Translate this page into:
Exclusive Breastfeeding and Under-Five Mortality, 2006-2014: A Cross-National Analysis of 57 Low- and-Middle Income Countries
✉Corresponding author email: reazuine@globalhealthprojects.org
Abstract
Background:
Few studies have examined the long-term, cross-national, and population-level impacts of exclusive breastfeeding on major global child health indicators. We investigated the overall and independent associations between exclusive breastfeeding and under-five mortality in 57 low- and-middle-income countries.
Methods:
Data were obtained from the latest World Health Organization, United Nations, and United Nations Children's Fund databases for 57 low- and middle-income countries covering the periods 2006-2014. Multivariate linear regression was used to estimate the effects of exclusive breastfeeding on under-five mortality after adjusting for differences in socioeconomic, demographic, and health-related factors.
Results:
In multivariate models, exclusive breastfeeding was independently associated with under-five mortality after adjusting for sociodemographic and health systems-related factors. A '0 percentage-points increase in exclusive breastfeeding was associated with a reduction of 5 child deaths per 1,000 live births. A one-unit increase in Human Development Index was associated with a decrease of 231 under-five child deaths per 1,000 live births. A $100 increase in per capita health care expenditure was associated with a decrease of 2 child deaths per 1,000 live births. One unit increase in physician density was associated with 2.8 units decrease in the under-five mortality rate.
Conclusions and Global Health Implications:
Population-level health system and socioeconomic factors exert considerable effect on the association between exclusive breastfeeding and under-five mortality. Given that the health policy and socioeconomic indicators shown to influence exclusive breastfeeding and under- five mortality are modifiable, policy makers could potentially target specific policies and programs to address national-level deficiencies in these sectors to reduce under-five mortality in their countries.
Keywords
Exclusive breastfeeding
Developing Countries
Under-five Mortality
Child Health
Health Systems Policy
Low- and Middle-income countries
Human Development Index
Introduction
Exclusive breastfeeding is the practice of feeding infants only on breast milk without any additional food or drink, even water, for the first six months of life.[1,2] Exclusive breastfeeding enhances the overall benefits of breast milk, which is widely recognized as the ideal form of nutrition for infants. To achieve optimal growth, development, and health of infants, major national, global health, and professional organizations recommend exclusive breastfeeding of infants for the first six months of life, and continued breastfeeding along with appropriate complementary foods for up to two years of age or beyondJ[1,3] In addition to exclusive breastfeeding, experts recommend that breastfeeding be initiated within the first hour of an infant's life, it should be on demand—that is as often as the child wants—and without the use of bottles, teats, or pacifiers.[1]
The short and long-term health benefits of exclusive breastfeeding for infants and mothers have been well-reported. These benefits include protection from infectious diseases, reduction in the risks of chronic diseases, diabetes, asthma, lymphoma, leukemia, Hodgkin's disease, gastrointestinal tract infection, atopic eczema, and improvement in cognitive functioning.[4-6] Breast milk contains and provides all the nutrients an infant needs for healthy development; it is safe and rich in antibodies that protect infants from the two leading causes of child mortality namely pneumonia and diarrhea worldwide; and breast milk is readily available and affordable.[6,7] Optimal breastfeeding of all children aged 0-23 months could lead to an annual savings of about 800,000 under-five children's lives around the world.[8] Exclusive breastfeeding has also been associated with natural birth control for the first six months after birth, reduction in the risks of breast and ovarian cancers among mothers later in life, reduction in obesity rates, and faster return to their pre-pregnancy weights.[6]
