Translate this page into:
How much are Ecuadorians Willing to Pay to Reduce Maternal Mortality? Results from a Pilot Study on Contingent Valuation
Corresponding author email: mroldos@usfq.edu.ec/isabrld@aol.com
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Context:
There is an established association between the provision of health care services and maternal mortality. In Ecuador, little is known if the societal value is greater than the resources expended in preventive medicine.
Aims:
The purpose of this research is to investigate Ecuadorians’ willingness to pay to prevent maternal death and disabilities due to complications of care during childbirth in the context of universal coverage.
Methods and Materials:
The study elicited a “contingent” market on morbidity and mortality outcomes, specific to Ecuador’s epidemiologic profiles between a hypothetical market that included a 50% reduction in the risk of maternal mortality from 100 to 50 per 100,000, and a market that included a 50% reduction in the risk of maternal morbidity from 4,000 to 2,000 per 100,000.
Results:
The average amount participants are willing to pay (WTP) to prevent maternal mortality in the context of universal coverage, was $176 a year (95% CI=$172, $179). The unadjusted mean WTP for a reduction in the maternal morbidity risk was $135 (95% CI=$132, $139). Translated into Value of statistical Life, participant´s from this study valued the prevention of one statistical maternal death at USD $352,000.
Conclusion:
Results suggest that the costs of maternal care do not outweigh the benefit of prevention, and that Ecuadorians are willing to pay a significant amount to reduce the risk of maternal mortality.
Global Health Implications:
Reduction of maternal mortality will remain an important global developmental goal in the upcoming years. Having a monetary approximation on the value of these losses may have important implications in the allotting financial and technical resources to reduce it.
Keywords
Willingness to Pay
Maternal Mortality
Maternal Morbidity
Ecuador
Contingent Valuation
1. Introduction
Reducing population-level rates of maternal morbidity and mortality is an important developmental goal for many countries of the world. Ecuador´s maternal mortality is 87 deaths per 100,000 of live births.[1] The United Nations and governments around the world targeted a 75% reduction in maternal mortality by 2015, through two main strategies: (i) increasing antenatal care and[2] training of skilled birth attendants.[3] Ecuador’s specific strategy to meet this goal is the CONE program (Spanish acronym for Essential Obstetric and Neonatal Care). CONE is implemented through the public network of health services and private partnerships for patient referrals.[4] Thus, the implementation is segmented in a network of services. Maternal health specifically is delivered at the first level of care. According to the World Health Organization’s (WHO) “3 delays” model, maternal mortality can be attributable to inadequate health care provision.[5,6] In brief, the 3 delays framework provides an understanding of the factors that result in obstetric emergencies into the following delays: i) the women’s and family’s decision to seek health care; ii) issues related to accessing medical facilities such as transportation barriers, roads or others; and iii) the receipt of inadequate and appropriate care.[7]
Universal coverage is undoubtedly a critical component to reducing maternal mortality and improving the general health of a nation.[5] In Ecuador, universal coverage was first applied to maternal health care through the Free Maternity and Child Care Law (LMGAI). LMGAI was launched in 1994 and implemented through 2006. It was set to improve maternal and child health care outcomes of Ecuador’s most vulnerable populations.[8] However, even with the implementation of LFMC maternal mortality did not decrease, and maternal services remained partial. For example, around 28% of deliveries nationwide took place without the presence of a skilled birth attendant, of which, 75% occurred in rural areas.[9]
In Ecuador, little is known about how society values maternal health, particularly whether that societal value is greater than the resources expended for free access to services through the universal health care system. One way to assess the societal value given to the prevention of maternal deaths in particular, is to ask society about their willingness to pay (WTP) to prevent these deaths. This approach, called contingent valuation, is a survey-based method whereby respondents are asked to trade off mortality risk for wealth or income.[10] The resulting estimate, averaged across a population and multiplied times the risk reduction, represents the value that society places on preventing a statistical death. This estimate can then be used as the measure in a cost-benefit analysis where the costs of the free access to maternal health services through the universal healthcare system can be compared to the benefits of preventing maternal deaths.
