Translate this page into:
Oral Health Status of Pregnant Women Attending Antenatal Clinic in Cameroon

*Corresponding author: Ashu Michael Agbor, Department of Oral Health/Dentistry, Universite des Montagnes, Bangangte, Cameroon. agborasm@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Agbor AM, Zencha LN, Essome H, Ndikum CB, Foumane P. Oral health status of pregnant women attending antenatal clinic in Cameroon. Int J MCH AIDS. 2025;14:e009. doi: 10.25259/IJMA_27_2024
Abstract
Background and Objective:
Pregnancy is characterized by complex physiological and psychological changes that can affect the oral health of women. There is a paucity of literature on the oral health status of pregnant women in Cameroon. The objective of our study was to describe the oral health status of pregnant women attending the Laquintinie antenatal clinic in Douala, Cameroon.
Methods:
A descriptive cross-sectional study from January 2021 to June 2021 was conducted involving pregnant women who attended the antenatal clinic at Laquintinie Hospital and provided informed consent. A pretested questionnaire was administered in both French and English. Intraoral and extra-oral examinations were carried out to identify oro-facial pathologies.
Results:
Two hundred ninety-four pregnant women participated in our study, with ages ranging from 17 to 45 years (mean age = 26 years ± 5.1 standard deviation). Of these 144 (51.7%) were employed, 195 (70%) were married, and 168 (60.6%) had tertiary education. More than 20 (70%) were multiparous, and 111 (40%) were in the first trimester of pregnancy. Three-quarters, 210 (75%), had good knowledge of tooth cleaning, 182 (65.2%) brushed their teeth once daily, and 189 (68%) brushed only in the morning. Only a few 9 (3.2%) knew how to take care of their baby’s teeth, and 84 (30.1%) had been to a dentist. Halitosis was observed in 82 (29.3%), and all our participants had calculus deposits. The predominant oral pathologies were dental caries 168 (60.2%), gingivitis 143 (51.3%), and periodontitis 126 (45.2%). A third, 92 (33%) of the women had swelling of the gums during pregnancy, while 68 (24.5%) did not experience any change. In addition, 62 (22.2%) experienced bleeding, 43 (15.4%) pain, 10 (3.6%) ulcerations, and 10 (3.6%) epulis (pyogenic granuloma). Three out of four 210 (75.3%) of the women needed restoration for carious lesions.
Conclusion and Global Health Implications:
The oral health status of pregnant women in the Laquintinie antenatal clinic was poor, with a higher prevalence of dental caries and periodontal diseases ranging from mild to severe gingivitis and gingival epulis.
Keywords
Adult Periodontitis
Antenatal Care
Cameroon
Dental Caries
Oral Health
Pregnant Women
INTRODUCTION
Pregnancy, though a physiological process and a sign of good health, is a period that is characterized by changes in the internal milieu of a woman developing a fetus. This period is associated with morphological, physiological, social, and psychological changes in the woman’s body, affecting her oral health and quality of life. Psychological changes can occur from the very beginning to the end of pregnancy, including the postpartum period.[1]
Dental caries and periodontal disease are historically considered the most important global oral health burdens, without exempting pregnant women. These diseases pose significant health problems in most industrialized countries, affecting 60–90% of school-aged children and adults. At present, the distribution and severity of dental caries vary in different parts of the world and within the same region or country.[2]
Dental caries experience in children is measured using the decayed, missing, and filled teeth (DMFT) index, which is relatively high in the Americas (DMFT = 3.0) and in the European Region (DMFT = 2.6), whereas the index is lower in most African countries (DMFT = 1.7).[3] In most developing countries, the levels of dental caries were low until recent years, when the prevalence rates of dental caries and dental caries experience are now tending to increase.[3] This high DMFT index is largely due to the increasing consumption of sugars and inadequate exposure to fluorides, which help arrest the already existing dental caries and prevent new carious lesions by remineralizing hard dental tissues. An increase in the DMFT index in developing countries has been observed in the past 20 years as a result of rapid urbanization. In contrast, a decline in caries has been observed in most industrialized countries.[4,5] This pattern is the result of several public health measures, including the effective use of fluorides (in the form of sodium fluoride and silver diamine fluoride), together with changing nutritional choices, lifestyles, and improved self-care practices.[4] However, it must be emphasized that dental caries, as a disease of children, cannot be eradicated, but only controlled to a certain degree. In Cameroon, a prevalence of 70–78% of dental caries in children has been reported.[5]