National and global health efforts aimed at promoting exclusive breastfeeding have primarily focused on increasing and tracking the number of mothers around the world who exclusively breastfeed their infants and on individual-level determinants and effects of exclusive breastfeeding on specific health outcomes.[7,9-12] Given this interest, many prior studies have focused on the benefits of exclusive breastfeeding in mitigating health care risks and preventing chronic and infectious diseases such as gastrointestinal problems, asthma, diabetes, obesity, leukemia, lymphoma, and reproductive- aged cancers. There is a paucity of recent studies examining the long-term, cross-national, and population-level impacts of exclusive breastfeeding on major global child health indicators such as under-five mortality rates. To our knowledge, the prior studies that examined the protective effects of exclusive breastfeeding on under-five mortality were based in single sub-Saharan African countries and involved a sample of women.[13-16] Investing all research examining increase in breastfeeding rates alone could be counterproductive given that, despite concerted efforts, only modest improvements have been achieved in increasing exclusive breastfeeding rates in several decades globally.[7]
In this study, we investigate the association between exclusive breastfeeding and under-five mortality, a leading child health indicator, using data from 57 low- and middle-income countries. The aims of our study were two-fold. First, we investigated whether the rates of exclusive breastfeeding were independently associated with under-five mortality. Secondly, we investigated whether the associations, if any, identified in the above were attenuated or otherwise in the presence of other health systems-level factors in 57 countries in our study. We hypothesized an inverse relationship between exclusive breastfeeding and under-five mortality rates. In other words, we expected that under-five mortality rates would be lower in countries with higher rates of exclusive breastfeeding. Understanding how exclusive breastfeeding rates and under-five mortality rates are associated in the presence of other population-level and health-systems factors in countries that share similar socioeconomic, demographic, and health characteristics is important. This information would be useful for policy and program planners in identifying areas of potential intervention that will make a difference in the lives of infants and mothers in their respective countries, and ultimately lead to increase in the uptake of exclusive breastfeeding.
Methods
To quantify the association between exclusive breastfeeding and under-five mortality, we obtained data on indicators from multiple global health data sources for the 57- low and middle-income countries included in our analyses spanning 2006 to 2014. The data on exclusive breastfeeding were from the Global Databases on Infant and Young Child Feeding.[17] Data on under-five mortality were from the World Health Statistics 2015 published by the World Health Organization (WHO).[18] Data on the Human Development Index (HDI) and Gender Inequality Index (GII) were from the United Nations 2014 Human Development Report,[19] while data on health- related indicators namely improved drinking water usage, sanitation usage, physician density, antenatal coverage, births attended, and healthcare expenditure were from the WHO's 2015 World Health Statistics.[18] Where necessary, we augmented missing data on few countries with data from comparable countries as determined by their Gross National Income (GNI). Countries and study covariates were selected based on prior research, field experience, and the need to examine countries with similar socioeconomic and global health systems indicators.[20]
Study variables
Our dependent variable was under-five mortality which is defined as the probability of dying by age 5 per 1,000 live births.[18] Our independent variable was exclusive breastfeeding greater than or equal to 6 months which is defined as the percentage of infants 0 to 5 months of age who are fed exclusively with breast milk.[18] Our study covariates were eight national/health systems- level sociodemographic indicators: HDI, GII, improved drinking water usage, sanitation usage, physician density, antenatal coverage, births attended by trained health personnel, and health care expenditure.