The purpose of this research was to investigate Ecuadorians’ WTP to prevent maternal death and disabilities due to complications of care during childbirth in the context of universal coverage. To our knowledge, this is the first study to bring the question to individual citizens of how much they value universal coverage in relation to one of the most critical health problems in Ecuador. This question has rarely been studied recently and elsewhere. Evidence on WTP studies on alternatives to prenatal care was studied with a comparison between a general practitioner/midwife led care versus obstetrician led care with no significant differences between them and a WTP of 2500 Euros,[11] while in Tanzania a group of researchers investigated the willingness of patients and households to pay for rural district hospital services in the north-western region with significant differences between outpatient services and in-patient services ranging from 358 Tsd per a one day admission day to 2218 Tsd for an hernia operation.[12] In the United States a WTP study was used to inform The United States Preventive Services Task Force on the frequency and WTP of pregnant women to receive a sonogram during their pregnancy. Their results indicates that most women want a sonogram during pregnancy, and many are willing to pay for the examination.[13]
Ecuador is a country of 16,144,000 people with close to equal distribution between men and women, with a live expectancy of 74 years for men and 79 years for women and a total expenditure on health per capita of 1,040 USD.[1] Under-five infant mortality is 57 live births per 1,000 with other and congenital causes as main causes, and main causes of adults deaths as Ischaemic heart disease, stroke and lower respiratory diseases.[1]
The results of this study have the potential to influence future assessments of the returns on investment in the Ecuadorian healthcare infrastructure to prevent maternal mortality.
2. Methodology
This study is part of a research endeavor to study intentional and unintentional violence, and compared methods and results in a sample in the United States in Georgia, and another sample in Ecuador. The parent project estimated the monetary value that individuals place on maternal mortality and child maltreatment preventive programs. The results of the societal WTP to prevent child maltreatment was published elsewhere.[14] Specifically, this paper presents the results of the contingent valuation to prevent maternal mortality and morbidity through universal coverage in Ecuador.
2.1. Data collection
Data collection was conducted between February and June 2012 with a convenience sample of adult residents living in the two largest cities in Ecuador, Quito and Guayaquil. The only inclusion criteria for this study was being older than 18 years of age. Study participants were recruited in utility centers where Ecuadorians pay their utility bills such as water, electricity and municipality services located at shopping malls, community centers, and small shops. The study obtained University of San Francisco de Quito and The University of Georgia’s Institutional Review Board approvals. Each survey took between 15 and 20 minutes, and participants received a $15 phone card to compensate for their time.
The study sample was randomly split to address separately the question on the value placed on reduction of maternal mortality and morbidity, between a hypothetical market that included a 50% reduction in the risk of maternal mortality from 100 to 50 per 100,000, and a market that included a 50% reduction in the risk of maternal morbidity from 4,000 to 2,000 per 100,000. The survey included verbal protocols to establish the “contingent” market which included maternal and infant data on morbidity and mortality outcomes, specific to Ecuador’s epidemiologic profiles.
Following research by Corso et al 2011 and best practices to represent the denominator neglected, we provided a visual aid (a laminated page of 100,000 dots) to illustrate the hypothetical population, with dots highlighted in red to indicate those at risk of maternal death.[15] Next, participants were asked to respond to questions related to the scripts: “Yes they would pay for the program” or “No they would not pay for the program” based on a randomly selected WTP value (between $10 and $300 in Ecuador US$). Randomization was accomplished by having the bid values in a bag and randomly selecting a paper with a bid value. If the response was “No,” a second question was posed using a WTP value that was $25 lower than the initial bid; if the response was “Yes,” then the second question posed was $25 higher than the initial bid. This process was done one time.
After completing the contingent valuation task by completing the survey described above, respondents were asked to rate their confidence in their ability to pay this amount if the opportunity arose.
The study used a dichotomous approach to elicit WTP values in contingent valuation surveys,[10] and tested respondents WTP based on payment mechanism. To do this, half of the sample was asked about WTP in annual taxes and the other half was asked about WTP in annual donations. The study wanted to measure government confidence in the provision of services versus receiving services from a private sector.
