Translate this page into:
Psychological Distress and Heart Disease Mortality in the United States: Results from the 1997-2014 NHIS-NDI Record Linkage Study
*Corresponding author email: hyunjung.lee0001@gmail.com
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Objective:
Despite the long-term decline, heart disease has remained the leading cause of death in the United States (US) over the past eight decades, accounting for 23% of all deaths in 2017. Although psychological distress has been associated with cardiovascular disease mortality, the relationship between different psychological distress levels and heart disease mortality in the US has not been analyzed in detail. Using a national longitudinal dataset, we examined the association between levels of psychological distress and US heart disease mortality.
Methods:
We analyzed the Kessler 6-item psychological distress scale as a risk factor for heart disease mortality using the pooled 1997-2014 data from the National Health Interview Survey (NHIS) linked to National Death Index (NDI) (N=513,081). Cox proportional hazards regression was used to model survival time as a function of psychological distress and sociodemographic and behavioral covariates.
Results:
In Cox models with 18 years of mortality follow-up, the heart disease mortality risk was 121% higher (hazard ratio [HR]=2.21; 95% CI=1.99,2.45) in adults with serious psychological distress (SPD) (p<0.001), controlling for age, and 96% higher (HR=1.96; 95% CI=1.77,2.18) in adults with SPD (p<0.001), controlling for age, gender, race/ethnicity, immigrant status, education, marital status, poverty status, housing tenure, and geographic region when compared with adults without psychological distress. The relative risk of heart disease mortality associated with SPD decreased but remained significant (HR=1.14, 95% CI=1.02,1.28) after controlling for additional covariates of smoking, alcohol consumption, self-assessed health, activity limitation, and body mass index. There was a dose-response relationship, with relative risks of heart disease mortality increasing consistently at higher levels of psychological distress. Moreover, the association varied significantly by gender and race/ethnicity. The relative risk of heart disease mortality for those who experienced SPD was 2.42 for non-Hispanic Whites and 1.76 for non-Hispanic Blacks, compared with their counterparts who did not experience psychological distress.
Conclusions and Global Health Implications:
US adults with serious psychological distress had statistically significantly higher heart disease mortality risks than those without psychological distress. These findings underscore the significance of addressing psychological well-being in the population as a strategy for reducing heart disease mortality.
Keywords
Psychological Distress
Heart Disease Mortality
NHIS-NDI
Longitudinal
Social Determinants
1. Introduction
Heart disease is the most costly health condition among leading chronic diseases.1 The estimated direct medical costs of heart disease for hospital, office-based provider visits, and prescribed medicine and indirect costs such as productivity lost or mortality totaled $204.8 billion in the United States during 2013-2014.1 Despite the long-term decline, heart disease has remained the number one leading cause of death in the US over the past eight decades, accounting for 23% of all deaths in 2017.2 Mortality from cardiovascular disease (CVD), including heart disease and stroke, is substantially higher among Blacks/African-Americans and individuals with lower socioeconomic status (SES) compared with Whites and those with higher SES, respectively.3,4 The major CVD risk factors include individual-level demographic and socioeconomic characteristics (e.g., racial/ethnicity, gender, marital status, income, education, occupation, employment, place of residence), health behaviors (e.g., cigarette smoking, physical inactivity, unhealthy diet), physical and mental health status (e.g., obesity, diabetes, depression), and neighborhood and environmental characteristics.1,4–9
Psychological distress including depression and anxiety have also been associated with CVD, including heart disease and stroke.8–14 A meta-analysis of 28 studies showed that the overall risk of depression on CVD was 1.46.11 The relative risk varied by populations and methodology, ranging from 1.32 to 1.57.11 Despite the well-established morbidity studies, there are few studies on the association between psychological distress and heart disease mortality. Rasul and colleagues found an association between psychological distress and coronary heart disease mortality, using the 30-item General Health Questionnaire (GHQ-30), among adults aged 45-64 years in urban Scotland.10 Another study found that those with depression have a higher risk of cardiac mortality, compared with non-depressed adults, for both cardiac patients and adults without cardiac disease, aged 55-85 years in the Netherlands.15 Russ et al. found that, among adults aged 35 years and older in England, psychological distress measuring GHQ was associated with CVD mortality.16
Although psychological distress, which is a general term for symptoms of depression and anxiety, has been associated with CVD morbidity and mortality, including heart disease mortality,8,11,12,14,15,17–19 the relationship between different levels of psychological distress and heart disease mortality in the US has not been analyzed in detail using longitudinal data. For example, it is not known whether heart disease mortality increases relative to increases in psychological distress and whether this relationship varies by gender, race/ethnicity, and SES. To address this gap in research, we examine the association between psychological distress levels and heart disease mortality rates and relative risks in the US, using a nationally representative longitudinal dataset with an 18-years of mortality follow-up and five categories of the Kessler 6 (K6) nonspecific distress scale. Specifically, we addressed the following research questions:
-
How do total heart disease mortality rates and risks vary in relation to different levels of psychological distress?
-
To what extent do socioeconomic and demographic factors such as education, income/poverty level, housing tenure, race/ethnicity, nativity/immigrant status, and marital status account for the relationship between psychological distress and heart disease mortality?
-
Does controlling for sociodemographic factors as well as health status (activity limitation and self-assessed health) and health-risk factors such as smoking, obesity, and alcohol consumption account for the excess heart disease mortality associated with psychological distress?
-
Does the association between psychological distress and heart disease mortality vary among racial/ethnic groups such as non-Hispanic Whites, non-Hispanic Blacks, Hispanics, American Indians and Alaska Natives (AIANs), and Asian/Pacific Islanders (APIs)?