HDI is a composite measure of three basic human development indices, which includes a life expectancy index, an education index, and an income index.[19] Values for HDI vary between 0 and 1, with 0 representing the lowest level of development and 1 representing the highest level.[19] GII is an aggregate measure that depicts gender-based disadvantages based on three dimensions: reproductive health, empowerment, and the labor market.[19] GII values vary between 0 and 1, with 0 indicating equal faring between men and women.[19] Healthcare expenditure is the per capita total expenditure on health expressed in purchasing power parity (PPP) and is internationally-denominated to the United States dollar.[18] Improved drinking water usage is measured as the percentage of the population using an improved drinking water source and improved sanitation usage is measured as the percentage of the population using an improved sanitation facility.[18] Physician density is measured as the number of medical doctors per 10,000 population in a particular area.[18] Antenatal care coverage is the percentage of women between the ages of 15 and 49 with a live birth within a given time period that received four or more antenatal care visits during pregnancy.[18] Births attended is the percentage of births attended by skilled health personnel.[18]
Statistical analysis
Pearson correlation coefficients were computed to examine the bivariate associations between under- five mortality, exclusive breastfeeding, and other covariates. Multivariate Ordinary Least Squares (OLS) regression models were used to determine the independent effects of exclusive breastfeeding and other covariates on under-five mortality rates. Unstandardized regression coefficients (b's) were used to estimate the effect on child mortality associated with per unit change in exclusive breastfeeding and other independent variables. Standardized regression coefficients (β's) were used to estimate the relative impacts of the predictors on under-five mortality rates. Percentage variance explained (R2) determined the goodness of fit of the multivariate models. Statistical analyses were conducted using STATA version 12.[21]
Results
Descriptive statistics
Table 1 presents the 57 countries included in the study, while Figure 1 presents the prevalence of exclusive breastfeeding and under-five mortality rates across the countries. Table 2 presents the description of the study variables. The average under- five mortality rate across the 57 countries was 69.0 child deaths under age 5 per 1,000 live births. Singapore had the lowest under-five mortality rate (2.8 deaths per 1,000 live births), while Angola had the highest under-five mortality rate (167.4). Majority of sub-Saharan African countries had higher under- five mortality rates than their Asian counterparts. Exclusive breastfeeding rates varied among the 57 countries, with an average of 34.0%. Djibouti had the lowest exclusive breastfeeding rate of 1% Mortality are for 2013. Sources: Global Databases on Infant and Young Child Feeding, 2015; World Health Statistics, 2015. while Rwanda had the highest rate of exclusive breastfeeding (85%) followed by Cambodia (74%) and Malawi (71%). Although not shown here, data for the study covariates varied across the countries. In general, Asian countries had an HDI greater than 0.5, with Singapore having the highest HDI of 0.90 among all 57 countries in our analysis. Sub-Saharan African countries of Niger Republic, the Democratic Republic of Congo, and Central African Republic had the lowest HDI at 0.34. The average HDI score was 0.54 for all the 57 countries combined. All the 57 countries had an average GII score of 0.51. Nigeria and Singapore had very low GII values of 0.07 and 0.09, respectively, while Niger and Chad had the highest GII value of 0.71. Singapore and Malaysia both had 100% of their populations using an improved drinking water source, while the Democratic Republic of Congo and Mozambique had the lowest improved drinking water usage at 46% and 49%, respectively. Singapore had the highest sanitation usage (100%) among all 57 countries. Very low levels of sanitation usage were observed among many of the sub-Saharan African countries; Niger Republic had the lowest percentage at 9% followed by Malawi at 10%. All African countries except Algeria, Tunisia, Libya, and Egypt had physician densities of less than 10, meaning that, for every 10,000 persons in these countries, there were fewer than 10 available physicians. Many of the sub-Saharan African countries had an even lower number of less than one available physician per 10,000 persons. Egypt had the highest physician density at 28.3 among all 57 countries, followed by Singapore at 19.5. Antenatal care coverage was highest for Thailand and Brunei (93%) and lowest for Djibouti (7%). The percentage of births attended by skilled health personnel was 100% for 5 of the 57 countries: Libya, Singapore, China, Thailand, and Brunei. Ethiopia had the lowest percentage of births attended by skilled personnel at 10%. The per capita total expenditure on health was lowest in Zimbabwe (PPP int. $20) and highest for Singapore (PPP int. $3,215). The average healthcare expenditure across the 57 countries was PPP int. $342.18.
