Translate this page into:
Housing and Inequalities in US Life Expectancy, Child and Youth Mortality, and All-Cause and Cause-Specific Mortality, 1979-2020: Results from the National Longitudinal Mortality Study and the National Vital Statistics System
* Corresponding author email: gsingh@mchandaids.org.
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 4.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Background:
Limited research exists on the association between housing, life expectancy, and mortality disparities in the United States (US). Using longitudinal individual-level and pooled county-level mortality data from 1979 to 2020, we examine disparities in life expectancy, child and youth mortality, and all-cause and cause-specific mortality in the US by several housing variables.
Methods:
Using the 1979-2011 National Longitudinal Mortality Study (N=1,313,627) and the 2011-2020 linked county-level National Mortality Database and American Community Survey, we analyzed disparities in life expectancy and all-cause and cause-specific disparities by housing tenure, household crowding, and housing stability. Multivariate Cox proportional hazards regression was used to analyze individual-level mortality differentials by housing tenure. Age-adjusted mortality rates and rate ratios were used to analyze area-level disparities in mortality by housing variables.
Results:
US homeowners had, on average, a 3.5-year longer life expectancy at birth than renters (74.22 vs. 70.76 years), with advantages in longevity associated with homeownership being greater for males than for females; for American Indians/Alaska Natives, non-Hispanic Whites, and non-Hispanic Blacks than for Asian/Pacific islanders and Hispanics; and for the US-born than for immigrants. Compared with renters, homeowners had 22% lower risks of all-cause mortality, 15% lower child mortality, 17% lower youth mortality, and significantly lower mortality from cardiovascular diseases, all cancers combined, stomach, liver, esophageal and cervical cancer, diabetes, influenza and pneumonia, COPD, cirrhosis, kidney disease, HIV/AIDS, infectious diseases, unintentional injuries, suicide, and homicide.
Conclusion and Global Health Implications:
Several aspects of housing are strongly associated with life expectancy, child and youth mortality, and all-cause and cause-specific mortality in the US. Policies that aim to provide well-designed, accessible, and affordable housing to residents of both developed and developing countries are important policy options for addressing one of the most fundamental determinants of health for disadvantaged individuals and communities and for reducing health inequities globally.
Keywords
Housing
Life Expectancy
Mortality
Social Determinants
Cause of Death
Race/Ethnicity
Children & Youth
Disparities
Housing Tenure
Household Crowding
Housing Stability
Longitudinal
1. Introduction
Although there are many studies linking various aspects of housing to physical and mental health inequalities in the US,1–3 studies on the association between housing, life expectancy, and mortality disparities are limited. Especially lacking are studies linking housing tenure (home ownership vs. renting) to inequalities in child and youth mortality and all-cause mortality and mortality from leading causes of death such as cardiovascular disease (CVD), cancer, diabetes, chronic obstructive pulmonary disease (COPD), cirrhosis, kidney disease, infectious diseases, and injuries. To our knowledge, there is only one prior study that has shown differences in life expectancy between homeowners and renters in the US.4 The study found that the life expectancy of US homeowners at age 18 was 4.1 years longer than that for renters and the life expectancy gap by housing tenure was greater for women than for men, and for non-Hispanic Whites than for non-Hispanic Blacks and Hispanics.4
Longitudinal studies from the United Kingdom and other European countries show a strong association between housing tenure and housing quality and mortality, with renters experiencing significantly higher mortality risks than homeowners, even after controlling for other social determinants.5,6 For England and Wales, differences in mortality by housing tenure have increased over time in both relative and absolute terms, with the renters or those living in social housing experiencing even higher relative risks of mortality than homeowners in more recent time periods.5
Although individual-level studies linking housing variables to mortality are lacking, a number of aggregate-level ecological studies have examined the relationship between several aspects of housing such as neighborhood deprivation and residential segregation and mortality in the US.7–20 The US socioeconomic deprivation indices developed by Singh and colleagues for different time periods have included, in addition to education, income, poverty, occupation, employment, and transport, a number of housing variables such as homeownership rate, household crowding, lack of complete plumbing facilities, median number of rooms per housing unit, housing units with 4 or more bedrooms, median home value, gross rent, monthly mortgage, and annual real estate taxes. 7,8,13–18 These deprivation indices, constructed at various geographic levels such as census tracts, counties, ZIP codes, cities, towns, places, and metropolitan areas, have been used to analyze temporal inequalities in life expectancy, infant and child mortality, all-cause mortality, and mortality from CVD, cancer, diabetes, respiratory diseases, and HIV/AIDS, showing marked and persistent or increasing disparities in life expectancy and mortality over time. 3,7,8,13–18
Given the wide gap in research on housing and mortality in the US, we use prospective individual-level data from the National Longitudinal Mortality Study (NLMS) to derive life expectancy estimates and all-cause and cause-specific mortality rates and risks by housing tenure.21,22 Additionally, by linking the 2011-2020 pooled mortality data from the National Vital Statistics System (NVSS) to the 2015-2019 American Community Survey (ACS) data at the county level, we examine associations between two housing variables, household crowding, and housing stability, with all-cause and cause-specific mortality rates at the area level.23–25
2. Data and Methods
2.1. The National Longitudinal Mortality Study (NLMS)
To examine the association of housing tenure with all-cause and cause-specific mortality, we used the 1979-2011 NLMS data. The NLMS is a longitudinal dataset for examining socioeconomic, occupational, and demographic factors associated with all-cause and cause-specific mortality in the US.21,22 The NLMS was conducted by the National Heart, Lung, and Blood Institute in collaboration with the US Census Bureau, the National Cancer Institute, the National Institute on Aging, and the National Center for Health Statistics.21,22 The NLMS consisted of 39 Current Population Survey (CPS) and census cohorts between 1973 and 2011 whose survival (mortality) experiences were studied from 1979 to 2011.21 The CPS is a sample household and telephone interview survey of the civilian non-institutionalized population in the US and is conducted by the US Census Bureau to produce monthly national statistics on unemployment and the labor force. Data from death certificates on the fact of death and the cause of death were combined with the socioeconomic and demographic characteristics of the NLMS cohorts by means of the National Death Index.21,22 Detailed descriptions of the NLMS have been provided elsewhere.21,22
We used the public-use NLMS file to derive cohort-based mortality risks during 1979-2011, with a maximum mortality follow-up of 11 years or 4,018 days.21 Child (<18 years) mortality, youth (15-24) mortality, and all-cause and cause-specific mortality risks and life expectancy at birth were the outcome variables in the NLMS. Housing tenure (home ownership vs. renting) was the main independent variable. Differentials in mortality risks by housing tenure were adjusted by multivariate Cox proportional hazards regression for a number of sociodemographic covariates, such as age (continuous), sex (male, female), race/ethnicity (non-Hispanic White, non-Hispanic Black, Asian/Pacific Islander, Hispanic, other) marital status (currently married, widowed, divorced/separated, never married), nativity/immigrant status (US-born, foreign-born), rural-urban residence, educational attainment (<12, 12, 13-15, 16 years), occupation (professional and managerial; sales, clerical and technical support; service; craft and repair; laborer; military; unemployed and not in labor force), and income/poverty level (<100% of poverty level, 100%-149%,150-199%, 200-299%, 300-399%, 400-599%, and at or above 600% of poverty level).16,17,22
The 1979-2011 sample included 1,313,627 individuals aged ≥20 years at the baseline and 156,617 deaths during the 11-year mortality follow-up. In estimating the mortality risk, all those surviving beyond the 11-year follow-up (measured in days) during the follow-up period were treated as right-censored observations. Relative risks of mortality were estimated by hazard ratios derived from the Cox regression models.17 In the NLMS, age-adjusted mortality rates and life expectancy estimates by housing tenure were computed using the person-years approach.16 Follow-up of mortality and survivorship in the NLMS are not available beyond 2011.
