Translate this page into:
The Health Determinants of Accessibility to Clubfoot Treatment in LMICs: A Global Exploration of Barriers and Solutions
*Corresponding author email: sharaf554@gmail.com
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Background:
Clubfoot or Congenital Talipes Equinovarus (CTEV) treatment in newborn infants involves simple, non-invasive manipulation and is primarily managed non-surgically if identified early. In low- and middle-income countries (LMICs), less than 15% of patients with CTEV access treatment. This cross-sectional questionnaire study conducted descriptive and regression analysis of institutional reasons for CTEV management in LMICs.
Methods:
A cross-sectional study was undertaken of 1,489 medical institutions in 62 LMICs. Data were evaluated from the “World Health Organization Situation Analysis tool” database. We analyzed characteristics of institutions that manage and did not manage CTEV. With the use of a multivariate linear regression model, we identified a set of factors linked to referral for non-management of CTEV.
Results:
A total of 72.7% (1,083/1,395) of institutions surveyed did not manage CTEV. The most common reason cited for not managing CTEV was a lack of sufficient skills, 92.1% (668/725, P<0.001). A total of 39.4% (286/725) of institutions also cited a lack of functioning equipment as a reason. Multivariate linear regression analysis showed lack of training, lack of supplies, and lack of functioning equipment were most closely related to non-management of CTEV.
Conclusion and Global Health Implications:
We identified that failure to manage CTEV may result from a lack of skills and medical equipment. Increasing the capacity of sustainable training programs may reduce the presently available skill deficit in treating CTEV in LMICs and provide improved health outcomes for those with CTEV. While considerable progress has been made in building capacity for the treatment and management of CTEV in LMICs, structured training programs that support conservative manipulative methods to manage CTEV should be initiated globally.
Keywords
Clubfoot
Accessibility
Health Determinants
Global
Barriers to Care
Treatment
1. Introduction
Clubfoot or Congenital Talipes Equinovarus (CTEV) is one of the most common pediatric congenital orthopedic conditions, estimated to occur in 1-2 per 1,000 live births.1 While the severity may vary from mild to severe deformity of the feet, early detection and treatment within the first few weeks of birth provides the best chance for non-surgical intervention. The Ponseti method, the most commonly practiced non-surgical approach, involves manipulating the child’s foot into a plantigrade position through the use of casts or braces which align the joint into the correct anatomical position. Significant lifetime disability may result if left unmanaged and in a proportion of patients the Ponseti method does not fully correct the defect and surgical intervention is required.1,2 Other indications for surgical management include syndromic, neurogenic CTEV, and neglected idiopathic CTEV.3,4 Over the last decades, the Ponseti method has spread globally to over 100 countries and has dramatically improved the prognosis of CTEV.5
New indicators have shown high rates of unmet care for CTEV in LMICs via estimates of backlogs for nonfatal conditions requiring surgical treatment.6 Despite being able to be managed non-surgically with basic training if identified early, less than 15% of patients with CTEV undergo treatment in LMICs.7 While considerable progress has been made in building capacity for the treatment and management of CTEV in LMICs, more research is required to understand the state of CTEV treatment globally, as well as to understand the characteristics of institutions that are and are not providing CTEV management.
The purpose of this study was to conduct a global survey to evaluate whether institutions provide management of CTEV and examine the characteristics of institutions that are and are not providing CTEV management. Using the World Health Organization Situational Analysis Tool, we performed an analysis of the management and reasons for non-management of CTEV in 62 LMIC countries and 1,489 medical institutions. This study also evaluated the types of hospitals not managing CTEV and the reasoning behind their referral to higher leveled institutions. Such information may be useful to current and future training programs aiming to address the global burden of CTEV.8
2. Methods
This is a cross-sectional study developed using the World Health Organization (WHO) Situational Analysis Tool database, created to assess the availability and capacity of Emergency and Essential Surgical services in LMICs. The database, compiled at the World Health Organization from 2007 until 2016 by the Essential and Emergency surgical care research group in Geneva, Switzerland, includes a convenience sample of 1,489 institutions from LMICs. It contains a total of 108 data points of entry to address four core sections: infrastructure, healthcare personnel, surgical equipment, and the availability of surgical interventions in participating countries. The data was collected by WHO country offices, ambassadors of the WHO Essential and Emergency surgical care research group, and the Ministries of Health representatives. These groups of individuals requested responses from each of the health care facilities. Participating hospitals used an online or a paper questionnaire. Questions were based on the WHO Tool for Situational Analysis to Assess Emergency and Essential Surgical Care survey can be found in the WHO Integrated Management for Emergency & Essential Surgical Care.8,9 IRB approval was not required as patient-level information was not included in the database.