2. Methods
2.1. Data
The data for this study are derived from the National Health Interview Survey (NHIS) linked to the National Death Index (NDI).20 As a nationally representative, annual cross-sectional household interview survey, NHIS provides demographic, socio-economic, and health characteristics of the civilian, non-institutionalized population in the US. The National Center for Health Statistics (NCHS) developed public-use versions of NHIS linked with death certificate records from the NDI. For this study, we used the 1997-2014 public-use linked mortality file containing 18 years of mortality follow-up data from the date of survey participation through December 31, 2014.21
2.2. Sample
The study sample was restricted to adults aged 18 and older from the years of 1997 to 2014 NHIS sample adult files. The sample ineligible for mortality follow-up was eliminated from the analysis. The study sample was defined as adults without missing values in covariates using the STATA “svy, subpop” option. Thereby, all missing values in the study sample were excluded from the analyses but used for weights. The final pooled eligible sample size excluding missing values was 513,081. For missing values for poverty status (16.2%), body mass index (BMI) (3.5%) and alcohol consumption (1.7%), we created missing covariate categories to prevent omission of many observations from the analysis.
2.3. Measurement
We examined two mortality-related outcomes: age-adjusted mortality rates and relative risk of heart disease mortality as measured by hazard ratios. Follow-up time for individuals who died during the study period was estimated by the number of months from the month/year of interview to the month/year of death. Since the NHIS-NDI database provides only the quarter of death, we assumed that death occurred in the middle of quarter, February, May, August, or November.22
2.4. Psychological Distress
Psychological distress was measured by the Kessler 6 (K6) nonspecific distress scale23 of six symptoms. Respondents were asked: “during the past 30 days, how often you feel (1) so sad that nothing could cheer you up; (2) nervous; (3) restless or fidgety; (4) hopeless; (5) that everything was an effort; and 6) worthless.” The scores [5-point scale: all (4); most (3); some (2); a little (1); none of the time (0)] of each of the six symptoms of mental illness or nonspecific psychological distress were summed to create the K6 scale, ranging in value from 0 to 24. We created a 5-level categorical variable with scores of 0, 1-2, 3-5, 6-12, and 13-24 from the K6 scale; a score of 13 or higher was defined as serious psychological distress (SPD).24
2.5. Covariates
Based on the previous literature, we selected the following covariates for model estimation: age, gender, race/ethnicity, nativity/immigrant status, marital status, education, poverty status, housing tenure, region of residence, self-reported health status, activity limitation, BMI, smoking status, alcohol consumption, and survey years.16,22,24–27 Age was categorized into 14 five-year age groups. Race/ethnicity consisted of non-Hispanic Whites, non-Hispanic Blacks, Hispanics, AIANs, APIs, and non-Hispanic other races. Nativity/immigrant status was categorized as US-born, who were born in one of the 50 states or the District of Columbia, or foreign-born. Educational attainment was defined by four categories as less than high school diploma, high school diploma, some college, and college degree or more. Marital status was categorized as currently married, widowed, divorced/separated, and never married. Poverty status was defined by five categories based on the ratio of family income to poverty threshold (<100%; >=100% & <200%; >=200% & <400%; >=400%; missing). Housing tenure was dichotomized, with 1 being renters and zero equaling homeowners. Region of residence was defined by four categories, Northeast, Midwest, South, and West. Self-reported health status was dichotomized, with 1 being fair or poor health and zero being excellent, very good, or good health. Activity limitation was defined as one for a person with any Instrumental Activities of Daily Living (IADL), Activities of Daily Living (ADL), functional, or activity limitations in any of the pertinent rounds, and zero otherwise. BMI was defined by four categories, <25, 25-29, 30-39, ≥40, and missing. Smoking status was defined by three categories as never, former, and current smokers. Alcohol consumption was defined by four categories: lifetime abstainer, former drinker, current drinker, and unknown.
2.6. Analytic Approach
We computed age-adjusted mortality rates per 100,000 person-years of exposure for heart disease according to psychological distress level. In computing person-years for age-specific and age-adjusted heart disease mortality rates, deaths were assumed to occur uniformly throughout the follow-up period rather than being clustered in the first part of the period. Mortality rates were age adjusted by the direct method using the age distribution of the 2000 US Standard Population.2 Standard errors of age-adjusted mortality rates were computed, and mortality rate ratios (RR) associated with psychological distress level were tested for statistical significance.
Cox proportional hazards models were used to derive relative risks of heart disease mortality, controlling for individual characteristics and year-fixed effects. The model assumes that hazard rates are a log-linear function of parameters representing the effects of covariates.28,29 Individuals surviving beyond the follow-up period and those dying from causes other than heart disease were treated as right-censored observations. The Cox models were estimated separately for females and males and for different racial/ethnic groups.
We checked the hazards proportionality assumption29 by inspecting the plots of ln(-ln{S(t)]) [log(-log) survival function] against survival time t for the various covariate categories including those for psychological distress, gender, race/ethnicity, education, poverty level, activity limitation, and self-reported health status.30 These plots were found to be approximately parallel and hence the proportionality assumption was taken to be satisfied by the data.
Complex survey design procedures were used to account for clustering, multiple stages of selection, and disproportionate sampling. To correct the bias from the ineligible adults for linkage to the NDI due to insufficient identifying data, we used eligibility-adjusted weights developed by NCHS, instead of the standard sample weight.31 The sample weights were adjusted by dividing by the number of pooling years. All the analyses were conducted by STATA 15 and the Cox model was fitted using stcox procedure.32
3. Results
3.1. Descriptive Statistics
Table 1 provides descriptive statistics for individual characteristics by psychological distress levels. Approximately 3.1% of the sample had SPD (K6 score ≥13). The study sample consisted of non-Hispanic Whites (70.9%), non-Hispanic Blacks (11.4%), Hispanics (12.7%), and APIs (4.0%). The total number of heart disease deaths during the 18-year follow-up was 10,889.
