Translate this page into:
Strengthening Maternal Death Surveillance Systems for Evidence-Based Decision Making in Sub-Saharan Africa: The Case of the Center Region in Cameroon
*Corresponding author email: anasta_siauk@yahoo.com
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Background:
The article seeks to document the experience of implementing Maternal Death Surveillance and Response (MDSR) in the Center Region of Cameroon. The paper raises awareness on the need for implementing MDSR, shares progress and lessons learned and reflects on the implications for public health practice.
Methods:
A desk research involving the collection and analysis of secondary data using tables with specific themes in excel, following the review of existing resources at the Regional Delegation of Public Health-Center from the year 2016 to 2019.
Results:
The findings depict the existence of MDSR policies and sub-regional committees. Although, the number of regional maternal death notifications increased from 19 to 188 deaths between 2016 and 2019, the implementation of death review recommendations was only estimated at 10% in 2019. While 66% of deaths occurred in Yaoundé, 72% of these were deaths reported to have occurred in tertiary institutions out of which 75% were attributed to late referrals. Hemorrhage constituted 70/144 (48.6%) of the known direct causes of death. Maternal death related co-factors such as the use of partograph during labor had a high non-response rate (84%) and represents a weakness in the data set.
Conclusion and Global Health Implications:
Across the board, stakeholder engagement towards MDSR was increased through continuous awareness-raising, dissemination of surveillance tools, the institutionalization of the District Health Information Software (DHIS 2) and the “No Name No Blame” policy. However, the reporting and investigation of deaths for informed decisions remain a daunting challenge. For a resource-scarce setting with limited access to blood banks, the application of life-saving cost-effective interventions such as the use of partographs and the institution of a functional referral system among health units is likely to curb the occurrence of deaths from hemorrhage and other underlying causes. The success of these will require a robust strengthening of the health system.
Keywords
Maternal Death
MDSR
Partograph
Referral System
Center Region
Cameroon
1. Introduction
1.1. Background
Maternal death occurs when a woman dies while pregnant or within 42 days after giving birth, irrespective of the duration and site of the pregnancy, from any cause related to or aggravated by the pregnancy or its management, but not from accidental or incidental causes.1 There is a global priority to curb the maternal mortality ratio to the target of 70 maternal deaths per 100,000 live births as established by the 2030 Agenda.2
Cameroon is a country in Sub-Saharan Africa with a population estimated at 22 million inhabitants residing in 10 administrative regions.3 The Center Region is the second most populated with over 4 million inhabitants.3 While an estimate of 71% of these inhabitants reside in the capital city of Yaoundé, women of reproductive age (15-49 years) constitute about 25% of the total regional population.4 The Maternal Mortality Ratio (MMR) was estimated at 782 deaths per 100,000 live births in 2011,5 with a 48% reduction between 2011 and 2018 (406 deaths per 100,000 live births).6 Thus, achieving the national target of 140 deaths per 100,000 live births in 2030 will require strong political commitment and a robust strengthening of the health system.
Over the years, the government and its partners have implemented strategies towards reducing preventable maternal and perinatal deaths. One of these was the establishment of the Maternal and Perinatal Death Surveillance and Response System (MPDSR) in 2014, with the notification of maternal and perinatal deaths being mandatory. According to the National Strategic Plan to reduce maternal and child mortality, Cameroon seeks to curb the maternal mortality ratio by 6.2% annually.7 However, the shortcoming of the existing monitoring and evaluation system is a challenge for achieving this objective.