2.1. Study Sample
Between January 1, 2007 and December 31, 2016, we identified hospitals that responded and did not respond to the portion of the WHO related to CTEV management. The survey primarily characterized hospitals responding as either (1) treating CTEV or (2) not treating CTEV, and those (3) not responding to the CTEV management section. Among the hospitals responding, we also captured hospital characteristics, specific reasons for not treating CTEV, namely (1) lack of training, (2) lack of medical supplies/drugs, and (3) lack of functioning equipment, in addition to the type of hospital, ranging from Level 1 to Level 3. According to the World Health Organization (WHO), Surgical Care at the District Hospital guidelines, Level 1 (Small Hospital or Health Center) is defined as a hospital with a small number of beds, the ability to perform minor procedures, and the availability of oxygen concentrator. Level 2 (District/Provincial Hospital) is defined as the first referral hospital of 100-300 beds with the ability to perform the same as Level 1, with the addition of complete anesthesia, resuscitation, and airway management system including oxygen concentrators (cylinder), and pediatric anesthesia systems. Level 3 (Referral Hospitals) is defined as a hospital with greater than 300 beds, basic intensive care facilities, the ability to perform the same as Levels 1 and 2 with the addition of pediatric and neonatal surgery, facial and intracranial surgery, and bowel surgery, among other interventions.10
A comparative analysis to evaluate characteristics of institutions responding to the CTEV section of the survey was conducted to evaluate for survey bias. Next, descriptive analysis was conducted, including frequencies and proportions by associated country of each hospital institution treating CTEV, as well as based on the type of hospital. We utilized a multivariate linear regression technique, a statistical modeling approach to evaluate the key factors for hospitals associated with management vs non-management of CTEV. This regression analysis was conducted based on the following independent variables, namely lack of skills, lack of function equipment and lack of supplies/drugs, with a single dependent outcome variable being treatment vs nontreatment of CTEV. All tests of hypotheses were two-tailed with a type-1 error rate set at 5%. All statistical analyses were performed using SPSS IBM version 23 (Armonk, NY, USA). The institutional review board determined this study as exempt as the study uses institutional-level data.
3. Results
A total of 1,489 LMIC health care facilities were examined. Facilities included district hospitals, health centers, private hospitals, sub-district community hospitals, general and provincial hospitals. A median of 5 hospitals or health care institutions responded per country included in the analysis. Not all medical institutions of each country responded to the questionnaire. Comparative analysis was conducted of institution respondents vs non-respondents, summarized in Table 1.
| Level of Hospital | Responding Institutions | Non-Responding Institutions | Comparison |
|---|---|---|---|
| N (%) | N (%) | P-value | |
| Level I | 1113 (74.7) | 345 (62.2) | < 0.001 |
| Level II | 230 (15.4) | 118 (21.3) | |
| Level III | 146 (9.8) | 92 (16.6) | |
| Type of Hospital | N (%) | N (%) | |
| District Hospital | 47 (3) | 21 (4) | < 0.001 |
| District/Rural/Community Hospital | 294 (20) | 78 (15) | |
| General Hospital | 122 (8) | 69 (13) | |
| General/Teaching Hospital | 46 (3) | 28 (5) | |
| Health Center | 345 (24) | 131 (24) | |
| Private/NGO/Mission Hospital | 253 (17) | 86 (16) | |
| Provincial Hospital | 89 (6) | 48 (9) | |
| Sub-district/Rural/Community | 261 (18) | 76 (14) | |
| Type of Country | N (%) | N (%) | |
| Low Income Country | 412 (28) | 171 (32) | 0.162 |
| Low- and Middle-Income Country | 1077 (74) | 384 (72) | |
Statistically significant differences were found between respondents and non-respondents based on the level of the institution and type of hospital - as level 1 institutions and district hospitals were more likely to respond.