| Sample size | %1 | |
|---|---|---|
| Sample size | 513,081 | 100 |
| K6 | ||
| 0 | 245,153 | 48.44 |
| 1-2 | 104,982 | 20.92 |
| 3-5 | 79,731 | 15.55 |
| 6-12 | 64,952 | 11.96 |
| ≥13 | 18,263 | 3.13 |
| Age | ||
| 18-34 | 149,316 | 31.30 |
| 35-49 | 145,043 | 29.19 |
| 50-64 | 116,558 | 23.03 |
| 65-79 | 75,062 | 12.42 |
| 80+ | 27,102 | 4.06 |
| Sex | ||
| Male | 225,329 | 48.07 |
| Female | 287,752 | 51.93 |
| Race/ethnicity | ||
| Non-Hispanic White | 326,054 | 70.93 |
| Non-Hispanic Black | 73,905 | 11.44 |
| Hispanic | 87,223 | 12.68 |
| American Indian/Alaska Native | 3,246 | 0.63 |
| Asian/Pacific Islander | 21,035 | 4.03 |
| Non-Hispanic other race | 1,618 | 0.29 |
| Outcome | ||
| Number of heart disease deaths | 10,889 | 100 |
| K6=0 | 4,940 | 45.65 |
| 1-2 | 2,096 | 19.75 |
| 3-5 | 1,659 | 15.21 |
| 6-12 | 1,646 | 14.65 |
| ≥13 | 548 | 4.75 |
3.2. Heart Disease Mortality Rates by Psychological Distress Levels
The age-adjusted heart disease mortality rate for adults with SPD was 366 deaths per 100,000 person-years, 75% higher than the rate of 209 deaths for those without psychological distress (Table 2). The age-adjusted mortality rate was 45% higher for those with K6 scores of 6-12 and 22% higher for those with K6 of 3-5, compared to that for adults with a K6 score of zero (no psychological distress). Adults with higher psychological distress levels (K6 scores) had consistently higher age-adjusted heart disease mortality rates. Females had 40% lower heart disease mortality than males (184 deaths vs. 305 deaths per 100,000 person-years). Males with SPD had a heart disease mortality rate of 536 deaths per 100,000 person-years, while females with SPD had a heart disease mortality rate of 286 (Table 2).
| Psychological distress level | Age-adjusted mortality rate (standard error) | Rate ratio |
|---|---|---|
| Sample size | 513,081 | |
| Overall (both sexes combined) | 234.67 (2.25) | |
| Male | 304.84 (4.10) | 1.00 (ref.) |
| Female | 184.15 (2.54) | 0.60*** |
| Psychological distress level (K6) | ||
| Both sexes combined | ||
| 0 | 208.95 (2.98) | 1.00 (ref.) |
| 1-2 | 223.09 (4.87) | 1.07 |
| 3-5 | 253.89 (6.22) | 1.22*** |
| 6-12 | 302.77 (7.46) | 1.45*** |
| ≥13 | 366.37 (16.11) | 1.75*** |
| Male | ||
| 0 | 267.97 (5.12) | 1.00 (ref.) |
| 1-2 | 309.07 (9.63) | 1.15*** |
| 3-5 | 347.81 (12.46) | 1.30*** |
| 6-12 | 391.54 (14.88) | 1.46*** |
| ≥13 | 536.48 (35.12) | 2.00*** |
| Female | ||
| 0 | 155.53 (3.39) | 1.00 (ref.) |
| 1-2 | 172.12 (5.31) | 1.11** |
| 3-5 | 199.59 (6.76) | 1.28*** |
| 6-12 | 254.25 (8.33) | 1.63*** |
| ≥13 | 285.90 (17.32) | 1.84*** |
Age-adjusted mortality rates are per 100,000 person-years using the 2000 US Standard Population. Rate ratios (RR) and standard errors were used to compare mortality rates for K6 categories. Rate ratios were statistically significantly different from 1.
3.3. Cox Proportional Hazards Models
In the Cox regression model 1, controlling for age and survey year, the heart disease mortality risk was 121% higher (hazard ratio [HR]=2.21; 95% CI=1.99,2.45) in adults with SPD (p<0.001), compared with adult without psychological distress (Table 3). In model 2, after controlling for age and survey year and socioeconomic and demographic characteristics, the heart disease mortality risk was 96% higher (HR=1.96; 95% CI=1.77,2.18) in adults with SPD (p<.001), compared with adult without psychological distress. In model 3, after controlling for all covariates including age, survey year, sex, race/ethnicity, nativity/immigrant status, education, marital status, poverty status, housing tenure, region, self-assessed health status, activity limitation, BMI, smoking status, and alcohol consumption, the overall heart disease mortality risk was 14% higher (HR=1.14; 95% CI=1.02,1.28) in adults with SPD (p<.05) than that in adults without SPD. In all three models, adults with K6 scores of 3-5 or 6-12 experienced a significantly higher heart disease mortality risk than those without any psychological distress. In general, the higher the psychological distress level, the higher the heart disease mortality risk. Trend in mortality risks by psychological distress level was statistically significant for all models.
