Translate this page into:
Interbirth Intervals of Immigrant and Refugee Women in the United States: A Cross-Sectional Study
* Corresponding author email: olorunsaiyec@arcadia.edu
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 4.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Background and Objective:
Despite guidelines recommending an interval of at least 18–24 months between a live birth and the conception of the next pregnancy, nearly one-third of pregnancies in the United States are conceived within 18 months of a previous live birth. The purpose of this study was to examine the associations between multiple immigration-related variables and interbirth intervals among reproductive-aged immigrant and refugee women living in the United States.
Methods:
This was a cross-sectional, quantitative study on the sexual and reproductive health (SRH) of reproductive-aged immigrant and refugee women in the United States. The data were collected via an online survey administered by Lucid LLC. We included data on women who had complete information on nativity and birth history in the descriptive analysis (n = 653). The exposure variables were immigration pathway, length of time since immigration, and country/region of birth. The outcome variable was interbirth interval (≤18, 19–35, or ≥36 months). We used multivariable ordinal logistic regression, adjusted for confounders, to determine the factors associated with having a longer interbirth interval among women with second- or higher-order births (n = 245).
Results:
Approximately 37.4% of study participants had a short interbirth interval. Women who immigrated to the United States for educational (aOR = 4.57; 95% CI, 1.57–9.58) or employment opportunities (aOR = 2.27; 95% CI, 1.07–5.31) had higher odds of reporting a longer interbirth interval (19–35 or ≥36 months) than women born in the United States. Women born in an African country had 0.79 times the odds (aOR = 0.79; 95% CI, 0.02–0.98) of being in a higher category of interbirth interval.
Conclusion and Global Health Implications:
Although all birthing women should be counseled on optimal birth spacing through the use of postpartum contraception, immigrant and refugee women would benefit from further research and policy and program interventions to help them in achieving optimal birth spacing. SRH research in African immigrant and refugee communities is especially important for identifying ameliorable factors for improving birth spacing.
Keywords
African Immigrants
Birth Spacing
Immigrant Women
Interbirth Interval
Interpregnancy Interval
Maternal Health
Refugee Women
1. Introduction
Current guidelines recommend an interval of at least 18–24 months between a live birth and the conception of the next pregnancy.1,2 However, nearly one-third of pregnancies in the United States are conceived within 18 months of a previous birth.3 Short interbirth interval is associated with adverse birth and infant outcomes and increased risks of maternal morbidity during pregnancy and at delivery.4-8 Moreover, most of the adverse outcomes of short interval births are concentrated in marginalized populations, including immigrants.9,10
Factors associated with short interbirth interval include younger maternal age, marital status, and delayed initiation of childbearing.6,7 Short duration of, or non-exclusive breastfeeding, and prior experience of infant death or pregnancy loss are also associated with short interpregnancy intervals.11-13 Importantly, unintended pregnancies have significantly shorter birth intervals than planned pregnancies.6,14 Other factors associated with short interbirth intervals include race and ethnicity and lower socioeconomic status.7,11,15 Hispanic and Black individuals have comparatively higher risks of short interval births.6,11
Although health is a public good and health care should be universally available and accessible to individuals and communities, some groups of the population face significant barriers to accessing health care services.16-18 For example, marginalized populations, such as immigrant and refugee communities, face barriers to health care, particularly sexual and reproductive health (SRH) care, due to language barriers, cultural norms, unfamiliarity with the US health care system, lower socioeconomic status, and a lack of culturally appropriate services.19-22 In addition, due to the intersecting influences of immigration policies, language, and socioeconomic barriers, immigrant and refugee populations have even less access to health care services, including SRH and contraception.19-21,23
Federal immigration laws in the United States prevent undocumented immigrants and documented immigrants who have been in the country for less than 5 years from enrolling in publicly funded health insurance programs offered through Medicaid.24,25 Access to essential health education and services, such as SRH care, family planning services, and contraception for spacing or limiting births, is extremely limited for low-income immigrant and refugee women unless state exemptions are available.26 Moreover, a lack of culturally competent health care providers and racism directed at immigrants constitute additional barriers to SRH care and optimal birth spacing in this population.26 Consequently, individuals from immigrant and refugee populations are more likely to report using less effective contraception methods, which may increase their risk for short interval births.27 Studies on interbirth intervals involving immigrant and refugee women have mostly relied on birth certificate data, which lack a number of key sociodemographic variables, thereby limiting the ability to adequately adjust the analyses for potential confounding factors.10,28,29
The purpose of this study, therefore, was to examine the associations between multiple immigration-related variables and interbirth interval among immigrant and refugee women living in the United States. The findings can contribute to filling some knowledge gaps about the factors associated with short interbirth intervals in immigrant and refugee women and identify groups at higher risk for short interbirth interval.