A total of 1,395 institutions sufficiently responded to the initial portion questionnaire in which they reported whether they did or did not treat CTEV. 21.0% (312/1,395) of institutions provided treatment for CTEV while 72.7% (1,083/1,395) of institutions did not manage CTEV (Figure 1). Management differed among the level of facilities with level 3 institutions being more likely to facilitate CTEV treatment compared to non-level 3 institutions (OR 12.3, 95 % CI: 8.28 to 18.26) (Table 2). In total, 725 (725/1,083) of the participating institutions highlighted specific reasons for non-management.
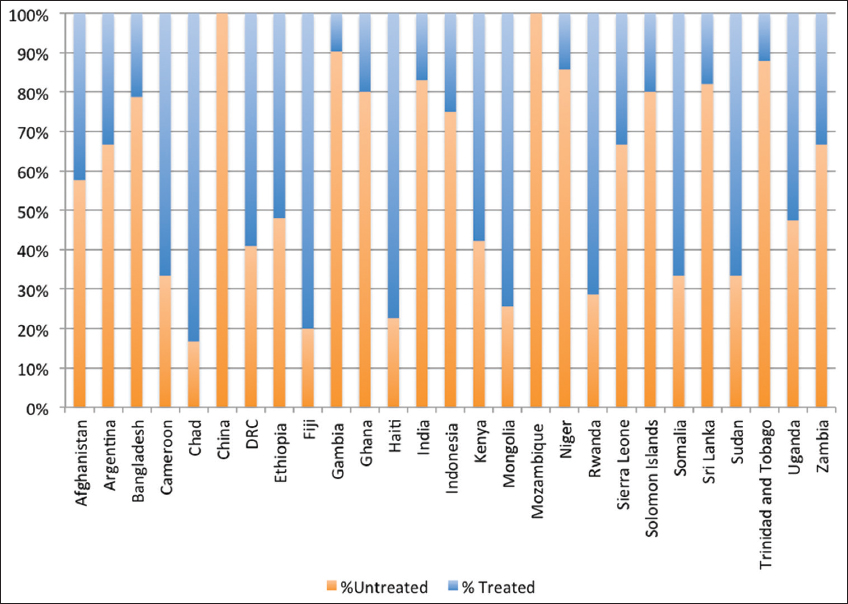
- CTEV vs non-CTEV management by Country
| Level 1 | Level 2 | Level 3 | CTEV Treated | CTEV Not Tx - Ref | CTEV Not Tx - Not Ref | CTEV Skills | CTEV Equip | CTEV Supplies | ||
|---|---|---|---|---|---|---|---|---|---|---|
| Afghanistan | LIC | 16 | 4 | 6 | 9 | 11 | 4 | 8 | 3 | 4 |
| Argentina | MIC | 5 | 3 | 1 | 4 | 4 | 1 | 2 | 1 | 0 |
| Bangladesh | LIC | 251 | 9 | 9 | 26 | 169 | 63 | 145 | 82 | 83 |
| Cameroon | MIC | 1 | 2 | 0 | 2 | 1 | 0 | 1 | 1 | 1 |
| Chad | LIC | 3 | 0 | 3 | 5 | 0 | 1 | 1 | 0 | 0 |
| China | MIC | 1 | 0 | 7 | 0 | 0 | 8 | 0 | 0 | 0 |
| DRC | LIC | 8 | 10 | 1 | 10 | 9 | 0 | 9 | 8 | 7 |
| Ethiopia | LIC | 13 | 8 | 2 | 11 | 5 | 5 | 4 | 0 | 0 |
| Fiji | MIC | 1 | 2 | 2 | 4 | 1 | 0 | 0 | 0 | 0 |
| Gambia | LIC | 69 | 6 | 0 | 2 | 44 | 17 | 36 | 19 | 14 |
| Ghana | MIC | 18 | 4 | 0 | 2 | 19 | 1 | 19 | 8 | 7 |
| Haiti | LIC | 38 | 15 | 1 | 23 | 21 | 5 | 14 | 3 | 3 |
| India | MIC | 211 | 20 | 13 | 26 | 96 | 103 | 86 | 26 | 42 |
| Indonesia | MIC | 3 | 0 | 1 | 1 | 2 | 1 | 1 | 1 | 1 |
| Kenya | LIC | 81 | 31 | 17 | 36 | 81 | 8 | 64 | 47 | 45 |
| Mongolia | MIC | 36 | 4 | 3 | 3 | 22 | 6 | 21 | 14 | 10 |
| Mozambique | LIC | 2 | 2 | 0 | 0 | 3 | 1 | 3 | 0 | 0 |
| Niger | LIC | 15 | 3 | 3 | 3 | 14 | 4 | 12 | 2 | 5 |
| Rwanda | LIC | 0 | 2 | 5 | 5 | 1 | 1 | 1 | 0 | 1 |
| Sierra Leone | LIC | 7 | 4 | 1 | 2 | 8 | 2 | 6 | 0 | 0 |
| Solomon Islands | MIC | 8 | 1 | 1 | 2 | 8 | 0 | 8 | 1 | 1 |
| Somalia | LIC | 10 | 4 | 1 | 10 | 4 | 1 | 2 | 0 | 1 |
| Sri Lanka | MIC | 33 | 5 | 1 | 1 | 27 | 5 | 16 | 9 | 8 |
| Sudan | MIC | 0 | 3 | 0 | 2 | 1 | 0 | 1 | 1 | 1 |
| Trinidad and Tobago | MIC | 52 | 1 | 1 | 0 | 39 | 13 | 33 | 12 | 21 |
| Uganda | LIC | 27 | 9 | 2 | 10 | 24 | 4 | 21 | 10 | 9 |
| Zambia | MIC | 0 | 6 | 3 | 2 | 5 | 1 | 3 | 0 | 0 |
| Other Countries | 205 | 72 | 62 | 111 | 152 | 57 | 151 | 38 | 23 | |
| Total | 1113 | 230 | 146 | 312 | 771 | 312 | 668 | 286 | 287 | |
The most commonly cited reason for not managing CTEV was a lack of sufficient clinical skills, 92.1% (668/725). Skills ranged from conservative and surgical approaches to management. 39.4% (286/725) of institutions also cited lack of functioning equipment as a reason. Further, 39.6% (287/725) of institutions also cited lack of medical supplies/drugs as a reason for not treating CTEV. Lack of clinical skills significantly affected the treatment of CTEV in hospitals in low- and middle-income countries (P<0.050). There was a significant positive correlation between lack of skills and non-CTEV management by a rate of 58% based on multivariate linear regression analysis (Figure 2, Table 3). Multivariate linear regression analysis showed that among multiple reasons for non-management of CTEV, that a lack of clinical skills is the primary correlating factor with non-CTEV management.