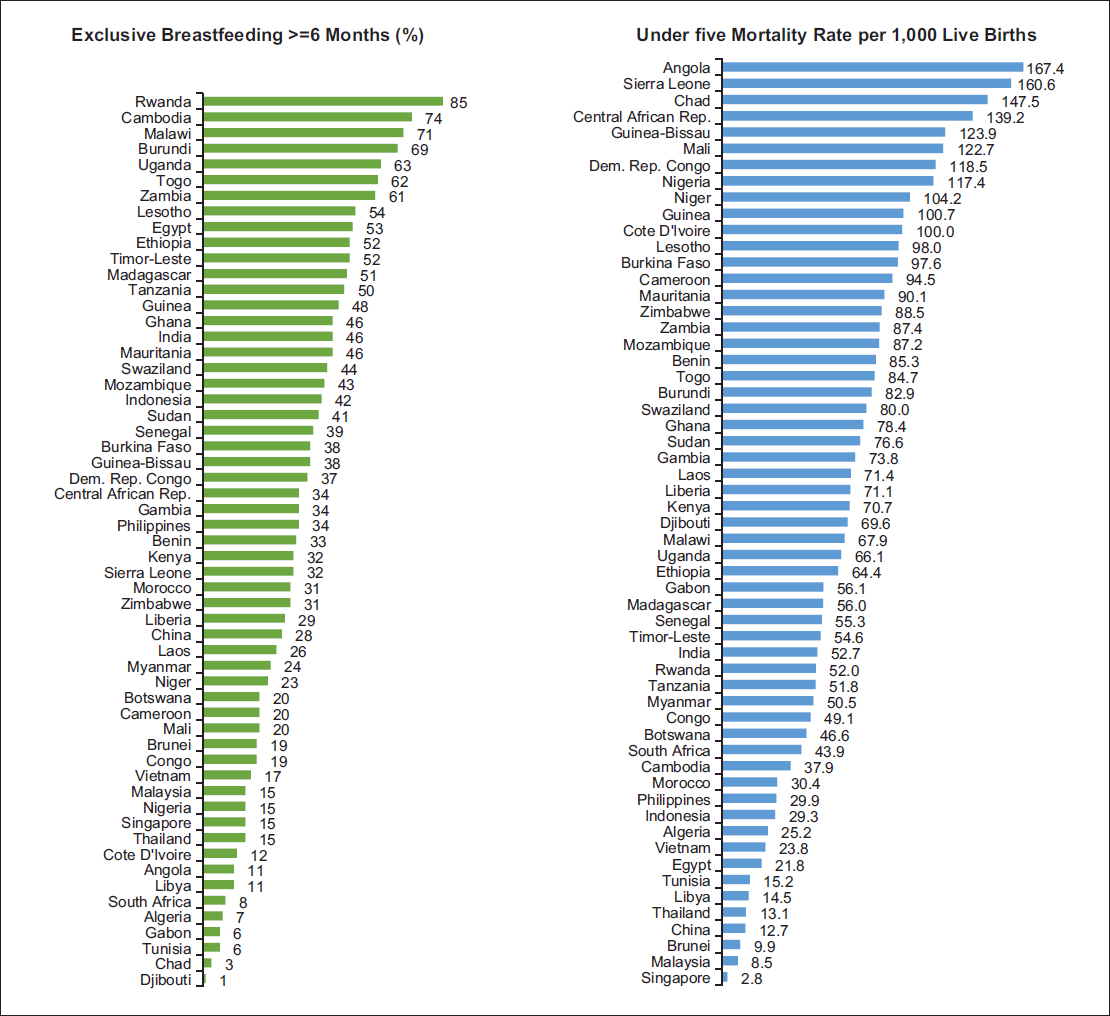
- Exclusive Breastfeeding and Under-fìve Mortality in 57 Low-and-Middle-Income Countries. Data for Exclusive Breastfeeding are for 2008-2012. Data for Under-fìve
| Regions | N | Country |
|---|---|---|
| Africa | 44 | Algeria, Angola, Benin, Botswana, Burkina Faso, Burundi, Cameroon, Central African Republic, Chad, Congo, Cote d’Ivoire, Democratic Republic of Congo, Djibouti, Egypt, Ethiopia, Gabon, Gambia, Ghana, Guinea, Guinea-Bissau, Kenya, Lesotho, Liberia, Libya, Madagascar, Malawi, Mali, Mauritania, Morocco, Mozambique, Niger, Nigeria, Rwanda, Senegal, Sierra Leone, South Africa, Sudan, Swaziland, Togo, Tunisia, Uganda, United Republic of Tanzania, Zambia, Zimbabwe |
| Asia | 13 | Brunei, Cambodia, China, India, Indonesia, Lao People's Democratic Republic, Malaysia, Myanmar, Philippines, Singapore, Thailand, Timor-Leste, Vietnam |
Notes: N = Number of countries. aBased on the United Nations' geographical regions
| Variable | N | Minimum | Maximum | Median | Mean±SD | SE mean |
|---|---|---|---|---|---|---|
| Under-five mortality rate | 57 | 2.8 | 167.4 | 69.6 | 68.98±39.37 | 5.21 |
| Exclusive breastfeeding | 57 | 1 | 85 | 33 | 33.97±19.73 | 2.61 |
| Human development index | 57 | 0.34 | 0.90 | 0.50 | 0.54±0.13 | 0.02 |
| Gender inequality index | 57 | 0.07 | 0.71 | 0.55 | 0.51±0.15 | 0.02 |
| Healthcare expenditure | 57 | 20 | 3215 | 175 | 342.18±511.14 | 67.7 |
