Translate this page into:
HIV Serodiscordance among Couples in Cameroon: Effects on Sexual and Reproductive Health
∗ Corresponding author email: nkenfou@yahoo.com
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Background and Objectives:
One of the main reasons for risky sexual behavior observed in HIV serodiscordant couples despite the knowledge of the partner’s status and counselling is childbearing. In Cameroon, there are few reports on HIV serodiscordant couples. This paper describes the influence of HIV on sexual relationships and decision to procreate.
Methods:
This cross-sectional study was conducted in five health centers. Self-administered questionnaire was used to collect social and demographic information, while semi-structured in-depth individual and couple interviews were used to explore sexual relationships and decisions about fatherhood/motherhood. Blood samples were collected from the couples and tested for HIV to confirm serodiscordance. The data were analyzed using the GraphPad Prism Version 6 software.
Results:
A total of 53/192 (27.6%) HIV serodiscordant couples participated in the study, and 18/74 (24.32%) HIV positive seroconcordant couples and 32/80 HIV negative seroconcordant couples were used as controls. The majority of HIV-positive partners in serodiscordant couples were women (30/53), of whom 25/30 were on antiretroviral therapy. Nearly half of the respondents (23 /53) reported tensions related to serodiscordance, shown by reduced sex frequency. The use of condoms was not systematically observed among seroconcordant and serodiscordant couples with respective proportions of 55.55% and 20.75% (p = 0.0086). Thirty seven out of 53 HIV serodiscordant couples wanted children, among them, seven couples did not have any and expressed their aspiration for parenthood despite fear of infecting one’s partner.
Conclusion and Global Health Implications:
Sexuality of serodiscordant couples as well as of HIV positive seroconcordant couples was affected by the presence of HIV/AIDS. The desire to procreate may lead couples to adopt risky sexual behaviors. It is important to define specific guidelines for serodiscordant couples in order to improve their sexual life and consequently enable them to procreate with minimal risk of infecting their partner and or to transmit the virus to their baby.
Keywords
HIV
Serodiscordance
Sexual health
Childbearing
Cameroon
Reproductive health
1. Introduction
HIV/AIDS continues to be a significant global health problem. Sub-Saharan Africa remains the most affected region with heterosexual intercourse being the main mode of HIV transmission. In the generalized epidemics in Africa, a large proportion of new HIV infections occur between couples in established relationships, making discordance a major contributor to the spread of HIV.1,2 Studies in Sub-Saharan Africa have shown a prevalence of HIV discordance among couples of 3-20% in the general population and 20-35% among couples with one partner seeking HIV care (serodiscordant).3-7
Although discordant couples account for a substantial proportion of new infections, neither program nor testing and counselling are geared for such couples.4 A key challenge for HIV-discordant couples is minimizing the risk of HIV transmission to their negative partner (s) and subsequently to any child conceived.8,9 This has led to increasing attention to, and advocacy for, the provision of reproductive assistance (such as sperm washing or in-vitro fertilization (IVF) to reduce the risks of HIV transmission and to satisfy the desire of motherhood/fatherhood with little or no risk.10 However, providing reproductive assistance to discordant couples is often not done in resource-constrained settings and there has been little policy and programmatic focus or guidance to ensure access to these sexual and reproductive health services within a human rights framework.11
In Cameroon, there are no specific strategies for monitoring serodiscordant couples, therefore national prevalence is not known, the difficulties faced by these couples on a daily basis and their attitudes towards sexual relations and the desire to procreate is not documented. What impact might HIV serodiscordance have on sexual relationships and decisions to have children or not remains largely unanswered. The objective of this work was to describe the influence of HIV on sexual relationships and assess the influence of serodiscordance on reproductive health among serodiscordant couples in Yaoundé-Cameroon.