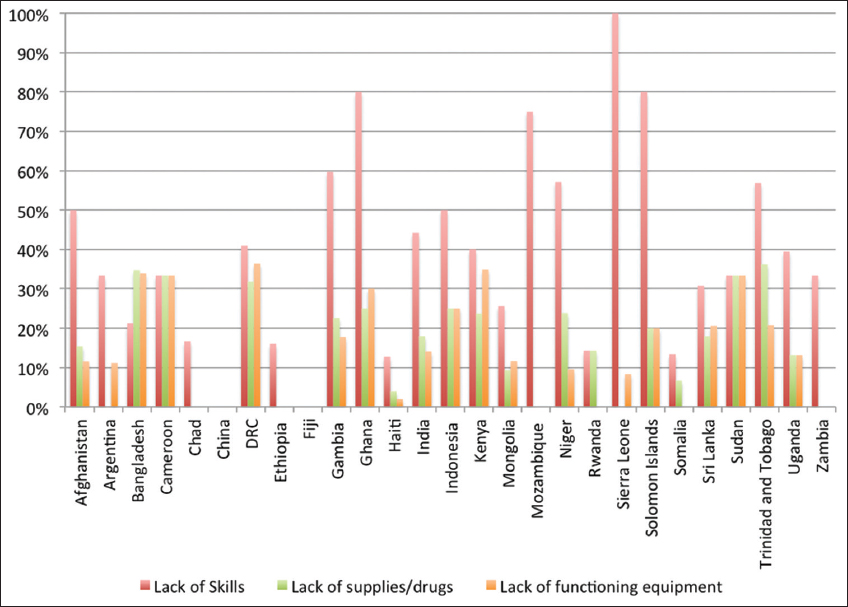
- Breakdown of The Driver for Lack of CTEV Treatment by Country
| LCL | UCL | t Stat | p-value | |
|---|---|---|---|---|
| Lack of Skills | 0.19 | 0.98 | 3.03 | 0.006 |
| Lack of Functioning Equipment | -2.21 | 0.84 | -0.93 | 0.360 |
| Lack of Supplies/Drugs | -0.87 | 2.16 | 0.88 | 0.389 |
| ANOVA | d.f. | SS | MS | F [p-value] |
| Regression | 3.00 | 0.56 | 0.19 | 3.38 [0.036] |
Multivariate linear regression analysis: Factors in CTEV Non-Management % Untreated = 0.36287 + 0.58292 * Lack of Skills - 0.68894 * Lack of functioning equipment + 0.64438 * Lack of supplies/drugs
4. Discussion
4.1 Discussion
This study highlights institutions in low and middle-income countries that lack sufficient management of CTEV. The Ponseti method offers a non-invasive and cost-effective method of treatment to those across the globe, especially in LMICs.11
The method has become widely accepted as the gold standard of treatment and has rapidly spread across the globe, drastically improving the care of those with CTEV.5 Despite this, there continue to be disparate levels of treatment across LMICs, especially within local and district hospitals. Our analysis reveals that a lack of appropriate skills in handling the treatment of CTEV is the most common reason for a lack of treatment and subsequent referral to another institution from level 1 and 2 institutions. The lack of appropriate equipment and medical supplies were also cited as common reasons for the non-treatment of CTEV. Despite being able to be managed with minimal, non-surgical training, a large proportion of patients are not being treated in local or district hospitals in LMICs. Multiple barriers exist to proper care include financial barriers for the hospital and patient, lack of parental knowledge of the disease, and lack of follow-up.12–16 Follow up has been shown to be influenced by transportation availability and costs, proper brace use, and perceived health status among other factors.17
4.2. Training Programs
This study further supports the notion that the major challenge for the availability of surgical services for children in LMICs worldwide is the low-skilled workforce and appropriate infrastructure.6,18,19 A recent Zambian study using the WHO SAT tool also demonstrated that lack of surgical skill was the leading factor in limiting the availability of 93% of pediatric procedures.20 We further confirmed this notion in our analysis which revealed a significant correlation between lack of skills and the non-treatment of CTEV at a rate of 86.1%. Addressing the lack of a skilled workforce is paramount in the proper treatment of CTEV across the globe. Training programs specific to CTEV have been previously explored and have been reported to significantly increase the proper use of the Ponseti method globally.21 Programs such as the early nationwide manipulation of CTEV established in Malawi’s 25 health districts have already proven to be successful. One year following the intervention, 20 out of the 25 clinics that were created were still operational and had successfully managed over 300 patients (out of 482 cases of CTEV, 327 were corrected to the plantigrade position).22 Similar training programs for other low-cost technologies such as ultrasound used in low- and middle-income countries have also proven to be successful. 12,23