2. Methods
This was a cross-sectional, quantitative study on the sexual and reproductive health of immigrant women in the United States (n = 657). The data were collected via an online survey administered by Lucid LLC, which supports the recruitment of samples for academic research through its academic marketplace, Theorem.30 Lucid is able to reach and recruit diverse audiences through partnerships with multiple vendors. Eligibility for the online survey was based on self-identification as a woman, aged 18–44 years, English proficiency, and residency in the United States. We included data on 653 women who had complete information on nativity and birth history in the descriptive analysis (n = 653). For the regression analysis, we excluded women with fewer than two births (n = 408); hence, the final analytic sample was 245 women with two or more births.
2.1. Study Variables
Exposure: The exposure variables were immigration-related factors, such as (1) length of time since immigration to the United States (US-born [unexposed]: ≤5, 6–10, or >10 years); (2) immigration pathway (US-born [unexposed]: conflict/persecution, employment, education, or family reunification); and (3) place of birth (grouped into the following regions: US-born [unexposed], North America [non-US], Africa, Asia, other Western countries (i.e., Europe and Australia), South and Central America, or the Caribbean).
Outcome: We calculated the outcome variable, interbirth interval, using data from the most recent and previous births. The question on birth interval was adapted from the Pregnancy Risk Assessment Monitoring System (PRAMS) questionnaire31 and was only applicable to participants who had more than one live birth. The adapted questions was “when your youngest child was born, how old was the child born just before your youngest child?” Participants could select one of the following responses: 0–12 months, 13–18 months, 19–24 months, more than 2 years but less than 3 years, 3–5 years, or more than 5 years. Based on guidelines that recommend a minimum interval of 18 months between a live birth and a subsequent pregnancy,1 we coded the outcome as an ordinal variable consisting of the following categories: ≤18 months (short interbirth interval), 19–35 months, and ≥36 months.
Covariates: Covariates were theoretically selected from existing studies.6,7,11,15,29 Questions providing data on covariates were mostly adopted from the PRAMS and National Survey of Family Growth (NSFG).31,32 Covariates included age, marital status (single or married), parity (none, 1, 2, or ≥3), ethnicity (Hispanic or non-Hispanic), and racial group (Black, Asian, White, or others [i.e., Middle Eastern, North African, or more than one race]). Prior research has shown that socially and structurally marginalized populations, such as people of color and immigrant groups, have a higher likelihood of having short interval births than White people.9,10,19 Therefore, we conceptualized race and ethnicity as separate variables to disentangle the structural (i.e., race) and social (i.e., ethnicity) relationships with the outcome and to avoid masking possible overlaps and heterogeneity in the study sample.33-36
Other covariates included insurance (none, public, or private), income (≤$20,000, $20,001–$40,000, $40,001–$75,000, or >$75,000), education (high school or less, some college or associate degree, bachelor’s degree, or graduate or professional degree), and language spoken predominantly at home (English, French, Spanish, and others [i.e., Arabic, Armenian, Chinese, Creole, Farsi, Hindi, Kirundi, Vietnamese, and Yoruba, based on participants’ self-report]).
2.2. Statistical Analysis
We computed frequency distributions of participants’ sociodemographic characteristics. Because the outcome variable was ordered, we used multivariable ordinal logistic regression to compare the odds of having a longer interbirth interval (i.e., 19–35 or ≥36–months) versus ≤18 months (short), while adjusting for potential confounders. Results are expressed as odds ratios and 95% confidence intervals. The level of statistical significance was set at p < 0.05. We analyzed the data using Stata version 15 (College Station, Texas).
2.3. Ethical Approval
The institutional review board of Arcadia University approved the survey (21-06-01). All participants provided written informed consent prior to completing the survey.