2. Methods
This was a cross-sectional study conducted from September 2016 to December 2017 in five hospitals ((1) District Hospital of Efoulan, (2) Nkoldongo, (3) Biyem-Assi, (4) Cité-verte, Obala and (5) CMA of Nkomo). Serodiscordant couples consulting in these five hospitals constituted our study population. We included seroconcordant couples as controls, both HIV seronegative and HIV seropositive. The term couple refers to two persons living in a household and related by marriage or concubinage for a period of at least 12 months and having sex together. The medical records of HIV positive patients were reviewed at the HIV care units to identify serodiscordant and HIV positive seroconcordant couples, after which they were contacted by telephone. For those who consented, an appointment was made for interview and blood collection. HIV negative seroconcordant couples were recruited at the family planning services mainly during premarital counselling. The data were collected using a questionnaire offered to each partner separately and then together. The questionnaire was provided in French or English depending on participant preference. This questionnaire collected sociodemographic data, therapeutic follow-up and childbearing decision. Subsequently, blood was collected from both partners to confirm or refute their declared status. For this, HIV/AIDS test was carried out according to the national algorithm: a first rapid test using Determine® HIV1/2 (Abbott Diagnostic Division, Hoofddorp, The Netherlands) and a second confirmatory test with KHB® HIV (Shanghai Kehua Bio-engineering Co., Ltd., China). In case of discordant results to these two tests, the sample was re-analyzed by ELISA.
2.1. Study Variables
There were two study dependent variables were: (1) HIV status, and (2) Alteration of sexual relations: defined in this work by the frequency of sex before and after the knowledge of HIV status. Our covariable was the desire to procreate. Finally, our study independent variables were: antiretroviral treatment: to assess the risk of disease transmission; condom use, that is looking for risky sexual behaviors; marital status: defined in this work as married or cohabiting; gender, to know which gender was the most infected in a couple; sexual orientation: allows to identify the type of couple to be involved in the study; and fidelity: defined in this work by the number of sexual partners with whom the members of the couple have sexual relations.
2.2. Statistical Analysis
The data were analyzed using the Graph Pad Prism Version 6 software, San Diego California, USA. The χ2 or Fischer test was used to compare the qualitative variables among group (desire of childbearing and assisted procreation) and the Student’s t-test was used to compare the means (weekly frequency of sexual intercourse) with a significance level set at 5%. The study was approved by the National Research Ethics Committee for Human Health (N° 2016/04/ 758/ CE/CNERSH/SP). Before conducting the study, written informed consent was obtained and all identifying information (names, initials) were then omitted to ensure the confidentiality of participants.
3. Results
3.1. Social Demographic Characteristics
A total of 346 couples were contacted: 192 HIV serodiscordant; 74 HIV positive seroconcordant; and 80 HIV seronegative concordant couples. Fourteen couples were excluded: 7 serodiscordant couples (three for seroconversion of negative partner and 4 for insufficient data); one HIV positive seroconcordant; and another six HIV negative seroconcordant couples (for insufficient data). So, out of 192 serodiscordant couples, a total of 53 (27.6%) agreed to participate and were included in this study. In all, 18 HIV positive seroconcordant couples out of 74 (24.32%); and 32 out of 80 (40%) HIV negative seroconcordant couples took part in the study. All couples were monogamous and heterosexual. The average age of serodiscordant couples was 37 years (with extremes of 21-67 years) compared to 38 years for seroconcordant couples (with extremes of 16-58 years) and 32.6 years for HIV negative seroconcordant couples (with extremes 19-54 years).
Independently of the group considered (serodiscordant or seroconcordant), they were more married couples than cohabiting couples with an average marriage duration of 5.3 years in serodiscordant couples compared to 6.5 years in HIV positive seroconcordant couples (Table 1). Among serodiscordant couples, women were more infected 30/53 (56.60%) than men 23/53 (43.39%) although the difference was not significant (p = 0.1739).
| Variables | Serodiscordant couples (N = 53) | HIV positive seroconcordant couples (N = 18) | HIV negative seroconcordant couples (N= 32) | |
|---|---|---|---|---|
| Mean age (range) in years | 37 (21-67) | 38 (16-58) | 32.6 (21-55) | |
| Marital status | Married | 32 (60.37 %) | 10 (55.55 %) | 20 (62,5) |
| Concubinage | 21 (100 %) | 8 (100 %) | 12 (37,5) | |
| Means duration in years in current relationship | 5.3 (1-17) | 6.5 (3-20) | 3.8 (1-8) | |
| HIV negative who tested for HIV in the last 6 months | 13 / 53 (24.53 %) | ____ | 8 / 32 (25%) | |
| Couples in which women were HIV positive | 30/53 (56.60 %) | ______ | _____ | |
| HIV positive individuals on ARV treatment | 46/53 (86.79 %) | 18/18 (100 %) | _____ | |
| P value | 0.0225 | |||
| Means ARV treatment duration in years (range) | 1 (2 days – 14 years) | 2.3 (3 month- 10 years) | _____ | |
| Sex orientation of couple (Heterosexual) | 53/53 (100 %) | 18/18 (100 %) | 32 (100%) | |
| Sex with only one partner | 43/53 (81.13%) | 16/18 (88.88 %) | 25 (78.81%) | |
| P value | 0.637 | |||
| Desire of childbearing | 37 (69.8 %) | 13 (72.22 %) | _____ | |
| P value | 0.8465 | |||
Non applicable, or non-available
The HIV status declared by included participants were confirmed during the studies from rapid test. Those with discordant declared status were excluded. We observed in this study that HIV positive seroconcordant couples were more compliant for their ARVs treatment compared to serodiscordant couples (P = 0.0225). Sexual intercourse with a single partner existed in 81.13% (43/53) of serodiscordant couples versus 88.88% of HIV positive seroconcordant couples.