1.2. Problem Statement and Justification
Accurate and timely information on health intervention coverage, quality, and equity, is the foundation for public health practice. This is because good measurement facilitates accountability for both national and international bodies, as it improves the ability to monitor progress towards set objectives. The global impetus to improve Maternal, Neonatal and Child Health (MNCH) as defined by the 2030 sustainable development goals (SDGs) requires not only a rigorous measurement system but also accountability for actions taken to prevent deaths and their impact on other maternal and child health outcomes.8 In Cameroon, a lot of work has been done in Maternal deaths surveillance, however, little has been documented for the purpose of disseminating the progress and lessons learned. Previous research has focused on clinical reviews and the identification of clinical factors associated with deaths,9-11 with limited information on maternal death surveillance activities especially those conducted at sub-national levels (regional and district).12This article, therefore, seeks to describe the implementation of Maternal death surveillance and Response (MDSR) system in the Center Region, summarizing the key achievements, challenges, lessons learned, and proposing recommendations for informed decision making and health system strengthening.
It describes MDSR activities conducted from 2016 to 2019 through a presentation of findings from the secondary analysis of existing MDSR activity reports in the Center Region.
2. Methods
The study was a desk research and consisted of collecting and analyzing secondary data following a review of existing resources at the Regional Delegation of Public Health from the year 2016 to 2019. The Regional Delegation of Public Health is a subnational health care department and an epicenter for data collection, analysis for informed decision making, and the coordination of public health interventions. Within the framework of maternal death surveillance and response activities, data transmission follows two channels. The first is using an electronic system called District Health Information Software (version 2.36) for the notification of deaths at the facility and community level by health workers in primary health care institutions. The second channel is through the transmission of hard copies of individual death reports (notification forms, investigation forms and the deaths review reports) by the district health officers.
A data entry sheet was created using Microsoft Excel 365 to enter information from the death reports. The variables abstracted from these included the demographic variables, place of death, cause of death and their co-factors. The reporting of these variables was however not available for most death reports. Thus, to ensure the validity of death reports from District Health Information Software (DHIS2) and complement the missing information in the audit reports, the regional staff in collaboration with the district health officials conducted a data triangulation exercise with the MDSR focal persons at the level of the notifying health facilities through phone interviews or site visits whenever possible.
Furthermore, as per the WHO guidelines for monitoring MDSR indicators,13 institutional reports such as the MDSR strategic plan, regional MDSR reports, and others were reviewed to understand the policies and frameworks put in place for MDSR activities at the regional level. The key MDSR surveillance indicators assessed were the availability of MDSR policies, the existence of functional review committees at regional and sub-regional levels, the cascade of deaths investigated and reviewed across the years as well as key interventions put in place to strengthen the surveillance system. The data were summarized using frequencies and proportions for the variables assessed.
3. Results
3.1. MDSR Policies and Indicators
In Cameroon, there is a ministerial text which has mandated the notification of deaths within 24 hours at the level of the health facility and the creation of district review committees. Table 1 presents an evaluation of the MDSR policies and the key surveillance indicators for the Center Region. As of 2019, the findings from the document review revealed the existence of MDSR policies, regional review committees and the availability of annual regional reports with recommendations although there was no documented evidence of a results-based framework for the implementation of these recommendations. Same-day death notification and the implementation of review recommendations were both estimated at 10%. There was a documented achievement of 100% for MDSR capacity building of district health officials. Despite, the observed progress from previous years, only 50% of districts had a functional review committee, which organized and shared review reports with the Regional Delegation of Public Health.
| Presence of MDSR Indicators | 2017 | 2018 | 2019 |
|---|---|---|---|
| Availability of MDSR policies for notification, investigation, and review of maternal deaths | Yes | Yes | Yes |
| Existence of sub-national review committee- Regional level | No | Yes | Yes |
| Production of regional annual reports and recommendations | No | Yes | Yes |
| Existence of a results-based framework for the implementation of regional recommendations | No | No | No |
| Existence of a sub-regional review committee in the 30 health districts of the region | No | Partial | Yes |
| Proportion of deaths notified to the regional office within 24 hours of its occurrence | NA | NA | 10% |
| Proportion of death-linked recommendations implemented | NA | NA | 10% |
| Proportion of districts with at least two surveillance officers trained in MDSR | 37% | 40% | 100% |
| Proportion of districts with MDSR action plans | 33% | 40% | 80% |
| Proportion of districts that have organized a death review with reports submitted to the region | 17% | 20% | 50% |
NA= Not Available
Across the board, as depicted by the MDSR annual cascade (Figure 1), there has been an increase in the death reports submitted to the region from the districts and health facilities for informed decision-making. The number of maternal deaths notified increased from 19 to 188 between 2016 and 2019. A similar trend was observed for the number of deaths investigated and reviewed (Figure 1).

