Translate this page into:
Newborn Survival Case Study in Rwanda - Bottleneck Analysis and Projections in Key Maternal and Child Mortality Rates Using Lives Saved Tool (LiST)
*Corresponding author email: felix.sayinzoga@rbc.gov.rw
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Background and Objective:
The Newborn Survival Case study in Rwanda provides an analysis of the newborn health and survival situation in the country. It reviews evidence-based interventions and coverage levels already implemented in the country; identifies key issues and bottlenecks in service delivery and uptake of services by community/beneficiaries, and provides key recommendations aimed at faster reduction in newborn mortality rate.
Methods:
This study utilized mixed method research including qualitative and quantitative analyses of various maternal and newborn health programs implemented in the country. This included interviewing key stakeholders at each level, field visits and also interviewing beneficiaries for assessment of uptake of services. Monitoring systems such as Health Management Information Systems (HMIS), maternal and newborn death audits were reviewed and data analyzed to aid these analyses.
Results:
Policies, protocols, various guidelines and tools for monitoring are already in place however, implementation of these remains a challenge e.g. infection control practices to reduce deaths due to sepsis. Although existing staff are quite knowledgeable and are highly motivated, however, shortage of health personnel especially doctors in an issue. New facilities are being operationalized e.g. at Gisenyi, however, the existing facilities needs expansion.
Conclusion and Global Health Implications:
It is essential to implement high impact evidence based interventions but coverage levels need to be significantly high in order to achieve higher reduction in newborn mortality rate. Equity approach should be considered in planning so that the services are better implemented and the poor and needy can get the benefits of public health programs.
Keywords
Bottleneck Analysis
Lives Saved Tool
Rwanda
Maternal and Newborn Health
Neonatal Mortality
1. Background and Introduction
1.1. Situational analysis of Newborn health in Rwanda
Rwanda is a landlocked country bordered by Uganda in the North, Burundi in the South, Tanzania in the East and Democratic Republic of Congo in the West. The country has an estimated population of 11,533,476[1] living within an area of 26,338 square kilometers (sqkm) (Population density: 437inhabitants/sqkm). Rwanda is divided into four geographically based provinces North, South, East, and West and the City of Kigali (Figure 1). The lower administrative areas consist of 30 districts, 416 sectors, 2,148 cells, and 14,837 villages. The current population growth rate is 2.6% and Total Fertility Rate is 4.2.[2] The major population is young with around half of the population under 19 years of age. School attendance now stands at about 92% (for population aged 6 years or more having ever attended school).[2] Extreme poverty has reduced from 45% to 39% (2010-11 to 2013-14 period),[3] thus indicating progress in economic situation of people. The major population in the country live in rural areas and around 84% of the population is estimated to stay in these areas.[4]

- Political and Administrative Maps of Rwanda; Source: UN Country Data and Rwanda Development Board: http://www.theiguides.org/public-docs/guides/rwanda
Rwanda has come a long way and recovered substantially from the 1990s, which was marked by civil war, genocide, mass movements of refugees, and economic deterioration. The first decade of the new millennium (2000-10) was characterized by an improvement and recovery of the political and economic situation of the country. Rwanda has demonstrated that constant focus on improving health systems in the country could yield rich dividends. An example of this is that the country reached Millennium Development Goals (MDG) targets 4 and 5 in 2015 (Table 1).
| Reference period | Point decline 2015-2000 | % decline 2015-2000 | MDG Goals | HSSP III | ||||
|---|---|---|---|---|---|---|---|---|
| 2000 | 2005 | 2010 | 2015 | By 2015 | 2018 | |||
| Under 5 mortality rate (per 1000) | 196 | 152 | 76 | 50 | 146 | 74 | 52 | 42 |
| Infant mortality rate (per 1000) | 107 | 86 | 50 | 32 | 75 | 70 | −28 | 22 |
| Neonatal mortality rate (per 1000) | 44 | 37 | 27 | 20 | 24 | 55 | 12 | 10 |
| Maternal mortality ratio (per 1 lakh) | 1071 | 750 | 476 | 210 | 861 | 80 | 268 | 220 |
| Total fertility rate | 6 | 6.1 | 4.6 | 4.2 | 1.8 | 30 | 4.5 | 3.4 |
1.2. Significant policy changes to address maternal and infant mortality in Rwanda
Some salient policy changes led to efforts to reduce maternal and child mortality in Rwanda. These include introduction of a community health insurance scheme that contributed to the removal of barriers to access health services, health seeking behaviors, provision of quality health services boosted by performance-based financing (PBF) schemes, strong political leadership, commitment and vision leading to innovative reforms and evidence-based strategies and policies based on ground realities.[5] However, the gains in reducing maternal and child mortality could not be translated towards reducing newborn mortality as is evident with slower decline in newborn mortality rate (NMR).
There has been a steady decline in almost all the key indicators as shown in Table 1. The above table in interpreted in the form of a graph as below (Figure 2):
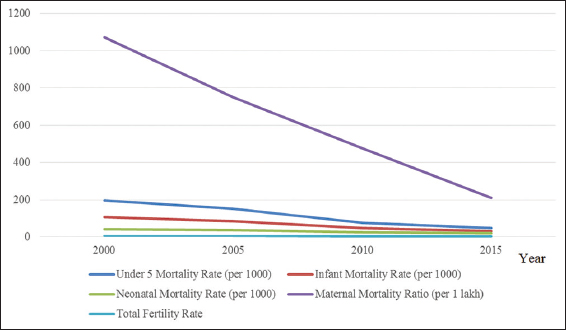
- Decline in Key Mortality indicators in Rwanda, 2000 to 2015; Source: Rwanda Demographic and Household Survey Reports
The highest percentage decline has been in Maternal Mortality Ration (MMR) and lowest in Total Fertility Rate (TFR). Within key maternal and child mortality indicators, there has been a slower decline in NMR. There could be several reasons for this decline, an understanding of which is crucial to develop a future policy to reduce NMR e.g. the use of modern contraception among women increased from 10 to 45% during the period from 2005–10[7] and is possibly one of the key reasons for this decline in TFR.