3. Results
3.1. Social and Demographic Characteristics of the Study Participants
The descriptive analysis included 653 women. The mean age of women in the sample was 29.2 (±7.4) years (Table 1). Approximately 410 (62.9%) of the participants are classified as Black. Additionally, 506 women (77.5%) identified as non-Hispanic. Approximately 50.1% of the participants had public insurance, 135 (20.6%) had two children, and 110 (16.9%) had three or more children. Approximately 22.4% of the women had a bachelor’s degree, and 28.0% reported an annual household income of $20,001–$40,000. Approximately 86.83% of the women spoke English, 9.5% spoke Spanish, and 2.0% spoke French, predominantly at home; “other” languages spoken predominantly at home by 1.7% of the women included Arabic, Armenian, Creole, Chinese, Farsi, Hindi, Kirundi, Vietnamese, and Yoruba. Furthermore, 398 (61%) were born in the United States, 68 (10.4%) in South and Central America, and 66 (10.1%) in Africa (Table 1). Approximately 18.3% of all women in the sample migrated to the United States for employment-based reasons, and 19.9% had been in the United States for more than 10 years.
| Variable | N (%) |
|---|---|
| Reason for immigration | |
| US-born (non-immigrant) | 398 (61.0) |
| Conflict/insecurity | 50 (7.7) |
| Education | 43 (6.6) |
| Employment | 119 (18.3) |
| Family-based | 43 (6.4) |
| Length of time since immigration | |
| US-born (non-immigrant) | 398 (61.0) |
| ≤5 years | 72 (10.9) |
| 6–10 years | 54 (8.3) |
| >10 years | 130 (19.91) |
| Birthplace | |
| US-born (non-immigrant) | 398 (61.0) |
| North America (non-US) | 9 (1.4) |
| Africa | 66 (10.11) |
| Asia | 27 (4.13) |
| Europe | 43 (6.6) |
| South and Central America | 68 (10.41) |
| Caribbean | 42 (6.43) |
| Race | |
| Black/African American | 410 (62.9) |
| Asian/Asian American | 61 (9.4) |
| White | 137 (21.01) |
| Other racial groupsa | 45 (6.8) |
| Ethnicity | |
| Hispanic | 144 (22.1) |
| Non-Hispanic | 506 (77.5) |
| Missing | 3 (0.5) |
| Maternal age (years) | |
| Mean (standard deviation) | 29.2 (7.4) |
| Parity | |
| None | 269 (41.2) |
| One | 139 (21.2) |
| Two | 135 (20.7) |
| Three or more | 110 (16.9) |
| Marital status | |
| Single | 342 (52.4) |
| Married/Cohabiting | 311 (47.63) |
| Insurance type | |
| None | 67 (10.3) |
| Public | 327 (50.08) |
| Private | 256 (39.20) |
| Household income | |
| ≤$20,000 | 168 (25.73) |
| $20,001–$40,000 | 183 (28.02) |
| $40,001–$75,000 | 158 (24.6) |
| >$75,000 | 72 (28.2) |
| Highest educational level | |
| High school or less | 187 (28.7) |
| Some college or associate | 232 (35.6) |
| Bachelor’s | 146 (22.4) |
| Graduate or professional | 87 (13.34) |
| Language spoken predominantly at home | |
| English | 567 (86.83) |
| French | 13 (2.0) |
| Spanish | 62 (9.5) |
| Other languagesb | 11 (1.7) |
3.2. Frequency Distribution of Interbirth Intervals of Women in the Study
Approximately 37.4% of the study participants had an interbirth interval of ≤18 months, 23.7% had interbirth intervals of 19–35 months, and 39.0% reported interbirth intervals of ≥36 months (Figure 1).
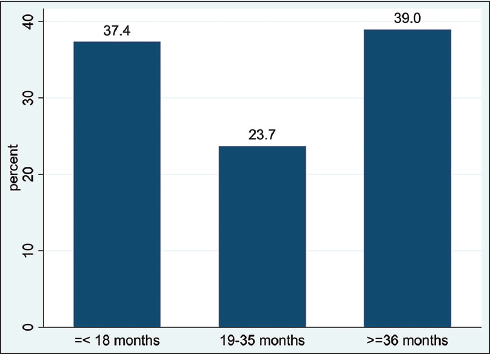
- Frequency distribution of interbirth interval among women in the study (n = 245)
3.3. Unadjusted Analysis of Factors Associated With Interbirth Intervals
In the unadjusted multivariable ordered logistic regression, women who immigrated to the United States for educational (OR = 2.56; 95% CI, 1.02–6.41) and employment opportunities (OR = 1.95; 95% CI, 1.14–3.33) were more likely to report longer interbirth intervals (i.e., 19–35 or ≥36 months) than US-born women (unexposed, Table 2). Women who had lived in the United States for <5 years were less likely to have longer interbirth interval (OR = 0.33; 95% CI, 0.26–1.00), whereas women who had lived in the United States for >10 years had nearly twice the odds of reporting longer interbirth intervals (OR = 1.92; 95% CI, 1.17–2.94) than US-born women. African-born women had 84% lower odds of being in longer interbirth interval categories (OR = 0.16; 95% CI, 0.04–0.49) than US-born women, whereas women born in other Western countries had higher odds of being in the longer interbirth interval categories (OR = 2.78; 95% CI, 1.06–7.28).