Oral diseases and disorders create short-term and prolonged physical discomfort, pain, infection, tooth loss, and temporary and permanent loss of oral function. They are responsible for chewing, swallowing, and speaking, and can disrupt sleep and productivity. As such, poor oral health has been associated with decreased school performance, poor social relationships, and less success later in life.[6] Oral diseases, even in adults, can affect the general health of an individual and one’s ability to get and keep a job. Several reports have linked low-grade infection in the mouth (periodontal disease and dental abscesses) to systemic illnesses such as cardiovascular diseases (heart disease), respiratory ailments (pulmonary or lung disease), and poor pregnancy outcomes (low birth weight and miscarriage).[6,7] Oral disorders can also lead to dementia, erectile dysfunction, cancers, infertility, kidney diseases, and rheumatoid arthritis.[6,7]
During pregnancy, there are increased levels of estrogen and progesterone. Furthermore, estradiol levels in plasma are reported to increase up to 30 times higher than those found during a reproductive cycle.[8] Estrogen regulates cellular proliferation, differentiation, and keratinization, but progesterone affects the permeability of the microvasculature and also changes the production of collagen.[8] It is these hormonal alterations during pregnancy that are responsible for the high incidence of dental diseases like gingivitis and may even contribute to low salivary pH, dental hard tissue demineralization, and subsequently increased incidence of dental caries.[8,9] During this period, the gingiva without preexisting inflammation remains unaffected. Gingival changes usually occur in association with poor oral hygiene and local irritants such as calculus, plaque, and food debris. The bacterial flora in dental plaque is the major cause of gingival and periodontal diseases. However, the hormonal and vascular changes that accompany pregnancy often exaggerate the inflammatory response to the local irritants.[9]
The prevalence of dental caries in pregnant women varies between 74% and 99.9%.[10] Among other oral pathologies, pregnancy gingivitis is common among pregnant women and presents as a nonspecific, vascularizing, and proliferative inflammation with large amounts of infiltrated inflammatory cells.[10,11] The onset of pregnancy gingivitis coincides with the selective growth of periodontal pathogens, such as Prevotella intermedia and Eikenella corrodens in subgingival plaque from the 3rd to 4th month of pregnancy.[10,11]
Apart from the direct consequences of hormonal changes, women tend to experience an alteration of their oral health and oral hygiene habits during pregnancy.[11] This, coupled with vomiting, has adverse effects on the oral cavity as it favors the build-up of plaque and decreases the pH of the oral cavity, thereby enhancing the formation of dental caries and periodontal diseases.[11] There is a paucity of literature on the oral health status and treatment needs of pregnant women in Cameroon. The present study was carried out to assess the oral health status and treatment needs of pregnant women attending the Laquintinie General Hospital of Douala.
METHODS
Study Design
The method used for our study followed the Strobe guidelines for observational studies.[12] We carried out a descriptive, cross-sectional study between January 2021 and June 2021 at the antenatal clinic of the department of obstetrics and gynecology of the Laquintinie Hospital, a second-category specialist referral hospital with more than 30 specialists. The hospital records an average of 160,000 consultations and 7,983 hospitalizations annually. The hospital has 800 beds and a team of 58 doctors, including 42 specialists. The gynecological and obstetrical department was established in 1931. The gynecological unit has 5 consultants, gynecologists, 30-bed wards, and neonatal, maternity, and surgical units.
Sampling and Eligibility Criteria
We enrolled pregnant women attending antenatal clinics at Laquintinie Hospital who agreed to participate in our study during the study period. The study included pregnant women who gave written consent. To minimize selection bias, we ensured that those who accepted to participate were not systematically different from those who declined to take part in the study.
The sample size was estimated at 296 participants using the Lorentz formula: N = p (1-p) Z/d2 and taking p = 54.9% for the prevalence of dental caries. Azodo et al., in a study on dental pain and associated factors among pregnant women, revealed the prevalence (p) of dental caries to be 54.9%.[11]
Data Collection Instrument and Technique
A pre-tested questionnaire in English and French was tested on 10 participants. Data collection was carried out by the principal investigator (AMA), who was trained and calibrated in a specific clinical and theoretical workshop using the ICDAS-II methodology (Kappa index = 0.94).
Data were collected in two phases: a structured questionnaire was used to gather participants’ personal data, followed by a clinical examination to assess the patient’s oral health. The questionnaire was used for collecting information on the socio-demographic data of the participants, such as oral hygiene knowledge and practice, oral health history, and oral health knowledge and practices, among others.
