Translate this page into:
Determinants of Home Delivery among Women Aged 15-24 Years in Tanzania
✉Corresponding author email: kimarioflorence@gmail.com
-
Received: ,
Accepted: ,
Abstract
Background:
The United Nation's Sustainable Development Goal number 3 aims at reducing the maternal mortality rate by less than 70/100,000 live births globally and 216/100,000 live births in developing regions by 2030. Despite several interventions in Tanzania, maternal mortality has increased from 454/100,000 live births in 2010 to 556/100,000 live births in 2015. Home delivery and maternal young age contribute to maternal deaths. Reducing home deliveries among women aged 15-24 years may likely decrease the prevalence of maternal deaths in Tanzania. This study investigated the determinants of home delivery among women aged 15- 24 years in rural and mainland districts of Tanzania.
Methods:
This study uses a mixed-methods approach using data collected as part of the evaluation of government and UNICEF interventions in 13 districts of Tanzania mainland from October and November 2011. Results from the secondary analysis were supplemented by qualitative data collected between February and April 2019 from four rural districts: Bagamoyo, Tandahimba, Magu, and Moshi.
Results:
A total of 409 adolescents and young women who delivered one year before the quantitative data collection were included in the final analysis. A quarter of them gave birth at home. Having at least four antenatal care (ANC) visits (OR=0.23, 95% CI: 0.12-0.41, p<0.01), planning place of delivery (OR=0.22, 95%CI: 0.14-0.36 p<0.01), and knowledge of the danger signs during pregnancy (OR=0.36, 95% CI: 0.22-0.57, p<0.01) were significantly associated with the place of delivery.
Conclusion and Global Health Implications:
Maternal level of education, number of ANC visits attended, planned place of delivery, and knowledge of danger signs during pregnancy were the determinants of the choice of place of delivery among women aged 15-24 years in Tanzania. Understanding these risk factors is important in designing programs and interventions to reduce maternal deaths from women of this age group which contributes about 18% of all maternal deaths in Tanzania.
Keywords
Adolescents
Young women
Home delivery
Tanzania
Sub-Saharan Africa
1. Introduction
Home delivery refers to a natural process of giving birth at home alone or with the assistance of a close relative or traditional birth attendant. During home delivery, there are a lot of unexpected health complications, including maternal severe bleeding, severe lacerations, sepsis which may result in the death of the mother and newborn.1 Delays in obtaining adequate medical and/or obstetric emergency care are one of the leading causes of maternal deaths in the world. Mbaruku et al.2 described delays in making decisions to seek care, arrival at a health facility or obtaining adequate care as among the most common types of risks for maternal death.2 Studies recommend health facility delivery and strengthened referral pathways as effective strategies for reducing maternal deaths in low-income countries.3,10
Sub Saharan Africa has an annual maternal mortality rate of 920/100,000 live births, the highest compared to other parts of world.4 Within Africa, Sierra Leone has the highest maternal mortality (1,360 deaths per 100,000 live births)5 and more than half of home deliveries, despite laws prohibiting pregnant women from home delivery in the country.6 Uganda, one of the East African countries, has shown remarkable achievements in reducing the maternal mortality rate from 438 deaths per 100,000 live births in 2011 to 336 deaths per 100,000 live births in 2013.7 The proportions of women who delivered at health facilities in Uganda increased from 42% in 2006 to 57% in 2011 and stands at 74% in 20I6.8
The maternal mortality rate in Tanzania has remained high and stands at 556 per 100,000 live births.9 Current data show that more than half of all births occur in health facilities and are assisted by skilled attendants.9 There is a scarcity of data in Tanzania that explain the determinants of home delivery among adolescent mothers. Studies have identified some of the risk factors for home delivery (age, education, socio-economic status) in the general population.10,16 Similarly, Gyesaw et al.11 identified age, social-economic status, education, and low knowledge on maternal health as risk factors for home deliveries among adolescent mothers.11 This study was aimed at investigating the determinants of home delivery among adolescents and young mothers living in the 13 districts of Tanzania mainland.