| Variable | Unadjusted OR (95% CI) |
|---|---|
| Immigration pathway | |
| US-born | 1.00 (Referent) |
| Conflict/insecurity | 0.87 (0.40–1.90) |
| Education | 2.56 (1.02–6.41) |
| Employment | 1.95 (1.14–3.33) |
| Family-based | 1.26 (0.54–2.94) |
| Length of time since immigration | |
| US-born | 1.00 (Referent) |
| ≤5 years | 0.33 (0.26–1.00) |
| 6–10 years | 1.13 (0.53–2.42) |
| >10 years | 1.92 (1.17–3.17) |
| Birthplace | |
| US-born | 1.00 (Referent) |
| Africa | 0.16 (0.04–0.49) |
| Asia | 1.28 (0.51–3.21) |
| Other Western countries | 2.78 (1.06–7.28) |
| South and Central America | 1.56 (0.78–3.10) |
| Caribbean | 1.05 (0.05–2.17) |
| Race | |
| Black/African American | 1.00 (Referent) |
| Asian/Asian American | 1.17 (1.02–15.48) |
| White | 1.35 (1.09–6.22) |
| Other racial groups | 1.58 (0.62–3.98) |
| Ethnicity | |
| Hispanic | 1.00 (Referent) |
| Non-Hispanic | 0.51 (0.25–1.03) |
| Maternal age (years) | 1.08 (1.04–1.13) |
| Parity | |
| Two | 1.00 (Referent) |
| Three or more | 2.67 (1.57–4.52) |
| Marital status | |
| Single | 1.00 (Referent) |
| Married/cohabiting | 1.24 (0.80–1.91) |
| Insurance type | |
| None | 1.00 (Referent) |
| Public | 0.35 (0.14–0.87) |
| Private | 0.40 (0.16–0.99) |
| Household income | |
| ≤$20,000 | 1.00 (Referent) |
| $20,001–$40,000 | 1.21 (0.67–2.19) |
| $40,001–$75,000 | 1.51 (0.92–1.09) |
| >$75,000 | 1.25 (0.68–2.30) |
| Highest educational level | |
| High School or less | 1.00 (Referent) |
| Some college or associate | 2.09 (1.22–3.59) |
| Bachelor’s | 2.01 (1.09–3.69) |
| Graduate or professional | 1.01 (0.53–1.94) |
| Language spoken predominantly at home | |
| English | 1.00 (Referent) |
| French | 0.25 (0.05–1.28) |
| Spanish | 2.22 (1.05–4.72) |
| Other languages | 1.71 (0.27–10.94) |
3.4. Adjusted Analysis of Factors Associated With Interbirth Intervals
Women who migrated to the United States for educational reasons (aOR = 4.57; 95% CI, 1.57–9.58) and employment reasons (aOR = 2.27; 95% CI, 1.07–5.31) had statistically significant higher odds of being in longer interbirth interval categories than US-born women (unexposed) in the multivariable ordinal logistic regression model adjusted for potential confounders (Table 3). For African-born women, the odds of reporting longer interbirth intervals were markedly reduced but remained statistically significant (aOR = 0.79; 95% CI, 0.02–0.98); the association for other Western-born women was reduced but no longer statistically significant in the adjusted model. The association between length of time since immigration (<5 years) and interbirth interval was also reduced and lost statistical significance in the adjusted model; other categories of length of time since immigration were not associated with the outcome.