We also collected data on participants’ confidence in their response using a 5 Likert scale that measured “very confident”, “confident”, “neutral”, “somewhat confident” and “not at all confident”, and several socio-demographic characteristics that have been shown to influence WTP in other studies, including age, gender, race/ethnicity, years of education, marital status (categorized in single, married, divorced and widowed), income, and self-reported general health (Measured using SF-12 health related quality of life question: “In general, how would you rate your health”).
2.2. Data analysis
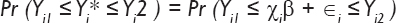
For the data analysis we assumed a WTP value Yi * that is represented by the model
Yi * = χiβ + ∈i, where the εi are normally distributed with a mean zero and the Xi represent individual respondent characteristics. While Yi * was not directly observed for respondent i, it is known to lie in the interval [Yi1, Yi2] based on responses elicited in the contingent valuation survey and the corresponding likelihood contribution is:
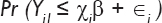
When an upper bound is unknown (right-censored data) the likelihood contribution is:
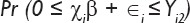
When a lower bound is unknown (left-censored data), we set a lower bound of zero, and the likelihood contribution is:
The maximum likelihood function was estimated with interval regression using the intreg command in Stata version 13 (Stata Corp, College Station, TX, USA).
The primary independent variable of interest for the model was the indicator of whether the respondent was asked to respond to a question about mortality or morbidity. Mortality and Morbidity independent analysis was done for each independent variable At the beginning of the model building process, we decided to include age and gender in the model regardless of significance or model fit. To build the model, we used a forward stepwise procedure with the potential independent variables, including a variable if it significantly improved model fit as measured by the Akaike Information Criterion (AIC).[16] Use of the AIC allows for a trade-off between improvements in the goodness of fit and increasing complexity from adding additional independent variables.[17] We estimated the mean WTP value for both the mortality and morbidity samples using the final model. Bootstrapped standard errors (1,000 replications) were used to calculate bias-corrected 95% confidence intervals (CIs) on the mean WTP.[18]
3. Results
The study’s goal was to reach a sample of 400 people, of which 99% agreed to participate. Those that declined to participate did so because of lack of time and uninterested to participate. The final study sample consisted of a total of n=398 people, n=223 who were asked to respond to a risk reduction in maternal mortality risk, and n=175 who were asked to respond to a risk reduction in maternal morbidity risk. A description of study participants is presented in Table 1.
| Variable | Maternal mortality Mean (SD) or % N=223 | Maternal morbidity Mean (SD) or % N=175 | Difference |
|---|---|---|---|
| Age, years | 32.9 (11.8) | 33.1 (11.3) | Ns |
| Female | 42.6 | 48.6 | Ns |
| Race/Ethnicity | Ns | ||
| Mestizo | 83.0 | 85.1 | |
| White | 10.3 | 10.3 | |
| Black | 4.5 | 4.0 | |
| Other | 2.2 | 0.6 | |
| Single | 53.8 | 52.6 | Ns |
| Years of education | 13.4 (3.5) | 13.9 (3.4) | Ns |
| Poor healtha | 20.6 | 22.9 | Ns |
| Household income, $ | p<0.01 | ||
| ≤$10 000 | 48.0 | 69.1 | |
| >10 000 | 10.4 | 22.3 | |
| Missing | 41.4 | 8.6 | |
| Confident in ability to payb | 50.1 | 58.3 | Ns |
a Measured using SF12 question: In general, how would you rate your health,
The study participant’s descriptive characteristics included age, gender, race, marital status, years of accumulative education, perception of health status and annual income. There was no-significant difference between the two sub-samples (mortality and morbidity) and the only variable statistically significantly different between the two subsample was income.