- Distribution of maternal death surveillance cascade indicators per annum (2016 to 2019)
3.2. MDSR Data Quality Assessment
Of the 188 deaths assessed, the average non-response rate was estimated at 53.3%. As presented in Table 2, the non-response rate to questions related to some key variables assessed such as the use of partograph (84%), level of education (71%), professional status (62%) and marital status (61%) was high.
| MSDR Variable | Non-Response Counts (N) | Proportion (%) |
|---|---|---|
| Period of death | 111 | 59 |
| Place of death | 96 | 51 |
| Status of arrival at the hospital | 74 | 44 |
| Mode of Delivery | 110 | 58 |
| Use of partograph | 159 | 84 |
| Professional status | 116 | 62 |
| Age | 35 | 19 |
| Gravida | 46 | 24 |
| Marital Status | 115 | 61 |
| Level of Education | 134 | 71 |
3.3. Analysis of Death Reports
3.3.1. Demographic Characteristics
Out of the 188 deaths reported during the year 2019, 30% and 40% of these were of the age groups 16-25 years and 26-35 years respectively (Table 3). Fifty percent (50%) of these were pregnant women of gravida one to four. Only 12% of the deaths were identified as married, while 26% and 6% of these were respectively unemployed and involved in small trade. A high non-response rate was, however, noted for the following variables: marital status (61%), level of education (71%) and professional status (62%).
| Variable | Number of deaths | Proportion (%) |
|---|---|---|
| Age at death (years) | ||
| No response | 35 | 19 |
| 16-25 | 57 | 30 |
| 26-35 | 76 | 40 |
| 36-45 | 19 | 10 |
| 46-55 | 1 | 1 |
| Gravida | ||
| No Response | 46 | 24 |
| 1-4 | 94 | 50 |
| 5-8 | 43 | 23 |
| 9-12 | 5 | 3 |
| Marital status | ||
| No Response | 115 | 61 |
| Unmarried | 51 | 27 |
| Married | 22 | 12 |
| Level of education | ||
| Not Educated | 6 | 3 |
| Primary | 17 | 9 |
| Secondary | 24 | 13 |
| Tertiary | 7 | 4 |
| No Response | 134 | 71 |
| Profession | ||
| No response | 116 | 62 |
| Petty trade* | 12 | 6 |
| Unemployed** | 49 | 26 |
| Worker*** | 11 | 6 |
3.3.2. Place of Death/Status Upon Arrival at Hospital
A total of 37% of the maternal deaths occurred in the facility; 15% were on transit; 5% were deaths reported from the community and 51% with no responses. Out of the 188 deaths reported during the year 2019, 66% (125/188) occurred in the city of Yaoundé from which a total of 77% (90/125) were registered by the tertiary institutions (Figure 2). Among the deaths reported by these tertiary institutions, 75% were attributed to late referrals for proper care and management (Figure 2). The results from the review provide evidence of women who arrived at the hospital in a critical state (39/188 deaths) or arrived already dead (30/188 deaths). Some cited reasons for the late referrals are listed as follows; limited health worker knowledge on the identification of danger signs and timely referral, limited knowledge on where to seek proper care by a health worker and communities (21% (40/188) of deaths were reported to have visited more than two health facilities in search of proper care), and the financial limitations which sometimes resulted to a denial of referral by the family due to the fear of high out of pocket expenditures at the referred institutions.14,15
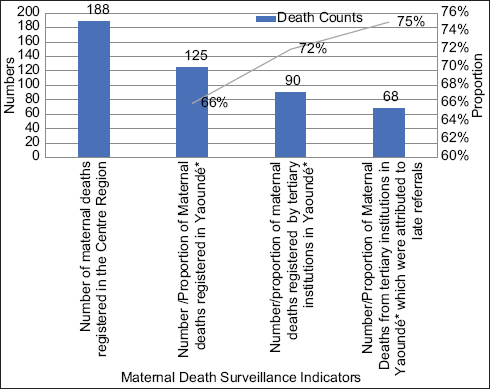
- Cascade of key maternal deaths surveillance indicators in the Yaoundé Center Region and attributes to late referrals in 2019
- *Capital of the Center Region. It covers 6 out of the 30 health districts in the region.