| Drinking water usage | 57 | 46 | 100 | 75 | 75.11±15.65 | 2.07 |
| Sanitation usage | 57 | 9 | 100 | 37 | 43.97±27.97 | 3.70 |
| Physician density | 57 | 0.1 | 28.3 | 1.4 | 4.14±5.98 | 0.79 |
| Antenatal coverage | 57 | 7 | 93 | 58 | 59.77±20.37 | 2.70 |
| Births attended | 57 | 10 | 100 | 65 | 65.88±23.65 | 3.13 |
Note: N=Number of countries, SE mean-Standard error of mean, SD-Standard deviation
Bivariate analysis
Table 3 presents the results of our bivariate correlation analysis. There was a significant positive relationship between under-fìve mortality rate and GII (r = 0.41, P< 0.01). This indicated that a higher under-fìve mortality rate was associated with increased gender inequality. There was a significant inverse relationship between under-fìve mortality rate and improved drinking water usage (r = -0.57, P<0.01), sanitation usage (r = -0.62, P<0.01), physician density (r = -0.65, P<0.01), antenatal coverage (r = -0.51, P<0.01), and births attended (r = -0.61, P<0.01). A lower under-fìve mortality rate was associated with higher improved drinking water usage, sanitation usage, physician density, and births attended. In addition, the correlation between HDI and the under-fìve mortality rate was very strong, as indicated by the correlation coefficient of -0.81. There was no significant linear relationship between under-five mortality rate and exclusive breastfeeding (r = 0.05, P > 0.05).