2. Methods
2.1. Study Variables
This study comprises of a parent and follow-up study. The study's independent variables were important demographic characteristics such as maternal age, education, utilization of antenatal care (ANC) services that were explored with the outcome variables. The dependent variable was home delivery, a binary variable representing whether or not adolescents or young mothers delivered at home.
2.2. Description and Methodology for Parent Study
We analysed data from study entitled “Evaluation of Government of Tanzania and UNICEF interventions in seven learning districts” conducted between November and October 2011. The study was designed to assess the effectiveness of the area- based programming approach, the “theoretical model” of the 7 Learning Districts, (LDs) and draw lessons learned for future programming internally and in other countries. Interventions that were evaluated were training on maternal, neonatal, and child health (MNCH), Prevention of Mother to Child Transmission (PMTCT), and acute malnutrition among health care providers, mothers, and caregivers. Other interventions were provisions of supplies and equipment needed for vaccination activities and service deliveries, supplementation of vitamin A to children of 6-59 months and water, and sanitation and hygiene (WASH) constructions.
Study design and setting:
This was a cross-sectional which employed quantitative and qualitative research methods. The study was conducted in 7 learning Districts (LDs) which were Bagamoyo, Temeke, Hai, Siha, Magu, Makete and Mtwara rural, as compared to 6 non-learning districts (NLDS) which were- Mkuranga, Kinondoni, Moshi rural, Misungwi, Njombe, and Tandahimba. Before the selection of comparison districts, matching of districts was done based on the availability of health care services and population levels to ensure any differences at the end of the project were attributed to the intervention.
Data collection technique and tools:
Data collection tools were a mix of structured questionnaires that were administered to households and at health facilities. The survey team visited sampled households and interviewed caregivers or parents of children under the age of five, women who delivered in the previous year and youth (15-24 years). Complementary data were obtained from reports which were available in the study districts and relevant ministries and institutions. Household survey captured socio-demographic characteristics, maternal health, utilization of ANC and postnatal services, place of delivery, hand wash hygiene, and storage of drinking water.
Inclusion and exclusion criteria:
The inclusion criteria were: households living within 400 meters of a drinking water source in the dry season, households with young people aged 15-24 years, households that have children 0-59 months sleeping under bed nets and households that have breastfeeding women. In each sampled household, the head of household, all women with children aged 0-59 months, and all breastfeeding women were selected for the survey.
Sample size estimation and sampling technique:
The sample size of the household survey was calculated to detect 10% difference in the primary outcome (ownership of drinking water source, use of bed nets, children 0-59 months for nutrition intervention, and the presence of breastfeeding women who gave birth one year before the survey) post-intervention. Using 80% statistical power and a 95% confidence level, a minimum of 364 households were determined to be required per district. This amounted to a total of 4,368 households in both control and intervention sites.
2.3. Description and Methodology for Follow-up Study
Using data collected from the parent project, the follow-up study aimed to investigate the determinants of home delivery among women aged 15-24 years living in 13 districts of Tanzania mainland. Specifically, the study: (1) examined the prevalence of home delivery among women aged 15-24 years in Tanzania mainland; and (2) identified the risk factors for home delivery among women aged 15-24 years in Tanzania mainland. Besides, qualitative primary data were collected to supplement objective two above in Magu, Bagamoyo, Moshi rural, and Tandahimba districts.