2.2. Linkage of the National Vital Statistics System with the American Community Survey
To supplement the individual-level analysis, we conducted area-level analysis of 2011-2020 pooled mortality data by two housing variables, household crowding and housing stability. Specifically, we linked age, sex, race/ethnicity, and cause-specific mortality data from the 2011-2020 NVSS to the selected housing data from the 2015-2019 ACS at the county level using the common geocodes in the two databases.23–25 Household crowding was measured by the percentage of households with more than 1 person per room and grouped into 3 categories: counties with crowding <1.62% (low crowding), 1.62% to 4.84%, and ≥4.85% (high crowding). Housing stability was measured by the percentage of people living in the same house during the past year and was grouped into 3 categories: counties with housing stability <80% (low stability), 80% to 89.99%, and 90% to 100% (high stability).
We used county-level 2013 rural-urban continuum codes linked to the national mortality data to analyze metropolitan-nonmetropolitan patterns in mortality by household crowding and housing stability.3,26 Mortality rates were age-adjusted by the direct method using the age composition of the 2000 US population as the standard.
3. Results
3.1. Housing Tenure, Life Expectancy, Child and Youth Mortality, and Cause-Specific Mortality: The National Longitudinal Mortality Study
Figure 1 shows life expectancy at birth by housing tenure, sex, race/ethnicity, nativity/immigrant status, and rural-urban residence, based on cohort life tables. During 1979-2011, homeowners had a life expectancy of 74.2 years, about 3.5 years longer than the life expectancy of 70.8 years for renters. The difference in life expectancy between homeowners and renters was larger for males than females (4.0 vs. 3.6 years). The difference in life expectancy between homeowners and renters was largest for American Indians/Alaska Natives (AIANs) (3.9 years), non-Hispanic Whites (3.8 years), and non-Hispanic Blacks (3.6 years) and smallest for Asian/Pacific Islanders (APIs) (2.5 years) and Hispanics (0.3 years). US-born homeowners had 4.4 years longer life expectancy than US-born renters. The difference in life expectancy between homeowners and renters was only 0.7 years among the foreign-born. The difference in life expectancy between homeowners and renters was 3.6 years among urban residents and 3.7 years among rural residents.

- Life Expectancy at Birth (Years) by Housing Tenure, Sex, Race/Ethnicity, Nativity/Immigrant Status, and Rural-Urban Residence, United States, 1979-2011, The National Longitudinal Mortality Study
- Source: Data derived from the 1979-2011 National Longitudinal Mortality Study (NLMS). The life expectancy estimates roughly correspond to the midpoint of the study time period, i.e., 1995
Homeownership is associated with reduced mortality risks regardless of education or income level (Figure 2a,b). During 1979-2011, education and income levels were strongly and consistently associated with reduced all-cause mortality rates for both homeowners and renters. Within each level of education and income, homeowners had significantly lower mortality rates than renters (Figure 2a,b).
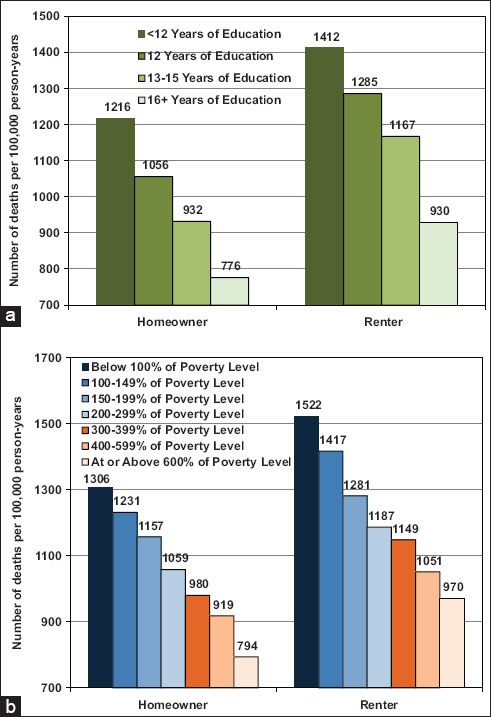
- (a, b) Age-Sex-Adjusted All-Cause Mortality Rates by Housing Tenure, Educational Attainment, and Family Income/Poverty Level, US Population Aged 20+ Years, 1979-2011
- Source: Data derived from the 1979-2011 National Longitudinal Mortality Study (NLMS). Differences in all-cause mortality rates by housing tenure and education and by housing tenure and family income were statistically significant at p<.01
Table 1 presents the results of the age-adjusted and covariate-adjusted Cox models, showing all-cause and cause-specific mortality risks associated with housing tenure. Overall, renters had 28% higher all-cause mortality than homeowners, with the risk of mortality being 31% higher for male renters and 25% higher for female renters. After controlling for socioeconomic and demographic factors, the relative risk of mortality was reduced but was still 13% higher for renters than homeowners. The reduced risk of mortality associated with homeownership was largest for AIANs and non-Hispanic Whites. AIAN renters had a 40% higher age-adjusted risk and a 30% higher covariate-adjusted risk of mortality than AIAN homeowners.