According to the Rwanda Four-Year Summary Report of Maternal and Newborn Deaths, 2012-2015, more than 50% maternal deaths occurred during the postpartum period, 15% of mothers died before delivery, 66% deaths occurred at district/provincial hospitals, 16% died at health centers and 5% occurred at home.[8] The major causes of death were postpartum hemorrhage (26.7%), sepsis/infection (14.2%), obstructed labor 11%, Eclampsia (10.4%).[7] This report added that 84% of these deaths were due to preventable causes and delay in seeking care contributed to 43% of the deaths and 36% of deaths were due to delay within health facility and 21% due to delay in transport. Interestingly for C-section, 54% delay within health facility was reported.
Furthermore, this report mentioned that61% neonatal mortalities were reported from low birth weight newborns (less than 2500 gm) and 39% from normal birth weight (more than 2500 gm). It was reported that 63% of neonatal deaths audited took place in the district/provincial hospitals, 24% at health centers and 4.5% at home. Almost 58% of deaths took place in the first 48 hours after birth and 89% within the first week. The major causes of neonatal deaths include birth asphyxia (39%), prematurity (32%) and sepsis/infection (10%).The audit further identified that 71% of neonatal deaths were preventable, 49% of mortality was associated with delay in care seeking, 27% due to late decision during labor and 24% due to insufficient neonatal case management.
1.3. Socio-Demographic characteristics of Rwanda population
The Rwanda Demographic and Household Survey estimates that females constitute around 52% of the population of Rwanda and 48% are males. The population increased from 4,831,527 in 1978 to 10,515,973 in 2012, indicating that the population of the country almost doubled within a span of 34 years.[2] The increase was largely due to rapid population growth, which remains high despite progressive decrease in natural growth rate and the total fertility rate.[2] About 56% of children under-five have their births registered and about 75% of adults are covered by health insurance.[2]
The illiteracy rate in Rwanda decreased from 29% to 23% among women aged 15 - 49 and from 22% to 19% among men in the similar age group during the period from 2005 to 2010.[2] According to the 2012 Census, Christianity is the most dominant religion practiced by 93% of the population (44% are Catholic, 38% Protestant and 12% Adventist), 2% Muslims and 0.4% who do not practice any religion. Kinyarwanda is the country’s first official language followed by English and French.[2]
Table 2 shows the country household population and place of residence, urban or rural. Majority of the country’s population is relatively young with almost 53.4% of the population less than 19 years of age. Majority of the population is below 40 years of age (82%) and around 46% of the population fall in the reproductive age group i.e. between 15 - 49 years of age. There are 89 males for every 100 females indicating a gender imbalance. The population of children within five and nine years is higher than children less than five years of age indicating a slight decline in total fertility rate.
| Age range | Urban | Rural | Rwanda | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Male | Female | Total | Male | Female | Total | Male | Female | Total | |
| < 5 | 14.6 | 13.8 | 14.2 | 15.9 | 13.9 | 14.9 | 15.7 | 13.9 | 14.8 |
| 5-9. | 13.8 | 12 | 12.9 | 16.7 | 14.6 | 15.6 | 16.2 | 14.2 | 15.1 |
| 10-14. | 11.6 | 10.4 | 11 | 14.8 | 13 | 13.8 | 14.2 | 12.5 | 13.3 |
| 15-19 | 9.4 | 12.1 | 10.8 | 10.6 | 9.2 | 9.9 | 10.4 | 9.7 | 10 |
| 20-24 | 10.9 | 11.9 | 11.4 | 7.2 | 8.1 | 7.6 | 7.8 | 8.7 | 8.3 |
| 25-29 | 10.5 | 10.7 | 10.6 | 6.9 | 7.5 | 7.2 | 7.5 | 8.1 | 7.8 |
| 30-34 | 9.5 | 9 | 9.3 | 6.9 | 7.3 | 7.1 | 7.4 | 7.6 | 7.5 |
| 35-39 | 5.7 | 6.1 | 5.9 | 4.4 | 5.4 | 4.9 | 4.6 | 5.5 | 5.1 |
| 40-44 | 4.4 | 4.2 | 4.3 | 3.5 | 4.5 | 4 | 3.7 | 4.4 | 4.1 |
| 45-49 | 3 | 2.7 | 2.8 | 3 | 3.6 | 3.3 | 3 | 3.4 | 3.2 |
| 50-54 | 2.2 | 1.9 | 2.1 | 2.9 | 3.3 | 3.1 | 2.7 | 3.1 | 2.9 |
| 55-59 | 1.3 | 1.7 | 1.5 | 2.4 | 3 | 2.7 | 2.2 | 2.8 | 2.5 |
| 60-64 | 1.1 | 1.1 | 1.1 | 1.7 | 2.2 | 2 | 1.6 | 2 | 1.8 |
| 65-69 | 0.7 | 0.6 | 0.7 | 1.1 | 1.3 | 1.2 | 1 | 1.2 | 1.1 |
| 70-74 | 0.4 | 0.8 | 0.6 | 0.8 | 1.3 | 1.1 | 0.8 | 1.2 | 1 |
| 75-79 | 0.3 | 0.5 | 0.4 | 0.5 | 0.8 | 0.6 | 0.4 | 0.7 | 0.6 |
| 80+ | 0.3 | 0.6 | 0.4 | 0.8 | 1 | 0.9 | 0.7 | 0.9 | 0.8 |
| 2000 | 2015 | % decline 2015-2000 | 2030 | |
|---|---|---|---|---|
| Under 5 mortality rate (per 1000) | 196 | 50 | 74 | 13 |
| Infant mortality rate (per 1000) | 107 | 32 | 70 | 9 |
| Neonatal mortality rate (per 1000) | 44 | 20 | 55 | 9 |
| Maternal mortality ratio (per 1 lakh) | 1071 | 210 | 80 | 42 |
| Total fertility rate | 6 | 4.2 | 30 | 2.94 |
Source: Rwanda Demographic and Household Survey Reports
| Strength | Weakness | Opportunities | Threats |
|---|---|---|---|
| Leadership and governance | |||
| Good Governance and leadership – Policies and Protocols are in place and strategic documents have been developed | Implementation of policies is weak at facility levels e.g., practice of hand washing, infection control practices | Growing focus on newborn health so policies and technical documents can be revised and strengthened and other evidence-based interventions can be implemented | |