Study design and settings:
This was a cross-sectional study design using both quantitative and qualitative approaches. For quantitative secondary data, we used secondary data from the parent project which were retrieved from the Ifakara Health Institute (IHI) database. For qualitative data collection, four districts were selected, two from the learning districts, namely, Magu and Bagamoyo districts and other two from the non-learning districts, namely, Tandahimba and Moshi rural districts. Magu is one of the districts in the Mwanza region with an area of 1,500 square kilometers, and a population of 229,759 where female make up 51.1% of the total population17 and 49 health facilities that serve approximately 4,689 population per health facility. Bagamoyo, one of the districts in the coastal Tanzania, with a population of 331,740 people and among them, 50.5% are female; it covers an area of 8463 square kilometers.17 The area has 25 health facilities that serve approximately 13,270 people per health facility. Tandahimba district is in the Mtwara region. This region has an area of 2,049 square kilometers with a total population of 227,514 and among them females are 53.7%.17 The district has 35 health facilities that serve approximately 6501 people per health facility. Moshi rural is one of the 7 districts in the Kilimanjaro region. The district has a total of 31 administrative wards, populated with 446,737 people, and among them 51.6% are females.17 The district has 89 health facilities that serve approximately 5,020 population per health facility. Ifakara Health Institute (IHI) is a leading health research organization in Africa, with a strong track record of developing, testing and validating, innovation for health. The IHI is driven by core strategic mandate for research, training and services. The institute's work spans across the full research lifecycle from basic science to policy and translation.18
Sample size and sampling approach:
In the quantitative part of the study, a dataset of adolescents below 20 years was meant to be used. However, the sample size was insufficient which led to the addition of another subset of data on young women aged 20-24 years (113 adolescents and 296 young women). In-depth interviews were conducted during qualitative work to explore healthcare workers' experiences and roles in maternal health care. Districts Reproductive and Child Health Coordinators (DRCHCo), nurses working within the Reproductive and Child Health (RCH) unit and Nurses in- charge of labor ward from the eight facilities (four district hospitals and four dispensaries/ health centers) were interviewed. Besides, eight traditional birth attendants (TBA) were interviewed from the four qualitative study districts. Health care providers were purposively sampled and a snowball technique was used for recruitment of TBAs with the help of DRCHCo.
Data collection technique and tools:
This study extracted quantitative data from the parent project on maternal health, place of delivery, utilization of ANC and postnatal services as well as socio-demographic characteristics with a focus on adolescents and young women who gave birth one year before the parent project data collection. In-depth interviews were conducted with key informants within the selected districts to supplements the quantitative data. An interview guide translated in Swahili was used to conduct in-depth interviews with key informants during this qualitative component of the study. Health care providers were interviewed at health facilities while TBAs were interviewed at their homes. The interview guide captured socio-demographic, ANC and delivery profiles. For the TBAs it captured perception and reasons for home deliveries among women aged 15-24 years.
Data management and statistical methods:
In this study, quantitative data collected from the household survey were retrieved from IHI server. A total of 21,688 members were identified in the surveyed households of which only 2,019 were female of reproductive age of which 1,791 were interviewed. Out of the women interviewed, only 453 were eligible for this analysis (aged between 15-24 years). Furthermore and extra 44 women were dropped during the analysis because they had missing information on the utilization of ANC and delivery characteristics. The final analysis was conducted for 409 (113 adolescents and 296 young mothers) who gave birth one year before data collection. Thus by definition, adolescents in this study were aged below 20 years, however, the cut-off age was extended to 24 years to increase the sample size to enable the generation of meaningful conclusions.
Statistical analysis was performed using Stata version 13 with all p-values at or below p<0.05 considered as statistically significant. Maternal characteristics, age, education, utilization of ANC services were compared across the reported place of birth of adolescent mothers. Descriptive analysis and univariate logistic regression were performed with a place of delivery, coded as “1” if the women deliver at home and “0” otherwise as an outcome variable. Predictor variables explored include maternal age, education, utilization of ANC and postnatal services.
Qualitative data analysis was done using thematic analysis framework involving six main steps namely, familiarization of the data, generating initial codes, searching for themes, defining and naming themes and producing the report.
3. Results
3.1. Social Demographic Characteristics of Women Interviewed
A total of 409 adolescent mothers and young women, 17 health care providers and 8 active TBAs were included in the analysis. Nearly three quarters (296) or 72.5% of interviewed mothers were aged between 20-24 years, while 27.5% (113) were aged below 19 years. Eight out of the 10 mothers interviewed had primary education while 17.4 % had secondary or higher levels of education.
