Translate this page into:
Geographic, Health Care Access, Racial Discrimination, and Socioeconomic Determinants of Maternal Mortality in Georgia, United States
*Corresponding author email: earmstrongmensah@gsu.edu
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Over the past decade, the United States has been taking steps to reduce its rising maternal mortality rate. However, these steps have yet to produce positive results in the state of Georgia, which tops the list of all 50 states with the highest maternal mortality rate of 46.2 maternal deaths per 100,000 live births for all women, and a maternal mortality rate of 66.6 deaths per 100,000 live births for African American women. In Georgia, several social determinants of health such as the physical environment, economic stability, health care access, and the quality of maternal care contribute to the high maternal mortality rate. Addressing these determinants will help to reduce the state’s maternal mortality rate. This commentary discusses the relationship between social determinants of health and maternal mortality rates in Georgia. It also proposes strategies for reversing the trend. We conducted an ecological study of the relationship between social determinants of health and maternal mortality in Georgia. We searched PubMed and Google Scholar and reviewed 80 English articles published between 2005 and 2021. We identified five key social determinants associated with high maternal mortality rates in Georgia - geographic location of obstetric services, access to health care providers, socioeconomic status, racism, and discrimination. We found that expanding Medicaid coverage, reducing maternal health care disparities among the races, providing access to maternal care for women in rural areas, and training a culturally competent health workforce, will help to reduce Georgia’s high maternal mortality rate.
Keywords
Maternal Mortality
Social Determinants
Pregnancy
Georgia
United States
1. Introduction
Maternal mortality is a public health issue that affects women all over the world. In 2020, the global maternal mortality rate was 152 deaths per 100,000 live births.1 Recognizing the gravity of the issue, the United Nations launched the Millennium Development Goals (MDGs) in 2000 to be achieved in 2015 and the Sustainable Development Goals (SDG) in 2015 to be achieved in 2030.2 MDG 5 focused on reducing maternal mortality by 75 percent by 20153 and currently, SDG 3 focuses on reducing global maternal mortality ratio to less than 70 per 100,000 live births.4 Thanks to these efforts, the global maternal mortality rate (MMR) has significantly declined in many parts of the world. Indeed, between 2000 and 2017, global MMR dropped from 451,000 maternal deaths per 100,000 live births to 295,000 maternal deaths per100,000 live births.5 Unfortunately, eight countries (American Samoa, Canada, Greece, Guam, Jamaica, St. Vincent and the Grenadines, and Zimbabwe) including the United States (US) have not been able to significantly reduce their MMR.
For over several decades, the US experienced a drastic decrease in MMR, however in recent decades, the country’s MMR has been trending upwards. According to available literature, between 1987 and 2016, MMR in the US increased from 7.2 maternal deaths per 100,000 live births to 16.9 maternal deaths per 100,000 live births.6 This is a paradox, as the US spends more money per capita on health care for its citizens, including pregnant women than any other country.7 According to available literature, Georgia had the highest MMR (66.3 maternal deaths per 100,000 live births) between 2013 and 2017 and currently ranks second highest in the country, surpassing the national average of 29.6 maternal deaths per 100,000 live births.8 The high MMR in Georgia is due to a number of social determinants of health including, geographic location of obstetric services, access to health care providers, socioeconomic status, lack of access to essential quality health care, racism, and discrimination.9
We conducted an ecological study on the relationship between social determinants of health such as the geographic location of obstetric services, access to health care providers, socioeconomic status, racism and discrimination, and maternal mortality rate in Georgia. We searched PubMed, Google Scholar and other search engines and reviewed 80 English articles published between 2005 and 2021. We conducted our search using a combination of keywords including maternal mortality, maternal mortality rate in Georgia, social determinants, and pregnancy. Thirty-six articles met our study’s inclusion criteria. Data on maternal mortality in Georgia were obtained from the Georgia Department of Public Health website. These data were used to highlight the maternal mortality issue in Georgia. This commentary discusses the relationship between social determinants of health and maternal mortality rates in Georgia. It also proposes strategies for reversing the trend.