| Cause of death | Both sexes combined1 | Male2 | Female2 | Both sexes combined3 | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Age-Adjusted | Age-Adjusted | Age-Adjusted | Covariate-Adjusted | |||||||||
| Hazard ratio | 95% confidence Interval | Hazard ratio | 95% confidence Interval | Hazard ratio | 95% confidence Interval | Hazard ratio | 95% confidence Interval | |||||
| All causes combined | 1.28 | 1.27 | 1.30 | 1.31 | 1.29 | 1.33 | 1.25 | 1.23 | 1.27 | 1.13 | 1.12 | 1.14 |
| Non-Hispanic White | 1.30 | 1.29 | 1.32 | 1.35 | 1.33 | 1.38 | 1.25 | 1.23 | 1.28 | 1.15 | 1.13 | 1.16 |
| Non-Hispanic Black | 1.26 | 1.22 | 1.30 | 1.26 | 1.20 | 1.32 | 1.26 | 1.20 | 1.32 | 1.08 | 1.04 | 1.12 |
| Non-Hispanic AIAN | 1.40 | 1.23 | 1.59 | 1.42 | 1.19 | 1.70 | 1.34 | 1.11 | 1.61 | 1.30 | 1.14 | 1.49 |
| Non-Hispanic API | 1.18 | 1.06 | 1.31 | 1.21 | 1.06 | 1.39 | 1.13 | 0.96 | 1.32 | 1.05 | 0.94 | 1.18 |
| Hispanic | 1.09 | 1.04 | 1.14 | 1.09 | 1.02 | 1.16 | 1.08 | 1.00 | 1.16 | 0.95 | 0.90 | 1.00 |
| Child (<18 years) mortality4 | 1.18 | 1.08 | 1.29 | 1.19 | 1.07 | 1.32 | 1.20 | 1.03 | 1.40 | 1.06 | 0.96 | 1.17 |
| Youth (15-24 years) mortality4 | 1.20 | 1.11 | 1.29 | 1.25 | 1.14 | 1.38 | 1.25 | 1.09 | 1.43 | 1.06 | 0.97 | 1.15 |
| Working ages 20-64 years | 1.58 | 1.55 | 1.61 | 1.57 | 1.54 | 1.61 | 1.58 | 1.53 | 1.62 | 1.20 | 1.17 | 1.22 |
| Cardiovascular diseases (CVD) | 1.24 | 1.22 | 1.27 | 1.23 | 1.20 | 1.26 | 1.24 | 1.21 | 1.27 | 1.12 | 1.10 | 1.14 |
| Heart disease | 1.26 | 1.23 | 1.28 | 1.22 | 1.19 | 1.26 | 1.26 | 0.12 | 1.30 | 1.12 | 1.10 | 1.15 |
| Stroke | 1.17 | 1.12 | 1.22 | 1.27 | 1.19 | 1.37 | 1.11 | 1.05 | 1.18 | 1.08 | 1.03 | 1.14 |
| All cancers combined | 1.09 | 1.06 | 1.11 | 1.12 | 1.08 | 1.16 | 1.08 | 1.05 | 1.12 | 1.06 | 1.04 | 1.09 |
| Lung cancer | 1.18 | 1.13 | 1.23 | 1.21 | 1.14 | 1.29 | 1.17 | 1.09 | 1.25 | 1.18 | 1.12 | 1.24 |
| Colorectal cancer | 1.03 | 0.96 | 1.11 | 1.05 | 0.94 | 1.17 | 1.03 | 0.93 | 1.13 | 1.01 | 0.93 | 1.09 |
| Prostate cancer | 0.94 | 0.85 | 1.05 | 0.93 | 0.83 | 1.04 | ||||||
| Breast cancer | 0.94 | 0.86 | 1.02 | 0.97 | 0.89 | 1.06 | ||||||
| Cervical cancer | 1.83 | 1.45 | 2.31 | 1.31 | 1.01 | 1.71 | ||||||
| Stomach cancer | 1.30 | 1.13 | 1.49 | 1.24 | 1.03 | 1.50 | 1.40 | 1.13 | 1.72 | 1.14 | 0.98 | 1.32 |
| Liver and IBD cancer | 1.46 | 1.24 | 1.71 | 1.55 | 1.26 | 1.92 | 1.34 | 1.04 | 1.73 | 1.22 | 1.02 | 1.46 |
| Esophageal cancer | 1.34 | 1.14 | 1.57 | 1.20 | 0.99 | 1.47 | 1.67 | 1.26 | 2.22 | 1.17 | 0.98 | 1.39 |
| Diabetes | 1.45 | 1.35 | 1.56 | 1.41 | 1.26 | 1.57 | 1.49 | 1.36 | 1.64 | 1.14 | 1.06 | 1.23 |
| Pneumonia and influenza | 1.40 | 1.31 | 1.50 | 1.45 | 1.32 | 1.59 | 1.37 | 1.25 | 1.50 | 1.21 | 1.13 | 1.29 |
| COPD | 1.36 | 1.29 | 1.43 | 1.39 | 1.29 | 1.49 | 1.36 | 1.26 | 1.47 | 1.13 | 1.06 | 1.2 |
| Liver cirrhosis | 1.64 | 1.48 | 1.80 | 1.79 | 1.58 | 2.03 | 1.42 | 1.21 | 1.67 | 1.12 | 1.01 | 1.25 |
| Nephritis/kidney diseases | 1.38 | 1.25 | 1.53 | 1.45 | 1.24 | 1.68 | 1.35 | 1.17 | 1.55 | 1.14 | 1.02 | 1.27 |
| Alzheimer’s disease | 0.73 | 0.65 | 0.84 | 0.61 | 0.48 | 0.79 | 0.79 | 0.68 | 0.92 | 0.83 | 0.72 | 0.94 |
| HIV/AIDS | 2.88 | 2.56 | 3.25 | 2.99 | 2.60 | 3.44 | 2.35 | 1.87 | 2.97 | 1.58 | 1.39 | 1.80 |
| Children aged <18 years4 | 2.54 | 1.34 | 4.82 | 2.02 | 0.89 | 4.56 | 3.94 | 1.31 | 11.88 | 1.84 | 0.92 | 3.79 |
| Youth aged 15-24 years4 | 2.46 | 1.74 | 3.48 | 2.01 | 1.36 | 2.97 | 7.11 | 2.92 | 17.32 | 31.75 | 1.2 | 2.56 |
| Other infectious diseases | 1.64 | 1.48 | 1.81 | 1.66 | 1.44 | 1.93 | 1.61 | 1.40 | 1.84 | 1.27 | 1.14 | 1.42 |
| Septicemia (sepsis) | 1.56 | 1.40 | 1.75 | 1.54 | 1.30 | 1.83 | 1.58 | 1.36 | 1.84 | 1.27 | 1.12 | 1.43 |
| Tuberculosis (TB) | 3.04 | 1.92 | 4.81 | 2.89 | 1.60 | 5.23 | 3.34 | 1.61 | 6.92 | 1.80 | 1.08 | 3.00 |
| Unintentional injuries | 1.41 | 1.32 | 1.50 | 1.41 | 1.30 | 1.52 | 1.33 | 1.20 | 1.47 | 1.14 | 1.06 | 1.22 |
| Motor vehicle accidents | 1.19 | 1.08 | 1.31 | 1.21 | 1.07 | 1.37 | 1.13 | 0.96 | 1.34 | 1.08 | 0.97 | 1.2 |
| Non-motor-vehicle injuries | 1.53 | 1.41 | 1.65 | 1.54 | 1.39 | 1.70 | 1.37 | 1.20 | 1.56 | 1.16 | 1.07 | 1.27 |
| Suicide | 1.27 | 1.14 | 1.40 | 1.31 | 1.17 | 1.47 | 1.13 | 0.91 | 1.41 | 1.11 | 0.99 | 1.24 |
| Homicide | 1.97 | 1.69 | 2.30 | 1.88 | 1.55 | 2.28 | 2.15 | 1.65 | 2.81 | 1.04 | 0.87 | 1.23 |
| Children aged <18 years4 | 2.95 | 2.30 | 3.77 | 3.28 | 2.46 | 4.36 | 2.24 | 1.36 | 3.70 | 1.27 | 0.95 | 1.68 |
| Youth aged 15-24 years4 | 1.84 | 1.45 | 2.33 | 2.18 | 1.66 | 2.87 | 1.34 | 0.83 | 2.16 | 1.03 | 0.79 | 1.33 |
| Firearm injuries | 1.21 | 1.09 | 1.35 | 1.25 | 1.11 | 1.41 | 1.08 | 0.83 | 1.39 | 0.96 | 0.85 | 1.08 |
| Children aged <18 years4 | 1.75 | 1.41 | 2.17 | 1.87 | 1.48 | 2.36 | 1.36 | 0.78 | 2.38 | 1.08 | 0.84 | 1.38 |
| Youth aged 15-24 years4 | 1.26 | 1.04 | 1.53 | 1.43 | 1.15 | 1.74 | 1.07 | 0.95 | 1.13 | 1.04 | 0.84 | 1.29 |
Children aged <18 years living in rented homes had 18% higher mortality than children in owner-occupied homes, with differences in racial/ethnic composition, household income, and rural-urban residence accounting for the excess mortality. Similar patterns existed in youth mortality; male and female renters aged 15-24 had a 25% higher mortality risk than homeowners. Controlling for covariates accounted for differences in youth mortality (Table 1).