3.2. Antenatal Care (ANC) Utilization
Women who gave birth in the two years preceding the survey were asked if they obtained antenatal care during the pregnancy for their most recent live birth. Of 409 women, 83.4% (340) attended at least one ANC visit and 50.3% attended four or more visits. Out of 340 women who attended at least one visit, 36.5% (125) started ANC visit during the first trimester as recommended by the World Health Organization (WHO) (Figure 1).
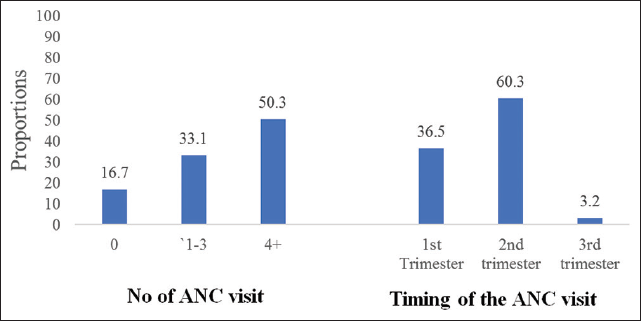
- ANC attendance among women aged 15-24 years in Tanzania
3.3. Stigma and Barriers to ANC Utilization
Results from key informant interviews described personal, facility and policy barriers to utilization of ANC, delivery and post-natal care services among adolescent mothers. Adolescent mothers had a tendency of stigmatizing themselves when not married and were often shy to attend ANC services. They often delayed reporting labor pain and poor postnatal attendances particularly when they have no support from their partner as highlighted in the statement below: “............. Stigma from family members, the one who impregnated and abandoned the girl. She cannot make decisions of when to start the clinic and where to go for delivery.” (In-depth interview with a Nurse, Moshi).
“If she is not married, she will feel shy to attend ANC and PNC. Often they are afraid to be named an adulterer or prostitute” (In-depth interview with a Nurse - Magu).
“............ These girls do not feel good when a health care provider asks them about their pregnancy” (In-depth interview with a Nurse, Bagamoyo).
The policy of asking pregnant adolescents to bring the partners in each ANC visit was reported as another barrier to the use of ANC services. Some of the adolescents were students and others have been married but with old men who refuse to escort them to the clinic. This resulted in delays starting ANC services or not attending at all.
“This issue of asking all women to start ANC with the escort of their partners is hard in our place; most girls are not married, so this policy should go with punishment to the household which doesn't implement it on time”. (In-depth interview with a nurse, Kahe-Moshi).
Furthermore, negative attitudes of health care providers towards adolescents came up so obviously resulting in some pregnant women refusing ANC services or visiting distant facilities.
“We usually receive client from extremely far areas, when you ask them why they don't go to the nearby facility..., they often say that providers of their nearby facility are not friendly. We need to change our attitudes because education about the importance of facility delivery will not help if we still use abusive languages to our clients' especially young girls.” (In-depth interview with a nurse, Magu).
3.4. Place of Delivery
Access to proper medical care and hygienic conditions during delivery reduces the risk of complications and infections for the mother and the baby. Overall, 24.1% (98) of adolescent women gave birth at home. When stratified by age group, 20.4% of those below 19 years gave birth at home, while 25.3% of those aged 20-24 years delivered at home. Among all 409 women interviewed, 63.9% planned for a place of delivery. Out of all women who had a plan for a place of delivery (260), 96.2% (250) planned to give birth at health facilities, and among those who planned to give birth in health facility only 88.4% (221) managed to do so; out of 10 women who planned to give birth at home, 70% (7) managed to do so (Table 1). Qualitative data also showed that privacy within the labor ward was another issue that came up as obvious as a reason for mothers choosing home delivery:
“.... the environment of delivery rooms are not good and several people delivered in the same ward, some of them don't want people to see their private parts..” (In-depth interview with a Nurse, Bagamoyo).