Training programs that focus specifically on non-invasive methods of treating CTEV have proven to be efficacious. However, CTEV cases in LMICs have been reported to have the highest rates of disease relapse and follow-up in previous training programs have been minimal.21,24 Addressing the root causes of relapse must be a priority in any educational program. Solutions identified in a systematic review of 24 studies examining CTEV barriers in LMICs were primarily education, in addition to financial assistance, for the patient and providers.17 As the Ponseti method includes serial casting, consistent follow-up is of the utmost importance. However, one of the highest barriers to care is the financial and temporal cost of travel to CTEV clinics. Subsequently, mapping the locations of Ponseti clinics has been suggested to understand the further current burden of travel on patients within LMICs. The formation of strategically placed clinics in low-access areas may help reduce transportation costs and increase the access and continuation of care. In addition to reducing transportation costs, the standardization of correct CTEV management must also be encouraged. This has been studied extensively and the six best practices to ensure sustainability in CTEV training programs have been elucidated. These include diagnosing CTEV early, organizing high volume Ponseti casting centers, the use of non-physician health workers, engaging families care, reducing barriers to access, and providing follow-up. 25
4.3. Lack of Supplies
Our analysis highlights a correlation between lack of medical equipment and insufficient treatment of CTEV. Many institutions reported damaged or faulty materials including plaster casts and braces, which are essential to the proper non-surgical approach to CTEV treatment. This lack of supplies has placed a higher burden on patients and providers in the acquisition of appropriate care. A previous study was in agreeance with this finding, showing that out of a population of 27 LMICs, only 67% had access to splints/braces all of the time.17 In contrast with the rest of the cohort where the lack of adequate skills was the primary cited reason for the non-management of CTEV, level 1 hospitals in Bangladesh cited the lack of medical supplies as their leading cause. Bangladesh has one of the highest rates of idiopathic CTEV, reporting over 5000 new cases per annum.26,27
This could suggest that the high rate of CTEV puts significant pressure on the clinical material available for each patient, such as material available for plaster casts. Furthermore, in an initiative named the Bangladesh Sustainable Clubfoot Project, Walk for Life (WFL), 13% of CTEV cases were noted to be atypical requiring special casts, furthering material costs.26 WFL consisted of 35 clinics involving overseas experts training a team of national paramedical staff including physiotherapists and non-medics. All cases underwent Ponseti casting and a total of 3,922 patients were successfully treated between 2009 and 2011. With a low complication rate of 2%, the program provides evidence for the notion that physiotherapists, paramedics and non-medics can be trained to deliver clubfoot manipulative treatment with good outcomes.