3.2. HIV-discordance, Intimacy and Sexual Relations
According to the survey, 23/53 partners said they had household tensions due to the discordance of HIV status, resulting in the reduction of sexual relations frequency with their partner. HIV positive seroconcordant couples as well as serodiscordant couples reported having sexual desire disorders with the proportion of 50% and 43.39 % without a significant difference (p= 0.39) between the two groups. But there was a significant difference (p=0.0001) when comparing these two types of couples with HIV negative seroconcordant couples. The systematic use of condoms (male only) was mainly reported among HIV positive seroconcordant couples (10/18) compared to serodiscordant couples (11/53) with respective proportions of 55.55% and 20.75% (p = 0.0086). Similarly, the condom was more often used in HIV positive seroconcordant couples (80%) (8/10) than in serodiscordant couples (60.38% (32/53) (p = 0.0086). Ten serodiscordant couples (18.86%) said they had never used condoms (Table 2).
| Variables | Serodiscordant couples (N = 53 couples) | HIV positive sero concordant couples (N = 18 couples) | HIV negative Seroconcordant couples (N=32) | |
|---|---|---|---|---|
| Tension because of discordant status | 23 / 53 (33.96%) | _____ | _____ | |
| Intimacy affected by HIV infection | 23/ 53 (43.39%) | 9/ 18 (50 %) | 0/32(0) | |
| P value | 0.0001 | |||
| Condom use | Never | 10/ 53 (18.86 %) | 0/ 18 (0.00 %) | _____ |
| Sometimes | 32/ 53 (60.37 %) | 08/ 18 (44.44 %) | _____ | |
| Always | 11/ 53 (20.75 %) | 10/ 18 (55.55 %) | _____ | |
| P value | 0.0086 | |||
Non applicable, or non-available
The weekly frequency of sexual relation was compared among serodiscordant couples before and after knowledge of their HIV status was ascertained (Figure 1). The result obtained showed a marked reduction in the frequency of sexual relation with a significant difference of p=0.0001 before and after HIV status knowledge. We further compared this weekly frequency in serodiscordant couples with that in HIV positive seroconcordant and HIV negative seroconcordant couples and found no difference between serodiscordant and HIV positive seroconcordant couples, but a significant difference was found between the above mentioned groups and HIV negative seroconcordant couples (P<0.0001 and p=0.0002 respectively).
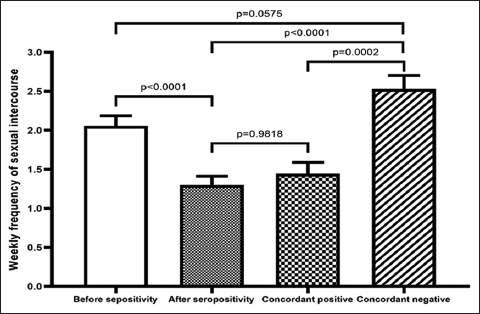
- Weekly frequency of sexual intercourse in serodiscordant, HIV positive seroconcordant an d HIV negative seroconcordant couples.
- Before and after seropositivity refer to sero-discordant couples; concordant positive refers to HIV Positive seroconcordant couples and concordant negative refers to HIV negative seroconcordant couples.
