Translate this page into:
Prevalence and Risk Factors Associated with HIV Infection among Pregnant Women in Odisha State, India
*Corresponding author email: elangovan@nie.gov.in
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Background and Objectives:
The purpose of this study was to analyze trends in HIV prevalence and risk factors associated with HIV infection among pregnant women attending antenatal clinics in Odisha State, India.
Methods:
Data were from the HIV Sentinel Surveillance (HSS) among pregnant women, a descriptive cross-sectional study using consecutive sampling method and conducted in India. Data and samples were collected from pregnant women attending select antenatal clinics that act as designated sentinel sites in Odisha State, India, during the three months surveillance period and in three surveillance years: 2013, 2015, and 2017. All eligible pregnant women aged between 15 and 49 years, attending the sentinel sites for the first time during the surveillance period, were included. Information on their socio-demographic characteristics and blood samples were also collected.
Results:
In total, 38,384 eligible pregnant women were included in the survey. Of these, 107 women were HIV positive, with an overall prevalence of 0.28%. HIV prevalence indicated a stabilizing trend between 2013 and 2017. However, pregnant women whose spouses were non-agricultural laborers, truck drivers, or migrants were significantly at higher risk of being infected. Likewise, HIV prevalence significantly increased over the years among pregnant women whose spouses were in the service sector (government or private). District-wise fluctuations in HIV prevalence was observed, with the district of Cuttack recording the highest prevalence among the districts.
Conclusion and Global Health Implications:
Women who are spouses of non-agricultural laborers, truck drivers or migrants need focused interventions, such as creating awareness on HIV and its prevention. Migration, due to poverty and its impact on sexually transmitted diseases among migrants from low and middle-income countries, have been documented globally. Single male migrant specific interventions are recommended to halt the disease progression among pregnant women and general population in Odisha, India.
Keywords
HIV sentinel surveillance
Pregnant women
HIV prevalence
Socio-demographic factor
Odisha
India
1. Introduction
1.1. Background of the Study
Member states of the World Health Organization (WHO) in 2011 implemented strategic initiatives to reduce the HIV prevalence and AIDS-related deaths; the Joint United Nations Programme on HIV/AIDS (UNAIDS) initiative called 95-95-95 strives to end AIDS by 2030.1 Since 2011, the HIV prevalence in India has declined drastically and its adult HIV prevalence in 2017 was 0.22%.2 Currently, 2.1 million people are estimated to be living with HIV/AIDS in India, of which, 79% are aware of their status and 56% are on anti-retroviral treatment (ART).3 Despite the declining trends in HIV prevalence, the rate of decline has stabilized in most parts of the country. At present, the epidemic is highly heterogeneous and is confined within pockets of high prevalence regions of India.4,5 Towards the goal of ending AIDS by 2030, no complacency at this point is acceptable;6 region-specific targeted interventions and improved ART linkage and adherence to halt the disease transmission are required. Female sex workers (FSW), men having sex with men (MSM), transgenders (TG) and injecting drug users (IDU) form the core risk group of HIV infection, their potential clients such as single male migrants (SMM) and long-distance truckers (LDT) comprise the bridge population. In India, 85% of the infection among the general population is driven through the heterosexual route and hence partners or spouses of the high-risk groups (HRGs) or the bridge population are at a higher infection risk.7 Apart from the controlling HIV among HRGs and bridge population; it is important to identify pockets of disease transmission patterns among general population to implement focused prevention interventions.
Odisha State, in east-coast of India, is geographically diverse with coastal and hilly terrains and more than 80% of its population reside in the rural regions.8 The state comprises of India’s third largest tribal population,9 and most of the residents in Odisha come from a low socio-economic background. Moreover, most of the districts in Odisha are often affected by natural calamities year after another, quite often disrupting the basic infrastructure of the State.10 Odisha state has maintained a low adult HIV prevalence since 2007 (0.30%) with a slow declining trend until 2015 (0.25%); whereas in 2017 it was estimated to be 0.13%.2
1.2.Objectives
Given the geographic adversities and poor socio-economic background of Odisha state, it is important to closely monitor the HIV prevalence trends among the general popuation for effective HIV management. HIV prevalence among pregnant women is one of the indicators of HIV prevalence among general population, as they represent the sexually active population. HIV sentinel surveillance (HSS) among the pregnant women is conducted biennially to estimate the levels and trend of HIV prevalence.11 HIV prevalence among the pregnant women in Odisha peaked in 2009 (0.73%), declined since 2011 until 2015 (0.24%), and increased to 0.28% in 2017 (Figure 1). Hence, analysing the factors associated with risk of HIV infection among pregnant mothers will be insightful for region-specific HIV interventions to halt the disease transmission among the general population. There are very few studies analyzing the trend and risk factors of HIV prevalence among the pregnant mothers in Odisha, and these studies are limited by smaller sample size.12, 13 The specific aim of the study was to analyze the levels and trend of HIV prevalence and factors associated with HIV infection risk among pregnant women in Odisha, State India.