| Variables | (Y) | (X1) | (X2) | (X3) | (X4) | (X5) | (X6) | (X7) | (X8) | (X9) |
|---|---|---|---|---|---|---|---|---|---|---|
| Under-five mortality rate (Y) | 1.00 | |||||||||
| Exclusive breastfeeding (X1) | 0.05 | 1.00 | ||||||||
| Human development index (X2) | −0.81* | −0.33* | 1.00 | |||||||
| Healthcare expenditure (X3) | −0.54* | −0.37* | 0.77* | 1.00 | ||||||
| Gender inequality index (X4) | 0.41* | 0.25 | −0.61* | −0.51* | 1.00 | |||||
| Drinking water usage (X5) | −0.57* | −0.24 | 0.56* | 0.41* | −0.36* | 1.00 | ||||
| Sanitation usage (X6) | −0.62* | −0.33* | 0.70* | 0.52* | −0.63* | 0.59* | 1.00 | |||
| Physician density (X7) | −0.65* | −0.31* | 0.76* | 0.67* | −0.52* | 0.47* | 0.69* | 1.00 | ||
| Antenatal coverage (X8) | −0.51* | −0.20 | 0.68* | 0.49* | −0.36* | 0.52* | 0.38* | 0.52* | 1.00 | |
| Births attended (X9) | −0.61** | −0.21 | 0.66* | 0.55* | −0.34* | 0.62* | 0.56* | 0.57* | 0.69* | 1.00 |
Note: *Statistically significant at p<0.05 level
Multivariate regression analysis
Table 4 presents the results of our multivariate regression analysis. In multivariate Model 1, one unit increase (i.e., one percentage point increase) in exclusive breastfeeding was associated with 0.5 units decrease in under-five mortality rate. Equivalently, a 10 percentage-points increase in exclusive breastfeeding was associated with a reduction of 5 child deaths per 1,000 live births. A one unit increase in HDI was associated with a decrease of 231 under-five deaths per 1,000 live births. Improved drinking water was inversely related to under-five mortality. One percentage point increase in improved drinking water source was associated with 0.47 units decrease in under-five mortality. In multivariate Model 1, a comparison of β's (standardized regression coefficients) indicated that HDI had the strongest effect on under-five mortality, followed by exclusive breastfeeding and improved drinking water. The child mortality impact of HDI was 3.2 greater than that of exclusive breastfeeding. In multivariate Model 2, a $100 US PPP increase in per capita health care expenditure was associated with a decrease of 2 under-five child deaths per 1,000 live births. In multivariate Model 2, physician density had the largest impact on child mortality, followed by improved drinking water source, exclusive breastfeeding, and healthcare expenditure. Covariates in the multivariate Models 1 and 2 explained 72% and 54% of the cross-national variance in under-five mortality, respectively.
| Model | Variables | b | β | t-stat | P-value | VIF | R2 | Adjusted R2 |
|---|---|---|---|---|---|---|---|---|
| 1 | Exclusive breastfeeding + | −0.498 | −0.250 | −3.33 | 0.002 | 1.12 | 73.6 | 72.1 |
| Human development index + | −230.685 | −0.789 | −8.98 | 0.000 | 1.55 | |||
| Drinking water | −0.474 | −0.188 | −2.20 | 0.32 | 1.47 | |||
| 2 | Exclusive breastfeeding + | −0.466 | −0.233 | −2.37 | 0.022 | 1.18 | 57.0 | 53.7 |
| Healthcare expenditure + | −0.016 | −0.207 | −1.62* | 0.111 | 1.98 | |||
| Drinking water + | −0.869 | −0.345 | −3.30 | 0.002 | 1.32 | |||
| Physician density | −2.758 | −0.419 | −3.25 | 0.002 | 2.01 |
Notes: b = Unstandardized regression coefficient; β = Standardized regression coefficient; R2 = Percentage variance explained; VIF = Variance inflation factor; *P=0.05 using one-tailed t-test
Discussion
Using multiple global health databases, we have quantified the associations between under-five mortality and exclusive breastfeeding in the presence of key socioeconomic and policy indicators in developing countries. Our findings support prior country-based studies in Ghana, India, and Tanzania that reported the protective effects of exclusive breastfeeding on under-five mortality.[13-15,22] However, our study adds upon these studies by providing quantifiable evidence across multiple countries using the latest cross-national sociodemographic, human development, and health care data. Our findings on the overwhelming effect of HDI on population-level health indicators in general and under-five mortality in particular are consistent with earlier findings.[20,22]
Prior studies have identified some of the social and economic barriers to exclusive breastfeeding in developing countries at the individual level including unemployment, low income, lack of breastfeeding friendly workplaces, and traditional practices.[11,23] Our study goes beyond the individual-level barriers and demonstrates the diversity of mediating macrosocioeconomic policy factors that affect the ultimate benefit of exclusive breastfeeding in reducing under- five mortality. To the best of our knowledge, this is one of the first studies to empirically document the direct impact of macro socioeconomic factors and exclusive breastfeeding on under-five mortality across various developing countries.