3.3. Desire for Procreation and Childbearing Strategies
In our study, HIV positive seroconcordant couples wanted children more than the serodiscordant couples without significant differences, with respective frequencies of 72.22% (13/18) and 69.8% (37/53) (Table 3). All childless couples (07/37) expressed a desire to meet a health professional for advice before any attempt to conceive was made. In all 5 hospitals where we had worked, the first condition required for procreation was to have an undetectable viral load. Then if the infected person was a woman, insemination of the sperm with a syringe after intercourse was proposed to the couple. In the case where the infected person was the male partner, the non HIV-infected (woman) was asked to take ARVs as pre and post exposure prophylactic therapy during the period of procreation attempts.
| Desire for childbearing | Serodiscordant couples (N = 53 couples) | HIV positive seroconcordant couples (N = 18 couples) |
|---|---|---|
| Did not want (additional) child/children | 16 (30.18 %) | 5 (27.77 %) |
| Wanted (additional) child/children | 37 (69.8 %) | 13 (72.22 %) |
| P value | 0.8465 | |
4. Discussion
Reproductive problems and solutions in serodiscordant and HIV positive seroconcordant couples are well-known and mastered by health staff in charge of the care of people living with HIV in Cameroon. However, this knowledge is not optimally put in practice as it is often during pregnancy that the couple is identified as serodiscordant or seroconcordant. Consequently, there is very little benefit from assisted reproduction, which increases the risks of contamination of the non-infected partner in serodiscordant couples and super-infection in seroconcordant couples. Yet both serodiscordant and HIV positive seroconcordant couples express the need for advice in order to have children.4 Artificial insemination and adoption are not common in the African socio-cultural context where biological procreation is a major way for parenthood for the couples.12 The desire for procreation, therefore, seems to be influenced by several actors or factors such as the health professional, the patient and the relationship between the patient and his/her partner with a great pressure from the society. This study identified the need to procreate in 69.8% of serodiscordant couples, close to that found by Beyeza-Kashesya et al. in 2010 in Uganda where 59% of serodiscordant couples wanted children. This desire to procreate is at the origin of the household tensions observed within couples due to the fear of infecting one’s partner.13 This points to the need to develop specific reproductive health strategies for both serodiscordant and HIV positive seroconcordant couples. These specific strategies may reduce these tensions among HIV infected concordant or serodiscordant couples. Assuring them of a safe reproductive solution will be very helpful. These strategies should start early enough with counseling (including sexual and reproductive health) when someone (male or female), married or not is diagnosed HIV positive. In Cameroon, the washing of semen for insemination is not carried out (technique advised when the man is the infected partner). However, insemination of semen collected in the condom is practiced if the infected partner is a woman. Nevertheless, there are no documents to assess this assisted reproduction, nor are there any studies on assisted reproduction in serodiscordant couples. In our study, of the various couples surveyed, 3 couples in which the woman was infected tried this technique with success.
Studies have shown that the correct use of condoms reduces the risk of HIV transmission by 80%.14 Condom use in a non-systematic way or never as declared by certain serodiscordant couples (79.24%) represents a major endogenous risk for the infection of the seronegative partner. This proportion of 79.24% is higher than that of Guira et al.15 where 59.5% of couples did not use condoms consistently, as well as those of Colman-Sarfo et al.16 where 40% did not use condoms. These findings suggest the need to define specific control strategies for this group in order to limit the spread of HIV infection because even in the case of undetectable viral load of the HIV virus, UNAIDS recommends the consistent use of condoms in serodiscordant couples.14 The main reason for not using condom was the need to procreate in 69.81% of cases, and this trend was observed in couples with no children as well as those with children. In this case, assisted procreation will then reduce this risk. Moreover, in the African sociocultural context, procreation is a social pressure in the life of a couple.17 Limited health assistance is therefore unfavorable to procreation without risk of HIV transmission, including STIs to seronegative partners in serodiscordant couples.18,19
4.1. Limitations
This study was carried out on 53 serodiscordant couples, which is a small sample size that does not allow us to generalize the results of this work to all serodiscordant couples. The couples were not followed up, therefore we do not know whether the tensions observed in the couples have decreased in the meantime and if couples have consulted professionals for more help and advice before trying to procreate.
4.2. Recommendations for Further Studies
For future studies it will be necessary to increase the sample size of the participants, to convince as many couples as possible to accept to be interviewed separately and then together, because many people refuse to be interviewed separately (in order to pretend to be trusted by their partners). It will also be important to follow-up with the couples as much as possible in order to fully appreciate the risk behaviors and the application of the different recommendations of the health personnel.