| Covariate | Age-year-adjusted model1 | Sociodemographically-adjusted model2 | Fully-adjusted model3 |
|---|---|---|---|
| P-value for trend | P<0.001 | P<0.01 | P<0.1 |
| K6 | |||
| 0 | 1.00 | 1.00 | 1.00 |
| 1-2 | 1.10 (1.04,1.17)** | 1.18 (1.11,1.25)*** | 1.09 (1.02,1.16)** |
| 3-5 | 1.27 (1.19,1.36)*** | 1.31 (1.22,1.40)*** | 1.08 (1.01,1.16)* |
| 6-12 | 1.65 (1.54,1.77)*** | 1.59 (1.48,1.71)*** | 1.12 (1.05,1.21)** |
| ≥13 | 2.21 (1.99,2.45)*** | 1.96 (1.77,2.18)*** | 1.14 (1.02,1.28)* |
| Sex | |||
| Male | 1.00 | 1.00 | |
| Female | 0.43 (0.41,0.45)*** | 0.46 (0.43,0.48)*** | |
| Race/ethnicity | |||
| Non-Hispanic White | 1.00 | 1.00 | |
| Non-Hispanic Black | 1.11 (1.03,1.19)** | 1.02 (0.95,1.10) | |
| Hispanic | 0.95 (0.86,1.04) | 0.97 (0.88,1.07) | |
| American Indian/Alaska Native | 1.18 (0.83,1.68) | 0.99 (0.69,1.41) | |
| Asian/Pacific Islander | 0.88 (0.73,1.07) | 0.88 (0.73,1.06) | |
| Non-Hispanic other race | 0.81 (0.43,1.54) | 0.80 (0.42,1.51) | |
| Nativity/Immigrant status | |||
| US-born | 1.00 | 1.00 | |
| Foreign-born | 0.80 (0.73,0.88)*** | 0.89 (0.82,0.98)* | |
| Education | |||
| Less than high school | 1.66 (1.53,1.80)*** | 1.27 (1.17,1.38)*** | |
| High school | 1.40 (1.30,1.51)*** | 1.20 (1.11,1.30)*** | |
| Some college | 1.40 (1.29,1.51)*** | 1.24 (1.15,1.35)*** | |
| College | 1.00 | 1.00 | |
| Marital status | |||
| Currently married | 1.00 | 1.00 | |
| Widowed | 1.29 (1.21,1.38)*** | 1.25 (1.17,1.34)*** | |
| Divorced/separated | 1.22 (1.14,1.31)*** | 1.11 (1.04,1.19)** | |
| Never married | 1.56 (1.42,1.72)*** | 1.51 (1.37,1.66)*** | |
| Poverty status (%) | |||
| <100 | 1.63 (1.48,1.80)*** | 1.25 (1.13,1.38)*** | |
| >=100&<200 | 1.49 (1.37,1.63)*** | 1.23 (1.13,1.34)*** | |
| >=200&<400 | 1.33 (1.22,1.44)*** | 1.19 (1.10,1.29) *** | |
| >=400 | 1.00 | 1.00 | |
| Missing | 1.34 (1.23,1.45)*** | 1.18 (1.09,1.27)*** | |
| Housing tenure | |||
| Renter | 1.30 (1.23,1.37)*** | 1.19 (1.13,1.26)*** | |
| Owner | 1.00 | 1.00 | |
| Region of residence | |||
| Northeast | 0.99 (0.92,1.07) | 1.04 (0.96,1.12) | |
| Midwest | 1.01 (0.94,1.08) | 1.01 (0.93,1.08) | |
| South | 1.07 (1.00,1.15)* | 1.03 (0.96,1.10) | |
| West | 1.00 | 1.00 | |
| Self-assessed health status | |||
| Excellent/very good/good | 1.00 | ||
| Fair/poor | 1.53 (1.45,1.62)*** | ||
| Activity limitation | |||
| No | 1.00 | ||
| Yes | 1.69 (1.60,1.78)*** | ||
| BMI | |||
| <25 | 1.00 | ||
| =>25 & <30 | 0.96 (0.90,1.01) | ||
| =>30 & <40 | 1.14 (1.08,1.22)*** | ||
| =>40 | 1.47 (1.28,1.69)*** | ||
| Missing | 0.94 (0.79,1.11) | ||
| Smoking status | |||
| Never smoker | 1.00 | ||
| Former smoker | 1.22 (1.15,1.28)*** | ||
| Current smoker | 2.13 (1.99,2.28)*** | ||
| Alcohol consumption | |||
| Lifetime abstainer | 1.00 | ||
| Former drinker | 1.02 (0.95,1.09) | ||
| Current drinker | 0.78 (0.73,0.83)*** | ||
| Unknown | 1.07 (0.85,1.33) | ||
Table 4 provides heart disease mortality risks separately for males and females by psychological distress levels after adjusting for socioeconomic and demographic characteristics. For males, the heart disease mortality risk was 179% higher (HR=2.79; 95% CI=2.39,3.26) in the age-year-adjusted model, 113% higher (HR=2.13; 95% CI=1.82,2.49) in the sociodemographically-adjusted model, and 25% higher (HR=1.25; 95% CI=1.06,1.47) in the fully-adjusted model among adults with SPD, compared with adults without psychological distress. For females, the heart disease mortality risk was 121% higher (HR=2.21; 95% CI=1.90,2.56) in the age-year-adjusted model, and 81% higher (HR=1.81; 95% CI=1.56,2.10) in the sociodemographically-adjusted model among adults with SPD, and not significantly different in the fully-adjusted model, compared with adults without psychological distress.