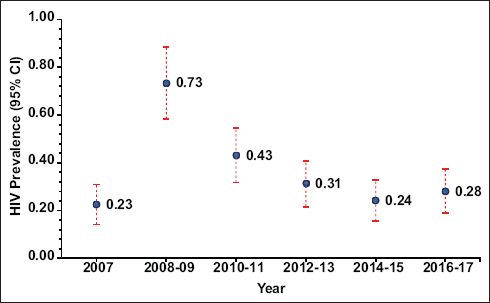
- HIV Prevalence among pregnant women attending ANC clinics in Odisha in the last six rounds of HIV Surveillance Survey (2007 – 2017)
2. Methods
2.1.Setting and Population
The methodology of HSS among ANC attendees has been discussed in detail in the operational manuals for HSS.14 This section discusses some of the key features required for this study. All eligible pregnant women aged between 15-49 years attending the selected antenatal clinic sites across the state for the first time during the surveillance period in 2013,2015 and 2017 were included. This was a cross-sectional study, using consecutive sampling method. The study setting was government-based antenatal clinics act as designated sentinel sites. Atleast one sentinel site per district was selected, to have adequate representation from all districts. HSS is conducted biennially from January to March.
Information on their socio-demographic characteristics and blood samples were collected from eligble respodents attending the sentinel sites during the surveillance period in the years 2013, 2015, and 2017. Sample size per sentinel site was fixed at 400.11 Recruitement was done until the end of three months surveillance period or until sample size was reached. The number of respondents enrolled were limited to 20 per day at each site to ensure the quality of the data collected. Unlinked Anonymous Testing (UAT) strategy was followed in HSS until 2015 and thereafter, it has been changed to Linked Anonymous Testing (LAT) strategy. A two-step testing protocol was followed to confirm the HIV test results. The entire team involved in the HSS were trained rigorously to ensure the authenticity of the data and samples collected.
2.2. Statistical Analysis
Descriptive statistics were used to describe the characteristics of the study samples. The association between HIV prevalence (outcome variable) and the socio-demographic characteristics of the respondents (explanatory variables) were examined using logistic regression method. Odds ratios with 95% CI and p-values were used to indicate the significance of the association between the explanatory and outcome variables. All data were analyzed using the Statistical Package for Social Sciences 26.0 (SPSS Inc., Chicago, Ill., USA). The study was exempted as this is a surveillance activity, since HIV test was anonymous and the results were not used for the purpose of determining the HIV status of a person. The participants were, however, informed about the purpose of the study. The same is endorsed in Item No. 6 under Chapter-III of the India HIV Act 2017.
3. Results
3.1. Sociodemographic Characterisitcs
The distribution of respondents and their HIV prevalence based on the socio-demographic characteristics of the ANC attendees of Odisha in the last three rounds of HSS has been represented in Table 1. The median age of the respondents was 24 years. A little over half the population were young mothers aged between 15 and 24 years. Nearly half the respondents had attended secondary schools, while 15% were illiterate and 20% had attended primary schools. Only 16% had higher secondary and tertiary level education. Almost half the respondents were primigravida; 70% were from the rural regions; and majority (93%) of the respondents were housewives. Highest proportion of the respondents’ spouses were non-agricultural laborers (17.2%) followed by small business owners (15.3%), service sector employees (14.9%), skilled/semi-skilled workers (14.2%), and agricultural cultivators (13.8%).