Homeownership was associated with a reduced risk of cardiovascular disease (CVD) mortality, with the impact of homeownership on reduced stroke mortality being significantly greater for men than for women (27% vs. 11%). Homeownership was associated with lower cancer mortality, and the association was particularly strong for cervical cancer mortality. Female renters had an 83% higher age-adjusted risk and 31% higher covariate-adjusted risk of cervical cancer mortality than female homeowners. Renters had higher mortality from stomach, liver, and esophageal cancer than homeowners, reflecting their higher risks of Helicobacter pylori infection, alcohol consumption, hepatitis infection, and smoking.27
Compared with homeowners, renters had 36-64% higher observed risks of mortality from diabetes, pneumonia and influenza, chronic obstructive pulmonary disease (COPD), cirrhosis, and kidney disease. Renters were at higher risk of infectious disease mortality; in age-sex-adjusted models, renters had 2.9 times higher risk of HIV/AIDS mortality, 3.0 times higher risk of tuberculosis mortality, and 1.6 times higher risk of sepsis mortality than homeowners. In age-sex-adjusted models, renters had 41% higher unintentional injury mortality, 27% higher suicide mortality, and 97% higher risk of homicide victimization, compared with homeowners (Table 1).
3.2. County-Level Associations between Household Crowding and Cause-Specific Mortality Rates
Table 2 shows age-adjusted all-cause and cause-specific mortality rates at the county level by household crowding (percentage of households with more than one person per room) during 2011 to 2020. Higher levels of household crowding in racial/ethnic minority communities were associated with higher all-cause mortality rates. For example, APIs and Hispanics in communities with higher levels of household crowding had 15 to 17% higher mortality rates than their counterparts in communities with lower levels of crowding. Similar relationships between household crowding and county-level mortality existed, particularly for AI/AN and non-metropolitan children and youth. AI/AN children and youth living in counties with high levels of household crowding had, respectively, 41% and 50% higher mortality rates than their counterparts living in counties with low levels of crowding. Children and youth living in non-metropolitan counties with high levels of household crowding had, respectively, 17% and 37% higher mortality rates than their counterparts living in counties with low levels of crowding.
| Cause of death | Household crowding (% households with>1 person per room, 2015-2019) | |||||||
|---|---|---|---|---|---|---|---|---|
| <1.62% | 1.62% to 4.84% | ≥4.85% | Relative Risk | |||||
| Mortality rate | SE | Mortality rate | SE | Mortality rate | SE | High vs. Low Crowding | ||
| All causes combined | 773.75 | 0.28 | 755.22 | 0.20 | 649.54 | 0.31 | 0.84 | * |
| Non-Hispanic White | 770.26 | 0.30 | 758.03 | 0.22 | 695.41 | 0.46 | 0.90 | * |
| Black | 924.15 | 1.15 | 898.75 | 0.64 | 790.08 | 1.08 | 0.85 | * |
| AIAN | 501.15 | 3.87 | 652.92 | 2.08 | 572.95 | 2.41 | 1.14 | * |
| API | 366.30 | 1.71 | 393.74 | 0.84 | 420.57 | 0.66 | 1.15 | * |
| Hispanic | 490.03 | 1.61 | 549.02 | 0.67 | 575.10 | 0.58 | 1.17 | * |
| Metropolitan area | 758.51 | 0.32 | 733.77 | 0.21 | 633.49 | 0.32 | 0.84 | * |
| Non-Metropolitan area | 822.87 | 0.59 | 869.29 | 0.53 | 827.88 | 1.51 | 1.01 | * |
| Children aged <18 years | 52.80 | 0.17 | 54.68 | 0.11 | 43.46 | 0.15 | 0.82 | * |
| Non-Hispanic White | 46.67 | 0.19 | 46.92 | 0.14 | 38.33 | 0.28 | 0.82 | * |
| Black | 91.20 | 0.58 | 86.97 | 0.31 | 67.93 | 0.54 | 0.74 | * |
| AIAN | 35.31 | 1.51 | 45.59 | 0.70 | 49.78 | 0.97 | 1.41 | * |
| API | 30.17 | 0.70 | 32.52 | 0.37 | 27.67 | 0.34 | 0.92 | * |
| Hispanic | 42.72 | 0.53 | 45.01 | 0.22 | 40.61 | 0.21 | 0.95 | * |
| Metropolitan area | 51.26 | 0.19 | 52.97 | 0.12 | 42.04 | 0.16 | 0.82 | * |
| Non-Metropolitan area | 58.39 | 0.38 | 65.22 | 0.32 | 68.22 | 0.83 | 1.17 | * |
| Youth aged 15-24 years | 71.23 | 0.26 | 72.21 | 0.17 | 59.67 | 0.25 | 0.84 | * |
| Non-Hispanic White | 68.16 | 0.29 | 66.82 | 0.22 | 57.78 | 0.47 | 0.85 | * |
| Black | 104.71 | 0.85 | 104.29 | 0.47 | 83.32 | 0.82 | 0.80 | * |
| AIAN | 58.33 | 2.75 | 77.47 | 1.35 | 87.38 | 1.81 | 1.50 | * |
| API | 27.46 | 0.88 | 33.55 | 0.52 | 32.28 | 0.52 | 1.18 | * |
| Hispanic | 53.12 | 0.87 | 60.55 | 0.37 | 55.79 | 0.35 | 1.05 | * |
| Metropolitan area | 69.96 | 0.29 | 69.85 | 0.18 | 57.30 | 0.25 | 0.82 | * |
| Non-Metropolitan area | 75.79 | 0.58 | 86.97 | 0.51 | 103.74 | 1.47 | 1.37 | * |
| Hypertension without heart disease | 7.75 | 0.03 | 8.46 | 0.02 | 11.03 | 0.04 | 1.42 | * |
| Non-Hispanic White | 7.24 | 0.03 | 7.53 | 0.02 | 10.12 | 0.05 | 1.40 | * |
| Black | 15.29 | 0.15 | 16.37 | 0.09 | 19.21 | 0.17 | 1.26 | * |
| AIAN | 4.53 | 0.38 | 7.43 | 0.24 | 7.41 | 0.29 | 1.64 | * |
| API | 4.20 | 0.19 | 6.06 | 0.11 | 9.16 | 0.10 | 2.18 | * |
| Hispanic | 4.62 | 0.16 | 6.38 | 0.08 | 9.98 | 0.08 | 2.16 | * |
| Liver cirrhosis | 10.22 | 0.03 | 10.82 | 0.02 | 11.74 | 0.04 | 1.15 | * |
| Non-Hispanic White | 10.54 | 0.04 | 11.30 | 0.03 | 11.51 | 0.06 | 1.09 | * |