| Sex or race/ethnicity | Heart disease deaths | Age-year-adjusted model | Sociodemographically-adjusted model | Fully-adjusted model |
|---|---|---|---|---|
| Male | n=225,329 | |||
| K6=0 | 2,802 | 1.00 (ref.) | 1.00 (ref.) | 1.00 (ref.) |
| 1-2 | 1,040 | 1.22 (1.13,1.32)*** | 1.23 (1.14,1.34)*** | 1.13 (1.05,1.23)** |
| 3-5 | 788 | 1.45 (1.32,1.60)*** | 1.38 (1.25,1.51)*** | 1.14 (1.03,1.25)** |
| 6-12 | 714 | 1.93 (1.74,2.14)*** | 1.63 (1.47,1.82)*** | 1.16 (1.04,1.29)** |
| ≥13 | 264 | 2.79 (2.39,3.26)*** | 2.13 (1.82,2.49)*** | 1.25 (1.06,1.47)** |
| P-value for trend | P<0.001 | P<0.01 | P<0.10 | |
| Female | n=287,752 | |||
| K6=0 | 2,138 | 1.00 (ref.) | 1.00 (ref.) | 1.00 (ref.) |
| 1-2 | 1,056 | 1.11 (1.02,1.21)* | 1.11 (1.02,1.21)* | 1.02 (0.94,1.12) |
| 3-5 | 871 | 1.28 (1.17,1.41)*** | 1.22 (1.11,1.34)*** | 1.02 (0.93,1.12) |
| 6-12 | 932 | 1.73 (1.57,1.91)*** | 1.52 (1.38,1.68)*** | 1.07 (0.97,1.19) |
| ≥13 | 284 | 2.21 (1.90,2.56)*** | 1.81 (1.56,2.10)*** | 1.04 (0.89,1.21) |
| P-value for trend | P<0.01 | P<0.01 | P=0.296 | |
| Non-Hispanic White | n=326,054 | |||
| K6=0 | 3,471 | 1.00 (ref.) | 1.00 (ref.) | 1.00 (ref.) |
| 1-2 | 1,635 | 1.13 (1.05,1.21)** | 1.20 (1.12,1.28)*** | 1.10 (1.03,1.18)** |
| 3-5 | 1,247 | 1.27 (1.18,1.37)*** | 1.31 (1.21,1.41)*** | 1.07 (1.00,1.16) |
| 6-12 | 1,116 | 1.69 (1.56,1.83)*** | 1.64 (1.51,1.78)*** | 1.14 (1.04,1.24)** |
| ≥13 | 374 | 2.42 (2.13,2.76)*** | 2.13 (1.88,2.42)*** | 1.19 (1.04,1.36)* |
| P-value for trend | P<0.001 | P<0.001 | P<0.05 | |
| Non-Hispanic Black | n=73,905 | |||
| K6=0 | 790 | 1.00 (ref.) | 1.00 (ref.) | 1.00 (ref.) |
| 1-2 | 268 | 1.16 (0.99,1.37) | 1.19 (1.01,1.4)* | 1.06 (0.90,1.25) |
| 3-5 | 210 | 1.19 (0.98,1.44) | 1.16 (0.95,1.41) | 0.97 (0.8,1.18) |
| 6-12 | 285 | 1.64 (1.41,1.92)*** | 1.51 (1.29,1.78)*** | 1.11 (0.94,1.31) |
| ≥13 | 79 | 1.76 (1.37,2.25)*** | 1.52 (1.18,1.94)** | 0.99 (0.76,1.29) |
| P-value for trend | P<0.05 | P<0.10 | P=0.956 | |
| Hispanic | n=87,223 | |||
| K6=0 | 547 | 1.00 (ref.) | 1.00 (ref.) | 1.00 (ref.) |
| 1-2 | 149 | 0.86 (0.69,1.07) | 0.94 (0.75,1.16) | 0.89 (0.72,1.10) |
| 3-5 | 164 | 1.32 (1.04,1.67)* | 1.44 (1.14,1.83)** | 1.25 (0.99,1.58) |
| 6-12 | 221 | 1.40 (1.16,1.70)** | 1.54 (1.27,1.88)*** | 1.16 (0.94,1.44) |
| ≥13 | 81 | 1.39 (1.02,1.90)* | 1.54 (1.12,2.10)** | 0.97 (0.71,1.34) |
| P-value for trend | P=0.144 | P=0.123 | P=0.985 | |
Table 4 also shows differential effects of psychological distress on heart disease morality for the three largest racial/ethnic groups. For non-Hispanic Whites and non-Hispanic Blacks, higher levels of psychological distress were generally associated with higher age-adjusted mortality risks. After controlling for age and survey year, non-Hispanic Whites with SPD had 142% higher heart disease mortality risks (HR=2.42; 95% CI=2.13,2.76), while non-Hispanic Blacks with SPD had 76% higher heart disease mortality risks (HR=1.76; 95% CI=1.37,2.25), compared with their counterparts with no psychological distress. Hispanics with SPD had 39% higher heart disease mortality risks (HR=1.39; 95% CI=1.02,1.90), but there was no consistent dose-response relationship. After controlling for socioeconomic and demographic characteristics, non-Hispanic Whites with SPD had 113% higher heart disease mortality risks (HR=2.13; 95% CI=1.88,2.42), while non-Hispanic Blacks with SPD had 52% higher (HR=1.52; 95% CI=1.18,1.94) and Hispanics with SPD had 54% higher heart disease mortality risks (HR=1.54; 95% CI=1.12,2.10), compared with their counterparts with no psychological distress. We did not find statistically significant differences in the fully-adjusted model for non-Hispanic Blacks and Hispanics.
Figure 1 provides estimated survivor functions for males and females and non-Hispanic Whites, non-Hispanic Blacks, and Hispanics according to psychological distress levels after adjusting for socioeconomic and demographic covariates in the Cox models. The estimated survival functions were steeper for males than for females. At the end of the 8-year follow-up, 98.54% of males with SPD were expected to survive from heart disease, compared with 99.31% of males with no psychological distress; the corresponding survival rates for males were 96.00% and 98.10% at the end of the 16-year follow-up. At the end of the 8-year follow-up, 99.57% of females with SPD were expected to survive from heart disease, compared with 99.76% of females with no psychological distress; the corresponding survival rates for females were 98.74% and 99.30% at the end of the 16-year follow-up.