The treatment that the Ponseti method offers is often considered highly cost-effective with a ratio of USD 22.46 per disability-adjusted life year averted. Despite this, 60% of the participants in WFL reported that the material costs of USD 40 were unaffordable. This highlights that despite the relatively “low-cost” and high cost-effectiveness, barriers continue to exist in terms of accessing proper CTEV care, even when treatment is available.28 The WFL program was especially successful as the non-governmental organization was welcomed with local and government support and was provided free of cost to patients and their families.
4.4. Possible Solutions
Results from studies examining CTEV management in LMICs using the Ponseti method have demonstrated that the use of local material and craftsmen are important to maintain the stability of clinical material production and use.26,29–31 A Steenbeek foot abduction brace made by local Kenyan craftsmen was trialed in 233 patients and was shown to increase rates of compliance, decrease discomfort, and reduce complications as compared to the widely used, low-cost, Dennis Brown brace.32 Increasing the rates of Steenbeek braces will likely help to develop the necessary CTEV workforce and reduce foreign material aid dependence – creating local, low-cost, and sustainable programs. It has also been shown that the use of recyclable plaster casts can also reduce the cost of equipment and increase the availability of CTEV braces and treatment.17
4.5. Building Sustainable Infrastructure
Ultimately, external interventions are often required to meet the financial needs of both the patient and practitioner in order to address shortfalls such as costs of transportation to health care facilities and clinical materials. Proper CTEV management in the context of service delivery in a national health system was shown to be successful in the Uganda sustainable CTEV program. Practitioners, medics, and non-medics participated in structured training programs on manipulative conservative techniques and were shown to improve CTEV outcomes. Non-governmental organizations have also played a vital role in the proper care of individuals with CTEV.30 In 2007 a collaboration of non-governmental organizations and ministers of health established a national training program across 10 different countries. Overall, 110 CTEV clinics were formed consisting of 643 trained practitioners in which 7,705 children were treated over a three-year span. The model was found to be successful and further supports the validity of training programs.33
Overall, this analysis highlights that lack of skills and effective medical equipment to manage CTEV are important contributory factors for the non-management of CTEV in LMICs. The importance of these factors compared to other parameters such as lack of interest, poor financial compensation, previous poor results or advanced disease on presentation to level 1 and 2 hospitals should also be explored in further studies. A recent study highlighted the importance of succinct surgical referrals and a process to monitor dropout rates of patients as an important factor for improved clubfoot management.34 Although it is impossible to conclude a direct link with lack of skills and lack of equipment from a snapshot study of institutions that responded to the WHO SAT questionnaire, our study does provide a strong correlation and proposed direction in managing the global burden of CTEV.
4.6. Strengths and Limitations
Although there have been previous reports assessing the strength of CTEV training programs, this is the first study to assess the CTEV surgical capacity in multiple LMICs worldwide using the WHO SAT tool. This study has highlighted targets for policy in specific LMICs. Limitations include the retrospective collection of data via the WHO situational analysis tool. The study is only a snapshot of institutions that filled out the tool and may not be fully representative of the demographics of the entire country and region in general. Furthermore, as the sampling strategy was based on all participating invited survey participants that actively answered the survey and were WHO institution affiliated hospitals, there may be a lack of representation from specific countries. There may also be reporting bias in responding vs non-responding institutions and WHO-institution affiliated vs unaffiliated hospitals.