3.3.3. Period of Maternal Deaths
The findings reveal that 32% of the deaths occurred during the postpartum period. There was however no information to distinguish between the immediate postpartum and the late postpartum. Fifty-four percent (54%) of the deaths notified had no response concerning the period of occurrence of deaths.
3.3.4. Direct and Indirect Cause of Deaths
With respect to Figure 3, the causes of maternal deaths were hemorrhage (37%), pre-eclampsia/eclampsia (12%), HIV/AIDS (9%). Other causes included abortion (6%), severe anemia (6%), septicemia (2%). Uterine rupture accounted for 24% (17/70) of the documented causes of hemorrhage.
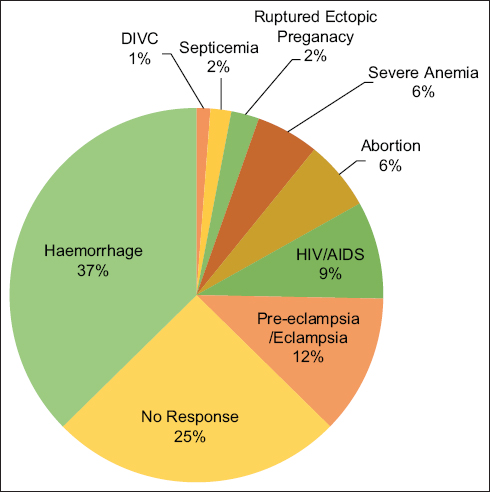
- Direct/indirect causes of Maternal deaths
4. Discussion
The discussion of the result is presented in three sections. Section 4.1. summarizes progress with the surveillance system. Section 4.2. explores the lessons learned from the implementation of the surveillance system. Section 4.3. examines some of the characteristics and the causes of maternal deaths registered in the year 2019.
4.1. Progress with the Surveillance System
As shown in Table 1, the Center Region has made progress towards the implementation of the MDSR policies. There are 30 subregional committees with a least two Health officials trained on implementing MDSR. This has contributed to the progress in the proportion of death reviews from 17% in 2017 to 50% in 2019. Over the years from 2016 to 2019, there was an observed progress in the practice of death notifications, death investigations and reviews (Figure 1). This improvement in the indicator is attributed to the capacity-building exercise conducted during the year 2019 across districts, health facilities and communities with financial support from the United Nations Fund for Population (UNFPA). Other factors, which were identified as key contributors to this are described below.
-
Engagement of regional stakeholders to take forward the agenda of ending the occurrence of preventable deaths. The MDSR supervision activities which were led by the Regional Delegate of Public Health and the reproductive health focal persons, spurred the uptake of MDSR activities at the operational level (health facilities).
-
Increased awareness raising/sensitization on MDSR through social media and among community health workers.
-
Development and the dissemination of surveillance tools (physical and electronic copies) at all levels of the health pyramid.
-
Integration of maternal death surveillance with other regional data quality assessment processes to capture and review unreported deaths.
-
The organization of proper investigations and verbal autopsies were also an asset for guiding decision-making during the clinical death reviews.
-
The use of electronic reporting systems (District Health Information Software). This has facilitated data visibility, investigation and review of deaths reported at the level of the health facility. Prior to this, most deaths were unreported due to the lack of a system that captures the deaths and does prompt verification monthly.