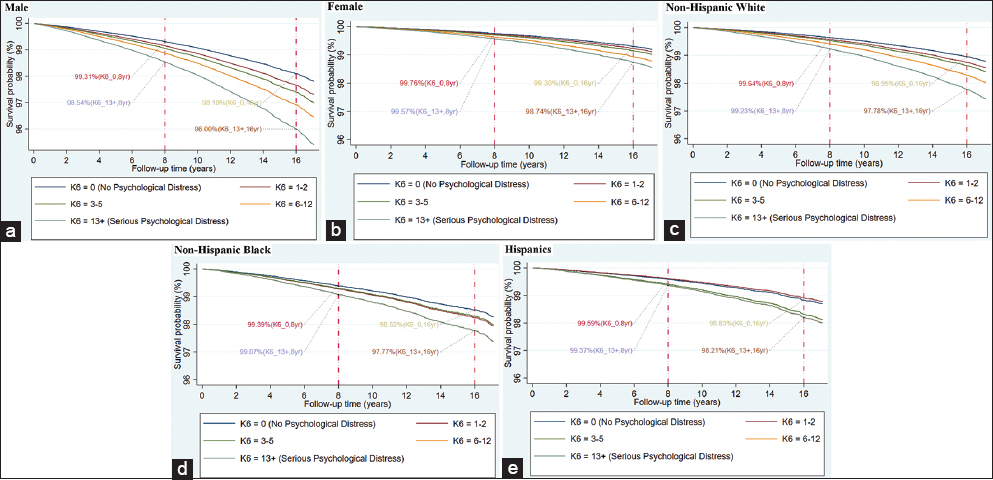
- (a-e). Adjusted Survivorship of US Adults Aged ≥18 Years by Psychological Distress Level (K6 Scores) and Sex or Race/ethnicity, 1997-2014 (derived from estimated Cox models of heart disease mortality adjusted for socioeconomic and demographic covariates)
The estimated survival functions were slightly steeper for non-Hispanic Whites than for non-Hispanic Blacks or Hispanics. At the end of the 8-year follow-up, 99.23% of non-Hispanic Whites with SPD were expected to survive from heart disease, compared with 99.64% of non-Hispanic Whites with no psychological distress; the corresponding survival rates for non-Hispanic whites were 97.78% and 98.95% at the end of the 16-year follow-up. At the end of the 8-year follow-up, 99.07% of non-Hispanic Blacks with SPD were expected to survive from heart disease, compared with 99.39% of non-Hispanic Blacks with no psychological distress; the corresponding survival rates for non-Hispanic Blacks were 97.77% and 98.52% at the end of the 16-year follow-up. At the end of the 8-year follow-up, 99.37% of Hispanics with SPD were expected to survive from heart disease, compared with 99.59% of Hispanics with no psychological distress; the corresponding survival rates for Hispanics were 98.21% and 98.83% at the end of the 16-year follow-up.
We conducted a sensitivity analysis to check for reverse causality between psychological distress and heart disease mortality by excluding individuals with a history of heart disease at the time of the survey. In samples with and without a history of heart disease diagnosis at baseline, the association between psychological distress and heart disease mortality was similar (71% and 54% higher relative mortality risks respectively for those with SPD in the sociodemographically-adjusted models, which reduced to statistical non-significance after additional adjustment for health status and health-risk factors) (Table 5). We also performed a sensitivity analysis to examine temporal robustness of psychological distress by re-estimating models using 2-year, 5-year, and 10-year follow-up times. As shown in Table 6, the longer follow-up dilutes the mortality impact of baseline psychological distress, as psychological distress is expected to differ from its baseline level over the longer follow-up.
| Psychological distress level | Age-year-adjusted model | Sociodemographically-adjusted model | Fully-adjusted model |
|---|---|---|---|
| Adults without the heart disease1 diagnosis at baseline | |||
| K6=0 | 1.00 (ref.) | 1.00 (ref.) | 1.00 (ref.) |
| 1-2 | 1.12 (1.03,1.22)* | 1.18 (1.08,1.29)*** | 1.12 (1.02,1.23)* |
| 3-5 | 1.20 (1.08,1.33)** | 1.23 (1.11,1.37)*** | 1.07 (0.96,1.19) |
| 6-12 | 1.46 (1.32,1.62)*** | 1.46 (1.31,1.62)*** | 1.11 (1.00,1.24) |
| ≥13 | 1.64 (1.41,1.90)*** | 1.54 (1.32,1.80)*** | 1.03 (0.88,1.21) |
| Adults with history of heart disease diagnosis at baseline | |||
| K6=0 | 1.00 (ref.) | 1.00 (ref.) | 1.00 (ref.) |
| 1-2 | 1.01 (0.93,1.09) | 1.08 (1.00,1.17) | 1.02 (0.94,1.11) |
| 3-5 | 1.16 (1.06,1.28)** | 1.19 (1.08,1.31)*** | 1.05 (0.95,1.15) |
| 6-12 | 1.41 (1.28,1.56)*** | 1.33 (1.20,1.47)*** | 1.04 (0.93,1.16) |
| ≥13 | 2.00 (1.70,2.35)*** | 1.71 (1.46,2.02)*** | 1.14 (0.96,1.35) |
| Psychological distress level | Age-year-adjusted model | Sociodemographically-adjusted model | Fully-adjusted model |
|---|---|---|---|
| 2-year mortality follow-up | |||
| K6=0 | 1.00 (ref.) | 1.00 (ref.) | 1.00 (ref.) |
| 1-2 | 1.15 (1.00,1.34)† | 1.23 (1.06,1.42)** | 1.10 (0.95,1.28) |
| 3-5 | 1.51 (1.30,1.75)*** | 1.55 (1.33,1.8)*** | 1.18 (1.02,1.37)* |
| 6-12 | 2.16 (1.86,2.52)*** | 2.10 (1.80,2.45)*** | 1.31 (1.12,1.54)** |
| ≥13 | 2.99 (2.35,3.80)*** | 2.70 (2.12,3.44)*** | 1.37 (1.07,1.76)* |
| 5-year mortality follow-up | |||
| K6=0 | 1.00 (ref.) | 1.00 (ref.) | 1.00 (ref.) |
| 1-2 | 1.11 (1.01,1.22)* | 1.19 (1.08,1.31)*** | 1.09 (0.99,1.20) |
| 3-5 | 1.40 (1.27,1.54)*** | 1.43 (1.30,1.58)*** | 1.15 (1.04,1.26)** |
| 6-12 | 1.89 (1.72,2.08)*** | 1.84 (1.66,2.03)*** | 1.23 (1.11,1.36)*** |
| ≥13 | 2.56 (2.19,3.00)*** | 2.29 (1.96,2.69)*** | 1.26 (1.07,1.48)** |
| 10-year mortality follow-up | |||
| K6=0 | 1.00 (ref.) | 1.00 (ref.) | 1.00 (ref.) |
| 1-2 | 1.13 (1.05,1.20)** | 1.20 (1.12,1.28)*** | 1.10 (1.03,1.18)** |
| 3-5 | 1.31 (1.21,1.41)*** | 1.33 (1.23,1.44)*** | 1.09 (1.01,1.18)* |
| 6-12 | 1.68 (1.56,1.82)*** | 1.62 (1.50,1.76)*** | 1.12 (1.04,1.22)** |
| ≥13 | 2.28 (2.02,2.58)*** | 2.03 (1.79,2.29)*** | 1.15 (1.01,1.31)* |
4. Discussion
In this large prospective study of 513,081 US adults using a relatively long mortality follow-up of 18 years, we found marked and consistent gradients in age-adjusted heart disease mortality rates according to levels of psychological distress. Even after controlling for several demographic and socioeconomic characteristics, significantly higher risks of heart disease mortality existed for the total population, for males and females, and for non-Hispanic Whites, non-Hispanic Blacks, and Hispanics who experienced moderate to serious levels of psychological distress. Estimation of age-adjusted heart disease mortality rates and derivation of relative risks of heart disease mortality by psychological distress levels after adjusting for sociodemographic, behavioral, and health characteristics is a novel and unique feature of our study, as such analyses had not been undertaken previously in the US, to the best of our knowledge.