| Exposure Variablesa | Adjusted OR and 95% CI |
|---|---|
| Immigration pathway | |
| US-born | 1.00 (Referent) |
| Conflict/insecurity | 0.86 (0.23–3.20) |
| Education | 4.57 (1.57–9.58) |
| Employment | 2.27 (1.07–5.31) |
| Family-based | 0.36 (0.03–3.74) |
| Length of time since immigration | |
| US-born | 1.00 (Referent) |
| ≤5 years | 0.50 (0.23–1.01) |
| 6-10 years | 0.34 (0.03–3.77) |
| >10 years | 0.41 (0.03–4.74) |
| Birthplace | |
| US-born | 1.00 (Referent) |
| Africa | 0.79 (0.02–0.98) |
| Asia | 3.18 (0.27–37.73) |
| Other Western countries | 2.72 (0.21–34.55) |
| South and Central America | 3.40 (0.32–7.07) |
| Caribbean | 1.52 (0.15–15.70) |
4. Discussion
We examined the relationships between immigration-related factors and interbirth interval among women living in the United States. The results revealed that more than a third (37.4%) of births occurred within 18 months of a previous live birth. We also found significant relationships between immigration pathway and place of birth with interbirth intervals, but no relationship between the length of time since immigrating to the United States and outcome.
Our findings contribute to the literature on birth interval not only in the general US populations but also in the country’s immigrant and refugee populations. We found a slightly higher prevalence of short interval births (37%) than the national average of approximately 30%14 and population-based studies that reported interbirth intervals ranging from 11% to 35%.6,14,29 Studies have reported an above-average prevalence of short birth intervals in Black people, including Black immigrants.6,10,37 Because Black women were overrepresented in our sample, this may have contributed to the higher prevalence of short interbirth intervals (≤18 months) observed in the results of the present study.
After adjusting for potential confounders, the association between shorter duration of time since immigration to the United States and interbirth interval lost significance. The length of time since immigration has been linked to health beliefs and behaviors, such as the use of disease management and preventative services for physical, mental, and sexual and reproductive health.23,38-40 The length of stay in the receiving country has been used to asses acculturation and how immigrants change over time as a result of contact with other cultures after immigration.23,41 It has also been linked to immigrants’ initial health advantage, and health deterioration has been linked to longer duration of stay as a result of exposure to social and environmental determinants of health.42 Simbiri et al.23 argue in a study on care seeking that length of stay in the United States was not as important as language proficiency for immigrants accessing HIV prevention and care services. In the present study, nearly 87% of participants reported speaking English predominantly at home. Hence, adjusting the analysis for language spoken predominantly at home could have contributed to the null results we observed. We are not aware of any previous studies that examined associations between length of stay and interbirth interval in the United States. Nevertheless, this result warrants further investigation and confirmation using larger population-based data sets.
Our results revealed that a woman’s place of birth was associated with interbirth interval. Women born in an African country had lower odds of reporting longer interbirth intervals (i.e., 19–35 or ≥36 months) than the unexposed group (i.e., US-born women). Our result indicating shorter interbirth interval among African-born women is consistent with the results of previous studies that reported shorter interpregnancy intervals among African-born women relative to women born in the United States and other parts of the world.10,28 Specifically, Zhang et al.10 found that African-born women had a mean birth-to-pregnancy interval that was about 6.5 and 15.4 months shorter than those of US-born White and Black women, respectively. Similarly, another study in Utah found that African-born women had higher parities and shorter intervals between pregnancies than White women born in the United States.43 The authors suggested that their finding could be due to religious beliefs, cultural preferences for large families, and a lack of access to family planning methods, consistent with the existing literature.23,28,43-46
Women who immigrated to the United States for educational or employment opportunities had significantly longer interbirth intervals than women born in the United States. We are not aware of any previous studies that examined interbirth intervals in people who migrated to the United States for educational or employment opportunities. This result is plausible because student visa policies require good academic standing, which may be hampered by closely spaced pregnancies and the cost of childcare, which may be unaffordable to most international students.47,48 The same argument may be true for women who immigrated for employment opportunities, in which case, closely spaced pregnancies may interfere with employment prospects. Taken together, voluntary immigrants, regardless of immigration pathway, may have greater motivation and self-efficacy to space childbearing in order to avoid jeopardizing their visa status due to the physical, financial, and social implications of pregnancy, birthing, and childcare.48,49
The results also indicated that women who migrated to the United States due to conflict or persecution had no significantly different odds of being in longer interbirth interval categories than women born in the United States. A recent study of Somali and Congolese refugee women found that the lasting influence of cultural identity and birth spacing norms, post-resettlement, contribute to the use of less effective contraceptive methods (e.g., condoms, withdrawal, oral contraceptives, and fertility awareness methods) during the postpartum period.50 Some of these methods, if not used correctly and consistently, may contribute to short interbirth intervals in immigrant and refugee women. However, our results do not support this explanation and warrants further investigation.