| Variables | Category | 2013 (n= 12783) | 2015 (n=12801) | 2017 (n= 12800) | OR (95% CI) | |||
|---|---|---|---|---|---|---|---|---|
| (%) | HIV (%) | (%) | HIV (%) | (%) | HIV (%) | |||
| Age group | 15-24 | 57.6% | 0.24% | 56.0% | 0.20% | 54.3% | 0.26% | 1.00 |
| 25-49 | 42.4% | 0.41% | 44.0% | 0.30% | 45.7% | 0.31% | 1.45 (0.99 - 2.12) | |
| Educational status | Illiterate | 15.9% | 0.34% | 16.8% | 0.19% | 11.8% | 0.13% | 1.00 |
| Primary | 23.3% | 0.40% | 17.6% | 0.22% | 20.0% | 0.16% | 1.18 (0.59- 2.37) | |
| Secondary | 45.4% | 0.33% | 49.8% | 0.27% | 51.1% | 0.34% | 1.36 (0.75 - 2.49) | |
| Higher secondary and Above | 15.3% | 0.10% | 15.8% | 0.25% | 17.1% | 0.32% | 1.00 (0.47 - 2.12) | |
| Gravida | First | 51.2% | 0.29% | 50.2% | 0.25% | 46.3% | 0.30% | 1.00 |
| Second | 34.8% | 0.36% | 36.0% | 0.17% | 38.3% | 0.27% | 0.94 (0.62 - 1.44) | |
| Third | 10.7% | 0.15% | 10.3% | 0.38% | 11.5% | 0.20% | 0.86 (0.44-1.69) | |
| Fourth or more | 3.3% | 0.70% | 3.5% | 0.45% | 3.9% | 0.40% | 1.82 (0.83 - 4.02) | |
| Residence | Urban | 31.0% | 0.31% | 29.3% | 0.27% | 27.2% | 0.35% | 1.00 |
| Rural | 69.0% | 0.30% | 70.7% | 0.22% | 72.8% | 0.26% | 0.85 (0.56 - 1.28) | |
| Occupation of the respondent | AL | 2.2% | 0.00% | 1.8% | 0.45% | 1.0% | 0.79% | 1.00 |
| NAL | 2.5% | 0.00% | 1.9% | 0.00% | 0.9% | 0.92% | 0.47 (0.04 - 5.19) | |
| DS | 0.3% | 0.00% | 0.1% | 0.00% | 0.1% | 0.00% | - | |
| S/SSW | 0.4% | 0.00% | 0.3% | 2.78% | 0.4% | 0.00% | 2.30 (0.21 - 25.58) | |
| PB/SSO | 0.4% | 0.00% | 0.2% | 0.00% | 0.2% | 0.00% | - | |
| SE/LBO | 0.1% | 0.00% | 0.0% | 0.00% | 0.0% | 0.00% | - | |
| Service (Govt./Pvt) | 2.3% | 0.00% | 2.5% | 0.63% | 1.7% | 0.45% | 1.14 (0.19- 6.84) | |
| Student | 0.1% | 0.00% | 0.3% | 0.00% | 0.2% | 0.00% | - | |
| Hotel Staff | 0.0% | 0.00% | 0.0% | 0.00% | 0.0% | 0.00% | - | |
| Trucker | 0.0% | 0.00% | 0.0% | 0.00% | 0.0% | 0.00% | - | |
| LTW | 0.1% | 0.00% | 0.0% | 0.00% | 0.0% | 0.00% | - | |
| AC | 0.1% | 0.00% | 0.8% | 0.00% | 0.1% | 0.00% | - | |
| House Wife | 91.6% | 0.34% | 92.2% | 0.22% | 95.3% | 0.27% | 0.88 (0.22 - 3.57) | |
| Occupation of the spouse | AL | 11.2% | 0.21% | 10.2% | 0.08% | 11.2% | 0.28% | 1.00 |
| NAL | 17.0% | 0.65% | 19.4% | 0.37% | 15.2% | 0.36% | 2.38 (1.09 - 5.20)* | |
| DS | 0.3% | 0.00% | 0.1% | 0.00% | 0.3% | 3.03% | 6.19 (0.77 - 50.02) | |
| S/SSW | 13.6% | 0.35% | 12.4% | 0.32% | 16.5% | 0.14% | 1.35 (0.56 -3.21) | |
| PB/SSO | 14.3% | 0.33% | 15.0% | 0.10% | 16.5% | 0.19% | 1.07 (0.44 - 2.62) | |
| SE/LBO | 3.8% | 0.41% | 2.7% | 0.29% | 2.4% | 0.00% | 1.36 (0.36 - 5.14) | |
| Service (Govt./Pvt) | 14.9% | 0.11% | 15.5% | 0.30% | 14.3% | 0.60% | 1.74 (0.76 - 3.98) | |
| Student | 0.1% | 0.00% | 0.1% | 0.00% | 0.1% | 0.00% | - | |
| Hotel Staff | 1.8% | 0.44% | 1.1% | 0.70% | 1.1% | 0.00% | 2.05 (0.43 -9.70) | |
| Trucker | 2.3% | 0.34% | 2.0% | 0.38% | 2.6% | 1.20% | 3.53 (1.22 - 10.20)* | |
| LTW | 6.2% | 0.38% | 6.1% | 0.51% | 5.9% | 0.27% | 2.02 (0.78 - 5.25) | |
| AC | 13.8% | 0.11% | 14.7% | 0.00% | 13.0% | 0.00% | 0.20 (0.04 - 0.92)* | |
| Unemployed | 0.5% | 0.00% | 0.6% | 0.00% | 0.6% | 0.00% | - | |
| NA | 0.1% | 0.00% | 0.1% | 10.00% | 0.4% | 0.00% | 7.99 (0.99 - 64.84) | |
| Spouse migration | Yes | 8.0% | 0.59% | 10.1% | 0.63% | 6.3% | 0.50% | 2.35 (1.41 - 3.91)** |
| No | 92.0% | 0.29% | 89.9% | 0.19% | 93.7% | 0.26% | 1.00 | |