| Black | 7.78 | 0.10 | 7.19 | 0.05 | 7.15 | 0.10 | 0.92 | |
| AIAN | 17.73 | 0.65 | 28.00 | 0.37 | 28.09 | 0.46 | 1.58 | * |
| API | 3.34 | 0.15 | 3.50 | 0.07 | 3.71 | 0.06 | 1.11 | * |
| Hispanic | 11.54 | 0.23 | 13.60 | 0.09 | 16.17 | 0.09 | 1.40 | * |
| Liver and IBD cancer | 5.79 | 0.02 | 6.54 | 0.02 | 7.67 | 0.03 | 1.32 | * |
| Non-Hispanic White | 5.49 | 0.02 | 5.86 | 0.02 | 5.94 | 0.04 | 1.08 | * |
| Black | 8.08 | 0.10 | 8.35 | 0.06 | 7.95 | 0.10 | 0.98 | |
| AIAN | 5.62 | 0.39 | 8.23 | 0.22 | 6.57 | 0.25 | 1.17 | |
| API | 7.17 | 0.22 | 8.83 | 0.12 | 9.23 | 0.10 | 1.29 | * |
| Hispanic | 7.70 | 0.20 | 9.03 | 0.08 | 9.57 | 0.07 | 1.24 | * |
| Stomach cancer | 2.48 | 0.02 | 2.88 | 0.01 | 4.08 | 0.02 | 1.65 | * |
| Non-Hispanic White | 2.18 | 0.02 | 2.25 | 0.01 | 2.62 | 0.03 | 1.20 | * |
| Black | 5.24 | 0.09 | 5.27 | 0.05 | 5.09 | 0.09 | 0.97 | |
| AIAN | 1.88 | 0.23 | 2.81 | 0.14 | 4.13 | 0.20 | 2.20 | * |
| API | 4.10 | 0.17 | 4.50 | 0.09 | 5.27 | 0.07 | 1.29 | * |
| Hispanic | 4.18 | 0.15 | 4.64 | 0.06 | 5.29 | 0.05 | 1.27 | * |
| Influenza and pneumonia | 14.71 | 0.04 | 13.84 | 0.03 | 15.67 | 0.05 | 1.07 | * |
| Non-Hispanic White | 14.84 | 0.04 | 13.96 | 0.03 | 15.29 | 0.07 | 1.03 | * |
| Black | 14.68 | 0.15 | 15.09 | 0.08 | 18.82 | 0.17 | 1.28 | * |
| AIAN | 10.34 | 0.58 | 12.84 | 0.30 | 15.61 | 0.42 | 1.51 | * |
| API | 7.63 | 0.26 | 8.75 | 0.13 | 15.31 | 0.13 | 2.01 | * |
| Hispanic | 8.61 | 0.22 | 9.90 | 0.09 | 13.86 | 0.09 | 1.61 | * |
| Tuberculosis (TB) | 0.09 | 0.00 | 0.13 | 0.00 | 0.26 | 0.01 | 2.89 | * |
| Non-Hispanic White | 0.07 | 0.00 | 0.08 | 0.00 | 0.09 | 0.01 | 1.29 | * |
| Black | 0.19 | 0.02 | 0.24 | 0.01 | 0.25 | 0.02 | 1.32 | * |
| AIAN | 0.34 | 0.05 | 0.48 | 0.07 | 1.41 | * | ||
| API | 0.54 | 0.06 | 0.62 | 0.03 | 0.67 | 0.03 | 1.24 | * |
| Hispanic | 0.14 | 0.03 | 0.21 | 0.01 | 0.32 | 0.01 | 2.29 | * |
| HIV/AIDS | 1.04 | 0.01 | 1.93 | 0.01 | 2.52 | 0.02 | 2.42 | * |
| Non-Hispanic White | 0.54 | 0.01 | 0.87 | 0.01 | 1.55 | 0.02 | 2.87 | * |
| Black | 5.42 | 0.08 | 7.63 | 0.05 | 9.40 | 0.11 | 1.73 | * |
| AIAN | 0.74 | 0.13 | 1.17 | 0.07 | 1.09 | 0.09 | 1.47 | * |
| API | 0.21 | 0.03 | 0.29 | 0.02 | 0.43 | 0.02 | 2.05 | * |
| Hispanic | 1.45 | 0.07 | 1.57 | 0.03 | 2.09 | 0.03 | 1.44 | * |
| Homicide | 4.95 | 0.03 | 6.66 | 0.02 | 5.66 | 0.03 | 1.14 | * |
| Non-Hispanic White | 2.52 | 0.02 | 3.09 | 0.02 | 2.91 | 0.04 | 1.15 | * |
| Black | 21.74 | 0.16 | 21.36 | 0.09 | 16.70 | 0.14 | 0.77 | * |
| AIAN | 4.41 | 0.31 | 7.07 | 0.17 | 7.30 | 0.22 | 1.66 | * |
| API | 1.46 | 0.08 | 1.83 | 0.05 | 1.78 | 0.04 | 1.22 | * |
| Hispanic | 3.80 | 0.10 | 5.36 | 0.05 | 5.34 | 0.04 | 1.41 | * |
| Alzheimer’s disease | 27.29 | 0.05 | 28.45 | 0.04 | 29.28 | 0.07 | 1.07 | * |
| Non-Hispanic White | 27.58 | 0.05 | 29.65 | 0.04 | 34.64 | 0.10 | 1.26 | * |
| Black | 27.09 | 0.21 | 25.38 | 0.12 | 23.85 | 0.20 | 0.88 | * |
| AIAN | 13.74 | 0.72 | 17.63 | 0.40 | 12.45 | 0.40 | 0.91 | |
| API | 10.89 | 0.32 | 12.06 | 0.16 | 15.98 | 0.13 | 1.47 | * |
| Hispanic | 19.04 | 0.35 | 21.50 | 0.15 | 25.48 | 0.13 | 1.34 | * |
SE=standard error. AIAN=American Indian and Alaska Native. API=Asian and Pacific Islander. IBD=Intrahepatic bile duct.
The higher the level of household crowding, the higher the rate of mortality from hypertension. For example, non-Hispanic Whites living in areas with high levels of household crowding were 40% more likely to die from hypertension than Whites in areas with low levels of crowding. Consistent gradients in mortality by household crowding were found for several prominent causes of death, including cirrhosis, liver and stomach cancer, influenza and pneumonia, tuberculosis (TB), HIV/AIDS, and Alzheimer’s disease, with the magnitude of the association varying by race/ethnicity. Compared to those living in areas with low household crowding, those living in areas with high levels of crowding had a 15% higher risk of cirrhosis mortality, 32% higher risk of liver cancer mortality, 65% higher stomach cancer mortality, and 7% higher influenza and pneumonia mortality. Those living in areas with high levels of household crowding were, respectively, 2.4 and 2.9 times more likely to die from HIV/AIDS and TB than those living in areas with low crowding.
3.3. County-Level Associations between Housing Stability and Cause-Specific Mortality
Table 3 shows age-adjusted cause-specific mortality rates from 2011 to 2020 at the county level by housing stability levels (defined as the percentage of those living in the same house during the past year) stratified by race/ethnicity and metropolitan area. Low housing stability was associated with increased mortality from all causes combined and child mortality in rural, non-metropolitan areas, and from stroke, COPD, liver cirrhosis, suicide, and Alzheimer’s disease. Those living in areas of low housing stability had a 15% higher risk of stroke mortality than those living in areas with high housing stability. The stroke mortality risk associated with low housing stability increased by 34% for Blacks and 56% for APIs. The risk of cirrhosis mortality and suicide in the Hispanic population increased by 48% and 64% in areas with low housing stability, respectively.