The findings of our study are largely consistent with those from two previous studies of psychological distress and heart disease mortality.15,16,33 In our study, the age-adjusted relative risk of heart disease mortality associated with serious levels of psychological distress were 2.21, compared with 2.05 and 4.90 respectively with age- and sex-adjusted estimates in the previous European studies.15,16 In our full model with sociodemographic, health status, and behavioral factors of smoking, alcohol consumption, and obesity, the adjusted risk of heart disease mortality associated with SPD was 1.14, compared with 1.72 and 3.90 respectively in the previous studies with slightly different covariates of health status such as blood pressure and diabetes.15,16 Consistent with a previous study of a Scottish cohort, we found that males had a higher relative risk of heart disease mortality associated with psychological distress, compared with females.33 In our study, the age-adjusted relative risk of heart disease mortality associated with SPD were 2.79 for males and 2.21 for females, compared with 1.93 for males and 1.37 for females in the previous study with 5 years of follow-up.33 Although our study differs from the other studies in its measurement of psychological distress and consideration of covariates, we found a robust dose-response relationship between psychological distress and heart disease mortality.15,16
Our study has provided the evidence of a strong link between psychological distress and heart disease mortality, but does not shed any light on biological or physiological mechanisms through which psychological distress might affect the development of the disease or mortality. Psychological distress may increase the risk of heart disease through various potential mechanisms. Psychological distress can promote inflammatory process or stressors, and activate automatic nerve system or hypothalamic-pituitary-adrenal (HPA) influences, which have been associated with poor cardiovascular outcomes.5,8,9,13 As a mediator, psychological distress is highly correlated with traditional CVD risk factors such as smoking, adherence to medical treatment, and obesity.5,8,9 As mentioned earlier, the well-established major CVD risk factors include individual demographic and socioeconomic characteristics, health behaviors, physical and mental health status, and neighborhood environments.1,4–9 In our analysis, we controlled for several of these factors, which are associated with both psychological distress and heart disease mortality in an expected manner.1,4–9 In our study cohort, adults with SPD had a 2.4 times higher smoking rate (42.2% vs. 17.3%; data not shown) and a 1.6 times higher obesity rate (35.5% vs. 22.7%; data not shown) than those without psychological distress. Additionally, in our study cohort, individuals experiencing SPD were 1.7 times more likely to be uninsured (25.0% vs. 15.1%), 2.6% less likely to have a usual source of care (83.3% vs. 85.5%), and 5.7 times more likely to delay seeking care due to cost (31.6% vs. 5.6%), compared to those without psychological distress. Further research is needed to address pathways through which psychological distress increases heart disease mortality.
4.1. Limitations
This study has limitations. First, our study only contains the NHIS sample eligible for linkage to the NDI. Excluding samples ineligible for linkage may lead to biased mortality estimates. To address this bias, we used the adjusted original sampling weight to account for the NHIS-NDI mismatches.31 Second, our findings may be affected by the omitted-variable bias. While our Cox regression models were controlled for self-reported health status, BMI, activity limitation, and physical health status, there could be other potential confounders. Antipsychotic medication use,25 undiagnosed or diagnosed mental illness16 could affect the association between psychological distress and mortality. Third, symptoms in K6, such as “sad, nervous, restless, hopeless, effort, and worthless”, might not capture all diagnostic criteria of psychological distress. Although the 6 items capture several diagnostic criteria in Diagnostic and Statistical Manual of Mental Disorders (DSM-5) or ICD-10, the scale does not provide a clinical diagnosis of depression or anxiety.16 However, K6 is a valid measure of psychological distress in terms of good precision in the scale distribution and consistent levels of severity across socio-demographic subsamples.34 Fourth, since the NHIS excludes the institutionalized population, who may have higher levels of psychological distress and mortality, heart disease mortality risks associated with psychological distress in this study might be underestimated. Fifth, all the covariates in the NHIS-NDI database were time-fixed at the baseline as of the survey date. Several of the covariates such as SES, health status, behavioral risk factors, and psychological distress could have varied over the long mortality follow-up period of 18 years, which would have influenced their estimated impact on heart disease mortality. Future studies need to evaluate the temporal robustness of psychological distress patterns in heart disease mortality using longitudinal datasets with time-varying covariates.
5. Conclusions and Global Health Implications
With 18 years of mortality follow-up in a large, nationally representative study of over a half million US adults aged 18 years and older, we found that individuals with serious psychological distress had more than twice the age-adjusted risk of mortality from heart disease than those with no psychological distress. The association between psychological distress and heart disease mortality remained marked and statistically significant even after controlling for several sociodemographic, behavioral, and health characteristics. Consistent with previous studies on all-cause and cancer mortality, we found a dose-response relationship between psychological distress levels and mortality from heart disease.25,35–37 Psychological distress is a major health condition in the United States, with 45 million (or 18.5%) of adults at risk for moderate to serious levels of distress.38 Our study findings indicate psychological distress to be an important predictor of heart disease mortality; they underscore the significance of addressing psychological well-being and prevention and treatment of psychological distress in the general and heart disease-patient populations as a potential strategy for reducing heart disease mortality.