2. Prevalence of Maternal Mortality in Georgia
Maternal mortality is:
The annual number of female deaths from any cause related to or aggravated by pregnancy… during pregnancy and childbirth or within 42 days of termination of pregnancy, irrespective of the duration and site of the pregnancy (WHO, 2021, p1).
Maternal mortality may either be pregnancy-related or pregnancy-associated. Pregnancy-related mortality occurs when a woman dies while pregnant or within 42 days of termination of pregnancy irrespective of the cause of death, and pregnancy-associated mortality occurs when a woman dies after childbirth due to health conditions exacerbated from the effects of her pregnancy.10 In the US, approximately 17% of maternal deaths occur on the day of delivery, 52% during the postpartum period, 19% between one to six days of the postpartum period, and 21% between one to six weeks of the postpartum period.
Between 2012-2016, there were 66 pregnancy-associated deaths per 100,000 live births and 26 pregnancy-related deaths per 100,000 live births among women in Georgia.11 Findings of the Georgia Maternal Mortality Review Committee show that from 2012 to 2014, 101 women in Georgia died from pregnancy-related deaths and 149 from pregnancy-associated deaths.12 Approximately 18% of the pregnancy-related deaths occurred during pregnancy, and 82% during the postpartum period.12 Pregnancy-related maternal mortality was higher among African American women (47 deaths per 100,000 live births) compared to White women (14.3 deaths per 100,000 live births).12 According to the Georgia Department of Public Health, common causes of pregnancy-associated deaths in Georgia are motor vehicle crashes, drug toxicity, and homicides.13 Aggregate data from the Georgia Department of Health show that pregnancy-related deaths in Georgia are primarily due to cardiomyopathy, cardiovascular diseases, hemorrhage, embolism, preeclampsia, and eclampsia.14
In 2010, Amnesty International ranked Georgia as the state with the worst maternal mortality rate in the US.15 About a decade later (2021), the state was ranked as having the second-worst MMR in the US - 48.4 per 100,000 live births (Figure 1).16 Demographic factors such as age, marital status, educational level, and race of women have also been found to be associated with high maternal mortality in Georgia.17 In 2012, the prevalence of pregnancy-related and pregnancy-associated deaths among women in Georgia was highest among women aged 20-24 years (29.4%) followed by women aged 25-29 years (24.7) (Table 1).17 In 2013, the prevalence increased for all age groups except for women aged 20-24 years (25.3%), 25-29 years (21.5%), and women aged 35-39 years (8.9%) (Table 1).13
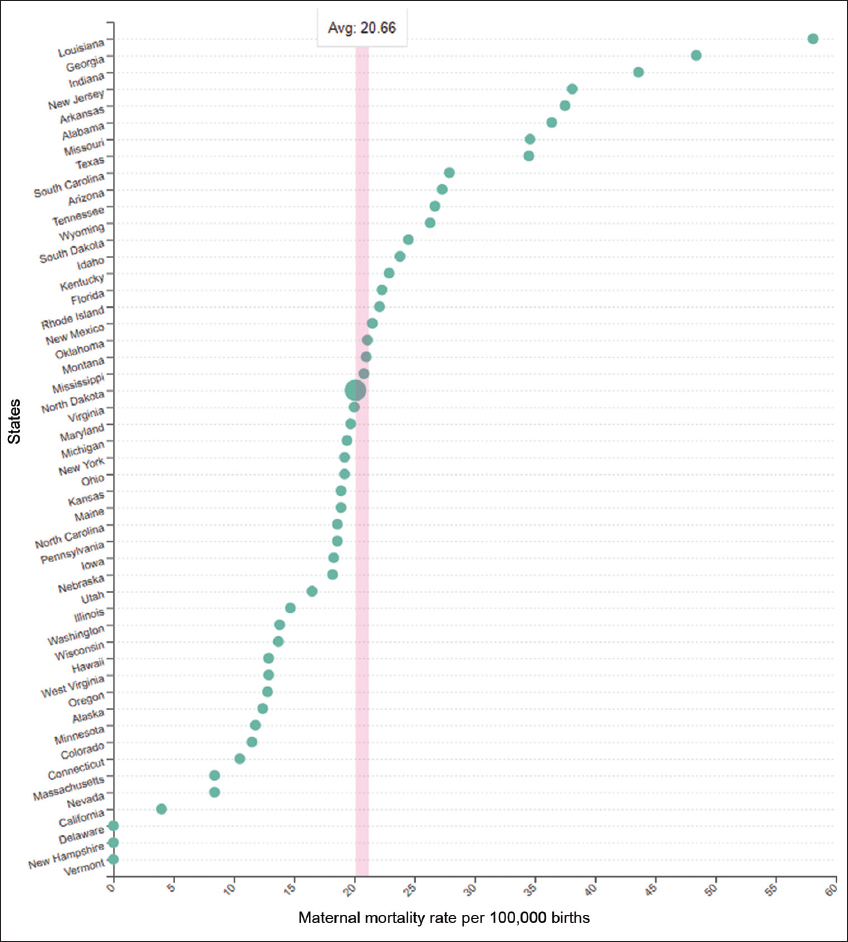
- Maternal mortality rate by state, 2021. World Population Review. https://worldpopulationreview.com/state-rankings/maternal-mortality-rate-by-state. Published 2021.16
| Demographics | Pregnancy-related and Pregnancy-associated Deaths in 2012 (n=85) | Pregnancy-related and Pregnancy- associated Deaths in 2013 (n=79) |