Clinical examination was conducted under bright light while seated in a portable dental chair placed in the consultation room in the clinic.
Intra-oral examination was carried out on oral hard and soft tissues, and any abnormalities detected on the oral mucosa, the gingival, or any oral lesions were recorded on a data capture sheet.
According to the World Health Organization recommendations, the presence of dental caries and periodontal status were assessed using the DMFT and Community Periodontal Index of Treatment Needs (CPITN) [Table 1] indices, respectively. The treatment needs of the patients were established from the DMFT, CPITN indices, and from the results of other oral examinations.[12]
| Variable | Frequency | Percentage |
|---|---|---|
| Age range (years) | ||
| 17–20 | 7 | 5.0 |
| 20–25 | 106 | 38 |
| 25–30 | 106 | 38 |
| 30–35 | 34 | 12.2 |
| 35–40 | 15 | 5.4 |
| >40 | 4 | 1.4 |
| Occupation | ||
| Employed | 172 | 61.5 |
| Unemployed | 107 | 38.5 |
| Place of residence | ||
| Rural | 71 | 25.0 |
| Urban | 208 | 75.0 |
| Marital status | ||
| Married | 196 | 70.4 |
| Divorced | 65 | 23.2 |
| Single | 15 | 5.4 |
| Widowed | 3 | 1.0 |
| Level of education | ||
| Tertiary | 169 | 60.6 |
| Secondary | 87 | 31.2 |
| Primary | 22 | 7.9 |
| Not educated | 1 | 0.3 |
Statistical Analysis
The data collected were analyzed using the Statistical Package for the Social Sciences software and Microsoft Excel software.
RESULTS
Socio-demographic Profile of Participants
We recruited 294 pregnant women aged between 17 and 45 years with a mean age of 26 ± 5.1 standard deviation (SD) years. One third, 106 (38%) of the participants were from the 20 to 25 age group, 7 (6.0%) participants were from the 17 to 20 age group, 106 (38) participants were from the 25 to 30 age group, 34 (12.2%) participants were from 30 to 35 age group, 15 (5.4%) participants were from 35 to 40 age group, and 4 (1.4%) of the participants were more than 40 years old [Table 1].
Three-quarters, 172 (75%) of the participants were employed, 107 (38.5%) were unemployed, 208 (75.0%) resided in urban areas, while 71 (25.0%) lived in rural areas. More than two-thirds, 196 (70.4%) were married, 65 (23.2%) were divorced, 15 (5.4%) were single, and 3 (1.0%) were widowed. Two-thirds, 169 (60.6%) had tertiary education, 87 (31.2%) had secondary education, 22 (7.9%) had primary education, and 1 (0.3%) had no formal education [Table 1].
Clinical Profile
The average gestational age was 4 ± 1.02 months. A third, 111 (39.8%) of the participants were in their first trimester, 107 (38.4%) in the second trimester, and 61 (21.9%) in the third trimester. Three-quarters, 205 (73.5%) were multiparous, 72 (25.8%) were primiparous, and 2 (0.7%) were nulliparous.
Oral Health Knowledge, Practice and Hygiene
Oral health knowledge
Three-quarters, 210 (75.3%) of the women affirmed that cleaning could prevent tooth decay, 50 (17.9%) did not, and 19 (6.8%) did not know the importance of cleaning the teeth [Table 2]. More than half, 162 (58.1%) of the women thought that their gums were unhealthy, 94 (33/7%) healthy, and 23 (8.2%) did not know the state of their gums. Only 9 (3.2%) of the women took care of their baby’s teeth [Table 2].
| Variables | Number (n=279) | Percentage |
|---|---|---|
| Do you think tooth cleaning can prevent tooth decay? | ||
| Yes | 210 | 75.3 |
| No | 50 | 17.9 |
| Don’t know | 19 | 6.8 |
| Condition of your gums at the moment | ||
| Unhealthy | 162 | 58.1 |
| Healthy | 94 | 33.7 |
| Don’t know | 23 | 8.2 |
| Looking after babies’ teeth | ||
| Yes | 9 | 3.2 |
| No | 270 | 96.8 |
All women had calculus deposits, 82 (29.3%) halitosis, and 195 (69.9%) of pregnant women experienced hypersalivation.