4.1. Strengths and Limitations of the Study
A key strength of this study is our ability to recruit foreign-born women from 40 states and the District of Columbia to participate in an online survey. Previous quantitative studies on immigrant and refugee women were typically limited to a single or few states. In addition, previous studies used birth certificate data, which may result in a larger sample size; however, such studies were limited in their ability to adjust for known confounders based on the variables available in the birth certificate data. The use of primary data collected in the present study allowed us to adjust the analysis for multiple factors that are not typically available in birth certificate records and examine the effects of multiple immigration-related exposure variables on interbirth interval. Notably, we were able to examine the association between immigration pathway and interbirth interval. This is a novel finding and contribution to research on birth spacing and pregnancy intervals in the United States.
Despite these strengths, this study has some limitations. Because we used a non-probability sampling method, our results are not generalizable to all immigrant and refugee women in the United States. The final analytic sample was small, limiting the generalizability of our findings. Nonetheless, we found statistically significant associations between the exposures and outcomes. Some of the associations observed may have been stronger in a larger sample of foreign-born women. The measures assessed were based on self-reported data, which may have been influenced by social desirability bias. However, the majority of the survey questions on the outcome and sociodemographic variables were adopted from the PRAMS and NSFG, which are validated and reliable national surveys.31,32
5. Conclusion and Global Health Implications
In this study, we examined the associations between immigration-related factors and interbirth intervals of immigrant and refugee women living in the United States. We found that the prevalence of short interval births was higher in this sample than the national average. The study’s key findings revealed that women who immigrated for educational or employment opportunities had significantly higher odds of reporting longer interbirth intervals than women born in the United States. Our findings contribute to our understanding of the interbirth intervals of immigrant and refugee women in the United States. Because immigration is becoming an increasingly important health determinant,21 the various immigration pathways should be considered when planning and delivering health services to foreign-born women in the United States. Our results also indicated that women born in Africa have shorter interbirth intervals than other women in the sample. Despite rapid growth in African immigration to the United States in recent years, the population has remained underrepresented in health research and services.51,52 As immigration from sub-Saharan Africa to the United States continues, there is a need for more research to understand this population’s SRH needs to provide responsive reproductive health care. While our study provides preliminary insights into immigration-related factors associated with interbirth interval among immigrant and refugee women in the United States, more research focusing on specific immigrant groups who may be at increased risk for short interbirth interval and its associated implications for pregnancy and birth outcomes is needed. Future research should prioritize African-born immigrant and refugee women, as well as recent immigrants.
Acknowledgments:
The authors thank the participants who took part in the survey and provided the data for this study. The authors acknowledge the contributions of Jiana Saigh, MPH/MAC, Lauren Fisher, MPH/MMS student at Arcadia University, and Casey Sawyer, MPH/DPT student at Arcadia University, for their contributions to initial research on the topic and survey development.
Compliance with Ethical Standards
Conflicts of Interest: The authors declare no competing interests.
Financial Disclosure: Dr. Olorunsaiye has received research support from the Society of Family Planning Research Fund during the period of this study.
Funding/Support: There was no funding for this study.
Ethics Approval: The Institutional Review Board of Arcadia University approved the study (21-06-01). All participants provided written informed consent prior to completing the survey.
Disclaimer: None.
References
- Short interpregnancy intervals:an evidence-based guide for clinicians. Obstetrical &Gynecological Survey. 2015;70(7):458-464.
- [Google Scholar]
- World Health Organization 2007
- Interpregnancy intervals in the United States:data from the birth certificate and the national survey of family growth. National Vital Statistics Reports:From the Centers for Disease Control and Prevention, National Center for Health Statistics, National Vital Statistics System. 2015;64(3):1-10.