|---|---|---|
| Maternal Age | ||
| <20 | 5.9% | 6.3% |
| 20-24 | 29.4% | 25.3% |
| 25-29 | 24.7% | 21.5% |
| 30-34 | 18.8% | 29.1% |
| 35-39 | 14.1% | 8.9% |
| 40+ | 7.1% | 8.9% |
| Marital Status | ||
| Married | 37.6% | 43.0% |
| Never Married | 28.2% | 48.1% |
| Other/ Unknown | 34.1% | 8.9% |
| Educational Level | ||
| No High school Diploma | 30.4% | 27.1% |
| High school Diploma | 51.9% | 49.4% |
| Associates Degree | 6.3% | 11.8% |
| Bachelor’s Degree | 6.3% | 8.2% |
| Master’s Degree or Higher | 5.2% | 1.2% |
| Unknown | 0% | 2.4% |
| Race | ||
| Black/African American | 48.2% | 46.8% |
| White | 42.5% | 43.0% |
| Hispanic | 5.9% | 7.6% |
| Other/ Unknown | 3.6% | 2.5% |
Data obtained from Georgia Department of Public Health: Georgia maternal mortality 2012 case review at https://dph.georgia.gov/maternal-mortality; and Georgia Department of Public Health: Reducing maternal mortality in Georgia 2013 Case Review Update at https://dph.georgia.gov/maternal-mortality.13,17
In 2012, MMR was higher (37.6%) among married women in Georgia than among women who had never been married (28.2%), however, in 2013, both groups saw an increase in MMR - 43.0% and 48.1%, respectively. Between 2012 and 2013, women in Georgia with no education, high school diploma, or an associate degree were 88.3% to 88.6% more likely to have complications during pregnancy compared to women who had a bachelor’s degree or higher.13,17 Regarding race, maternal mortality was highest among African American women (48.2% - 46.8%), followed by Whites (42.5% - 43%) and then Hispanics (5.9% - 7.6%) in Georgia between 2012 and 2013 (Table 1).13,17
In 2018, Georgia’s overall MMR was 20% higher than the national average of 46.2 deaths for every 100,000 births. The MMR was highest among African American women (approximately 66.6 deaths for every 100,000 births) and much less among Hispanic women (18.1 deaths for every 100,000 births).18
3. Social Determinants and Maternal Mortality
The geographic location of obstetric services, access to health care providers, socioeconomic status, racism, and discrimination contribute to the high MMR in Georgia.19
3.1. Geographic Location of Obstetric Services and Access to Health Care Providers
Over the last several decades, Georgia has experienced a string of hospital labor and delivery services closures across the state, especially in rural areas.20 Between 1994 and 2015, there were 34 labor and delivery unit closures in hospitals outside Metropolitan Atlanta (Figure 2). In 2015, only 46 of the 159 counties in Georgia had labor and delivery units.20 In 2019, 93 of the 109 rural counties in Georgia lacked a hospital labor and delivery unit, and 75 lacked an obstetrician-gynecologist(OB/GYNs).21 Consequently, about 83% of women in rural Georgia who once had a birthing facility close to their home, now have to travel long distances to other counties to access prenatal care and hospital delivery services.22 The loss of time during travel sometimes requires these women to have a Cesarean section or induced birth, all of which have the tendency to result in birth complications and death.23