| Living with | Spouse | 99.9% | 0.31% | 99.9% | 0.24% | 99.6% | 0.28% | 1.00 |
| NA | 0.1% | 0.00% | 0.1% | 8.33% | 0.4% | 0.00% | 5.22 (0.72 - 37.91) | |
3.2. HIV Prevalence
The distribution and HIV prevalence based on the socio-demographic characteristics of the ANC attendees of Odisha in each three rounds of HSS has been analyzed and presented in Table 1. It has been observed that the proportion of young mothers gradually decreased with each round of HSS. Likewise, while the proportion of illiterates or less-educated gradually decreased, the proportion of mothers with higher education slowly increased with each round of HSS. Certain occupations of the respondents’ spouses and the migration status of the spouses were significantly associated with higher risk of HIV prevalence. Respondents whose spouses were non-agricultural laborers (OR: 2.38 CI: 1.09 - 5.20) or truck drivers (OR: 3.53 CI: 1.22 - 10.20) were at a significantly higher risk of infection. Similarly, respondents whose spouses were migrants (OR: 2.35 CI: 1.41 - 3.91) were at higher risk of infection that those whose spouses were non-migrants. District-wise HIV prevalence reflects a fluctuating trend. (Table 2). Cuttack has maintained a high prevalence (>1%) in all three rounds of HSS.
| District | 2013 | 2015 | 2017 | Trend |
|---|---|---|---|---|
| Anugul | 0.50 | 0.25 | 0.25 |  |
| Balangir | 0.25 | 0.25 | 0.50 |  |
| Balasore* | 1.50 | 1.00 | 0.00 |  |
| Bargarh | 0.50 | 0.25 | 0.00 |  |
| Baudh | 0.00 | 0.25 | 0.00 |  |
| Bhadrak | 0.00 | 0.00 | 0.25 |  |
| Cuttack | 1.75 | 1.00 | 2.75 |  |
| Deogarh | 0.25 | 0.25 | 0.25 |  |
| Dhenkanal | 0.25 | 0.00 | 0.50 |  |
| Gajapati | 0.00 | 0.00 | 0.00 |  |
| Ganjam* | 0.88 | 0.75 | 0.00 |  |
| Jagatsinghapur | 0.00 | 0.00 | 0.25 |  |
| Jajapur | 0.00 | 0.00 | 0.25 |  |
| Jharsuguda | 0.25 | 0.75 | 0.50 |  |
| Kalahandi | 0.00 | 0.75 | 0.00 |  |
| Kandhamal | 0.00 | 0.00 | 0.25 |  |
| Kendrapara | 0.25 | 0.00 | 0.00 |  |
| Kendujhar | 0.00 | 0.00 | 0.00 |  |
| Khordha | 0.00 | 0.25 | 0.00 |  |
| Koraput | 0.13 | 0.13 | 0.00 |  |
| Malkangiri | 0.00 | 0.00 | 0.00 |  |
| Mayurbhanj | 0.00 | 0.00 | 0.50 |  |
| Nabarangapur | 0.25 | 0.25 | 1.00 |  |
| Nayagarh | 0.00 | 0.25 | 0.25 |  |
| Nuapada | 0.00 | 0.00 | 0.00 |  |
| Puri | 0.50 | 0.25 | 0.25 |  |
| Rayagada* | 1.50 | 0.00 | 0.25 |  |
| Sambalpur | 0.25 | 0.25 | 0.25 |  |
| Sonapur | 0.00 | 0.00 | 0.00 |  |
| Sundarearh* | 0.00 | 0.00 | 0.75 |  |
4. Discussion
This study aims to analyze the variables associated with risk of HIV infection among the most vulnerable ANC population in Odisha. Based on the overall analysis, some of the occupations of the spouses of the respondents and the migration status of the spouses were significantly associated with the infection risk of the ANC population in Odisha. Spouses of migrants / non-agricultural labourers or truckers were at a higher risk of infection. (Table 1). The prevalence of HIV among ANC whose spouses were employed in the government or private sectors also significantly increased with each round of HSS, while the representative proportion of respondents remained the same. Likewise, majority of the infected women were house-wives. Keeping in mind these observations, the study arrives at some of the key factors to be concentrated in terms of halting and reversal of disease progression among the general population in Odisha.