A third, 92 (33%) of the women had swelling of the gums during pregnancy, 68 (24.5%) did not experience any change, 62 (22.2%) experienced bleeding, 43 (15.4%) pain, 10 (3.6%) ulcerations, and 10 (3.6%) epulis (pyogenic granuloma) [Figure 1].
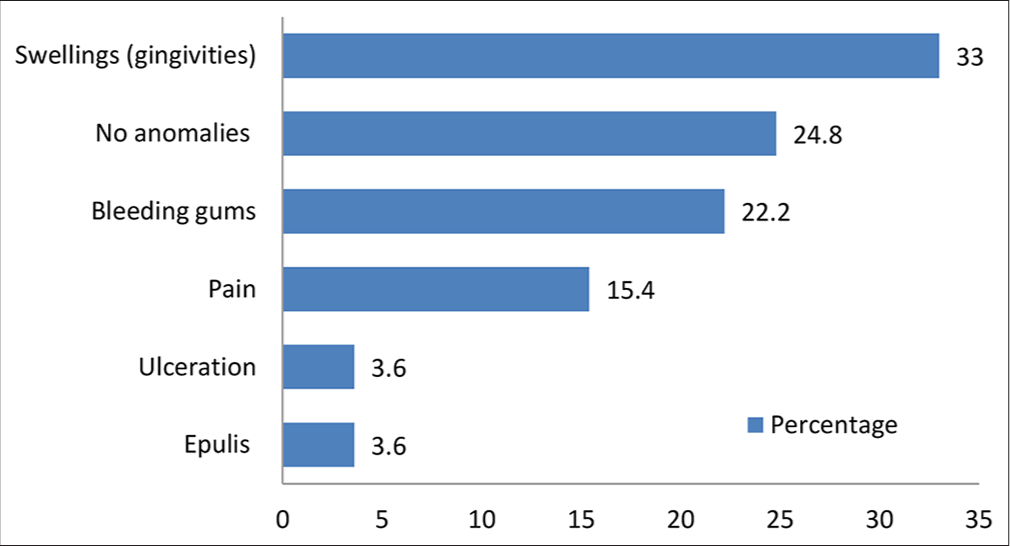
- Changes in the gums since pregnancy.
Oral health habits and practice
The majority, 278 (99.6%), brushed their teeth with a toothbrush. Of these, 182 (65.2%) brushed once a day, 79 (28.3%) twice a day, 17 (61%) more than twice a day while 1 (0.4%) did not brush during pregnancy. Most brushing was done in the morning 189 (68%), after each meal 70 (25.2%), 12 (4.3%) before bedtime, and 7 (2.5%) before meals; toothpicks 170 (60.9%) were used for cleaning, 68 (24.4%) mouth wash, and dental floss 24 (8.7%) [Table 3].
| Variables | Number (n=279) | Percentage |
|---|---|---|
| Dental cleaning material | ||
| Toothbrush | 278 | 99.6 |
| Others | 1 | 0.4 |
| Number of daily brushings | ||
| Once | 182 | 65.2 |
| Twice | 79 | 28.3 |
| More than twice | 17 | 6.1 |
| Never | 1 | 0.4 |
| Time of brushing | ||
| Morning | 189 | 68.0 |
| After each meal | 70 | 25.2 |
| Before bedtime | 12 | 4.3 |
| Before each meal | 7 | 2.5 |
| Tools for oral hygiene | ||
| Toothpicks | 170 | 60.9 |
| Mouthwash | 68 | 24.4 |
| Dental floss | 24 | 8.7 |
A third of the pregnant women, 106 (38%), consumed sweet drinks and foods more than twice a day, 99 (35.5%) twice a day, 66 (23.6%), and 8 (2.9%) did not consume sweets.
About three-quarters of 207 (72.1%) of the women had never been to a dentist, 51 (18.3%) visited the dentist only when they experienced pain, 27 (9.7%) during a routine visit. During pregnancy, 84 (30.1%) had consulted their health services, 195 (69.9%) did not, and 43 (15.4%) used traditional medicines. A third, 104 (37.4%), had knowledge of how to take care of a baby’s teeth before they had their baby, 78 (28%) acquired this knowledge while they were pregnant, 55 (19.7%) after they had their first baby, and 42 (15%) saw no need of having knowledge of taking care of the baby’s teeth.
Oral pathologies and their antecedents
Three-quarters, 210 (75.5%) of the women presented with dental pain, 208 (74.6%) with gum pain.