The type of facility also needs to be considered. Despite CTEV being listed as an essential intervention in the WHO Surgical Care at the district hospital publication, depending on the institution specialized CTEV care may not be expected to be available at primary referral facilities. Since most of the SAT data comes from primary referral facilities, in some instances this may impact the representation of CTEV management. As a result, responding institutions may not be representative of the entire health care treatment options of that country. Also of note, the SAT data were collected over a 10-year period and CTEV management has changed gradually as adoption of the Ponseti technique has spread. Those centers reporting that they were unable to manage CTEV at the start of the data collection period may now be able to, due to the availability of Ponseti training courses and materials. Isolated centers that advocate and use the Ponseti technique may not be captured by the SAT data.
5. Conclusion and Global Health Implications
This study adds further insight into the insufficient level of proper CTEV management in LMICs. Lack of clinical skills and physical materials were often cited as reasons for the nontreatment via the Ponseti method. Structured training programs that support conservative manipulative methods to manage CTEV would serve well in LMIC medical institutions and should be encouraged globally.27,29,35,36 We also raise the importance of furthering training programs that focus on addressing long-term recovery and follow-up in order to reduce the significant CTEV treatment deficit in LMICs.
Acknowledgments:
There is nothing to report.
Compliance With Ethical Standards
Conflicts of Interest: The authors declare no conflicts of interest.
Financial Disclosure: There is nothing to disclose.
Funding/Support: None.
Ethics Approval: There is no patient-level information included within this study, thus no ethical approval has been pursued in this study.
Disclaimer: None.
References
- Clubfoot:etiology and treatment. Indian J Orthop. 2008;42(1):22. doi:10.4103/0019-5413.3ↀ
- [Google Scholar]
- Congenital idiopathic clubfoot:prevention of late deformity and disability by conservative treatment with the Ponseti technique. Pediatr Ann. 2006;35(2):128-136. doi:10.3928/0090-4481-20060201-13
- [Google Scholar]
- Correction of neglected idiopathic club foot by the Ponseti method. J Bone Joint Surg Br. 2007;89(3):378-81. doi:10.1302/0301-620X.89B3.18313
- [Google Scholar]
- Update on Clubfoot:Etiology and Treatment. Clin Orthop Relat Res. 2009;467(5):1146-1153. doi:10.1007/s11999-009-0734-9
- [Google Scholar]
- Worldwide spread of the Ponseti method for clubfoot. World J Orthop. 2014;5(5):585-90. doi:10.5312/wjo.v5.i5.585
- [Google Scholar]
- The burden of pediatric surgical conditions in low and middle income countries:a call to action. J Pediatr Surg. 2012;47(12):2305-2311. doi:10.1016/j.jpedsurg.2012.09.030
- [Google Scholar]
- The development of a training course for clubfoot treatment in Africa:Learning points for course development. BMC Med Educ. 2018;18(1):163. doi:10.1186/s12909-018-1269-0
- [Google Scholar]
- Validation of the World Health Organization tool for situational analysis to assess emergency and essential surgical care at district hospitals in Ghana. World J Surg. 2011;35(3):500-504. doi:10.1007/s00268-010-0918-1
- [Google Scholar]
- WHO 2011
- Surgical Care at the District Hospital. Pediatric Anesthesia. 2004;14(4):369. doi:10.1046/j.1460-9592.2003.01256.x
- [Google Scholar]
- Cost-effectiveness of club-foot treatment in low-income and middle-income countries by the Ponseti method. BMJ Glob Health. 2016;1(1):e000023. doi:10.1136/bmjgh-2015-000023
- [Google Scholar]
- Ponseti Brasil:a national program to eradicate neglected clubfoot - preliminary results. Iowa Orthop. 2011;31:43-8.