-
Use of concomitant reporting tools for surveillance. For example, WhatsApp forums and platforms were created to ensure timely notifications and orientations to respond in the hard-to-reach areas. WhatsApp discussion platforms were created across the 30 health districts in the region. This also enhanced the collaboration among the health facilities in the management of essential obstetrical commodities. It also enhanced the coordination of MDSR activities between the region, districts, and health facilities.
-
Development of a regional action plan and MDSR monitoring and evaluation framework to support the follow-up of MDSR activities in the region. Prior to the year 2019, there was no regional action plan nor monitoring and evaluation framework.
4.2. Lessons Learned from The Implementation of MDSR in the Center Region
The long-term goal of an MDSR system is to ensure the timely identification, investigation, and review of the deaths to orient evidence-based decision-making for the prevention of deaths from similar causes. The assessment of MDSR reports identified some challenges and lessons for future consideration as described below.
MDSR data quality and challenges for inferential statistics
MDSR can guide change if its monitoring and evaluation framework is built on timely, complete, and reliable data. Despite the progress with maternal death notifications, the data, however, is a shortfall compared to the expected deaths in the region. The reason for this is because the current health information system has limitations with capturing deaths occurring in the community (outside the health facilities).
In addition, there are challenges with same-day notification and the timely submission of death reports. One of the guiding principles of the MDSR monitoring system is to ensure the timely notification and prompt action for the prevention of deaths from similar causes.13 While no information on this was found for the previous years, an assessment of the 2019 data reports found that only 10% of the 188 deaths were notified on the same day (Table 1). Annual sessions of active onsite data collection was a key strategy adopted as it facilitated access to patients’ files and captured maternal deaths not reported in District Health Information Software (DHIS2).14 This delay in notification may have likely contributed to a delay in the response to the causes of deaths.
Over the last two years, there was a transition from simple notification of deaths through DHIS2 to proper investigations and the organization of death reviews in the Center Region. This process has helped in the verification of deaths as it addressed the issues of underreporting and misclassification. However, the investigations were assessed as substandard with an average high non-response rate (53.3%) in the reporting of core variables (age, place of birth, profession), required for the identification of sociocultural attributes to deaths. It is reported that a high non-response rate and the occurrence of systemic issues will have a serious impact on the inferences made about the population dynamics.16
The variable, which was least likely to be reported, was the use of partograph (71% non-response rate). The partograph is used to present a pictorial overview of the deviation in the state of well-being of the mother and the fetus as well as the progress of labor.17 It has been demonstrated to save lives through the timely identification and treatment of life-threatening complications.18 In Ghana, the use of partograph was found to be associated with improved birth outcomes (reduced incidence of birth asphyxia). 19 Thus, the non-response regarding the use of the partographs is a barrier to identifying the probable causes of maternal deaths and addressing them.
Although no evidence was found to explain this situation, it is likely that the high nonresponse could be translated as non-use of partographs, for which previous research has attributed it to the lack of knowledge, motivation and supervision of the health workers.20
It is therefore critical to implement strategies that may boost the uptake and the reporting on the use of partographs such as integrating the reporting of partographs as a monthly performance indicator, building the capacity of health workers and establishing a reward or sanction system on its use.
Lack of regulations enforcement strategies for the application of national guidelines
This was a major challenge identified during the process of strengthening the surveillance and the response to deaths. Measures for the regulation of practices and follow-up of recommendations from death reviews were unavailable at all levels of the health pyramid. For example, although the lack of knowledge and the non-availability of partographs were some of the reasons for the non-use, the findings from some reports reveal that knowledgeable health workers were not using the tool while it was available.14,15 Therefore, it is likely that the absence of measures that sanction the non-use of partographs at delivery and other malpractices such as the unauthorized induction of labor during delivery is a barrier to progress.