Dental caries 168 (60.2%), gingivitis 143 (51.3%), and periodontitis 126 (45.2%) were the most common pathologies among pregnant women. Other pathologies present included enamel fluorosis 67 (23.5%), mobile teeth 61 (21.9%), mouth ulcers 30 (10.8%), dental trauma 30 (10.8%), and gingival epulis 22 (7.9%) [Figure 2].

- Distribution of participants according to the oral diseases.
Oral pathologies impacted the patients psychologically 84 (30.1%), affected their esthetics 126 (45.2%), and caused persistent discomfort 129 (45.9%) or disrupted their feeding habits 223 (79.9%) [Figure 3].
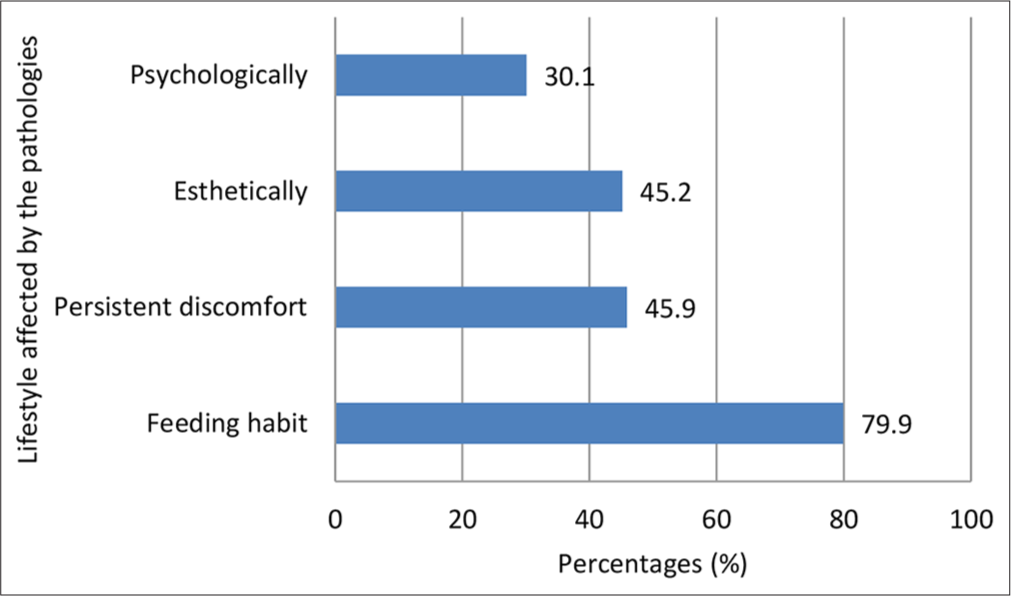
- Distribution of participants based on the impact of oral health issues on their lifestyle.
Treatment Needs
For periodontal treatment needs, 210 (75.3%) needed to improve their oral hygiene, 142 (51.2%) needed scaling, and 61 (21.9%) needed deep scaling or curetting.
For restorative treatment needs, 210 (75.3%) needed restorative treatment, 61 (21.9%) needed tooth extraction, and 43 (15.4%) needed urgent dental treatments. Other treatment needs, such as orthodontics and prostheses, were not significant.
DISCUSSION
The current study revealed that increased salivation, halitosis, periodontal infection, and dental caries were very common in pregnant women. In the current study, the mean age of the pregnant women was 26 years ±5.1s.d which is similar to the results obtained by Takang et al. and Michael et al. both in Cameroon who had 24.9, 2 years, and George et al. in Australia,[13-15] but slightly different from another study carried out at the Raichur District in India where Gupta and Acharya reported a mean age of 21.8 years ± 2.12 SD.[10] These might be due to cultural differences, as a larger proportion of the population in our study had tertiary education and had children after university education and after employment, similar to the scenario reported in Australia.