Less than 20% responded “No” to either bid amount presented, 100% of participants agreed to the initial bid of $10, 84% to the initial bid of $50 dollars, and 46% to the bid of $100, and decreasing thereafter. Table 2 presents the results of the interval regression for reducing the risk of maternal morbidity or mortality, including only those covariates that were significant in the model.
| Variable | Coefficient | Standard error | P |
|---|---|---|---|
| Mortality1 | 45.6 | 11.0 | <0.001 |
| Age | 0.2 | 0.5 | ns |
| Female | 18.8 | 10.7 | ns |
| Mestizo | 32.0 | 13.8 | 0.021 |
| Years of education | 4.9 | 1.5 | 0.001 |
| Confidence in ability to pay | 45.9 | 11.4 | <0.001 |
| Constant | 64.7 | 29.1 | 0.026 |
A scope test suggested a significant difference between the valuation of morbidity and mortality. Economic theory suggests willingness-to-pay (WTP) should be significantly higher for a higher risk than for a lower risk. Our scope test determined that people were willing to pay more to reduce the risk of mortality than for morbidity. Overall, this model with covariates was statistically significant at the base model without any covariates. However, the overall model fit was poor based on the R2 value of 0.102, indicating that very little of the variance in the estimates were actually explained by the model. However, income, and the higher the income the higher one should expect WTP to be, was statistically significant in the model (p <0.05).
Table 3 shows average amount participants were willing to pay to prevent maternal mortality in the context of universal coverage, from a model with no other covariates. The mean estimated WTP was $176 (95% CI=$172, $179). The unadjusted mean WTP for a reduction in the maternal morbidity risk was $135 (95% CI=$132, $139).
| Outcome variable | Mean WTP | 95% CI |
|---|---|---|
| Maternal mortality (N=223) | $176 | $172, $179 |
Value of statistical life (VSL) is a summary measure of the willingness-to-pay for a mortality risk reduction, and a key input into the calculation of the benefits of policies or projects that affect mortality risk or excess death. The mortality benefits are computed as the expected number of deaths avoided by the policy change times the average WTP value, and is therefore defined as the rate at which the people are prepared to trade off income for risk reduction. Translated into Value of statistical Life, the WTP estimates produced in this study suggest that participants valued the prevention of one statistical maternal death at USD $352,000. There is no need to convert this finding to international dollars since Ecuador dollarized the economy in 1999.
4. Discussion
In this study, respondents were willing to pay a considerable amount of money, US$176 per year, to prevent maternal mortality, or $132 to prevent maternal morbidity risk. The scope test performed confirmed people’s willingness to pay more to reduce the risk of mortality than for morbidity. This results may be related to a national campaign to reduce maternal mortality by the Ministry of Health (MOH) and the global pressure to meet the United Nations Millennium Developmental Goals.
Despite the MOH’s attempt for universal coverage, out of pocket per person health expenditures (% of private expenditure on health) in Ecuador is at US$83.68 per month in 2011, according to the World Bank,[19] representing close to 20% of Ecuadorian’s disposable income. The total of national expenditures in maternal health care services is difficult to estimate given the multiple programs, levels of services and delivery partners. Data from the Free Maternity and Child Care Law (LMGAI) program indicate that the central government invested close to 29 million dollars a year to provide the following services: prenatal check-ups, care for normal and at-risk births, cesarean sections, post-partum care, obstetric emergencies, intra-family violence prevention, laboratory services and medicines, in addition to prevention programs in family planning methods, and HIV. In 2012, the LMGAI reported covering the costs of 315,000 births, with an average cost of close to $USD 100 per birth.[20]
Despite the monies invested in the provision of maternal and infant health care services these are not enough to prevent maternal mortality. Among efforts, the MOH must strengthen the Directorate of Health Quality Services to improve the delivery of maternal health services and reduce the number of maternal deaths. To do so, it need to prioritize the re-assignment of functions of community-centered committees to study maternal deaths in each territorial zone of the country. The results of this study suggest that the costs of maternal care do not outweigh the benefit of prevention, and that Ecuadorians are willing to pay a significant amount to reduce the risk of maternal mortality.
5. Conclusions and Global Health Implications
There are several limitations of this study to consider. First, the data were collected from a convenience sample from 2 large urban cities, which may not be representative of the total population of Ecuador and the rural and ethnic diversity of the country. However, this sample does include a majority of lower SES people and include the two largest cities of the country that represent close to 40% of the population of the country and therefore the WTP estimates can be a considered a lower bound estimate of society’s true WTP to prevent maternal mortality. The second limitation is common to many CV studies, where our initial bid can have a biased because of the hypothetical nature of the questioning. However, these biases were partially controlled by randomizing participants to the initial bid values and using dichotomous choice responses. With such a small sample, we were not able to test for validity of responses in a scope test, that is determining whether WTP varied by changes in risk reduction.