In addition to this, the findings from review reports revealed that the minimum requirements for delivery rooms and application of reproductive health algorithms for the prevention of deaths were not respected by some health facilities. These measures can be put in place and made applicable at all levels of the health pyramid to help health workers adopt good health practices, consequently reducing the occurrence of facility-related preventable deaths. There is also the need to strengthen professional associations for medical and paramedical personnel, thus ensuring their effective identification of cases and adherence to good practice. This facilitates transparency in awarding sanctions or rewards. The non-existence of quality improvement strategies or the application of incentivized care model for best practices at labor and delivery was a considerable barrier to progress.
Absence of burial permits
A burial permit presents an opportunity for capturing deaths in the community. The experience with implementing MDSR over the years has shown that most of the deaths were captured at the level of the health facility with fewer deaths reported from the community. The reports reviewed showed that it was difficult to capture community deaths because the deceased women were buried as soon as they died. With the absence of burial permits, it is challenging to access information on maternal deaths occurring in the community. To close the existing data gaps, there is also a need to strengthen the vital registration system.
Integration of services as a strategy for addressing the limitations with sustainable financing for MDRS activities
Like many other programs, the availability of sustainable financing for an initiative is often a challenge. This has been the same for MDSR activities in the region. During the process of strengthening the MDSR systems from 2018 to 2019, it was noted that the progress with some MDSR activities (conducting proper death investigations, organizing reviews, and responding to the problems identified) was because of its integration with other reproductive health and HIV activities. For example, the integration with the HIV Point-of-care activities helped to track HIV-related maternal and neonatal deaths while the integration with the Low-Dose High-Frequency projects helped to raise awareness among health workers to conduct routine death audits and take prompt action. Therefore, the sustainability of MDSR activities depends on its successful integration within other health care programs. There still exist vertical health care programs which do not integrate maternal death as an outcome indicator. Given that ending maternal deaths is a core parameter for reproductive health, there is an urgent need for rigorous monitoring within the respective health programs.
No Name No Blame Policy
The “no name no blame culture” emanates from the belief that errors are inherent and should be addressed as systematic factors rather than being treated as personal faults. This slogan was widely used during the MDSR awareness-raising communication on social media (WhatsApp forums) and the review sessions. The marketing and the application of the “No Name No Blame Policy” are likely to have contributed to the increased facility death notifications. There are, however, concerns about its effect on the change in the mindset and the practice of the health workers with respect to minimizing the risks for maternal death. The reason for this is because the review reports continuously depicted the non-use of partographs as an associated cause of death irrespective of the capacity-building activities conducted to facilitate the uptake among health workers. Thus, it is critical to associate this policy with other compliant health measures that will compel health workers to adhere to national guidelines.
4.3 Characteristics and Causes of Deaths
Socio-demographic characteristics/attributes to late referrals
Despite the poor reporting, the data reviewed however provides an insight into the plausible causes of deaths for which there is an urgent need for prompt action. First, the findings from Table 2 reveal that most of the deaths (70%) were within the following age groups: 16-25 years (30%) and 26-35 years (40%). These age groups reflect the young population as per the definition from the African Union Commission.21 Given that young women represent the future generation and are likely to contribute to the economic growth of a country, there is a need for an in-depth analysis to understand the death trends and probable discrepancies when compared to the high-risk age group of 35-49 years as defined by WHO While awaiting the findings from future research, particular attention is needed to address urban facility deaths and attributes to late referrals in tertiary institutions, estimated at 66% and 75% respectively as depicted by the analysis which is likely to be associated with financial limitations of the aforementioned age group.
Furthermore, the findings from death reports revealed that 21% of women who died were likely to visit more than 2 health care facilities in search of proper care. The lack of knowledge on where to access proper care contributed to the delay, thus explaining why they arrived at the tertiary institution in a critical state or dead. Furthermore, most health facilities could not prevent, identify and manage obstetric complications whenever they occurred. 14,15 Thus, there is a need for health worker capacity building on the timely identification and response to emergency obstetric complications/management of high-risk pregnancies. This challenge was worsened by the existence of poorly structured referral systems. The onset of labor through delivery and the immediate postpartum period is a critical period for optimal surveillance of the pregnant woman and her newborn. Therefore, a functional referral system will facilitate access to emergency care as recommended.