4.1. Socio-demographic Factors Associated with Infection Risk among Pregnant Women
Respondents whose spouses were non-agricultural labourers or migrants were at a higher risk of HIV infection. Majority of the population in Odisha relies on agriculture for living and about 60% of the below poverty line population in rural Odisha are agricultural laborers or small farmers.15 With 11 major river systems, Odisha is prone to floods and cyclone and specifically most of the coastal districts are affected.10, 16 Hence, majority of the population in Odisha migrate to neighboring districts/states, owing to low income, loss from natural disasters, unemployment or inaccessibility to good infrastructure.17, 18 Seasonal outmigration is highly prevalent throughout the state especially in the districts of Kalahandi, Khordha, Jajpur, Balasore and Ganjam; whereas Cuttack experiences a higher proportion of in-migration.19 More specifically, Ganjam reports a larger volume of outmigrants who are involved in unskilled labor in the construction, industrial or transport sectors at the destination sites.20 The destination of the migrants were regions of high HIV prevalence including Surat in Gujarat, Maharashtra, Karnataka, Andhra Pradesh and Tamil Nadu.16 Given their poor educational and socio-economic background, these migrants are more susceptible to the infection risk,21 which is more prominent among single male migrants working in the textile mills in Surat. While targeted intervention (TI) program for migrant within the state focuses on the in-migrants, little is known about the interventions for the out-migrants. Currently, Odisha State AIDS Control Society (OSACS) has implemented transit interventions in 2016, targeting the migrants at most prominent transit sites in 11 districts.22 The effect of these transit interventions are to be monitored regularly, to achieve zero transmission among the migrants. On a positive note, migration in Odisha is highly regulated through the ‘Dadan System’ (A system for Inter-State migrant labors known as Dadan Labor).23 The state level Dadan Labor (Control and Regulation) Act strives to improve the living standards of the migrants.24 Efforts to integrate migrant-specific HIV interventions of the State AIDS Control Society with the Dadan system will be instrumental in HIV prevention and continuous management among migrants in Odisha.
4.2. State-level Risk behaviours of HRGs, Literacy and HIV Management
Reports from national Integrated Biological and Behavioral Surveillance (IBBS) and National Family Health Survey-4 (NFHS 4) were used to discuss the risk factors of disease progression and transmission among the general population. By comparing the HSS data and the existing state level reports, this study arrives at few important findings to be monitored with reference to HIV prevention and management. HRGs are the main focus group to reduce the infection risk among the general population. Identifying the factors associated with high-risk behavior among HRGs and attempts to achieve relevant behavior changes among HRG is essential to halt the disease transmission. Concurrently, ART linkage and adherence to ART is essential to eliminate HIV as a public health threat. Some of the factors hindering the above-mentioned in Odisha state are discussed.