Under-five mortality rate is a key indicator of infant and child health as well as reflection of the socioeconomic and surrounding health and healthcare conditions of a child's environment. As exclusive breastfeeding is thought to directly impact a child's nutrition and subsequent survival, we performed a study to examine the possible effect of exclusive breastfeeding on the under-five mortality rate. The most recent global health statistics were used to assess the relationship between exclusive breastfeeding and under-five mortality rates in the presence of several sociodemographic and health indicators in 57 low- and middle-income countries.
This study has limitations. This is an ecologic crosssectional study; thus, the associations we observed in the study may not be causally-related.[24] Some of the observed associations at the cross-national level may not hold at the individual level. However, given that a health indicator such as under-five mortality cannot be subjected to a randomized controlled trial, due to ethical concerns, ecological studies remain one of the most-robust methodologies for investigating critical issue such as national variations in under- five mortality rates. Further studies are needed to investigate whether the associations observed in this study hold for specific countries and for more advanced, industrialized countries. Subsequent research should also explore the quantifiable link between exclusive breastfeeding and other child health indicators such as infant mortality, stunting, and educational achievement.
Conclusions and Global Health Implications
In conclusion, this study found that in the presence of enabling health systems and sociodemographic indicators such as HDI, physician density, and healthcare expenditure, the association between exclusive breastfeeding and the under-five mortality rate in the 57 countries investigated becomes substantial and statistically significant. These findings suggest that the ability of exclusive breastfeeding to impact the under-five mortality rate is determined, in part, upon other sociodemographic and health factors and, in the presence of these other factors, the effect that exclusive breastfeeding has on the under-five mortality rate is increased. Our findings support the importance of a health system as the overall hub upon which health governance, financing, service delivery, health workforce, information and medicines and vaccines and other technologies work together in improving health outcomes for all citizens.[25] The results of this study indicate that while exclusive breastfeeding is critical in improving child survival, its benefits to the overall improvement of child health, as measured by under-five mortality, are maximized in the presence of a robust environment of functional health systems and capacities. There also needs to be a supportive environment and overall health system of improved sociodemographic and health care factors that will help to drive the benefits of exclusive breastfeeding for the first 6 months of an infant's life. From a public health viewpoint, increasing the awareness of the importance of having supporting environment to further enhance the positive effects of exclusive breastfeeding may help policymakers and other healthcare decision makers improve the policy and programs that deal with infant and child health outcomes. Our study findings are essential to better inform programs and policies aimed at not only increasing exclusive breastfeeding and decreasing under-five mortality, but also improving the lives of children and mothers in these developing countries.
Human Subjects Review:
No IRB approval was required for this study, which is based on the secondary analysis of public-use global health databases.
Financial Disclosure:
None.
Acknowledgments:
The views expressed are the authors’ and not necessarily those of their respective institutions.
Conflicts of Interest:
None.
Funding/Support:
None.
References
- Organization (WHO). Exclusive Breastfeeding. [Online] Available from: http://www.who.int/nutrition/topics/exclusive_breastfeeding/en/ (accessed )
- [Google Scholar]
- Nutrient Adequacy of Exclusive Breastfeeding for the Term Infant During the First Six Months of Life. Switzerland, Geneva: World Health Organization; 2002.
- [Google Scholar]
- Breastfeeding and the Use of Human Milk. Pediatrics. 2005;115(2):496-506.
- [CrossRef] [PubMed] [Google Scholar]
- The Health and Well-Being of Children: A Portrait of States and the Nation, 2011-2012. Rockville, MD: U.S. Department of Health and Human Services; 2014.