| Health financing | |||
| Budget available for strengthening labor room and neonatology units | Space is limited and the costs for setting up units are high. The current norms do not include | Funds from donor agencies owing to growing focus on newborn health | High out of pocket expenses incurred by community in care seeking |
| Human resources | |||
| Highly motivated staff at all levels and recruited HR have strong commitment to improve health systems | Specialist Doctors are in short supply. Due to less number of academic institutes, the number of new doctors recruited will remain low. High staff turnover. | Willingness to learn and make a change in reducing newborn mortality. | Loss of skills learnt through training due to high turnover |
| Health service delivery | |||
| Maternal and neonatology units are available including KMC wards | Units lack space and too much overcrowding due to high number of admissions in some units. Management of equipment e.g., lack of knowledge to operate radiant warmers especially at health centers, replacement of phototherapy tunes, cleaning of filters in oxygen concentrators. Some of the components of Essential newborn care e.g., Prevention of Hypothermia, counseling on Breastfeeding. Assured Referral transport mechanisms e.g., Preapproval of transport by confirmation from higher level referral center, avoidance of referral for cases that can be managed locally etc., Quality of care protocols for infection control are not being implemented | Increased number of maternal and neonatology units even upcoming hospitals such as Gisenyi Hospitals | |
| Technology, medicines and equipment | |||
| Availability of norms for setting up newborn care units | Lack of maintenance mechanisms and knowledge among health staff especially at health center levels. | Strengthen existing protocols with maintenance mechanisms and guidelines | |
| Community ownership and participation | |||
| Excellent awareness of the public health care facilities especially type of treatment available at neonatology units. Aware about some of the danger signs in newborns | Lack of support from family especially during prolonged admissions | Motivated community health workers acting as a bridge between health systems and community. Young population of the country who can adopt healthy behaviors | Out of pocket expenses incurred in care seeking leading to request by family for early discharge from facilities. Uninsured population that constitutes around 21% of the population |
| Monitoring and evaluation | |||
| Strong HMIS, Rapid SMS model and use of data in planning | Use of management tools to strengthen facilities e.g., Delivery points – high case load facilities is not being done but can be prioritized for planning. Use of Death audits and live data to monitor each and every newborn admitted and prompt action | Review of newborn care tools in other countries and develop or adapt real time monitoring of data | |
| Social norms | There are no major bottlenecks in terms of care seeking or traditional practices |
| Legislation/Policy (Strategic plan MCH 2013-18) | Policies are already in policy, however, strategic plans needs to be revised to include social determinants of health in planning. |
| Budget/expenditure | Budget has been year marked for various activities, however, costing and release of funds is delayed |
| Management/coordination | At the national level there is a management structure that meets regularly once every three months and also various technical groups that have been constituted that meet regularly |
| Socio-cultural beliefs and practices | There are no major bottlenecks in terms of socio culture beliefs and practices |
| Availability of essential commodities (Adequate/inadequate) | Drugs and equipment required for Newborn care have been supplied to various neonatology units, however, mechanisms and protocols for using and maintaining these equipment are missing |
| Availability of human resources | There is HR shortage both for specialists (neonatologists, regular doctors) and also nurses |
| Physical accessibility and financial accessibility | Geographic access is an issue and there are some health centers located far off from district hospital, so delay in referring patients is an issue |
| Initial utilization | The initial utilization of services by beneficiaries is good, they have good aware about treatment available at neonatology units and there are no major bottleneck in this |
| Timely continuous utilization | With increase of utilization, timely continuous utilization is low and the major reason is lack of support from family especially in cases needing a longer duration of treatment |
| Effective quality coverage | Quality coverage and quality of care is a major bottleneck identified. Protocols for hand washing, infection control practices, disinfection are completely lacking. |
1.4. Population pyramid
Figure 3, indicates that majority of the population is relatively young. This shape is a result of fertility trends over the last few years, outcome of genocide in 1994 and related to migration.