Direct and indirect causes of deaths - the role of hemorrhage
Hemorrhage is a preventable cause of maternal death that has continuously plagued resource-limited countries.22,23 The findings reveal that it accounts for 48.6% (70/144) of the known causes of deaths and 37% (70/188) of all cases reported. This value is likely to be higher given the 25% non-response rate recorded in our review (Figure 3). Based on the information available, an estimated 24% (17/70) of the maternal deaths reported due to hemorrhage were related to uterine rupture/atony. All these are preventable causes of death which are likely to be associated with the poor quality of care in the health facility and particularly for those related to the induction of labor. 24,25 There is a need for future research to understand the factors associated with the occurrence of uterine ruptures.
Other causes of deaths requiring a prompt response are those resulting from preeclampsia/eclampsia (12%) and HIV/AIDS (9%). The HIV/AIDS maternal-related deaths is a concern as these deaths resulted from non-compliance to treatment and the recommendations from antenatal follow-up.15
4.4. Study Limitations
The study is a descriptive assessment of the experience with implementing MDSR systems. The data presented in this work is only limited to that captured within the framework of the health information system. However, in the absence of all other reliable data sources, this data provides meaningful insights for prompt and local response to deaths while waiting for feedback from demographic and health surveys which only occur once every 5 to 6 years. The study highlights some of the key areas necessary to strengthen the surveillance system and the need to improve the data collection mechanisms for inferential statistics in the future.
5. Conclusions and Global Health Implications
There is an increasing momentum to boost maternal deaths surveillance and response systems for the attainment of the 2030 Sustainable Development Goals. In the Center Region of Cameroon, there have been significant strides in strengthening the surveillance system. Some of these include the MDSR capacity building and sensitization activities among the key stakeholders, the development and dissemination of national policies/guidelines, reporting tools and the continuous advocacy for improvements in the reporting system.
However, there still exists a daunting challenge with ensuring the sustainability of these actions given the limited financial resources, the lack of motivation for frontline staff to respond to the causes of deaths, weaknesses in the enforcement of data management regulations to ensure the timely and accurate reporting of deaths for prompt action or policies which compel the application of national guidelines at all levels of the health pyramid.
Unlike other health conditions, the response to maternal deaths needs a high-level engagement of political leadership and the attention of decision-makers if the country is to successfully curb the occurrence of preventable deaths by the year 2030. The application of a Functional Referral system and the mandatory use of partographs are some cost-effective strategies that can be put in place to address the issues of late referrals and deaths in the urban city of Yaoundé capital of the Center Region, where most of the deaths reported occurred during the year 2019.
Acknowledgments:
We extend appreciation to all frontline health workers who have dedicated time and financial investment to make sure that the data is captured for this analysis. Our sincere gratitude to all colleagues and collaborators who supported and inspired our work. We wish to thank the Ministry of Public Health and particularly the National Program for Combating Maternal and Child Mortality, for their contribution towards strengthening the surveillance system and ensuring the availability of the tools and reports used in the review. We equally wish to thank our reproductive health implementing partners United Nations Population Fund (UNFPA), United Nations Children’s Fund (UNICEF), Elizabeth Glaser Pediatric AIDS Foundation (EGPAF), Cameroon Baptist Health Services (CBCHS) and International Association of Providers of AIDS Care (IAPAC) who spurred the fight towards ending preventable maternal and neonatal deaths in the Center Region. Special thanks are directed to Mr. Bongajum Emmanuel for the intellectual mentorship towards the compilation and the development of the manuscript.
Compliance With Ethical Standards
Conflict of Interest: The authors declare no competing interest.
