Google Scholar]
- Depression and gender. An international review. American Psychologist. 1997;52(1):25-31.
- [CrossRef] [PubMed] [Google Scholar]
- the South- African Stress and Health (SASH) study: 12-month and lifetime prevalence of common mental disorders. South African Medical Journal. 2009;99(5):339-44.
- [Google Scholar]
- Depression among medical outpatients with diabetes: A cross-sectional study at Jos University Teaching Hospital, Jos, Nigeria. Annnal Medical. 2010;9(1):5-10.
- [CrossRef] [PubMed] [Google Scholar]
- Depressive features among adult patients receiving antiretroviral therapy for HIV in Rustenburg district, South-Africa.
- [Google Scholar]
- President and Fellows of Harvard College. Depression, sex and age. Cambridge, MA: Harvard Health Publications; 2007. p. :1-5.
- [Google Scholar]
- Relationship of lifetime trauma and depressive symptoms to mortality in HIV. America Journal of Psychiatry. 2007;164(11):1707-13.
- [CrossRef] [PubMed] [Google Scholar]