- [Google Scholar]
- Promotion of Breastfeeding Intervention Trial (PROBIT): A Randomized Trial in the Republic of Belarus. Journal of the American Medical Association. 2001;285(4):413-420.
- [CrossRef] [PubMed] [Google Scholar]
- 10 Facts on Breastfeeding. Geneva, Switzerland: World Health Organization; [Online] Available from: http://www.who.int/features/factfiles/breastfeeding/facts/en/index2.html (accessed )
- [Google Scholar]
- Global trends in exclusive breastfeeding. International Breastfeeding Journal. 2012;7(12)
- [CrossRef] [PubMed] [Google Scholar]
- Infant and Young Child Feeding. Geneva, Switzerland: World Health Organization; 2014. Report No.: Fact Sheet No. 342
- [Google Scholar]
- Global Strategy for Infant and Young Child Feeding. Geneva, Switzerland: World Health Organization, United Nation. Children's Fund; 2003.
- [Google Scholar]
- Global Targets 2025: To Improve Maternal, Infant and Young Child Nutrition. Geneva, Switzerland: World Health Organization;
- [Google Scholar]
- Infant and Young Child Feeding Behaviors among Working Mothers in India: Implications for Global Health Policy and Practice. International Journal of MCH and AIDS. 2015;3(1):7-15.
- [CrossRef] [Google Scholar]
- Factors Influencing Breastfeeding Exclusivity During the First 6 Months of Life in Developing Countries: a Quantitative and Qualitative Systematic Review. Maternal Child Nutrition 2015 April 7
- [CrossRef] [PubMed] [Google Scholar]
- Determinants of Under-Five Mortality In Builsa District, Upper East Region, Ghana. Journal of Science and Technology. 2010;30(1):45-53.
- [CrossRef] [Google Scholar]
- Analysis of Under-five Mortality in Ghana Using Logit Model. International Journal of Statistics and Applications. 2014;4(4):192-197.
- [Google Scholar]
- Exclusive Breastfeeding Reduces Risk of Mortality in Infants up to 6 Mo of Age Born to HIV-positive Tanzanian Women. American Journal of Clinical Nutrition. 2012;96(5):1071-1078.
- [CrossRef] [PubMed] [Google Scholar]
- Exclusive Breast Feeding is the Strongest Predictor of Infant Survival in Northwest Ethiopia: a longitudinal Study. Journal of Health, Population an. Nutrition. 2015;34(9)
- [CrossRef] [PubMed] [Google Scholar]
- Global Databases-Infant and Young Child Feeding. New York, NY: United Nations Children's Fund; 2015.
- [Google Scholar]
- World Health Statistics 2015. Geneva, Switzerland: World Health Organization; 2015.
- [Google Scholar]
- Human Development Report 2014. New York, NY: United Nations Development Program; 2014.
- [Google Scholar]
- Global Inequalities in Cervical Cancer Incidence and Mortality are Linked to Deprivation, Low Socioeconomic Status, and Huma. Development. International Journal of MCH and AIDS. 2012;1(1):17-30.
- [CrossRef] [Google Scholar]
- Determinants of Under-Five Mortality in Rural Empowered Action Group States in India: An Application of Cox Frailty Model. International Journal of MCH and AIDS. 2012;1(1):60-72.
- [CrossRef] [PubMed] [Google Scholar]
- Social and Economic Barriers to Exclusive Breast Feeding in Rural Zimbabwe. International Journal of MCH and AIDS. 2015;3(1):16-21.
- [CrossRef] [Google Scholar]
- Utilizing Existing Databases. In: Hulley SB, Cummings SR, Browner WS, Grady DG, Newman TB, eds. Designing Clinical Research. Philadelphia, PA: Lippincott Williams & Wilkins; 2007. p. :207-221.
- [Google Scholar]
- Agency for International Development. Strengthening Health Delivery [Online] Available from: https://www.usaid.gov/what-we-do/global-health/health-systems (accessed )
- [Google Scholar]