Financial Disclosure: Nothing to declare.
Funding Support: There was no funding for the study.
Ethical Approval: The approval for this analysis was obtained from the regional health authorities represented by the Regional Delegate of Public Health in the Center Region of Cameroon.
Disclaimer: None.
References
- Trends in Maternal Mortality 2000 to 2017:Estimates by WHO, UNICEF, UNFPA, World Bank Group and the United Nations Population Division:Executive Summary. World Health Organization 2019
- United Nations 2016
- Ministry of Public Health 2021:6.
- Enquête Démographique et de Santéet àIndicateurs Multiples du Cameroun 2011. Calverton, Maryland, USA INS, ICF International 2012
- Enquête Démographique et de Santédu Cameroun 2018. Yaoundé, Cameroun et Rockville, Maryland, USA: INS,ICF International; 2020.
- Ministry of Public Health 2015
- Strengthening Health Management Information Systems for Maternal and Child Health:Documenting Mchip's Contributions. Baltimore:Jhpiego Corporation 2013:17.
- [Google Scholar]
- Maternal mortality in two reference hospitals in the city of Yaounde (Cameroon):epidemiological, clinical and prognostic aspects. Open J Obstet Gynecol. 2021;11(5):610-625. doi:10.4236/ojog.2021.115057
- [Google Scholar]
- Maternal mortality in Cameroon:a university teaching hospital report. Pan Afr Med J. 2015;21:16. doi:10.11604/pamj.2015.21.16.3912
- [Google Scholar]
- A review of maternal deaths at Douala general hospital, Cameroon:the referral system and other contributing factors. International Journal of Tropical Disease &Health 2015:124-133.
- [Google Scholar]
- Maternal Death Surveillance and Response:Country profile for MDSR implementation (Cameroon). Published 2015 https://www.who.int/publications/m/item/maternal-death-surveillance-and-response-country-profiles
- Maternal Death Surveillance And Response:Technical Guidance Information for Action to Prevent Maternal Death. World Health Organization 2013
- Regional Delegation of Public Health 2018
- Unpublished work ed2020
- The effects of non-response on statistical inference. J Health Soc Policy. 1996;8(1):49-62. doi:10.1300/J045v08n01_05
- [Google Scholar]
- Effect of partograph use on outcomes for women in spontaneous labour at term and their babies. Cochrane Database Syst Rev. 2018;8:CD005461. doi:10.1002/14651858.CD005461.pub5
- [Google Scholar]
- The partograph in childbirth:an absolute essentiality or a mere exercise? J Obstet Gynaecol India. 2018;68(1):3-14. doi:10.1007/s13224-017-1051-y
- [Google Scholar]
- Use and completion of partograph during labour is associated with a reduced incidence of birth asphyxia:a retrospective study at a peri-urban setting in Ghana. J Health Popul Nutr. 2019;38(1):12. doi:10.1186/s41043-019-0171-7
- [Google Scholar]
- Low Utilization of Partograph and Its Associated Factors among Obstetric Care Providers in Governmental Health Facilities at West Shoa Zone, Central Ethiopia. Int J Reprod Med. 2020;2020:3738673. doi:10.1155/2020/3738673
- [Google Scholar]
- African Union Commission 2006
- WHO analysis of causes of maternal death:a systematic review. Lancet. 2006;367(9516):1066-1074. doi:10.1016/S0140-6736(06)68397-9
- [Google Scholar]
- Maternal mortality in sub-Saharan Africa:the contribution of ineffective blood transfusion services. BJOG. 2008;115(11):1331-1339. doi:10.1111/j.1471-0528.2008.01866.x
- [Google Scholar]
- Incidence and factors associated with outcomes of uterine rupture among women delivered at Felegehiwot referral hospital, Bahir Dar, Ethiopia:cross sectional study. BMC Pregnancy Childbirth. 2018;18(1):447. doi:10.1186/s12884-018-2083-8
- [Google Scholar]