- [Google Scholar]
- Effect of the interval between pregnancies on perinatal outcomes. N Engl J Med. 1999;340(8):589-94. doi:10.1056/NEJM199902253400801
- [Google Scholar]
- Influence of interpregnancy interval on neonatal morbidity. Am J Obstet Gynecol. 2015;212(3):386.e1-9. doi:10.1016/j.ajog.2014.11.017
- [Google Scholar]
- Short interpregnancy intervals in the United States. Obstet Gynecol. 2013;122(1):64-71. doi:10.1097/AOG.0b013e3182955e58
- [Google Scholar]
- Short interpregnancy intervals and adverse pregnancy outcomes by maternal age in the United States. Ann Epidemiol. 2019;31:38-44. doi:10.1016/j.annepidem.2018.12.002
- [Google Scholar]
- Maternal morbidity and mortality associated with interpregnancy interval:cross sectional study. BMJ. 2000;321(7271):1255-1259. doi:10.1136/bmj.321.7271.1255
- [Google Scholar]
- The association between interpregnancy interval and severe maternal morbidities using revised national birth certificate data:A probabilistic bias analysis. Paediatr Perinat Epidemiol. 2020;34(4):469-480. doi:10.1111/ppe.12560
- [Google Scholar]
- Short birth-to-pregnancy intervals among African-born black women in Washington State. J Matern Fetal Neonatal Med. 2019;32(6):947-953. doi:10.1080/14767058.2017.1395850
- [Google Scholar]
- Short and long interpregnancy intervals:correlates and variations by pregnancy timing among US women. Perspect Sex Reprod Health. 2015;47(1):19-26. doi:10.1363/47e2615
- [Google Scholar]
- Birth intervals and perinatal health:an investigation of three hypotheses. Fam Plann Perspect 1991:62-70.
- [Google Scholar]
- Factors associated with short birth interval in low- and middle-income countries:a systematic review. BMC Pregnancy and Childbirth. 2020;20(1):156. doi:10.1186/s12884-020-2852-z
- [Google Scholar]
- Factors associated with pregnancy intention among women who have experienced a short birth interval:findings from the 2009 to 2011 Mississippi and 2009 Tennessee Pregnancy Risk Assessment Monitoring System. Ann Epidemiol. 2018;28(6):372-376. doi:10.1016/j.annepidem.2018.03.012
- [Google Scholar]
- Short interpregnancy intervals:results from the first baby study. Women's Health Issues. 2017;27(4):426-433. doi:10.1016/j.whi.2017.02.011
- [Google Scholar]
- From public health to public good:Toward universal wellbeing. Scand J Public Health. 2022;50(7):1062-1070. doi:10.1177/14034948221124670
- [Google Scholar]
- A Sense of Priorities for the Healthcare Commons. Am J Prev Med. 2006;31(1):99-102. doi:10.1016/j.amepre.2006.03.010
- [Google Scholar]
- Racial inequities in mortality and access to health care. The untold peril of rationing health care in the United States. J Leg Med. 2011;32(1):77-91. doi:10.1080/01947648.2011.550830
- [Google Scholar]
- Immigrants and health care:sources of vulnerability. Health Aff (Millwood). 2007;26(5):1258-68. doi:10.1377/hlthaff.26.5.1258
- [Google Scholar]
- The sexual and reproductive health of foreign-born women in the United States. Contraception. 2018;98(1):47-51. doi:10.1016/j.contraception.2018.02.003
- [Google Scholar]
- Immigration as a social determinant of health. Annu Rev Public Health. 2015;36:375-92. doi:10.1146/annurev-publhealth-032013-182419
- [Google Scholar]
- “In Africa, there was no family planning. Every year you just give birth”:Family planning knowledge, attitudes, and practices among Somali and Congolese refugee women after resettlement to the United States. Qual Health Res. 2020;30(3):391-408. doi:10.1177/1049732319861381
- [Google Scholar]
- Access impediments to health care and social services between Anglophone and Francophone African immigrants living in Philadelphia with respect to HIV/AIDS. J Immigr Minor Health. 2010;12(4):569-79. doi:10.1007/s10903-009-9229-8
- [Google Scholar]
- 2022. New Analyses on US Immigrant Health Care Access Underscore the Need to Eliminate Discriminatory Policies. https://www.guttmacher.org/report/new-analyses-us-immigrant-health-care-access-underscore-need-eliminate-discriminatory
- Health Coverage For Lawfully Present Immigrants. https://www.healthcare.gov/immigrants/lawfully-present-immigrants/
- Ensuring Human Rights in the Provision of Contraceptive Information and Services:Guidance and Recommendations 2014
- Contraception after delivery and short interpregnancy intervals among women in the United States. Obstet Gynecol. 2015;125(6):1471-1477. doi:10.1097/AOG.0000000000000841
- [Google Scholar]
- Health advantages and disparities in preterm birth among immigrants despite disparate sociodemographic, behavioral, and maternal risk factors in San Diego, California. Matern Child Health J. 2020;24(2):153-164. doi:10.1007/s10995-019-02836-y
- [Google Scholar]
- Prenatal care and subsequent birth intervals. Perspect Sex Reprod Health. 2012;44(1):13-21. doi:10.1363/4401312
- [Google Scholar]
- Validating the demographic, political, psychological, and experimental results obtained from a new source of online survey respondents. Research &Politics. 2019;6(1):2053168018822174.