| Variable | N | % |
|---|---|---|
| Planned for her delivery | ||
| Yes | 260 | 63.9 |
| Planned place of delivery | ||
| Health facility | 250 | 96.2 |
| Home | 10 | 3.85 |
| The actual place of delivery | ||
| Health facility delivery | 221 | 88.40 |
| Home delivery | 7 | 70.00 |
| Who helped during delivery | ||
| Health care provider | 297 | 73.0 |
| Traditional birth attendant | 60 | 14.7 |
| Relative | 50 | 12.3 |
ITwo women had missing values for place
3.5. Determinants of Home Delivery
Bivariate analyses indicated that women who attained secondary education or higher were less likely to give birth at home when compared to those with primary education (OR=0.75; 95% CI: 0.42-1.34, p=0.336). The number of ANC visits, planning place of delivery, and knowledge of the danger signs during pregnancy were significantly associated with place of delivery. Individuals with four or more ANC visits were 0.23 times less likely to give birth at home when compared to those who never attended any ANC visit (Table 2).
| Predictor Variable | N | n | % | OR (95% CI) | P-value |
|---|---|---|---|---|---|
| Education | |||||
| Primary education | 337 | 78 | 23.2 | 1 | |
| Secondary education | 70 | 20 | 28.6 | 1.33 (0.75-2.37) | 0.335 |
| Number of ANC visits | |||||
| 0 | 67 | 32 | 47.8 | 1 | |
| 1-3 | 135 | 31 | 23.0 | 0.32 (0.17-0.61) | <0.01 |
| 4+ | 205 | 35 | 17.1 | 0.23 (0.12-0.41) | <0.01 |
| Gestational age at first ANC visit | |||||
| First trimester | 124 | 21 | 16.9 | 1 | |
| Second trimester | 205 | 43 | 21.0 | 1.30 (0.73-2.32) | 0.375 |
| Third trimester | 11 | 2 | 18.2 | 1.01 (0.22-5.41) | 0.916 |
| Planned for a place of delivery | |||||
| No | 147 | 62 | 42.2 | 1 | |
| Yes | 260 | 36 | 13.9 | 0.22 (0.14-0.36) | <0.01 |
| Informed about danger signs | |||||
| No | 164 | 58 | 35.4 | 1 | |
| Yes | 243 | 40 | 16.5 | 0.36 (0.22-0.57) | <0.01 |
3.6. Traditional Birth Attendants' Opinions on Home Delivery
Traditional birth attendants who were interviewed reported that they supported home deliveries only on an emergency basis because the government has banned TBA practices. They provided some reasons why some women prefer home deliveries in the past, pointing to poverty as the main reason. Likewise, in the community, women who delivered at home were regarded as strong.
Other reasons mentioned were poor transportation especially during the rainy seasons and trust attached to the TBA. The following statement supports the above fact:
“Poverty (she does not have money for facility delivery) [makes you to] find a pregnant mother who went to ANC and advised to deliver at a big hospital, but she will keep quiet and wait for labor Pain, then comes to me ask for assistance, when I look at the card it shows that she was supposed to give birth at a big hospital.” (In-depth interview with TBA Number 1, Moshi).
“....In our community, it is perceived that a woman who gives birth at home is brave.” (In-depth interview with TBA, Number 1, Magu).