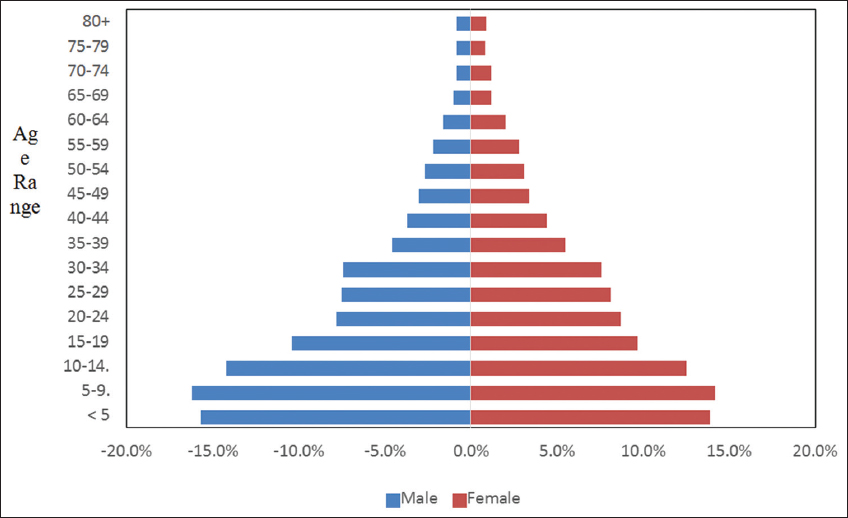
- Population Pyramid of Rwanda
1.5. Equity profile (RDHS 2014 -2015)
According to the Rwanda Demographic and Health Survey (RDHS) 2014-2015, 84% of the country’s population live in the rural areas; 74% of the population is covered by health insurance, including 84.8% in the richest quintile and 57% in the poorest quintile. In the urban areas, 75% of the population falls into the richest quintile as compared to only 9% in the rural areas and 23% of the rural population falls into the poorest quintile. Around 12% and 20% of women and men age 15-49 have no primary education in the lowest wealth quintile and 56% and 60% have some primary education in the same quintile respectively. Around 43% of men and 70% of the women age 15-49 do not access radio, TV or newspaper at least once a week in the lowest wealth quintile. Around 83% of women and 90% of men in the same age group are employed in the lowest wealth quintile. The median age of marriage for women with no education is 20.3 years in comparison to average age for marriage as 22 years. The Total fertility rate is 4.2, 3.6 in urban and 4.3 in rural areas (5.1 in case of lowest wealth quintile). About seven percent of teenage women (15-19 years) have already begun child bearing and at age 19, 215 of the young women have begun childbearing (16% already have at least 1 child and 5% pregnant for the first time).
NMR in rural areas stands at 24 in comparison to 15 in urban areas. Further neonatal mortality stands at 40 and 33 in case of maternal age less than 20 and between 40 – 49 years. The neonatal mortality stands at 33 for newborns born with less than 2 years of birth interval in comparison to 17 for more than 4 years of spacing between two births. Equity issues are also reported in access e.g. 82% of women in the age range 15-49 reported problems in accessing health care in the lowest wealth quintile.
1.6. Linear trend/analysis
The relationship between these indicators with time (i.e., year) is negative. In other words, with increase in time, there would be a steady decrease in mortality.
If this current trend of decline in mortality and TFR of key indicators from 2000 to 2015 is sustained, then by 2030 considering similar percentage decline, the country would reach above figures considering linear trend of decline.
1.7. Cost-effective interventions to improve newborn health in Rwanda
In line with the Lancet Newborn Series.[8] the following evidence-based interventions are recommended to reduce newborn mortality, with interventions currently implemented in Rwanda are represented by a tick (✓):
Pre-conception: Folic acid supplementation
-
Antenatal:
a) Tetanus Toxoid Immunization (✓)
b) Syphilis screening and treatment (✓)
c) Prevention of Pre-eclampsia and Eclampsia (Calcium supplementation) (✓)
d) Intermittent presumptive treatment for Malaria
e) Detection and treatment of asymptomatic bacteriuria
-
Intrapartum:
a) Antibiotics for preterm premature rupture of membranes (✓)
b) Corticosteroids for preterm labor (✓)
c) Detection and management of breech (caesarian section) (✓)
d) Labor surveillance (including Partograph) for early diagnosis of complications (✓)
e) Clean delivery practices (✓)
-
Postnatal:
a) Resuscitation of newborn baby (✓)
b) Breastfeeding (✓)
c) Prevention and management of hypothermia (✓)
d) Kangaroo Mother care (low birth weight infants in health facilities) (✓)
The current core strategies to improve maternal and child health in Rwanda are based on the continuum of care and life cycle approach. The strategies include access to family planning (counseling, services and supply), skilled care during pregnancy and childbirth, antenatal care (ANC), Skilled Birth Attendants, including Emergency Obstetric and Neonatal Care (EmONC), immediate postnatal care for the mother and the newborn) and post abortion care services. These interventions are implemented either at the facility and community levels or at the facility level only (e.g., Postnatal Care, PNC and EmONC).[9]
1.8. Objectives
The Newborn Case study in Rwanda was commissioned by the United Nations Children’s Fund (UNICEF) office to understand the key changes in policy, planning and strategies and suggest recommendations for the next phase. This was part of the Rwandan national government’s effort to strengthen maternal and newborn health in the country. The specific objectives of the Newborn Case Study (NCS) were to:
Analyze and document changes (increase or decrease) in key facility and community-based maternal and newborn health interventions and practices using the best available data; (during the period 2000-15);
Provide a detailed analysis on equity in Maternal and Newborn Health intervention/s, coverage/s across socio-economic status, rural/urban and education;
Determine the facilitating factors for change and remaining bottlenecks and barriers;
Conducting in-depth desk review, focus group discussion/s, interview of key informants and
Suggest actions that could be prioritized and accelerated in the future as per the current government strategies for maternal and child health and also aligned with the new Sustainable Development Goals (SDGs);
Examine current strategies and suggest linkages with the other sectors within Health and also related to social determinants of health in the field of newborn health;
Examine monitoring and evaluation (M&E) framework, mechanism for current use of data for action and suggest an M&E framework to cover agreed indicators based on parameters of quality of care, gender etc. in order to closely monitor newborn health in the country; and
Document the success stories from the field that could be considered feasible for scale up within Rwanda; and hare lessons learned with other countries.
2. Methodology
The Newborn Case Study (NCS) was based on a participatory approach by involving the key stakeholders at every step of the process. The process included conducting in-depth desk review, focus group discussion/s, interview of key informants etc. Data captured from 2000 until date were used for this analysis. The results have been presented in later sections as qualitative interpretation and quantitative based on HMIS information that was made available. In addition, bottleneck analysis and Lives Saved Tool analysis has been conducted which is described in later sections.