In sum, as financial resources become more restrictive and public health threats are at an all-time high, economic evaluations can bring information and analysis to help decision makers make the necessary comparisons and make informed decisions. The results from this study puts a monetary value to an intangible loss, a mother, through the estimate of her value of statistical life, but it also brings an estimate of how much an average citizen values maternal mortality. This estimate can have a potential implication on how low-income countries, such as Ecuador, collect monies from citizens to pay for public health and prevention programs. This study suggests that everyone has a role to prevent maternal mortality and the economic burden of prevention strategies and adequate health services can be shared among all Ecuadorians. What are the implications of the study findings for other countries in the region?
Acknowledgements
The research was made possible thanks to the support from The Compton Foundation/Population Reference Bureau International fellowship in Population, Environment and Human Security, and The University of Georgia, Economic Evaluation Research Group at the School of Public Health.
Compliance with Ethical Standards
Conflict of Interest: Authors declare they have no conflicts of interest.
Ethical Approval: Study was approved by two Institutional Review Boards.
Informed Consent: Informed consent was obtained from the study participants.
REFERENCES
- World Health Organization, World Health Observatory data 2015
- PATH e Instituto de Investigación Nutricional (IIN), Desarrollo de una estrategia para introducir la vacuna contra el Virus del Papiloma Humano (VPH) en el PerúResultados de la Investigación Formativa del Proyecto Vacunas contra el VPH: Evidencias para Impacto. PATH: Seattle, WA; 2009.
- United Nations, The Millenium Development Goals Report. 2015.
- Ministerio de Salud, Manual del Modelo de Atención Integral de Salud - MAIS, Subsecretaría Nacional de Gobernanza de la Salud Pública, Editor 2012
- An Introduction to Maternal Mortality. Reviews in Obstetrics and Gynecology. 2008;1(2):77-81.
- [Google Scholar]
- United Nations Population Fund, Maternal Mortality Update 2002: A Focus on Emergency Obstetric Care. New York: UNFPA; 2003.
- Applying the lessons of maternal mortality reduction to global emergency health. Bulletin of the World Health Organization. 2015;93(417)
- [Google Scholar]
- La Ley de Maternidad Gratuita y Atención a la Infancia (LMGYAI) en el Ecuador. Informe LACRSS. No. 62., Agencia de los Estados Unidos para el Desarrollo Internacional (USAID), Editor. Quality Assurance Project 2005
- [Google Scholar]
- Consejo Nacional de Salud and Ministerio de Salud Publica, Política de Salud y Derechos Sexuales y Reproductivos. 2007.
- Using surveys to value public goods: The contingent valuation method. Washington, DC: Resources for the Future; 1989.
- Using willingness to pay to value alternative models of antenatal care. Social Science & Medicine. 1997;44(3):371-380.
- [Google Scholar]
- Willingness to pay for district hospital services in rural Tanzania. Health Policy and Planning. 1996;11(4):428-437.
- [Google Scholar]
- The maternal perspective on prenatal ultrasound. Journal of Family Practice. 2000;49(7):601.
- [Google Scholar]
- A comparison of willingness to pay to prevent child maltreatment deaths in Ecuador and the United States. Injury Prevention. 2012;18(Suppl 1):A181.
- [Google Scholar]
- Using Visual Aids to Improve Communication of Risks about Health: A Review. The Scientific World Journal 2012 Article ID 562637
- [Google Scholar]
- A new look at the statistical model identification. Automatic Control, IEEE Transactions on. 1974;19(6):716.
- [Google Scholar]
- Model selection and multimodel inference: a practical information-theoretic approach. Springer Science &Business Media; 2002.
- [Google Scholar]
- Better bootstrap confidence intervals. Journal of the American statistical Association. 1987;82(397):171.
- [Google Scholar]
- Trading Economics. Out-of-pocket health expenditure (% of private expenditure on health) in Ecuador 2014
- Tablas_Número de Prestaciones y Valoraciones_Maternidad Gratuita y Hospitales. 2012
- [Google Scholar]