HIV Prevalence and Behaviour of HRG in Odisha: According to the IBBS report 2014-2015,25 a much higher proportion of FSWs and MSMs, when compared to that of the national average, reported to have engaed in sex activity at a much younger age. (Table 3) Higher proportion of FSWs in Odisha reported experiencing sexual violence. Similarly higher proportions were reported by MSM from Odisha. In general, at least one in 5 children in Odisha are sexually exploited before 14 years, leading to a larger proportion of the FSWs and MSM in Odisha involved in commercial sex activities at a very young age, which might also be due to their poor economic background. Sexual debut at a young age is often considered as a prominent risk factor for HIV infection.25 Sexual exploitation of young children and girls, leads to high-risk sexual behavior among young HRGs.26,27 Reports also document the outmigration of young tribal girls to northern states due to poverty and sexual violence in Odisha,28 and unfortunately, some of them are again sexually exploited at their destination places.29,30
| Sexual behavior of HRG | Odisha (Proportion %) | India (Proportion %) | ||||
|---|---|---|---|---|---|---|
| FSW | MSM | IDU | FSM | MSM | IDU | |
| First sexual intercourse at ≤ 14 years | 18.6 | 37.9 | 1.6 | 8.6 | 18.8 | 2.5 |
| First sexual intercourse at 15-17 years | 42.0 | 42.7 | 15.2 | 33.8 | 35.7 | 19.5 |
| Commercial sex at ≤ 14 years | 4.7 | 23.1 | - | 1.4 | 5.9 | - |
| Commercial sex at 15-17 years | 20.7 | 36.5 | - | 8.4 | 21.9 | - |
| Msm sexual debut at ≤ 14 years | - | 26.8 | - | - | 16.7 | - |
| Msm sexual debut at 15-17 years | - | 46.6 | - | - | 33.1 | - |
| Comprehensive knowledge on hiv | 58.1 | 59.5 | 47.6 | 42.5 | 45.5 | 42.6 |
| Aware that unprotected sex can cause hiv | 98.4 | 98.7 | 95.4 | 95.1 | 96.6 | 95.4 |
| Knows that ccu protects against hiv | 90.4 | 92.8 | 94.5 | 91.2 | 91.2 | 91.1 |
| Regular male partner | 91.8 | 78.5 | - | 62.2 | 54.3 | - |
| Ccu with regular male partner | 39.9 | 32.3 | - | 28.9 | 50.4 | - |
| Regular female partner | - | 46 | 82.1 | - | 48.2 | - |
| Ccu with regular female partner | - | 14 | 25.6 | - | 24.7 | - |
| Regular hijra partner | - | 61.4 | - | - | 21.8 | - |
| Ccu with regular hijra partner | - | 29.3 | - | - | 54.3 | - |
| Male/Hijra partner | - | - | 9.4 | - | - | 6.8 |
| CCU with Male/Hijra partner | - | - | 54.4 | - | - | 35.9 |
A clear knowledge-behavior gap exists when it comes to safe sexual practices in Odisha. While the comprehensive knowledge about HIV was more than that of the national average in all HRG, the proportion of FSWs having regular male partners or the proportion of MSM having regular transgender partner was the highest in Odisha. Concurrently, the proportion of consistent condom usage (CCU) with the regular partners was less than 35% among MSM and about 40% among FSWs. While about 46.8% of FSW and 40.5% MSM reported alcohol consumption during or before sex; in addition, about 2.5 % and 1.25% of the FSWs and MSM reported using shared needles for IDU practices. Such unsafe high-risk sexual and non-sexual practices among the HRG might pose severe threats of disease transmission among HRGs which might as well reflect among the general population through the bridge population, if left unaddressed.
Low Literacy: The NFHS-4 highlights the poor literacy rates among the general population in Odisha, particularly among women, as compared to the Southern states of India.8 Education reflects on other factors including age of marriage, childcare, personal hygiene and economy. For instance, the districts with less than 50% female literacy rate had higher proportion of child marriage (≥ 30%) and adolescent pregnancies (≥ 10%). Low economic status, early marriage and ignorance due to poor literacy might lead to their sexual exploitation leading to higher infection risks.28
ART Adherence: The National AIDS Control Organization (NACO) recommends timley ART linkage and continued adherence ensures complete eradication of HIV transmission. While referral and linkage to ART is substantially progressive, adherence to ART is a major issue faced by the OSACS in Odisha.22 While the FSWs are well aware of potential vertical transmission of HIV,25 the status of the same among the general population is unknown. Creating appropriate awareness and psychological support on the long-term effects of HIV infection among the general population and all HRGs might lead to improvised adherence to ART.31 Other factors related to ART non-adherence are duration of ART, opportunistic infections, the cost of travel to the ART centre or inaccessibility to the facility or loss of contact of the affected person and prevailing social stigma.32,33 Recent reports suggest absence of enabling environment in Odisha for providing adequate care and treatment from the healthcare professionals.34 Appropriate measures to improve ART adherence will also reduce the disease transmission.