4. Discussion
This study aimed to determine factors associated with home delivery among women aged 15-24 years from 13 districts of Tanzania mainland. The majority of the respondents were young women aged 20-24 years. Overall, a third of participants gave birth at home, which is in line with the 2015/2016 Tanzania Demographic Health Survey (DHS) which reported that 33% of adolescents and 37% of women give birth at home.12 Results from this study suggested that maternal age was associated with home deliveries with more matured women more likely to give birth at home. This is similar to the results of a study in Kenya which showed that older women had higher probabilities of home delivery compared to young mothers.14 However, another study conducted in rural Tanzania showed younger women were more likely to give birth at home.13
This study also found that maternal education was associated with home delivery. A woman's higher level of education was associated with reduced probabilities of home delivery. Moindi and his colleagues in Kenya also found very similar results.14 The number of ANC visits was strongly associated with a place of delivery with women having four or more ANC visits being less likely to give birth at home compared to women who had never attended ANC clinics. These results were in line with those of Konadu which showed that the number of ANC visits were strong indicators of a choice of place of delivery, whereby women who attended one to three ANC visits had higher odds of giving birth at home compared to those who had four or more visits.11 Furthermore, a study conducted in Northern Ethiopia showed a strong association between the number of ANC visits, plan for a place of delivery, and knowledge of the pregnancy danger signs and place of delivery.12
Data from our in-depth interview showed that personal challenges and lack of support from partners were some of the reasons for poor ANC uptakes and home delivery which were in line with the results of the study by Gross and colleagues.15 Poor infrastructure and privacy within the facility settings had also been reported as barriers to health facility delivery.15 Pfeiffer and colleagues reported the same findings showing that lack of privacy in the health facility as a discouraging factor for facility-based delivery.13 Moreover, in Tanzania, TBAs had stopped assisting women during home delivery and now encouraging them to go to the health facilities well in advance, which was similar to the findings by Pfeiffer and Rosemarie.13 This study suggests that the exploration of the effectiveness of community education on improving maternal healthcare should be done to address some of the community norms, infrastructures, and privacy in facility settings.
Limitations
This study has several limitations. The major limitation was our inability to conduct in-depth interviews with adolescents and young mothers because of political reasons, whereby the government was against adolescent (school girls) pregnancies. It was hard and time-consuming to try locating these girls for the study interview.
Recommendations
Since the needs of women aged 15-24 years differ in many ways, the government of Tanzania should consider tackling the health system challenges faced by these women by increasing health care providers with appropriate knowledge of how to deliver youth-friendly reproductive services in the facilities, reconstructing labor wards to provide privacy, and retraining health care providers on how to deal with young mothers. Furthermore, young women should be assisted with proper maternal health education in primary and secondary schools as well as in the community. Health information given to the community should contain information advising male partners to attend ANC so that they can get advice to assist their partners. Future studies should interview adolescents and young women who are pregnant and those who had delivered to share their experiences during pregnancy including their utilization of ANC and delivery.
5. Conclusion and global health implications
This study identified maternal level of education, several ANC visits, planned place of delivery, and knowledge about pregnancy danger signs as predictors of a place of delivery. Furthermore, lack of maternal education, negative emotions towards ANC attendance by young mothers, partners' support, and healthcare providers' attitudes towards early pregnant women were some of the factors predicting poor uptake of ANC services and home delivery among young women. It is important to consider these factors in the programming of interventions to reduce maternal deaths and removing barriers for accessing quality maternal health care both at the health system and societal levels.
Compliance with Ethical Standards
Funding Statement:
This research and publication of the article were funded by the African Development Bank project as part of the first author's scholarship at Nelson Mandela African Institute of Science and Technology (AfDB grant number 2100155032816).
Ethical Consideration:
The parent study was approved by the ethical committee of the Ifakara Health Institute and the National Institute for Medical Research (NIMRI) with clearance number IHIlIRBINo 14-2011. The follow-up study was approved by the Ifakara Health Institute review board (IHIlIRBINo: 10-2019). The study team paid a courtesy visit to the district administration before data collection. Individual written informed consent was obtained from each participant during fieldwork and confidentiality of all study participants was observed.
Acknowledgment:
The first author expresses her sincere appreciation to Dr. Mkopi of the Ifakara Health Institute (IHI) for his assistance during data analysis. My special thanks also go to Professor Olola Oneko and Professor Sia Msuya of Kilimanjaro Christian Medical University College (KCMUCo) for their thoughtful comments, inputs and technical advice.