| Cause of death | Housing stability (% living in the same house during past year, 2015-2019) | |||||||
|---|---|---|---|---|---|---|---|---|
| <80% | 80% to 89.99% | 90% to 100% | Relative Risk | |||||
| Mortality rate | SE | Mortality rate | SE | Mortality rate | SE | Low vs. High Stability | ||
| All causes combined | 758.56 | 0.71 | 738.87 | 0.16 | 746.91 | 0.41 | 1.02 | * |
| Non-Hispanic White | 746.65 | 0.78 | 753.79 | 0.18 | 764.16 | 0.48 | 0.98 | |
| Black | 934.73 | 2.40 | 894.64 | 0.56 | 802.98 | 1.25 | 1.16 | * |
| AIAN | 672.20 | 7.34 | 581.98 | 1.62 | 721.54 | 3.84 | 0.93 | |
| API | 389.83 | 3.39 | 411.67 | 0.53 | 363.71 | 1.50 | 1.07 | * |
| Hispanic | 600.71 | 2.96 | 557.80 | 0.46 | 566.24 | 1.19 | 1.06 | * |
| Metropolitan area | 751.51 | 0.75 | 722.02 | 0.17 | 690.28 | 0.47 | 1.09 | * |
| Non-Metropolitan area | 805.94 | 2.01 | 841.66 | 0.44 | 880.56 | 0.81 | 0.92 | * |
| Children aged <18 years | 52.60 | 0.35 | 52.08 | 0.09 | 48.98 | 0.23 | 1.07 | * |
| Non-Hispanic White | 44.19 | 0.41 | 45.93 | 0.11 | 46.08 | 0.30 | 0.96 | * |
| Black | 87.60 | 1.04 | 86.55 | 0.27 | 68.56 | 0.67 | 1.28 | * |
| AIAN | 46.43 | 2.41 | 41.48 | 0.57 | 71.39 | 1.76 | 0.65 | * |
| API | 30.34 | 1.27 | 30.71 | 0.26 | 25.04 | 0.69 | 1.21 | * |
| Hispanic | 45.65 | 0.82 | 43.48 | 0.16 | 37.14 | 0.42 | 1.23 | * |
| Metropolitan area | 52.74 | 0.37 | 50.73 | 0.09 | 41.25 | 0.25 | 1.28 | * |
| Non-Metropolitan area | 51.66 | 0.99 | 61.88 | 0.28 | 69.48 | 0.52 | 0.74 | * |
| Youth aged 15-24 years | 46.38 | 0.38 | 71.31 | 0.14 | 72.27 | 0.39 | 0.64 | * |
| Non-Hispanic White | 40.94 | 0.44 | 68.36 | 0.19 | 75.08 | 0.53 | 0.55 | * |
| Black | 74.31 | 1.22 | 105.94 | 0.42 | 81.16 | 0.99 | 0.92 | * |
| AIAN | 74.96 | 4.04 | 70.72 | 1.07 | 128.39 | 3.45 | 0.58 | |
| API | 20.52 | 1.08 | 33.57 | 0.38 | 30.57 | 1.12 | 0.67 | * |
| Hispanic | 49.46 | 1.17 | 58.88 | 0.27 | 52.15 | 0.73 | 0.95 | * |
| Metropolitan area | 47.19 | 0.42 | 69.54 | 0.15 | 61.24 | 0.42 | 0.77 | * |
| Non-Metropolitan area | 41.77 | 0.95 | 84.17 | 0.44 | 102.15 | 0.90 | 0.41 | * |
| Stroke | 38.52 | 0.16 | 37.86 | 0.04 | 33.48 | 0.08 | 1.15 | * |
| Non-Hispanic White | 36.48 | 0.17 | 36.33 | 0.04 | 33.16 | 0.10 | 1.10 | * |
| Black | 54.49 | 0.60 | 53.09 | 0.14 | 40.61 | 0.28 | 1.34 | * |
| AIAN | 26.32 | 1.57 | 25.10 | 0.36 | 27.08 | 0.78 | 0.97 | |
| API | 30.54 | 0.97 | 31.61 | 0.15 | 19.63 | 0.35 | 1.56 | * |
| Hispanic | 32.72 | 0.72 | 33.51 | 0.12 | 24.92 | 0.26 | 1.31 | * |
| Metropolitan area | 38.19 | 0.17 | 37.35 | 0.04 | 29.68 | 0.10 | 1.29 | * |
| COPD | 43.79 | 0.17 | 40.55 | 0.04 | 38.32 | 0.09 | 1.14 | * |
| Non-Hispanic White | 47.02 | 0.19 | 45.60 | 0.04 | 43.42 | 0.11 | 1.08 | * |
| Black | 33.15 | 0.46 | 29.98 | 0.10 | 24.09 | 0.22 | 1.38 | |
| AIAN | 30.93 | 1.66 | 29.81 | 0.38 | 26.23 | 0.76 | 1.18 | * |
| API | 12.41 | 0.63 | 12.42 | 0.09 | 9.28 | 0.25 | 1.34 | * |
| Hispanic | 19.26 | 0.56 | 17.76 | 0.09 | 16.58 | 0.21 | 1.16 | * |
| Metropolitan area | 42.63 | 0.18 | 38.21 | 0.04 | 32.15 | 0.10 | 1.33 | * |
| Liver cirrhosis | 11.45 | 0.09 | 10.98 | 0.02 | 9.66 | 0.05 | 1.19 | * |
| Non-Hispanic White | 11.28 | 0.10 | 11.29 | 0.02 | 9.53 | 0.06 | 1.18 | * |
| Black | 8.32 | 0.20 | 7.46 | 0.05 | 5.94 | 0.10 | 1.40 | * |
| AIAN | 30.11 | 1.31 | 25.49 | 0.29 | 33.70 | 0.76 | 0.89 | * |
| API | 3.19 | 0.28 | 3.69 | 0.05 | 2.78 | 0.12 | 1.15 | * |
| Hispanic | 19.68 | 0.47 | 14.86 | 0.07 | 13.29 | 0.17 | 1.48 | * |
| Metropolitan area | 42.63 | 0.18 | 38.21 | 0.04 | 32.15 | 0.10 | 1.33 | * |
| Nephritis/kidney disease | 13.59 | 0.09 | 13.00 | 0.02 | 13.48 | 0.05 | 1.01 | |
| Non-Hispanic White | 11.51 | 0.10 | 11.65 | 0.02 | 12.83 | 0.06 | 0.90 | * |
| Black | 29.43 | 0.44 | 25.94 | 0.10 | 19.64 | 0.20 | 1.50 | * |
| AIAN | 13.79 | 1.12 | 11.22 | 0.23 | 14.64 | 0.56 | 0.94 | |
| API | 8.59 | 0.52 | 8.56 | 0.08 | 6.06 | 0.20 | 1.42 | * |
| Hispanic | 13.38 | 0.46 | 11.62 | 0.07 | 11.00 | 0.17 | 1.22 | * |
| Metropolitan area | 13.29 | 0.10 | 12.64 | 0.02 | 11.84 | 0.06 | 1.12 | * |
| Suicide | 15.04 | 0.10 | 13.43 | 0.02 | 11.72 | 0.06 | 1.28 | * |
| Non-Hispanic White | 17.59 | 0.13 | 17.01 | 0.03 | 14.83 | 0.08 | 1.19 | * |
| Black | 6.90 | 0.17 | 6.35 | 0.04 | 4.46 | 0.09 | 1.55 | * |
| AIAN | 15.22 | 0.85 | 11.71 | 0.18 | 16.87 | 0.51 | 0.90 | |
| API | 6.98 | 0.35 | 6.54 | 0.06 | 5.56 | 0.17 | 1.26 | * |
| Hispanic | 8.77 | 0.25 | 6.68 | 0.04 | 5.34 | 0.10 | 1.64 | * |
| Metropolitan area | 14.87 | 0.11 | 12.80 | 0.02 | 9.61 | 0.06 | 1.55 | * |
| Unintentional injuries | 45.30 | 0.17 | 45.45 | 0.04 | 45.82 | 0.11 | 0.99 | * |
| Non-Hispanic White | 46.91 | 0.21 | 50.95 | 0.05 | 52.82 | 0.15 | 0.89 | * |
| Black | 41.49 | 0.46 | 42.92 | 0.11 | 34.90 | 0.26 | 1.19 | * |
| AIAN | 65.93 | 1.98 | 48.29 | 0.40 | 73.59 | 1.12 | 0.90 | |
| API | 19.51 | 0.70 | 16.85 | 0.10 | 12.93 | 0.27 | 1.51 | * |
| Hispanic | 37.53 | 0.62 | 31.51 | 0.09 | 28.52 | 0.23 | 1.32 | * |
| Metropolitan area | 44.79 | 0.18 | 43.72 | 0.04 | 39.07 | 0.12 | 1.15 | * |
| Alzheimer’s disease | 32.37 | 0.15 | 28.96 | 0.03 | 22.64 | 0.07 | 1.43 | * |
| Non-Hispanic White | 33.28 | 0.16 | 30.29 | 0.03 | 24.02 | 0.08 | 1.39 | * |
| Black | 30.22 | 0.47 | 26.61 | 0.10 | 18.01 | 0.19 | 1.68 | * |
| AIAN | 14.79 | 1.26 | 15.27 | 0.30 | 15.76 | 0.63 | 0.94 | |
| API | 14.59 | 0.71 | 15.31 | 0.11 | 6.64 | 0.22 | 2.20 | * |
| Hispanic | 26.01 | 0.69 | 24.36 | 0.10 | 18.25 | 0.23 | 1.43 | * |
| Metropolitan area | 32.27 | 0.16 | 28.66 | 0.03 | 18.98 | 0.08 | 1.70 | * |
SE=standard error. AIAN=American Indian and Alaska Native. API=Asian and Pacific Islander. IBD=Intrahepatic bile duct.