2.1. Assessment framework and matrix
The framework for NCS for this assignment is described below in Figure 4 and is based on the health systems M&E framework developed by the World Health Organization (WHO)[10] It focuses on following four domains viz. 1) System inputs, 2) Processes, 3) Outputs, and 4) Outcomes.
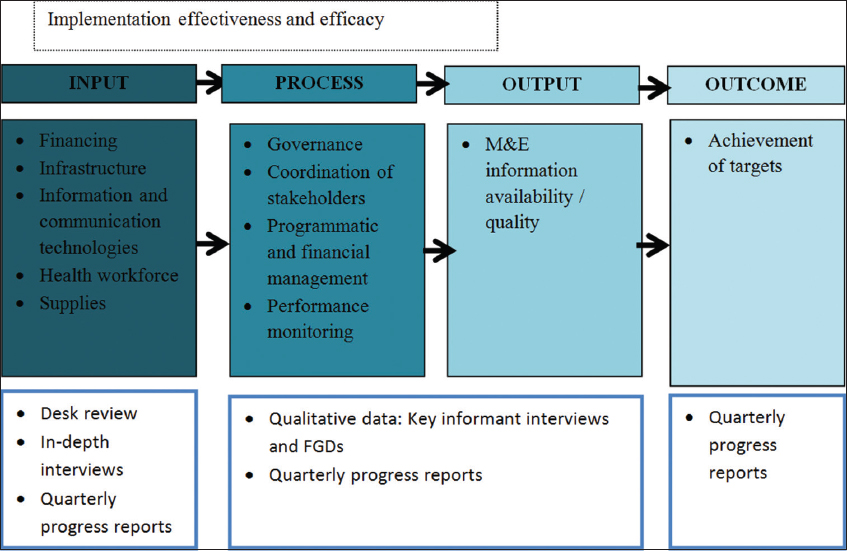
- Assessment framework for NCS Study in Rwanda Source: Adapted from WHO HSS building blocks framework
The review did not evaluate the impact resulting from historic interventions, because reduction in neonatal mortality by increasing coverage is beyond the goal and objectives of this assignment. However, this study used the most recent data as baseline, and capture present evidence based interventions and proposed interventions, proposed coverage levels (targets) and deduce NMR that the country could achieve in subsequent years.
2.2. Assessment approach
The NCS utilized a mixed methodology for complete review of Newborn health situation in the country. This methodology followed a concurrent strategy of triangulation, combining qualitative and quantitative methods and collect data simultaneously due to the short duration of the review.[11] The main advantage of this approach was application of quantitative and qualitative methods to evaluate the same indicators and thus to increase the robustness of the results.
Specifically, a defined set of questions for each objective and related indicator/s were assessed for their achievement until end of the year 2015 based on quarterly/annual reports provided by the implementing agencies. The data collected was analyzed against each indicator and conclusions were drawn based on quantitative and qualitative assessment of each indicator.
The review process was framed based on the six steps of the U.S. Centers for Disease Control and Prevention’s Guidelines for Program Evaluation in Public Health maintaining four standards: Utility, Feasibility, Propriety, and Accuracy.[12]
2.3. Quantitative data collection
In-depth review of various documents and routine reports such as quarterly/annual progress reports, Surveys such as District Household Survey (DHS), Health Monitoring Information System (HMIS) and RapidSMS, national and district reviews and other literature related to Rwanda Maternal, Child and Newborn Health Program were studied. In the next stage, review of the progress against set indicators was undertaken in the project log frame matrix.
2.4. Qualitative data collection
Qualitative assessment included the following components related to service providers’ and beneficiaries’ perspectives:
For each indicator with significant/low achievement, reasons, bottleneck, future plans for improving achievement and lessons learned were studied in detail. This activity provided insight to lessons learned, good practices and scalable solutions that can improve newborn health situation in the country.
Series of interviews were conducted with key stakeholders from different agencies, local community members, and local health care providers to understand their perspective. This activity provided insight into ongoing activities, potential to improve or scale up some components that could have a high impact on newborn mortality reduction.
Series of observations were made at State and District Health Facilities providing care to sick newborns in terms of treatment protocols, trainings and skills assessment for doctors and nurses. The main purpose of this activity was to assess the objectives related to reducing newborn mortality and provision of different levels of health facilities to manage sick newborns.
Series of observations were made during focus group discussions with the community health workers. The main purpose of this assessment was to assess linkage between the government and the beneficiaries, skills to screen and refer sick newborns to health facilities e.g. understanding of danger signs, referral transport etc.
Series of observation were made during focus group discussion with the community/beneficiaries. The main purpose of this assessment was to understand various government health programs related to newborn health, out of pocket expenses incurred by the family for care seeking, utilization of government referral mechanisms, provision of any type of incentives for delivery at health facilities vis. a vis. care available for home delivery, understanding of the key health messages e.g., early initiation of breastfeeding.
Tools such as Bottleneck analysis tool for critical maternal and newborn health interventions based on the 10 coverage determinants and Strength, Weaknesses, Opportunities, and Threats (SWOT) analysis based on the six health system building blocks and LiST were used to undertake this study.
2.5. Limitation of bottleneck and LiST analysis
The analysis is limited in evaluating and reviewing all evidence based interventions individually implemented in the country for maternal and newborn health in terms of its coverage, skills learnt etc. The case study is also limited in terms of reviewing each and every maternal and newborn care facility and suggesting specific changes for each unit. Further, the LiST analysis does not include social determinants of health.