4.3. Limitations and Recommendation for Further Studies
As the designated sentinel sites of the HSS are government-based ANC since, the study is limited only to those pregnant mothers attending the government ANCs. With a large tribal population, only about 85% of the child-births occur institutionally. Most tribal communities resist external interventions during child-births and traditional home-delivery practices are still widely prevalent.35 Traditional health providers, who offer home-delivery practices and pregnant women attending private ANCs should be included in the HSS, inorder to achieve uniform representation of all pregnant mothers in Odisha. A correlation between HIV prevalence and low socio-economic status and occupation and migration of the spouse has been established. However, the study lacks data on key behavioural and background characteristics of the respondents such as the HIV status of the spouse of the respondents, migration status of the respondents, accessibility to health care services, comprehensive knowledge of pregnant mothers on HIV, mother-to child transmission, adherence to ART, stigmatised attitude towards HIV positivity. Inclusion of these data might be helpful for future interventions.
5. Conclusion and Global Health Implications
Women whose spouses were either non-agricultural labourers, truck drivers or migrants also needed focused intervention programmes for prevention and mangement of HIV. While the joint efforts of NACO, Odisha SACS has been successful in providing adequate information and creating awareness on HIV and its prevention, still, there is a long way to go in terms of the disease management. Single male migrant specific interventions are recommended to halt the disease progression among vulnerable populations, such as their spouses or partners. Further, state-level interventions to improve the literacy rate of the residents of Odisha will be instrumental in improvising the overall quality of life of the people of Odisha State, India, including HIV prevention and management.
Migration due to poverty and its impact on sexually transmitted diseases have been documented globally. Migrants from low and middle income countries working in high income countries facing discrimination and lack of access to health care facilities have been reported. More research on prevention and treatment interventions among migrants is required to improve the HIV outcomes of migrants.
Acknowledgements:
The authors wish to thank the Project Director of Odisha State AIDS Control Society for their support in completing the surveillance activities in a timely manner. The authors also express their gratitude to the concerned Referral Laboratories, State Surveillance Team members and sentinel sites personnel.
Compliance with Ethical Standards
Conflicts of Interest: The author(s) declared that no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding/Support: The corresponding author received funding from National AIDS Control Organization (NACO) for conducting the HIV sentinel surveillance in the state of Odisha. Permission has also been received for authorship and publication of this article.
Ethics Approval: Ethical approval was exempted as this is a surveillance activity, where the HIV test is anonymous and the results were not used for the purpose of determining the HIV status of a person. The participants were, however, informed about the purpose of the study. The same is endorsed in Item No. 6 under Chapter-III of the India HIV act 2017.
References
- Eliminating HIV &AIDS in India: A roadmap to zero new HIV infections, zero discrimination &zero AIDS-related deaths. Indian Journal of Medical Research. 2016;144:789-92.
- [Google Scholar]
- 2018. HIV Estimations 2017: Technical Report. Available from:http://naco.gov.in/sites/default/files/HIV Estimations 2017 Report_3.pdf
- Declining Trends in HIV Prevalence Among Women Attending Antenatal Care Clinics Obfuscate the Continued Vulnerability of Adolescent Girls in Maharashtra, India (2005-2017) Journal of Acquired Immune Deficiency Syndromes. 2019;82(1):e13-e17.
- [Google Scholar]
- Stabilizing HIV prevalence masks high HIV incidence rates amongst rural and urban women in KwaZulu-Natal, South Africa. International Journal of Epidemiology. 2011;40(4):922-930.
- [Google Scholar]
- Sustained progress, but no room for complacency:Results of 2015 HIV estimations in India. Indian Journal of Medical Research. 2017;146(1):83.
- [Google Scholar]
- HIV/AIDS in India:An overview of the Indian epidemic. Oral Diseases. 2016;22:10-14.
- [Google Scholar]
- National Family Health Survey (NFHS-4), India, 2015-16: Odisha. Mumbai: IIPS; 2017.
- Planning for sustainable tribal development a case study of the Kondh tribe of the Kodhmal district Orissa. 2013. Shodhganga :a reservoir of Indian theses. Available from: http://hdl.handle.net/10603/91076
- [Google Scholar]
- Climate change and its worst effect on coastal Odisha: An overview of its impact in Jagatsinghpur District. IOSR Journal of Humanities and Social Science. 2018;23(1):1-15.
- [Google Scholar]
- Annual HIV Sentinel Surveillance, Country Report, 2008-09. New Delhi: NACO, Ministry of Health and Family Welfare Government of India; 2009.
- Utilization of the prevention of parent-to-child transmission of HIV (PPTCT) services in a tertiary care hospital, Odisha, India. Bangladesh Journal of Medical Science. 2014;13(2):163-9.