4. Discussion
In this paper, we have presented empirical evidence linking several aspects of housing to life expectancy, child and youth mortality, and all-cause and cause-specific mortality in the US, using both longitudinal individual-level data and county-level ecological analyses. Life expectancy at birth was 3.6 and 4.0 years longer for female and male homeowners, respectively than their renting counterparts. Overall, renters had 28% higher all-cause mortality than homeowners, but the reduced mortality or increased survival advantage associated with homeownership was greater among males than females. Housing tenure continued to be associated with all-cause mortality even after controlling for socioeconomic status. At each education or income level, homeowners had significantly lower mortality than renters. Compared with renters, homeowners had lower risks of mortality from several leading causes of death, including CVD, all cancers combined, stomach, liver, esophageal, and cervical cancer, diabetes, influenza and pneumonia, COPD, cirrhosis, kidney disease, HIV/AIDS, infectious diseases, unintentional injuries, suicide, and homicide. Although most of the analyses in our study are new, several of our findings are consistent with those observed in previous studies.4–6,28–31
Household crowding and housing instability at the county level contribute to increased mortality from several leading causes of death, including cardiovascular, respiratory, and infectious diseases, and injuries. The housing variables influence mortality not only through associated socioeconomic pathways, but their mortality effects may also operate via psychosocial stress, mental health problems, infections, smoking, drinking, physical inactivity, and inadequate access to health care associated with adverse housing conditions.
While adverse socioeconomic conditions (such as low educational attainment, poverty, and social deprivation) associated with household crowding may contribute to higher rates of mortality, several other factors associated with crowding such as higher levels of stress, mental health problems, alcohol consumption, close-contact infections, Helicobacter pylori infection, and hepatitis infection might also account for increased mortality from these causes.27
Housing is an important social determinant of health, which affects health, disease, mortality, and healthcare outcomes in a variety of ways.3,32,33 Homeownership and improvements in housing and neighborhood conditions have long been used as key policy instruments to improve population health and to reduce health disparities among populations.31,32,34 Home ownership is an indicator of wealth and represents a higher socioeconomic position in most societies, which is generally associated with better health. However, homeownership does not only represent material aspects of one’s social position. It also has other social and psychological meanings and benefits, such as increased attachment to one’s immediate neighborhood as well as to the larger community, higher community engagement, social connectedness, and social support, all of which are associated with people’s health and wellbeing.31,32,34,35
4.1. Limitations
Our study lacked data on psychosocial factors (social integration), physical and mental health status at baseline, health behaviors (diet, smoking, drinking, obesity, and physical inactivity), neighborhood factors including housing conditions, and healthcare access that could partly explain the association between housing tenure and cause-specific mortality. Secondly, we considered only a dichotomous measure of housing tenure (homeowners vs. renters) due to data availability. A multifaceted nature of housing tenure that differentiates renters who receive rental or housing assistance from a government program from those who do not receive any rental assistance would have provided additional insight into why renters experience a higher risk of mortality than homeowners.31,36,37 Compared with homeowners and non-rental assistance renters, public housing residents and rental assistance renters have higher levels of social isolation, unemployment, lower education and incomes, and higher rates of obesity, smoking, secondhand smoke exposure at home, asthma, poorer health status, depressive symptoms, and hypertension.31,32,36,38 Thirdly, NLMS did not have mortality/survivorship follow-up data after 2011. Having more recent follow-up data would have allowed us to examine whether disparities in life expectancy and mortality between homeowners and renters have widened over time. Finally, additional housing variables such as household crowding, housing quality, housing cost burden, and housing stability, which are lacking in NLMS, are needed at the individual or household level that can allow for a more thorough investigation of housing and inequalities in life expectancy, mortality, and other health outcomes.
5. Conclusion and Global Health Implications
Using both longitudinal individual-level analyses and county-level ecological analyses, our study shows that several aspects of housing such as housing tenure, household crowding, and housing stability are strongly associated with life expectancy, child and youth mortality, and all-cause and cause-specific mortality in the US. Homeowners had, on average, a 3.5-year longer life expectancy at birth than renters, with advantages in longevity associated with homeownership being greater for males than for females; for AIANs, non-Hispanic Whites, and non-Hispanic Blacks than for APIs and Hispanics; and for the US-born than for immigrants. Compared with renters, homeowners had lower risks of all-cause mortality and mortality from CVD, all cancers combined, stomach, liver, esophageal and cervical cancer, diabetes, influenza and pneumonia, COPD, cirrhosis, kidney disease, HIV/AIDS, infectious diseases, unintentional injuries, suicide, and homicide.
Sound housing policies that aim to provide well-designed, accessible, and affordable housing to urban as well as rural residents in both developed and developing countries are an important policy option for addressing one of the most fundamental determinants of health for disadvantaged individuals and communities and for reducing health inequities globally.39
Acknowledgments:
None.
Compliance with Ethical Standards
Conflicts of Interest: The authors declare that they have no conflict of interest.
Financial Disclosure: None to report.
Funding/Support: None.
Ethics Approval: No IRB approval was required for this study, which is based on the secondary analysis of two public-use federal databases.
Disclaimer: The views expressed are the authors’ and not necessarily those of their institutions.