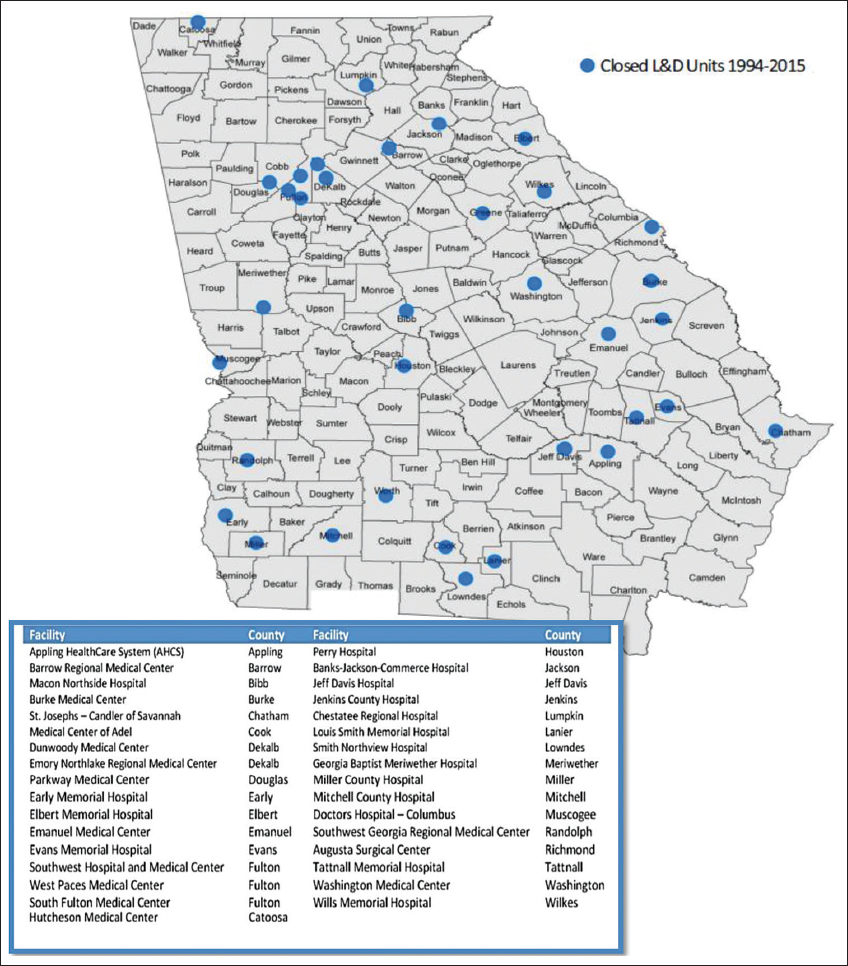
- Closed Labor and Delivery Unite in Georgia (1994-2015). Obtained from Pinto et al. Bridging the Gaps in Obstetric Care: Perspectives of Service Delivery Providers on Challenges and Core Components of Care in Rural Georgia, 2016.35
Regarding physician to population ratio, rural Georgia counties are greatly underserved by OB/GYNs.8 According to the Georgia Board of Health Care Workforce, the rate of OB-GYN physicians in Georgia is 12.6 per 100,000 residents.24 In rural Georgia, the rate is 127 actively practicing OB-GYNs for a population of 1,794,520, translating to 7.1 physicians per 100,000 residents.8 In Oglethorpe and Madison counties which are rural and have a population of 15, 054 and 29,650 respectively, there are no OB GYNs. In Barrow and Jackson counties which are also rural with populations of 80, 809 and 70, 422 respectively, there is only 1 OB-GYN – translating to 1.2 and 1.4 OB-GYNs respectively per 100,000 residents.8 In Oconee county another rural area, there are 5 OB-GYNs for a population of 39,272, translating to 12.7 OB-GYNs per 100,000 residents.8 The low numbers of practicing OB-GYN’s make it difficult for women in rural Georgia to receive much-needed pre-and postnatal care, putting them at risk for death.8
3.2. Socioeconomic Status
Low socioeconomic status (SES) has implications for MMR. Women with low SES have been found to be unaware of the possible relationship between not seeking or receiving timely and adequate prenatal and postnatal care, and negative maternal health outcomes.25 In Georgia, poor patient-health care provider communication has been linked to delayed or discontinued prenatal care-seeking behavior26 and the late referral of high-risk patients to specialists for attention.26 In their study to understand disparities in access to prenatal care in four study sites in Georgia, Hueston et al. stated that almost all study participants indicated that poor communication with their health care provider determined their continued utilization of services. Study participants said they became averse to care and disengaged from their health care providers when they felt they were being ignored or unheard.27
The lack of access to health insurance also negatively impacts MMR in Georgia. Although the Patient Protection and Affordable Care Act (ACA) allows states to expand Medicaid coverage to uninsured populations, Georgia has chosen not to expand coverage.28 This decision has left about 240,000 Georgian’s including pregnant women of low SES uninsured.28 According to Meyer et al., pregnant women in rural Georgia experience interruptions and inconsistencies in seeking prenatal and postnatal care due to the lack of access to health insurance.29 Among pregnant women in Georgia receiving Medicaid, it was observed that most had to rotate between health care providers and wait for long hours to receive care.29 This, they said was a disincentive for them to continue to seek prenatal and postnatal care.