In our study, 76% of the pregnant women were in the 20–30-year age group. Gupta and Acharya reported the 20–22 age group to be predominant.[9] This could be because the study was carried out in a rural setting where very young women are given early in marriage, as compared to Cameroon, where the majority of the women got pregnant after completing their tertiary education. Early marriage, especially for uneducated women, could affect the level of health education, leading to inadequate information about sexual and reproductive health and rights. In the current study, two-thirds of the women had tertiary education, followed by secondary education, which represented a third of the participants. This signifies that the majority of the women had sound educational backgrounds. This is the reason why 61.5% of the women are employed. Apart from the fact that education determines the level of empowerment and employability of an individual, it is an essential tool in having access to good oral health education as well as quality oral health care.[15]
The current study indicated that more than a third (40%) of pregnant women were in the first trimester. This result is similar to another study carried out in Cameroon by Tolefac et al., who reported that only 34% of women start their antenatal care in the first trimester.[16] These young women were highly educated and were aware of the fact that an early consultation is always very primordial for the screening of diseases and the well-being of their fetuses. Tolefac et al. reported in their study that about half of pregnant women do not start antenatal clinics early in the first trimester, largely due to large family size, low monthly income, and long distance to the hospital.[16] Our study indicated that three-quarters of the pregnant women were multiparous, which was similar to the results obtained by Gorge et al. in Sydney in 2013.[15] Multiparity affects oral hygiene and is directly associated with poor oral health status, especially when the income of the family is very low.
Periodontal Disease
In the current study, 75.3% of pregnant women noticed a change in their gum’s periodontal diseases (gingivitis 51.3% and periodontitis 45.2%). These results corroborate with Takang and Mbong, who observed that 73.2% of pregnant women in their study had periodontal diseases.[12] This could be explained by the fact that the settings of the studies are similar, with the same feeding habits. However, this was very low as compared to Gupta and Acharya in India, who reported that 95% of the pregnant women in their study had periodontitis.[9] Periodontitis is very common in women during pregnancy because during this period, some factors such as hormonal changes, stress, and changes in alimentary habits like frequent eating without brushing increase the level of dental plaque in the mouth. About 14.2–54.8% of pregnant women suffer from periodontal disease, and 11% develop periodontitis, which can destroy periodontal tissue and the distribution of bacteria and other inflammatory mediators.[16] Periodontal disease appears to be associated with adverse events in pregnancy due to the transport of biofilm bacteria into the bloodstream and into placental tissue, which might cause adverse events in the body’s immune response to infection.[16,17] This might lead to preterm birth and the low weight of the unborn child, pre-eclampsia, gestational diabetes, and perinatal mortality.[16,18]
The current study indicated that 69.9% of pregnant women had hypersalivation (ptyalism gravidarum). Here, the patients always complain of bad taste and maintain that swallowing the excessive or thickened saliva perpetuates the sense of nausea and vomiting.[18] It has been established that salivary secretion during pregnancy is under neural control and that stimulation of the parasympathetic nerve supply of the salivary gland causes a profuse watery secretion with very little organic content.[17,18] Hyper salivation is associated with vomiting and nausea, which can induce regurgitation, exposing the teeth to hydrochloric acid, reducing the pH of the oral cavity, resulting in the demineralization of dental hard tissues and subsequently resulting in dental hypersensitivity and dental caries.[10] Nausea and vomiting may cause a pregnant woman to avoid routine oral health practices such as tooth brushing and flossing. This could also lead to dental caries and gingivitis, both of which are bacterial infections.[10]
Oral Health-seeking Behavior
Our study also revealed that more than 70% (195) of pregnant women did not consult dental services. A recent study in Cameroon on the oral health-seeking behavior of Human Immunodeficiency Virus (HIV)-infected children revealed that 92.6% of the children have never been to a dentist.[19] The low uptake of dental services during pregnancy and in children can be attributed to the high cost of dental services.[20] Many women in resource-poor settings also lack access to dental care and dental insurance, which interferes with their ability to receive adequate oral care during pregnancy.[21,22] Insufficient routine examinations and delays in treatment of oral diseases may expose pregnant women to preventable dental infections.[22]
Having an inadequate diet and poor oral health during pregnancy can be detrimental to the health and well-being of the fetus.