- [Google Scholar]
- A study on prevalence of HIV infection among pregnant women attending antenatal clinic in a tertiary care hospital, Cuttack, India. International Journal of Community Medicine and Public Health. 2017;4(5):1504-1509.
- [Google Scholar]
- Operational Manual for Sentinel Sites. New Delhi: NACO, Ministry of Health and Family Welfare, Government of India; 2014.
- Irrigation, agriculture, Livelihood and poverty linkages in Odisha. Agricultural Economics Research Review. 2012. 2012;25(1):99-105.
- [Google Scholar]
- Climate migrants and urban adaptation in India and China. In Workshop in International Public Affairs, 2016 [39 Pages]. Available from: http://www.shram.org/uploadFiles/20170808032447.pdf
- [Google Scholar]
- Climate Change and Climate-Induced Disasters in Odisha , Eastern India :Impacts , Adaptation and Future Policy Implications. International Journal of Humanities and Social Science Invention. 2016;5(8):60-63.
- [Google Scholar]
- Dynamics of tribal migration in undivided Koraput district of Odisha , India. International Journal of Academic Research and Development. 2017;2(4):585-587.
- [Google Scholar]
- Migration of Labour in Kalahandi District of Odisha. Arts and Social Sciences Journal. 2019;10(430):2.
- [Google Scholar]
- The Role of Origin and Destination Site in HIV Risk of Male Migrant Laborers in India [Internet] ProQuest Dissertations and Theses 2016
- [Google Scholar]
- Migration and HIV in India: Study of select districts. 2011. New Delhi UNDP, NACO, and Population Council. http: //www.undp.org/content/dam/india/docs/migration_and_hiv_in_india__study_of_select_districts.pdf
- [Google Scholar]
- Annual Report 2016-17. In: Odisha State AIDS Control Society. Bhubaneshwar: OSACS, Department of Health and Family Welfare, Government of Odisha; 2017.
- [Google Scholar]
- Gharkhia System in Western Odisha. Journal of Land and Rural Studies. 2017;5(1):50-66.
- [Google Scholar]
- Circular Migration:A Reflection from KBK Districts, Odisha. Political Economy Journal of India. 2017;24(1):27-36.
- [Google Scholar]
- National Integrated Biological and Behavioural Surveillance (IBBS) 2014-15 High Risk Groups [Internet] 2014. NACO, Ministry of Family Health and Welfare, Government of India. New Delhi:NACO, Ministry of Family Health and Welfare, Government of India. [Pages 308] Available from: http://naco.gov.in/sites/default/files/IBBS Report 2014-15.pdf
- [Google Scholar]
- HIV and adolescents: focus on young key populations. Journal of the International AIDS Society. 2015;18(2Suppl 1):20076. doi:10.7448/IAS.18.2.20076
- [Google Scholar]
- Placing Young Women at the Centre:Reducing Young Women's Vulnerability to HIV in India 2007
- A study on violence against women in India. Social Science International. 2013;29(1):11-18.
- [Google Scholar]
- A Research Study On Migrant Tribal Women Girls in Ten Cities :A Study of Their Socio-Cultural and Economic Reference to Social Intervention. Sadar: Planning Commission, Government of India; 2003.
- Migration of Tribal Women: Its Socio-economic Effects-An in-depth Study of Chhatisgarh, Jharkhand, MP and Orissa. New Delhi: Planning Commission Government of India; 2010.
- [Google Scholar]
- Nonadherence to anti-HIV medication is associated with higher level of anxiety:Experience from a tertiary care hospital of Odisha. Indian Journal of Pharmacology. 2015;47(6):672-675.
- [Google Scholar]
- Determinants contributing for poor adherence to antiretroviral therapy:A hospital record-based study in Balasore, Odisha. Journal of Family Medicine and Primary Care. 2019;8(5):1720-1724.
- [Google Scholar]
- A study of adherence to antiretroviral therapy in a tertiary care hospital at Allahabad, India. Indian Journal of Sexually Transmitted Diseases and AIDS. 2019;40(1):46-50.
- [Google Scholar]
- Docs 'negligence kills foetus of HIV +woman at PRMMCH. 2019. Updated December 15. https: //www.orissapost.com/docs-negligence-kills-foetus-of-hiv-woman-at-prmmch/
- [Google Scholar]
- Beyond the template: the needs of tribal women and their experiences with maternity services in Odisha, India. International Journal for Equity in Health. 2018;17(1):1-3.
- [Google Scholar]