Conflicts of Interest:
The authors declare that there is no conflict of interest regarding the publication of this paper.
References
- Birth Preparedness and Complication Readiness (BPCR) Among Pregnant Women in Hard-To-Reach Areas in Bangladesh. PLoS ONE. 2017;12(12):1-19.
- [CrossRef] [PubMed] [Google Scholar]
- Perinatal audit using the 3-delays model in western Tanzania. International. Journal of Gynecology and Obstetrics. 2009;106(1):85-88.
- [CrossRef] [PubMed] [Google Scholar]
- Household decision-making about delivery in health facilities: evidence from Tanzania. Journal of Health, Population and Nutrition. 2009;27(5):696-703.
- [CrossRef] [PubMed] [Google Scholar]
- Use pattern of maternal health services and determinants of skilled care during delivery in Southern Tanzania: implications for achievement of MDG-5 targets. BMC Pregnancy Childbirth 2007:1-7.
- [CrossRef] [PubMed] [Google Scholar]
- Evidence to inform the future for maternal and newborn health. Best Practice & Research Clinical Obstetrics & Gynaecology. 2016;36:169-183.
- [CrossRef] [PubMed] [Google Scholar]
- Community-based birth waiting for homes in Northern Sierra Leone: Factors influencing women's use. Midwifery. 2016;39:49-56.
- [CrossRef] [PubMed] [Google Scholar]
- Rapid reduction of maternal mortality in Uganda and Zambia through the saving mothers, giving life initiative: results of year I evaluation. BMC Pregnancy Childbirth. 2017;17(1):42.
- [CrossRef] [PubMed] [Google Scholar]
- 2018. Uganda Demographic and Health Survey 2016. Kampala, Uganda and Rockville, Maryland, USA: UBOS and ICF. (accessed )
- [Google Scholar]
- Ministry of Health, Community Development, Gender, Elderly and Children (MoHCDGEC) [Tanzania Mainland], Ministry of Health (MoH) [Zanzibar], National Bureau of Statistics (NBS), Office of the Chief Government Statistician (OCGS), and ICF. 2016. Tanzania Demographic and Health Survey and Malaria Indicator Survey (TDHS- MIS) 2015-16. Dar es Salaam, Tanzania, and Rockville, Maryland, USA: MoHCDGEC, MoH, NBS, OCGS, and ICF (accessed )
- [Google Scholar]
- Factors affecting home delivery in rural Tanzania. Tropical Medicine and International Health. 2007;12(7):862-872.
- [CrossRef] [PubMed] [Google Scholar]
- Experiences of pregnancy and motherhood among teenage mothers in a suburb of Accra, Ghana: a qualitative study. International Journal of Women's Health. 2013;5:773-780.
- [CrossRef] [PubMed] [Google Scholar]
- Determinant factors of home delivery among women in Northern Ethiopia: A case-control study. BMC Public Health. 2017;17(1):289.
- [CrossRef] [PubMed] [Google Scholar]
- Delivering at home or in a health facility? Health-seeking behavior of women and the role of traditional birth attendants in Tanzania. BMC Pregnancy Childbirth. 2013;13:55.
- [CrossRef] [PubMed] [Google Scholar]
- Why mothers still deliver at home: understanding factors associated with home deliveries and cultural practices in rural coastal Kenya; A cross-section study. BMC Public Health. 2016;16(1):1-8.
- [CrossRef] [PubMed] [Google Scholar]
- Timing of antenatal care for adolescent and adult pregnant women in south-eastern Tanzania. BMC Pregnancy Childbirth 2012
- [CrossRef] [PubMed] [Google Scholar]
- Impact of Place of Delivery on Neonatal Mortality in Rural Tanzania. International Journal of Maternal and Child Health and AIDS. 2012;1(1):49-59.
- [CrossRef] [PubMed] [Google Scholar]
- (accessed )
- About Us. https://ihi.or.tz (accessed )