- [Google Scholar]
- Uganda Sustainable Clubfoot Care. Understanding the barriers to clubfoot treatment adherence in Uganda:A rapid ethnographic study. Disabil Rehabil. 2007;29(11-12):845-855. doi:10.1080/09638280701240102
- [Google Scholar]
- Barriers experienced by parents of children with clubfoot deformity attending specialised clinics in Uganda. Trop Doct. 2009;39(1):15-18. doi:10.1258/td.2008.080178
- [Google Scholar]
- Barriers experienced by service providers and caregivers in clubfoot management in Kenya. Trop Doct. 2015;45(2):84-90. doi:10.1177/0049475514564694
- [Google Scholar]
- Feasibility and barriers of treating clubfeet in four countries. Int Orthop. 2015;39(12):2415-22. doi:10.1007/s00264-015-2783-x
- [Google Scholar]
- The Ponseti method for clubfoot treatment in low and middle-income countries. J Pediatr Orthop. 2017;37(2):e134-e139. doi:10.1097/BPO.0000000000000723
- [Google Scholar]
- Surgical services for children in developing countries. Bull World Health Organ. 2002;80(10):829-35.
- [Google Scholar]
- Burden, need, or backlog:a call for improved metrics for the global burden of surgical disease. Int J Surg. 2014;12(5):483-486. doi:10.1016/j.ijsu.2014.01.021
- [Google Scholar]
- Pediatric emergency and essential surgical care in Zambian hospitals:a nationwide study. J Pediatr Surg. 2013;48(6):1363-1370. doi:10.1016/j.jpedsurg.2013.03.045
- [Google Scholar]
- The role of clubfoot training programmes in low- and middle-income countries:a systematic review. Trop Doct. 2020;50(4):291-299. doi:10.1177/0049475520931343
- [Google Scholar]
- Club foot treatment in Malawi –a public health approach. Disabil Rehabil. 2007;29(11-12):857-862. doi:10.1080/09638280701240169
- [Google Scholar]
- Trends in Ultrasound Use in Low and Middle Income Countries:A Systematic Review. Int J MCH AIDS. 2020;9(1):103-120. doi:10.21106/ijma.294
- [Google Scholar]
- What factors affect patient access and engagement with clubfoot treatment in low- and middle-income countries?Meta-synthesis of existing qualitative studies using a social ecological model. Trop Med Int Health. 2016;21(5):570-589. doi:10.1111/tmi.12684
- [Google Scholar]
- Clubfoot Care in Low-Income and Middle-Income Countries:From Clinical Innovation to a Public Health Program. World J Surg. 2014;38(4):839-848. doi:10.1007/s00268-013-2318-9
- [Google Scholar]
- The Bangladesh clubfoot project:The first 5000 feet. J Pediatr Orthop. 2013;33(4):e40-4. doi:10.1097/BPO.0b013e318279c61d
- [Google Scholar]
- The Bangla clubfoot tool:a repeatability study. J Foot Ankle Res. 2014;7(1):27. doi:10.1186/1757-1146-7-27
- [Google Scholar]
- Walk for life - the National Clubfoot Project of Bangladesh:The four-year outcomes of 150 congenital clubfoot cases following Ponseti method. J Foot Ankle Res. 2016;9:42. doi:10.1186/s13047-016-0175-0
- [Google Scholar]
- Management of idiopathic clubfoot after formal training in the Ponseti method:a multi-year, international survey. Iowa Orthop J. 2013;33:136-41.
- [Google Scholar]
- Towards effective Ponseti Clubfoot Care:the Uganda Sustainable Clubfoot Care Project. Clin Orthop Relat Res. 2009;467(5):1154-1163. doi:10.1007/s11999-009-0759-0
- [Google Scholar]
- Journal of Pediatric Orthopaedics Part B 2012
- Ponseti clubfoot management:Experience with the Steenbeek foot abduction brace. Paediatr Child Health. 2014;19(10):513-514. doi:10.1093/pch/19.10.513
- [Google Scholar]
- A collaborative public health approach to clubfoot intervention in 10 low-income and middle-income countries:2-year outcomes and lessons learnt. J Pediatr Orthop B. 2012;21(4):361-5. doi:10.1097/BPB.0b013e3283504006
- [Google Scholar]
- Indicators to assess the functionality of clubfoot clinics in low-resource settings:a Delphi consensus approach and pilot study. Int Health. 2018;10(5):340-348. doi:10.1093/inthealth/ihy033
- [Google Scholar]
- Initial program evaluation of the Ponseti method in Nigeria. Iowa Orthop J. 2012;32:141-9.
- [Google Scholar]
- Treatment of idiopathic clubfoot by ponseti technique of manipulation and serial plaster casting and its critical evaluation. Ethiop J Health Sci. 2012;22(2):77-84.
- [Google Scholar]