- [Google Scholar]
- The Pregnancy Risk Assessment Monitoring System (PRAMS):Overview of Design and Methodology. Am J Public Health. 2018;108(10):1305-1313. doi:10.2105/AJPH.2018.304563
- [Google Scholar]
- 2020. National Survey of Family Growth 2017-2019. https://www.cdc.gov/nchs/nsfg/nsfg_2017_2019_puf.htm
- Data and measurement issues in the analysis of health disparities. Health Serv Res. 2010;45(5 Pt 2):1489-507. doi:10.1111/j.1475-6773.2010.01143.x
- [Google Scholar]
- The critical role of racial/ethnic data disaggregation for health equity. Popul Res Policy Rev. 2021;40(1):1-7. doi:10.1007/s11113-020-09631-6
- [Google Scholar]
- A call to focus on racial domination and oppression:A response to “Racial and ethnic inequality in poverty and affluence, 1959–2015.″. Popul Res Policy Rev. 2019;38(5):615-654. doi:10.1007/s11113-019-09512-7
- [Google Scholar]
- US racial and ethnic relations in the twenty-first century. Ethn Racial Stud. 2017;40(13):2181-2209.
- [Google Scholar]
- Effect of interpregnancy interval on infant low birth weight:a retrospective cohort study using the Michigan Maternally Linked Birth Database. Matern Child Health J. 2003;7(3):169-78. doi:10.1023/a:1025184304391
- [Google Scholar]
- Adaptation of an acculturation scale for African refugee women. Journal of Immigrant and Minority Health. 2016;18(1):252-262.
- [Google Scholar]
- Acculturation and Health Behaviors of African Immigrants Living in the United States:An Integrative Review. ABNF Journal. 2016;27(3)
- [Google Scholar]
- The association between acculturation and cardiovascular disease risk in Ghanaian and Nigerian-born African immigrants in the United States:the Afro-Cardiac Study. J Immigr Minor Health. 2016;18(1):252-62. doi:10.1007/s10903-014-9998-6
- [Google Scholar]
- Acculturation:Living successfully in two cultures. Int J Intercult Relat. 2005;29(6):697-712. https://doi.org/10.1016/j.ijintrel.2005.07.013
- [Google Scholar]
- The effects of years lived in the United States on the general health status of California's foreign-born populations. J Immigr Minor Health. 2007;9(2):125-36. doi:10.1007/s10903-006-9017-7
- [Google Scholar]
- A Study of Pregnancy and Birth Outcomes among African-Born Women Living in Utah. Migration Policy Institute 2016
- [Google Scholar]
- Reproductive health outcomes in African refugee women:a comparative study. J Womens Health (Larchmt). 2019;28(6):785-793. doi:10.1089/jwh.2018.7314
- [Google Scholar]
- Reproductive health decision-making among US-dwelling Somali Bantu refugee women:A qualitative study. J Clin Nurs. 2018;27(17-18):3355-3362. doi:10.1111/jocn.14162
- [Google Scholar]
- Factors associated with access to maternal and reproductive health care among Somali refugee women resettled in Ohio, United States:a cross-sectional survey. J Immigr Minor Health. 2019;21(5):946-953. doi:10.1007/s10903-018-0824-4
- [Google Scholar]
- Different Worlds, Mutual Expectations:African Graduate Student Mothers and the Burden of US Higher Education. Journal of Education and Learning. 2013;2(2):201-209. doi:10.5539/jel.v2n2p201
- [Google Scholar]
- “Finally, I told my professor I was pregnant.”Becoming new mothers as international graduate students. Linguistics and Education. 2021;63:100922.
- [Google Scholar]
- Parenting on the path to the professoriate:A focus on graduate student mothers. Research in Higher Education. 2020;61(3):408-429.
- [Google Scholar]
- “In Africa, there was no family planning. Every year you just give birth”:family planning knowledge, attitudes, and practices among Somali and Congolese refugee women after resettlement to the United States. Qual Health Res. 2020;30(3):391-408. doi:10.1177/1049732319861381
- [Google Scholar]
- Family planning research in African immigrant and refugee women:a scoping review. J Transcult Nurs. 2022;33(3):416-426. doi:10.1177/10436596211072891
- [Google Scholar]