Dental Caries
The most common oral disease in our study was dental caries, affecting 75.3% of the pregnant women. The prevalence of dental caries in the current study was similar to that obtained by George et al.,[15] who registered a prevalence of 60.2%. Although caries activity has largely been attributed to the presence of oral streptococci such as Streptococcus mutans and Streptococcus sobrinus, recent studies have reported similar virulence factors expressed by Candida albicans, with oral levels of Candida recognized as indicators of caries activity and possible vertical transmission from mothers to early caries-affected children.[22]
Other Pathologies
Tooth mobility observed in our study, with a prevalence of 21.9%, may be associated with the presence of relaxin, a hormone known to assist with the preparation of the birth canal for delivery and thought to relax the periodontal fibers that hold the tooth in position. Gingival epulis was observed in 22 (8%) of our study and was similar to that obtained in a study in the Kwazulu Natal Province of South Africa (8.5%),[22] possibly due to the high levels of corticosteroids, though this has not yet been proven directly. Pregnancy epulis presents most commonly toward the end of the first trimester of pregnancy and typically recedes after delivery, occurring in approximately 0.2–9.6% of pregnancies.[10,22] It is most often seen in the gingiva, particularly as a result of poor oral hygiene[10,22] and is associated with increased progesterone levels in combination with bacteria and other local irritants.[10,22] Such lesions are generally not treated unless they bleed, interfere with mastication, or remain and do not resolve after delivery. It is imperative for women to be screened for oral health early in pregnancy and advised on the importance of good oral hygiene, the need for regular dental visits, and changes that may be expected in the oral cavity during pregnancy[12] to understand what these changes represent and be reassured of the safety of the treatment.
Treatment Needs
Restorative treatment was the highest treatment need, with a prevalence of 75.3%, which was slightly higher than the findings of Gupta and Acharya, who obtained a prevalence of 66%. This could be due to the difference in sampling frame of the two studies, with the present study being done only in public health centers. An effective model for assessing and conceptualizing the management of dental needs of pregnant women should be aimed at prevention rather than curative procedures, which may sometimes impact both the mother and her unborn baby.[10]
In the current study, 51.3% needed scaling. As part of routine counseling, healthcare providers should encourage all women to schedule a dental examination if it has been more than 6 months since their last examination or if they have any oral health problems. Patients often need reassurance that prevention, diagnosis, and treatment of oral conditions, including dental X-rays (with shielding of the abdomen and thyroid) and local anesthesia (lidocaine with or without epinephrine), are safe during pregnancy. Conditions that require immediate treatment, such as extractions, root canals, and restoration (amalgam or composite) of untreated caries, may be managed at any time during pregnancy.[10] Delaying treatment may result in more complex problems. Counseling should include reinforcement of routine oral health maintenance, such as limiting sugary foods and drinks, brushing twice a day with fluoridated toothpaste, flossing once daily, and dental visits twice a year. Dental providers should recommend the use of chlorhexidine-fluoridated mouth rinses and xylitol-containing chewing gum to decrease oral bacteria. No adverse effects have been reported with these products during pregnancy, but they have not been studied extensively. For patients with vomiting secondary to morning sickness, hyperemesis gravidarum, or gastric reflux during late pregnancy, the use of antacids or rinsing with a baking soda solution (i.e., one teaspoon of baking soda dissolved in 1 cup of water) may help neutralize the associated acid.[10]
Limitations of Study
Language posed a limitation since a lot of time was needed to explain things to the participants. The limited knowledge of pregnant women about oral health and its importance was a problem. Some of the participants’ level of education made it difficult to work. Furthermore, the small sample size prevents the generalization of these results. Bivariate analyses comparing different variables were not highlighted.
CONCLUSION AND GLOBAL HEALTH IMPLICATIONS
The study showed that pregnant women had poor oral hygiene and poor oral hygiene practices, and their quality of life might be affected. The oral health-seeking behavior was also poor. The prevalence of dental caries, periodontitis, and gingivitis was high. Other clinical conditions observed were hypersalivation, dental epulis, and ulcerations.
Recommendations
Dentists should be equipped with tools for early detection, diagnosis, and institution of general treatment protocols when faced with oro-facial manifestations associated with pregnancy. This will reduce other sequelae of dental diseases such as periodontitis, dental caries, and epulis.
Gynecologists should develop a working relationship with local dentists so as to make referrals to dentists a routine or integrate basic oral health into maternal and child health to avoid duplication of basic healthcare delivery, especially in resource-poor settings.
Routine oral health education should be instituted at the antenatal services of hospitals by a dental staff, which, in the long run, can improve the health-seeking behavior of the patients.
Key Messages
1) Pregnancy is a physiological process, however, patients may still present with dental caries, periodontal diseases, and epulis. 2) These can affect their quality of life and the development of the fetus. 3) Regular check-ups during pregnancy are inevitable in both maternal and child health.
Acknowledgments:
We wish to acknowledge the staff of Laquintinie Hospital for all their support.