2.6. Lives saved tool analysis (LiST) method
This tool, developed by the John Hopkins Bloomberg School of Public Health, helps to summarize the key interventions, projected coverage levels of each and can thus deduce where the mortality levels will reach in the defined period.[13] We used the Lives Saved Tool in calculating projections in key maternal and child mortality rates and different coverage levels as detailed in Tables 6 and 7. Based on these, we project that the under-five mortality rate will reduce to 29%; infant mortality rate will decrease to 16%; neonatal mortality rate will decrease to 8%; and maternal mortality ratio will decrease to 80% by the year 2030 (Figure 5).
| Indicator | 2015 | 2020 | 2025 | 2030 |
|---|---|---|---|---|
| Under five mortality rate | 50 | 45 | 34 | 29 |
| Infant mortality rate | 32 | 29 | 21 | 16 |
| Neonatal mortality rate | 20 | 18 | 11 | 8 |
| Maternal mortality ratio | 210 | 165 | 95 | 80 |
| Name of intervention | Baseline coverage | Source of data | Target (all values in %) | ||
|---|---|---|---|---|---|
| 2015 | 2020 | 2025 | 2030 | ||
| Tetanus toxoid vaccination | 82.4% | RDHS 2014-15 | 90 | 95 | 100 |
| IPTp or ITN | 67.7% | RDHS 2014-15 | 90 | 95 | 100 |
| Syphilis detection and treatment | 84.7% | HMIS 2015 | 90 | 95 | 100 |
| Calcium supplementation | NA | NA | 50 | 70 | 90 |
| Micronutrient supplementation | NA | NA | 50 | 70 | 90 |
| Balanced energy supplementation | NA | NA | 50 | 70 | 90 |
| Hypertensive disorder case management | NA | NA | 50 | 70 | 90 |
| Diabetes case management | NA | NA | 50 | 70 | 90 |
| Malaria case management | NA | NA | 50 | 70 | 90 |
| Magnesium sulphate management of pre-eclampsia | NA | NA | 50 | 70 | 90 |
| Fetal growth restriction detection and management | NA | NA | 50 | 70 | 90 |
| Skilled birth attendance | 90.7% | RDHS 201415 | 90.7 | 95 | 100 |
| Exclusive breastfeeding at 1 month | 93.5% | RDHS 201415 | 93.5 | 95 | 100 |
| Clean postnatal practices | NA | NA | 50 | 70 | 90 |
| Chlorhexidine | NA | NA | 50 | 70 | 90 |
| Hand washing with soap | NA | NA | 50 | 70 | 90 |
| Maternal Sepsis case management | NA | NA | 50 | 70 | 90 |
| Case management of premature babies | NA | NA | 90 | 95 | 100 |
| Oral antibiotics for neonatal sepsis | NA | NA | 50 | 70 | 90 |
| Active management of 3rd stage of labor | NA | NA | 68 | 95 | 100 |
| S. No. | Hospital | Total deliveries | C-section | Live births | Admissions (Neonatology) | Inborn | Outborn | Referred (Newborns referred to higher level=data from maternity) | Died (Death at birth=data from maternity) | % deaths vs. admissions |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Bushenge PH | 1714 | 821 | 1679 | 220 | 127 | 93 | 1 | 15 | 6.8 |
| 2 | Butare Chu Hnr (Huye) | 1861 | 726 | 1824 | NA | NA | NA | 0 | 1 | |
| 3 | Butaro DH | 1259 | 440 | 1229 | 508 | 251 | 257 | 0 | 6 | 1.2 |
| 4 | Byumba DH | 3468 | 1662 | 3399 | 772 | 487 | 285 | 0 | 19 | 2.5 |
| 5 | CHK (CHUK) HNR | 1919 | 870 | 1891 | NA | NA | NA | 4 | 16 | |
| 6 | Gahini DH | 1672 | 632 | 1642 | 454 | 271 | 183 | 0 | 17 | 3.7 |
| 7 | Gakoma DH | 1147 | 533 | 1144 | 106 | 57 | 49 | 16 | 11 | 10.4 |
| 8 | Gihundwe DH | 2262 | 958 | 2233 | 503 | 380 | 123 | 15 | 13 | 2.6 |
| 9 | Gisenyi DH | 4759 | 2452 | 4688 | 1329 | 833 | 496 | 0 | 13 | 1.0 |
| 10 | Gitwe DH | 2122 | 881 | 2119 | 476 | 286 | 190 | 194 | 13 | 2.7 |
| 11 | Kabaya DH | 1931 | 826 | 1888 | 442 | 280 | 162 | 0 | 13 | 2.9 |
| 12 | Kabgayi DH | 4263 | 1861 | 4261 | 864 | 673 | 191 | 44 | 19 | 2.2 |
| 13 | Kabutare DH | 2767 | 1127 | 2716 | 682 | 387 | 295 | 0 | 15 | 2.2 |
| 14 | Kaduha DH | 739 | 284 | 741 | 135 | 81 | 54 | 4 | 7 | 5.2 |
| 15 | Kanombe military hospital | 419 | 225 | 344 | NA | NA | NA | 3 | 1 | NA |
| 16 | Kibagabaga DH | 4813 | 1735 | 4727 | 1116 | 832 | 284 | 84 | 11 | 1.0 |
| 17 | Kibilizi DH | 1739 | 777 | 1730 | 468 | 276 | 192 | 9 | 19 | 4.1 |
| 18 | Kibogora DH | 2605 | 1141 | 2555 | 794 | 514 | 280 | 1 | 10 | 1.3 |
| 19 | Kibungo RH | 3019 | 1344 | 2974 | 713 | 385 | 328 | 0 | 12 | 1.7 |
| 20 | Kibuye RH | 2313 | 800 | 2250 | 397 | 233 | 164 | 1 | 5 | 1.3 |
| 21 | Kigeme DH | 2016 | 948 | 2008 | 662 | 411 | 251 | 141 | 8 | 1.2 |
| 22 | Kinihira PH | 1452 | 698 | 1439 | 371 | 258 | 113 | 0 | 10 | 2.7 |
| 23 | Kirehe DH | 2738 | 976 | 2655 | 726 | 316 | 410 | 2 | 31 | 4.3 |
| 24 | Kirinda DH | 1155 | 608 | 1139 | 379 | 293 | 86 | 195 | 6 | 1.6 |