Access to prenatal care allows pregnant women to receive health education, nutritional support, preventative care, and social services to ensure healthy outcomes for themselves and their child.30 Due to the lack of access to health insurance, some pregnant women with low SES in Georgia end up having to undergo unnecessary Cesarean sections and lack access to much-needed care for maternal conditions such as preeclampsia, premature rupture of membranes, and vaginal bleeding.31
3.3. Racism and Discrimination
As a result of racism, African American women in the US are often ignored by health care providers and thus, receive substandard care during pregnancy and delivery.19 It is therefore not surprising that this population experiences higher MMR than other races.19 In Georgia, about 21% of African American women experience some form of racism before, during, and or after birth.32 Per Taylor et al., pregnant African American women in Georgia often do not receive help from medical providers when they are in pain or are experiencing discomfort during and after the birthing process.19 This act has the tendency to negatively impact their health outcomes and lives.19 Maternal mortality is preventable, thus, no woman in Georgia, including African American women, should die during pregnancy or after delivery.
4. Reducing Maternal Mortality
4.1. Geographic Location and the Workforce
To increase access to quality pre and postnatal care, it is important for organizations such as the Georgia Nurses Association, Midwives of Georgia, Georgia Birth Advocacy Coalition, Georgia Composite Medical Board, and Georgia Hospital Association to collaborate and come up with strategies to provide maternal services to women in rural Georgia.33 This will ensure that health care professionals (certified nurse-midwives) other than OB-GYNs are trained and available to provide appropriate and quality maternal care to women in rural and underserved areas in Georgia.34
4.2. Socioeconomic Status
All women in Georgia, regardless of their socioeconomic status, location, and race, should have equal access to the resources they need to ensure positive pregnancy, birth, and postnatal health outcomes.19 To achieve this goal, Georgia legislators need to reconsider expanding Medicaid coverage, so pregnant women experiencing financial hardship can receive coverage for prenatal and postnatal care. Additionally, pregnant women in underserved, rural communities without health insurance should be given access to free or heavily subsidized quality maternal health care.12,35
4.3. Racism and Discrimination
Implicit bias, racism, and discrimination experienced by pregnant African American women at the hands of health care providers in Georgia need to be addressed through mandatory cultural competency training with a focus on equity and reproductive justice.19 Doing this will improve upon patient-provider interaction as well as patient satisfaction with the quality of care they receive.