Conflict of Interest: None.
Financial Disclosure: None to report.
Funding Source: Dr. Lee was supported in part by an appointment to the Research Participation Program at the Health Resources and Services Administration - Office of Planning, Analysis and Evaluation (HRSA-OPAE), administered by the Oak Ridge Institute for Science and Education (ORISE) through an interagency agreement between the US Department of Energy and HRSA.
Ethical Approval: The study was exempt from Institutional Review Board approval as it utilized a de-identified public use dataset.
Disclaimer: The views expressed are the authors’ and not necessarily those of the US Department of Health and Human Services or the Health Resources and Services Administration.
References
- Heart disease and stroke statistics—2018 update: a report from the American Heart Association. Circulation. 2018;137:e67-e492.
- [Google Scholar]
- Social determinants of health in the United States: addressing major health inequality trends for the nation, 1935-2016. Int J MCH AIDS. 2017;6(2):139-164.
- [Google Scholar]
- Widening socioeconomic and racial disparities in cardiovascular disease mortality in the United States, 1969-2013. Int J MCH AIDS. 2015;3(2):106.
- [Google Scholar]
- Depression as a risk factor for cardiac mortality and morbidity: a review of potential mechanisms. J Psychosom Res. 2002;53(4):897-902.
- [Google Scholar]
- Increasing area deprivation and socioeconomic inequalities in heart disease, stroke, and cardiovascular disease mortality among working age populations, United States, 1969-2011. Int J MCH AIDS. 2015;3(2):119.
- [Google Scholar]
- Widening geographical disparities in cardiovascular disease mortality in the United States, 1969-2011. Int J MCH AIDS. 2015;3(2):134.
- [Google Scholar]
- Anger, anxiety, and depression as risk factors for cardiovascular disease: the problems and implications of overlapping affective dispositions. Psychol Bull. 2005;131(2):260.
- [Google Scholar]
- Psychological distress, physical illness, and risk of coronary heart disease. J Epidemiol Community Heal. 2005;59(2):140-145.
- [Google Scholar]
- Depression and the risk for cardiovascular diseases: systematic review and meta analysis. Int J Geriatr Psychiatry. 2007;22(7):613-626.
- [Google Scholar]
- The relationship of depression to cardiovascular disease: epidemiology, biology, and treatment. Arch Gen Psychiatry. 1998;55(7):580-592.
- [Google Scholar]
- Why is depression bad for the failing heart? A review of the mechanistic relationship between depression and heart failure. J Card Fail. 2004;10(3):258-271.
- [Google Scholar]
- State of the art review:depression, stress, anxiety, and cardiovascular disease. Am J Hypertens. 2015;28(11):1295-1302.
- [Google Scholar]
- Depression and cardiac mortality: results from a community-based longitudinal study. Arch Gen Psychiatry. 2001;58(3):221-227.
- [Google Scholar]
- Association between psychological distress and mortality:individual participant pooled analysis of 10 prospective cohort studies. BMJ. 2012;345:e4933.
- [Google Scholar]
- Association between depression and mortality in older adults: the Cardiovascular Health Study. Arch Intern Med. 2000;160(12):1761-1768.
- [Google Scholar]
- Depression and risk of stroke morbidity and mortality: a meta-analysis and systematic review. JAMA. 2011;306(11):1241-1249.
- [Google Scholar]
- Depressive symptoms and increased risk of stroke mortality over a 29-year period. Arch Intern Med. 1998;158(10):1133-1138.
- [Google Scholar]
- IPUMS Health Surveys: National Health Interview Survey, Version 6.4 [dataset];. 2019 doi:https://doi.org/10.18128/D070.V6.4
- [Google Scholar]
- Public-Use Linked Mortality File 2015
- It is better to be a fat ex-smoker than a thin smoker: findings from the 1997–2004 National Health Interview Survey? National Death Index linkage study. Tob Control. 2014;23(5):395-402.
- [Google Scholar]
- Serious psychological distress among adults:United States, 2009–2013. NCHS Data Brief. 2015;203:1-8.
- [Google Scholar]
- Serious psychological distress, as measured by the K6, and mortality. Ann Epidemiol. 2009;19(3):202-209.
- [Google Scholar]
- Psychological distress and mortality among adults in the US household population. CBHSQ data Rev 2014
- [Google Scholar]
- Cancer disparities by race/ethnicity and socioeconomic status. CA Cancer J Clin. 2004;54(2):78-93.
- [Google Scholar]
- Socioeconomic and racial/ethnic disparities in cancer mortality, incidence, and survival in the United States, 1950–2014: over six decades of changing patterns and widening inequalities. J Environ Public Health. 2017 2017
- [Google Scholar]
- Applied Longitudinal Data Analysis: Modeling Change and Event Occurrence. Oxford university press; 2003.
- [Google Scholar]
- A comparative analysis of infant mortality in major Ohio cities: Significance of socio-biological factors. Appl Behav Sci Rev. 1994;2(1):77-94.
- [Google Scholar]
- The Linkage of National Center for Health Statistics Survey Data to the National Death Index —2015 Linked Mortality File (LMF) Methodology Overview and Analytic Considerations
- [Google Scholar]
- Stata Statistical Software: Release 15 2017
- Psychological distress, physical illness and mortality risk. J Psychosom Res. 2004;57(3):231-236.
- [Google Scholar]
- Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychol Med. 2002;32(6):959-976.
- [Google Scholar]
- Excess mortality due to depression and anxiety in the United States: results from a nationally representative survey. Gen Hosp Psychiatry. 2016;39:39-45.
- [Google Scholar]
- Psychological distress as a risk factor for dementia death. Arch Intern Med 2011 doi:10.1001/archinternmed.2011.521
- [Google Scholar]
- Psychological distress in relation to site specific cancer mortality:pooling of unpublished data from 16 prospective cohort studies. BMJ. 2017;356:j108.
- [Google Scholar]
- National Health Interview Survey 2018 https://www.cdc.gov/nchs/nhis/2019