References
- Where We Live Matters For Our Health:The Links Between Housing and Health. Issue Brief 2:Housing And Health. Robert Wood Johnson Foundation Commission to Build a Healthier America. Published September 2008. http://www.commissiononhealth.org/PDF/e6244e9e-f630-4285-9ad7-16016dd7e493/Issue%20Brief%202%20Sept%2008%20-%20Housing%20and%20Health.pdf
- [Google Scholar]
- Housing Instability. Healthy People 2020. https://www.healthypeople.gov/2020/topics-objectives/topic/social-determinants-health/interventions-resources/housing-instability
- Social determinants of health in the United States:addressing major health inequality trends for the nation, 1935-2016. Int J MCH AIDS. 2017;6(2):139-164. doi:10.21106/ijma.236
- [Google Scholar]
- Marked disparities in life expectancy by education, poverty level, occupation, and housing tenure in the United States, 1997-2014. Int J MCH AIDS. 2021;10(1):7-18. doi:10.21106/ijma.402
- [Google Scholar]
- Differences in mortality by housing tenure and by car access from the OPCS Longitudinal Study. Popul Trends. 1995;81:27-30.
- [Google Scholar]
- Housing wealth and mortality:A register linkage study of the Finnish population. Soc Sci Med. 2009;69(5):754-760. doi:10.1016/j.socscimed.2009.06.035
- [Google Scholar]
- Area deprivation and widening inequalities in US mortality, 1969–1998. Am J Public Health. 2003;93(7):1137-1143. doi:10.2105/ajph.93.7.1137
- [Google Scholar]
- Increasing inequalities in all-cause and cardiovascular mortality among US adults aged 25–64 years by area socioeconomic status, 1969–1998. Int J Epidemiol. 2002;31(3):600-613. doi:10.1093/ije/31.3.600
- [Google Scholar]
- Segregation and mortality over time and space. Soc Sci Med. 2018;199:77-86. doi:10.1016/j.socscimed.2017.07.006
- [Google Scholar]
- Residential segregation and lung cancer mortality in the United States. JAMA Surg. 2013;148(1):37-42. doi:10.1001/jamasurgery.2013.408
- [Google Scholar]
- Segregation and violence reconsidered:Do whites benefit from residential segregation? Am Sociol Rev. 2019;84(4):690-725.
- [Google Scholar]
- The Role of Racial Residential Segregation in Black-White Disparities in Firearm Homicide at the State Level in the United States, 1991-2015. J Natl Med Assoc. 2019;111(1):62-75. doi:10.1016/j.jnma.2018.06.002
- [Google Scholar]
- Widening socioeconomic inequalities in US life expectancy, 1980-2000. Int J Epidemiol 2006 doi:10.1093/ije/dyl083
- [Google Scholar]
- All-cause and cause-specific mortality among US youth:socioeconomic and rural-urban disparities and international patterns. J Urban Heal. 2013;90(3):388-405. doi:10.1007/s11524-012-9744-0
- [Google Scholar]
- Persistent socioeconomic disparities in infant, neonatal, and postneonatal mortality rates in the United States, 1969-2001. Pediatrics. 2007;119(4):e928-39. doi:10.1542/peds.2005-2181
- [Google Scholar]
- Widening socioeconomic and racial disparities in cardiovascular disease mortality in the United States, 1969-2013. Int J MCH AIDS. 2015;3(2):106.
- [Google Scholar]
- Socioeconomic and racial/ethnic disparities in cancer mortality, incidence, and survival in the United States, 1950–2014:over six decades of changing patterns and widening inequalities. J Environ Public Health. 2017;2017:2819372. doi:10.1155/2017/2819372
- [Google Scholar]
- Area deprivation and inequalities in health and health care outcomes. Ann Intern Med 2019 doi:10.7326/M19-1510
- [Google Scholar]
- Trends in US urban black infant mortality, by degree of residential segregation. Am J Public Health. 1996;86(5):723-726. doi:10.2105/ajph.86.5.723
- [Google Scholar]
- Metropolitan governance, residential segregation, and mortality among African Americans. Am J Public Health. 1998;88(3):434-438. doi:10.2105/ajph.88.3.434
- [Google Scholar]
- National Longitudinal Mortality Study, Reference Manual. Published 2012 http://www.census.gov/did/www/nlms/publications/reference.html
- Immigrant health inequalities in the United States:use of eight major national data systems. ScientificWorldJournal. 2013;2013:512313. doi:10.1155/2013/512313
- [Google Scholar]
- Deaths:Final data for 2019. 2021. National Vital Statistics Report. 70:1-87. https://www.cdc.gov/nchs/data/nvsr/nvsr70/nvsr70-08-508.pdf
- [Google Scholar]
- National Vital Statistics System, Mortality Multiple Cause-of-Death Public Use Data File Documentation. Hyattsville, MD: US Department of Health and Human Services; Published 2020 http://www.cdc.gov/nchs/nvss/mortality_public_use_data.htm
- The American Community Survey (ACS) Public Use Microdata Sample (PUMS), 2015-2019. Published 2021 https://www.census.gov/programs-surveys/acs/microdata.html
- Widening rural-urban disparities in life expectancy, US, 1969–2009. Am J Prev Med. 2014;46(2):e19-e29. doi:10.1016/j.amepre.2013.10.017
- [Google Scholar]
- WHO Housing and Health Guidelines. Geneva: World Health Organization; 2018.
- Psychological distress and heart disease mortality in the United States:results from the 1997-2014 NHIS-NDI Record Linkage Study. Int J MCH AIDS. 2020;9(3):260-273.
- [Google Scholar]
- The Association Between Psychological Distress and Cancer Mortality in the United States:Results from the 1997–2014 NHIS-NDI Record Linkage Study. Ann Behav Med. 2021;55(7):621-640. doi:10.21106/ijma.391
- [Google Scholar]
- Psychological distress, life expectancy, and all-cause mortality in the United States:results from the 1997–2014 NHIS-NDI record linkage study. Ann Epidemiol. 2021;56:9-17. doi:https://doi.org/10.1016/j.annepidem.2021.01.002
- [Google Scholar]
- 2020. Health Equity Report 2019-2020:Special Feature on Housing and Health Inequalities. Rockville, Maryland https://www.hrsa.gov/sites/default/files/hrsa/health-equity/HRSA-health-equity-report-printer.pdf
- Housing and public health. Annu Rev Public Health. 2004;25:397-418. doi:10.1146/annurev.publhealth.25.101802.123036
- [Google Scholar]
- Housing and health inequalities:a synthesis of systematic reviews of interventions aimed at different pathways linking housing and health. Health Place. 2011;17(1):175-184. doi:10.1016/j.healthplace.2010.09.011
- [Google Scholar]
- Housing and inequalities in health. J Epidemiol Community Health. 2002;56(9):645-646. doi:10.1136/jech.56.9.645
- [Google Scholar]
- Housing and inequalities in health:a study of socioeconomic dimensions of housing and self reported health from a survey of Vancouver residents. J Epidemiol Community Health. 2002;56(9):671-681. doi:10.1136/jech.56.9.671
- [Google Scholar]
- Subsidized Housing and Adult Asthma in Boston, 2010-2015. Am J Public Health. 2018;108(8):1059-1065. doi:10.2105/AJPH.2018.304468
- [Google Scholar]
- Examining ethnic inequalities in health and tenure in England:A repeated cross-sectional analysis. Health Place. 2017;46:82-90. doi:10.1016/j.healthplace.2017.04.011
- [Google Scholar]
- Use of a population-based survey to describe the health of Boston public housing residents. Am J Public Health. 2008;98(1):85-91. doi:10.2105/AJPH.2006.094912
- [Google Scholar]
- World Conference on Social Determinants of Health. Rio DeJaneiro, Brazil. October 19-21, 2011 https://www.who.int/publications/i/item/9789241502405