| 25 | Kiziguro DH | 2670 | 944 | 2550 | 677 | 371 | 306 | 0 | 23 | 3.4 |
| 26 | Masaka DH | 3341 | 1395 | 3287 | 675 | 363 | 312 | 0 | 6 | 0.9 |
| 27 | Mibilizi DH | 2698 | 1303 | 2679 | 621 | 400 | 221 | 3 | 18 | 2.9 |
| 28 | Mugonero DH | 982 | 201 | 948 | 179 | 78 | 101 | 1 | 7 | 3.9 |
| 29 | Muhima DH | 7632 | 2255 | 7563 | 1519 | 1341 | 178 | 590 | 40 | 2.6 |
| 30 | Muhororo DH | 1716 | 619 | 1685 | 445 | 292 | 153 | 0 | 6 | 1.3 |
| 31 | Munini DH | 1328 | 655 | 1310 | 322 | 171 | 151 | 140 | 11 | 3.4 |
| 32 | Murunda DH | 1807 | 874 | 1746 | 459 | 228 | 231 | 0 | 8 | 1.7 |
| 33 | Nemba DH | 1817 | 686 | 1775 | 661 | 443 | 218 | 0 | 12 | 1.8 |
| 34 | Ngarama DH | 1815 | 599 | 1781 | 652 | 397 | 255 | 1 | 10 | 1.5 |
| 35 | Nyagatare DH | 4177 | 1281 | 4040 | 1071 | 730 | 341 | 348 | 36 | 3.4 |
| 36 | Nyamata DH | 3457 | 1369 | 3341 | 706 | 370 | 336 | 378 | 3 | 0.4 |
| 37 | Nyanza DH | 2912 | 1313 | 2889 | 657 | 417 | 240 | 409 | 13 | 2.0 |
| 38 | RemeraRukoma DH | 2226 | 823 | 2209 | 614 | 324 | 290 | 0 | 17 | 2.8 |
| 39 | Ruhango PH | 2065 | 834 | 2063 | 470 | 306 | 164 | 0 | 10 | 2.1 |
| 40 | Ruhengeri RH | 5579 | 2276 | 5522 | 1950 | 1304 | 646 | 0 | 19 | 1.0 |
| 41 | Ruli DH | 1439 | 632 | 1417 | 498 | 318 | 180 | 88 | 6 | 1.2 |
| 42 | Rutongo DH | 1442 | 552 | 1428 | 236 | 140 | 96 | 0 | 0 | 0.0 |
| 43 | Rwamagana PH | 3606 | 1410 | 3507 | 898 | 623 | 275 | 0 | 31 | 3.5 |
| 44 | Rwinkwavu DH | 2725 | 766 | 2655 | 556 | 349 | 207 | 0 | 14 | 2.5 |
| 45 | Shyira DH | 982 | 313 | 982 | 229 | 148 | 81 | 1 | 5 | 2.2 |
| Total | 110568 | 44425 | 108652 | 26212 | 16744 | 9468 | 2673 | 586 | 2.2 | |
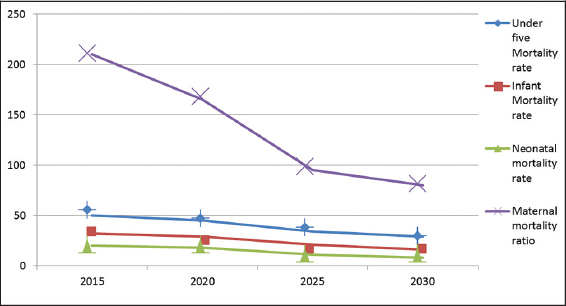
- Projections using LiST Tool in the year 2020, 2025 and 2030
2.7. Planning, management, coordination and oversight of implementation including operationalization of newborn care units at various levels
There are 48 hospitals in the country and most of them have maternal and newborn care facilities and are located in all 30 districts. The newborn care units are typically 6 to 14 bedded (radiant warmers) and have equipment such as incubators, phototherapy and oxygen concentrators besides drugs and other items required to run these units. The units lack accurate planning although they are being managed by an in-house arrangement including support from National level. At the health center levels, some of the centers have either none or one two radiant warmers.
In terms of implementation, it was observed that at various places, radiant warmers were set at 34°Celsius instead of recommended 37.5°Celsius. Staffs were not aware of when to change the tubes in phototherapy units and many of the oxygen concentrators either lacked filter to clean incoming air or the filters were very dirty. Most of the facilities visited lacked continuous uninterrupted 24 x 7 supplies of electricity and running water. Most of the staff at facilities made an in-house arrangement to wash hands; however, at some facilities, liquid hand soap was not available. Bag and mask was available at almost all facilities visited; however, it appeared as if it has seldom been used and staffs were unable to explain how it is cleaned after use. There were no protocols to leave shoes and changing into scrubs or hospital clothes while entering the newborn facilities. Therefore, quality of care at birth especially in newborn health facilities was missing. The newborn health facilities have designated space and space for Kangaroo Mother Care. In terms of implementation for supply of drugs and equipment, no delays were observed. The newborn facilities lack good governance in terms of implementation of quality of care at several of the facilities visited. Protocols for cleanliness e.g. ensuring clean hand washing and infection control mechanisms were severely lacking.
2.8. Monitoring and evaluation framework and health management Information system (HMIS) analysis
Muhima District hospital is the busiest unit in the country followed by Ruhengiri, Kibagababa, Gisenyi, Kabgayi and Nyagatare hospitals. The mortality figures within the newborn units vary from 0% in Rutongo hospital to 10.4% in Gakoma hospital. The number of deliveries reported from these units for the full year was 110,568; it comprised of C-section 44425 (40.1%); live births 108,652; still births1,916 (17.3 per 1000 live births), 26,212 admissions was neonatology (64% Inborn, 36% Outborn), 2,673 referred and 2.2% mortality within neonatology units.