5. Conclusion and Global Health Implications
Maternal mortality in Georgia is currently high. Expanding Medicaid coverage, reducing maternal health care disparities among the races, providing access to maternal care for women in rural areas, and training a culturally competent health workforce, will help to reduce Georgia’s high maternal mortality rate.
Acknowledgments:
None.
Compliance with Ethical Standards
Conflicts of Interest: The authors declare no competing interests.
Financial Disclosure: Nothing to declare.
Funding/Support: There was no funding for this study.
Ethics Approval: Not Applicable.
Disclaimer: None.
References
- Bill &Melinda Gates Foundation Goalkeepers. https: //www.gatesfoundation.org/goalkeepers/report/2021-report/progress-indicators/maternal-mortality/ Published 2021
- Road Map Towards the Implementation of the United Nations Millennium Declaration:Report of the Secretary-General. United Nations (UN) Secretary-General 2001
- [Google Scholar]
- Millennium Development Goals (MDGs) WHO. https: //www.who.int/news-room/fact-sheets/detail/millennium-development-goals-(mdgs) Published February 19, 2018
- [Google Scholar]
- The effect of socioeconomic status on all-cause maternal mortality:a nationwide population-based cohort study. Int J Environ Res Public Health. 2020;17(12):4606. doi:10.3390/ijerph17124606
- [Google Scholar]
- Maternal Mortality. UNICEF Data. https: //data.unicef.org/topic/maternal-health/maternal-mortality/ Published September 2019
- [Google Scholar]
- Centers for Disease Control and Prevention. https: //www.cdc.gov/reproductivehealth/maternal-mortality/pregnancy-mortality-surveillance-system.htm Published 2020
- Left Out:Barriers to Health Equity for Rural and Underserved Communities. https: //waysandmeans.house.gov/sites/democrats.waysandmeans.house.gov/files/documents/WMD%20Health%20Equity%20Report_07.2020_FINAL.pdf?utm_medium=email&utm_source=govdelivery Published July 2020
- In Georgia, the most dangerous state for pregnant women, policy change could save lives. Grady Newsource. https: //gradynewsource.uga.edu/in-georgia-the-most-dangerous-state-for-pregnant-women-policy-change-could-save-lives/ Published October 25, 2020
- [Google Scholar]
- Levels and Causes of Maternal Mortality and Morbidity. In: Black RE, Laxminarayan R, Temmerman M, Walker N, eds. Reproductive, Maternal, Newborn, and Child Health:Disease Control Priorities Vol 2. (3rd ed). Washington D.C: The International Bank for Reconstruction and Development/The World Bank Group; 2016.