5. Conclusion and Global Health Implication
This work shows that the sexual relationships among serodiscordant couples as well as HIV positive seroconcordant couples is impacted by the presence of HIV infection. The desire to procreate leads couples to adopt risky sexual behaviors. It is, therefore, essential to define policies that identify and counsel serodiscordant couples by providing them with assisted procreation techniques in order to improve their sexual life and consequently enable them to parenthood with minimal risk of infecting their partners.
Acknowledgement:
We thank all participants who made this work possible, as well as all the health staff who helped us to recruit the participants.
Compliance with Ethical Standards
Conflicts of Interest: All the authors declare that they have no conflict of interest.
Funding/Support: The funding of the study was through personnal contributions of the authors.
Ethics Approval: written consent was obtained from all participants.
References
- Global report:UNAIDS report on the global AIDS epidemic 2009 2009
- HIV-1-discordant couples in sub-Saharan Africa:explanations and implications for high rates of discordancy. Current HIV Research. 2007;5(4):416-429.
- [Google Scholar]
- Who infects whom?HIV-1 concordance and discordance among migrant and non-migrant couples in South Africa. AIDS. 2003;17(15):2245-2252.
- [Google Scholar]
- Couple-centred testing and counselling for HIV serodiscordant heterosexual couples in sub-Saharan Africa. Reproductive Health Matters. 2008;16(32):151-161.
- [Google Scholar]
- Prevalence and pedictors of HIV sero-discordance among cohabiting couples tested in northern Tanzania. PanAfrican Medical Journal. 2015;22:275.
- [Google Scholar]
- Discordant Couples:HIV Infection Among Couples in Burkina Faso, Cameroon, Ghana, Kenya, and Tanzania (June 12006) World Bank Policy Research Working Paper No. 3956. Available at SSRN: https://ssrn.com/abstract=923263
- [Google Scholar]
- Prevalence of HIV sero_discordance among couples in Sub Saharan Africa 2019, systematic review and Meta analysis. International Journal of Women's Health Care. 2020;5(1):18-24.
- [Google Scholar]
- Childbearing Decision Making:A Qualitative Study of Women Living with HIV/AIDS in Southwest Nigeria. AIDS Research and Treatment. 2012;2012:478065.
- [Google Scholar]
- Reproduction decision making for couples affected by HIV:a review of the literature. Top HIV Medications. 2004;12(2):61-67.
- [Google Scholar]
- Reproductive options for HIV-serodiscordant couples. AIDS Review. 2006;8(3):158-170.
- [Google Scholar]
- International Community of Women Living with HA, Moody K, Global Network of People Living with HA Sexual and reproductive health services and HIV testing:perspectives and experiences of women and men living with HIV and AIDS. Reproductive Health Matters. 2007;15(29 Suppl):113-135.
- [Google Scholar]
- “Maybe his blood is still strong”:a qualitative study among HIV-sero-discordant couples on ART in rural Uganda. BioMed Central Public Health. 2012;12:801.
- [Google Scholar]
- My partner wants a child:a cross-sectional study of the determinants of the desire for children among mutually disclosed sero-discordant couples receiving care in Uganda. BMC Public Health. 2010;10:247.
- [Google Scholar]
- Global report:UNAIDS report on the global AIDS epidemic 2010
- Sexuality and risk for sexual transmission of HIV among serodiscordant couples in Ouagadougou Burkina Faso. Bulletin de la Sociétéde Pathologie Exotique. 2013;106(1):43-47.
- [Google Scholar]
- Challenges faced by HIV Positive Partners Living in Discordance with HIV Negative Partners:A Case Study of 37 Military Hospital. Clinical Research in HIV/ AIDS. 2017;4(2):1-11.
- [Google Scholar]
- Sexual relations and childbearing decisions of HIV-discordant couples:an exploratory study in SouthAfrica and Tanzania. italic>Reproductive Health Matters. 2011;19(37):184-193.
- [Google Scholar]
- Encouraging results despite complexity of multidisciplinary care of HIV-infected women using assisted reproduction techniques. Human Reproduction. 2005;20(11):3136-3140.
- [Google Scholar]
- Assisted reproduction techniques for HIV serodiscordant couples:18 months of experience. Human Reproduction. 2003;18(6):1244-1249.
- [Google Scholar]