COMPLIANCE WITH ETHICAL STANDARDS
Conflicts of Interest: The authors declare no competing interests. Financial Disclosure: Nothing to declare. Funding/Support: There was no funding for this study. Ethics Approval: Ethical clearance was obtained from the Ethics Committee of the Faculty of Health Sciences, Université des Montagnes-Bangangte (No/2021/020/UdM/PR/CIE), dated January 2021. Authorization to carry out the study was obtained from the Directors of the different hospital committees. Declaration of Patient Consent: The authors certify that they have obtained all appropriate patient consent. Use of Artificial Intelligence (AI)-Assisted Technology for Manuscript Preparation: The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI. Disclaimer: None.
References
- Oral care in pregnancy. J Turk Ger Gynecol Assoc. 2019;20(4):264-8.
- [CrossRef] [PubMed] [Google Scholar]
- Global results on oral health. 2018. World Health Organization. [cited 2024 Jan 23]. Available from: https://www.who.int/team/noncommunicable-diseases/global-status-report-on-oral-health-2022
- [Google Scholar]
- Prevalence of periodontitis in adults in the United States: 2009 and 2010. J Dent Res. 2012;91:914-20.
- [CrossRef] [PubMed] [Google Scholar]
- A new classification scheme for periodontal and peri-implant diseases and conditions-introduction and key changes from the 1999 classification. J Periodontol. 2018;45(Suppl 20):S1-8.
- [CrossRef] [Google Scholar]
- Global burden of severe periodontitis in 1990-2010: A systematic review and meta-regression. J Dent Res. 2014;93:1045-53.
- [CrossRef] [PubMed] [Google Scholar]
- Children's dental health, school performance, and psychosocial well-being. J Pediatr. 2012;161(6):1153-9.
- [CrossRef] [PubMed] [Google Scholar]
- Oral health Status of diabetes mellitus patients in Southwest Cameroon. Odontostomatol Trop. 2015;38(150):49-57.
- [Google Scholar]
- Global burden of oral conditions in 1990-2010: A systematic analysis. J Dent Res. 2013;92:592-7.
- [CrossRef] [PubMed] [Google Scholar]
- Etiological diversity of caries. Gynecol Obstet Fertil. 2012;40:578-81.
- [CrossRef] [PubMed] [Google Scholar]
- Oral health status and treatment needs among pregnant women of Raichur District, India: A population based cross-sectional study. Scientifica (Cairo). 2016;2016:9860387.
- [CrossRef] [PubMed] [Google Scholar]
- Toothache experience and oral health care in pregnant women in Cameroon. J Kenyan Dent Assoc. 2011;2(179):183-87.
- [Google Scholar]
- Strobe guidelines for observational studies. [cited 2024 Nov 22]. Available from: https://www.equator-network.org/reporting-guidelines/strobe
- [Google Scholar]
- Oral health patterns among pregnant women attending antenatal clinic in Bamenda. Open J Obstet Gynecol. 2023;13(6):1111-26.
- [CrossRef] [Google Scholar]
- Oral health delivery in refugee camps in East Region of Cameroon. Afr Health Sci. 2023;23(2):606-15.
- [CrossRef] [PubMed] [Google Scholar]
- The oral health status, practices and knowledge of pregnant women in South-Western Sydney. Aust Dent J. 2013;58:26-33.
- [CrossRef] [PubMed] [Google Scholar]
- Why do pregnant women present late for their first antenatal care consultation in Cameroon? Matern Health Neonatol Perinatol. 2020;20(1):70.
- [Google Scholar]
- Periodontitis and preeclampsia in pregnancy: A systematic review and meta-analysis. Matern Child Health J. 2022;26:2419-43.
- [CrossRef] [PubMed] [Google Scholar]
- Periodontitis in pregnant women: A possible link to adverse pregnancy outcomes. Healthcare (Basel). 2023;11(10):1372.
- [CrossRef] [PubMed] [Google Scholar]
- Oral manifestations of HIV infection and dental health needs of children with HIV attending HIV treatment clinics in Western Cameroon. Int J MCH AIDS. 2024;13:e022.
- [CrossRef] [PubMed] [Google Scholar]
- Oral health status and treatment needs of pregnant women attending antenatal clinics in KwaZulu-Natal, South Africa. Int J Dent. 2019;2019:5475973.
- [CrossRef] [PubMed] [Google Scholar]
- Evaluation and management of sialorrhea of pregnancy with concomitant hyperemesis. J Natl Med Assoc. 1994;86:704-8.
- [Google Scholar]
- Methods of payment for oral health care in Yaoundé. J Public Health Afr. 2023;14(7):2223.
- [CrossRef] [PubMed] [Google Scholar]