The number of deliveries in the country was 323,976, live births in the country as reported from HMIS was 317,855, still births reported was 6,121 (still birth rate 19.25 per 1000 live births), total newborn deaths was 3,459 (neonatal mortality rate 10.88 per 1000 live births). Out of 3459 newborn deaths, 3204 died within first week of life (early NMR 10 per 1000 live births). Mortality within one week constitutes 92.6% of the total newborn mortality. The maternal deaths reported was 303 so maternal Mortality ratio was 93.5 per 100000 deliveries.
3. Recommendations
The in-depth review from the Newborn Case Study, Bottleneck analysis, and LiST tool has helped to document and reflect on the progress in reducing child and maternal mortality in Rwanda. At the same time, this review has helped to identify some gaps in terms of service delivery and uptake of services by the community. Based on these findings we present the following recommendations:
Revise the norms and requirements for facility based newborn care to include actual need based on population ratio, number of beds and dedicated human resources in newborn care. Busy units could be provided more resources and similarly health centers that cater to large number of deliveries.
Complete the revision of the component of home based newborn care and Post Natal Care (PNC) Guidelines. When completed, the revised PNC care would go a long way in identifying early signs of illness and prompt referral to designated units. A mechanism of assured referral together with use of a single number for “National Ambulance Service” with GPS-fitted vehicles can help to reduce delay in reaching health facilities. In addition, an interactive central software based system to track number of admissions can help reduce load at busy facilities and pre-approved incoming referral for admission at other facilities.
Implement policies and protocols that can reduce chances of developing infection/sepsis during pregnancy, labor and newborn period. Infection management protocols along with use of clean water, clean hands, clean instruments, interactive messages to pregnant women to increase their knowledge on safe pregnancy services, etc., would help to reduce sepsis.
Strengthen existing evidence based interventions by increasing effective coverage levels and consider rolling out other interventions such as pre-conception iron and Folic acid supplementation.
Develop an interactive software tool to monitor newborn health closely and guide providers on intrapartum and newborn protocol to ensure that every pregnant women and newborn admitted in a health facility are monitored closely and correctly managed. The newborns discharged from these units could be followed by up community health workers through use of Rapid SMS. It is recommended to follow up preterm and low birth weight newborn till the age of 1 year and 2 years respectively as these continue to remain vulnerable in this period and may die due to Hypothermia or Hypoglycemia.
Provide regular mentoring and a periodic visit to labor rooms and neonatology units is required in order to re-orient skills and handholding. Quality of life of newborns discharged from neonatology units for developmental delays can also be improved. In addition, establish early intervention centers at few hospitals e.g. provincial hospitals.
Interlink newborn health with other health related program in areas such as family planning, nutrition etc., and also interlink newborn health with social determinants of health e.g. regular supply of electricity and water, improving geographic access for busy units and busy health centers.
Follow up identified gaps and causes of mortality from death audits. Although death audits are taking place on a monthly basis, it is recommended that gaps identified should be promptly followed up so that preventable causes of mortality could be reduced.
Identify and prioritize high impact evidence based interventions and packaged as public health program e.g., EmONC for maternal health and facility and community based management of newborns for newborn health. The gains made under this policy could become a model not only for the African region but also for the whole world.
4. Conclusion and Global Health Implications
Over the last few years especially after 2005, a lot of improvement in the Rwandan health system has been made in terms of recruitment of health professionals, setting up/renovation of health facilities etc. The maternal and child health program has seen several improvements; however, the improvement in reduced newborn mortality had a slower pace in comparison to under five mortality and maternal mortality ratio.
In Rwanda, newborn healthcare equipment are now available in almost all district hospitals and many health centers, however, the protocols for their use are not in place. In addition, the recruited human resources especially doctors and nurses need to be trained in the proper use of these equipment, including their maintenance and troubleshooting and also in specialized trainings e.g., on essential newborn care.
Acknowledgements
The authors acknowledge the following members of the Newborn Technical Working Group, Ministry of Health, Government of Rwanda for providing key inputs during the conduct of the study and also during the Bottleneck Analysis workshop: Dr Evodia Dushimimana (MOH), Catherine Mugeni (MOH/RBC), Dr Richard Munyaneza (USAID MCSP), Dr Catherine Kirk (Partners in Health), Dr Joel Mubiligi (Partners in Health), Mathias Gakwerere (UNFPA), Dr Yvonne Umurungi (Catholic Relief Services), Pacifique Mukashema G (RBC, Remera, MoH) for providing coverage data and assistance in LiST analysis.
Conflict of Interest: The authors declare no conflicts of interest.
Ethical Approval: This study was based on the analysis of existing data.
Funding Support: This study was funded by UNICEF Office for Rwanda.
References
- 2013-14 (EICV4)
- 2012-18
- Rwanda Demographic Health Survey, Rwanda 2005, 2010 and 2015
- Changes in Fertility Decline in Rwanda: A Decomposition Analysis, International Journal of Population Research 2014 Article ID 48621
- Four Year Summary Report of Maternal and Newborn Deaths (2012-15) in Rwanda
- Evidence based, cost effective interventions: how many newborn lives can we save? Lancet. 2005;8;365(9463):977-988.
- [Google Scholar]
- Monitoring and evaluation of health systems strengthening: An operational framework, Geneva, Switzerland, November 2009
- Research Design: Qualitative, Quantitative and Mixed Methods Approaches. Sage Publications; 2003.
- Framework for program evaluation in public health, Morbidity and Mortality Weekly Report. 48 1999
- Baltimore, MD: John Hopkins Bloomberg School of Public Health; http://www.livessavedtool.org/