- [Google Scholar]
- Maternal mortality and maternity care in the United States compared to 10 other developed countries. The Commonwealth Fund. https: //www.commonwealthfund.org/publications/issue-briefs/2020/nov/maternal-mortality-maternity-care-us-compared-10-countries Published November 18, 2020
- [Google Scholar]
- Maternal Mortality Factsheet 2012-2016. DPH Georgia. https: //dph.georgia.gov/maternal-mortality
- [Google Scholar]
- Maternal Health &Rights Initiative:Maternal Health in Georgia. Reproductive Rights. https: //reproductiverights.org/wp-content/uploads/2020/12/USPA-MHRI-GA-FS-Final-ForPrint-Pages.pdf Published August 2019
- [Google Scholar]
- Reducing Maternal Mortality in Georgia 2013 Case Review Update. DPH Georgia. https: //dph.georgia.gov/maternal-mortality Published November 2017
- [Google Scholar]
- Maternal Mortality Report 2014. DPH Georgia. https: //dph.georgia.gov/maternal-mortality Published March 2019
- [Google Scholar]
- Amnesty International. https: //www.amnestyusa.org/reports/deadly-delivery-the-maternal-health-care-crisis-in-the-usa/ Published May 7, 2011
- World Population Review. https: //worldpopulationreview.com/state-rankings/maternal-mortality-rate-by-state Published 2021
- Georgia Maternal Mortality 2012 Case Review. DPH Georgia. https: //dph.georgia.gov/maternal-mortality Published June 2015
- [Google Scholar]
- Georgia's maternal mortality rate for women of color is a big problem. Harris Lowry Manton. https: //www.hlmlawfirm.com/blog/georgias-maternal-mortality-rate-for-women-of-color-is-a-big-problem/ Published November 8, 2019
- [Google Scholar]
- Eliminating racial disparities in maternal and infant mortality:A comprehensive policy blueprint. American Progress. https: //www.americanprogress.org/issues/women/reports/2019/05/02/469186/eliminating-racial-disparities-maternal-infant-mortality/ Published May 2, 2019
- [Google Scholar]
- 2016 State of the state of maternal &infant health in Georgia. Healthy Mothers, Healthy Babies Coalition of Georgia. https: //hmhbga.org/wp-content/uploads/AM16-Gober-SOS-Presentation-09282016.pdf Published October 4, 2016
- [Google Scholar]
- Lowering preventable maternal deaths in rural Georgia. J Sci Policy Gov. 2020;17(2)
- [Google Scholar]
- OBGYN shortage in rural Georgia hampers access to care. Georgia Commission on Women. https: //www.gacommissiononwomen.org/obgyn-shortage-in-rural-georgia-hampers-access-to-care/ Published 2021
- [Google Scholar]
- The rural maternity crisis. The Commonwealth Fund. https: //www.commonwealthfund.org/blog/2019/rural-maternity-care-crisis Published August 15, 2019
- [Google Scholar]
- Health Care Workforce Data. Health Care Workforce Georgia. https: //healthcareworkforce.georgia.gov/physician-workforce-data
- [Google Scholar]
- Socioeconomic disparities in adverse birth outcomes:a systematic review. Am J Prev Med. 2010;39(3):263-272. doi:10.1016/j.amepre.2010.05.012
- [Google Scholar]
- Delays in receiving obstetric care and poor maternal outcomes:Results from a national multicentre cross-sectional study. BMC Pregnancy Childbirth. 2014;14(159) doi:10.1186/1471-2393-14-159
- [Google Scholar]
- delayed prenatal care and the risk of low birth weight delivery. J Community Health. 2003;28(3):199-208. doi:10.1023/a:1022908307844
- [Google Scholar]
- Kaiser Family Foundation (KFF). https: //www.kff.org/interactive/womens-health-profiles/ Published January 2021
- Working towards safe motherhood:delays and barriers to prenatal care for women in rural and peri-urban areas of Georgia. Matern Child Health J. 2016;20(7):1358-1365. doi:10.1007/s10995-016-1997-x
- [Google Scholar]
- African American Women and prenatal care:Perception of patient-provider interaction. West J Nurs Res. 2015;37(2):217-235. doi:10.1177/0193945914533747
- [Google Scholar]
- Maternal mortality among African American women in the state of Georgia, causes, policy, and ethical considerations. J Ga Public Health Assoc. 2020;8(1):14-22.
- [Google Scholar]
- 9 Stunning facts about black maternal mortality. Georgia Birth Advocacy Coalition. https: //georgiabirth.org/blogcontent/2019/9/12/ef3j8mnc46a1pnmun8a28ghwr3wmjy Published September 12, 2019
- [Google Scholar]
- Nurse-midwives in Georgia:value for Georgia citizens. Midwives of Georgia:The Georgia Affiliate of American College of Nurse Midwives. https: //www.senate.ga.gov/committees/Documents/GeorgiaACNMWomensHealthcareAdequacyCommitteeTestimony118.pdf
- [Google Scholar]
- Bridging the gaps in obstetric care:perspectives of service delivery providers on challenges and core components of care in rural Georgia. Matern Child Health J. 2016;20(7):1349-57. doi:10.1007/s10995-016-1995-z
- [Google Scholar]





