Translate this page into:
Acceptability of HIV Screening in a Sample of International Students in the United States
#x002A;Corresponding author email: oluwasola.ayosanmi@mail.mcgill.ca
-
Received: ,
Accepted: ,
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Background and Objectives:
HIV transmission from persons unaware of their HIV status occurs more commonly than those who are aware of their status. Knowledge of one’s HIV status may encourage preventive behaviors. Anecdotal evidence suggests that many international students may be willing to accept HIV screening, but empirical evidence to support this claim is lacking. We sought to determine the willingness of international students in the United States (US) to accept HIV screening, if offered.
Methods:
We conducted a cross-sectional study using an online survey of international students at Western Illinois University, USA. The independent variable was the sociodemographic data of our participants; the dependent variable was the acceptance of HIV screening. The covariates were knowledge about HIV and the factors associated with the acceptance of the screening. Descriptive statistics and multivariate analysis were conducted.
Results:
A total of 185 respondents out of 491 students participated in the online survey. Of these, 107 (57.8%) were males, and 78 (42.8%) were females. Most of the respondents were from Asian countries (64.9%) and African countries (24.9%). The prevalence of acceptance of HIV screening was 74%. Among participants willing to accept screening, if offered, 90% perceived screening would be beneficial to their health. Meanwhile, 83% of those who would refuse the screening were not sexually active.
Conclusion and Global Health Implications:
Many international students may be interested in getting HIV screening if offered. Awareness of the benefits of HIV screening may influence the decision to screen. Findings may inform further studies that will lead to policy formulations for the health of international students in the US.
Keywords
HIV Screening
HIV Acceptability
International Students
College Students
1. Introduction
In the United States, an estimated 1.2 million people had the human immunodeficiency virus (HIV), the virus that causes AIDS, at the end of 2018, the most recent year for which this information is available. Of those people, about 14%, or 1 in 7, did not know they had HIV.1 Roughly 38,700 new HIV infections occurred in the U.S. in 2016.2 Undiagnosed HIV positive people transmit 30 % of these infections.1 Moreover, these HIV infections limit the effectiveness of HIV programs because testing is the entry point for HIV care and treatment.3,4 Early diagnosis of HIV is important because it helps people living with HIV to access prompt treatment and care as well as prevent progression to AIDS.
Additionally, the United States Preventive Services Task Force (USPSTF) acknowledged that primary prevention or avoidance of exposure to HIV infection was the most critical strategy to mitigate HIV-related morbidity and mortality in the U.S.5 The USPSTF, thus, recommended high-intensity behavioral counseling to persons at risk of HIV and other sexually transmitted diseases, including behavioral counseling focusing on individual attitudes, beliefs and self-efficacy.5 The recommendation targeted at-risk populations such as men who have sex with men, active injection drug users, pregnant women and those infected with other sexually transmitted infections. However, there seems not to be any consideration for the college students (domestic and foreign students), who have tendencies for risky sexual behaviors. Although a study was conducted among college students in the U.S. examing factors that determine their uptake of voluntary HIV testing and counseling,6 the perception of international students were either not considered or unreported.
The number of international students in the U.S. has been increasing recently with over a million international students, and most of them were from countries in Asia.7 Over 11,000 international students came from Sub-Saharan Africa.7 Although there is considerable variation in the burden of HIV among countries and regions, Sub-Saharan Africa remains most severely affected as shown in the World Health Organization (WHO) 2016 data map (Figure 1).8

- HIV prevalence among adults by WHO region
Furthermore, since there is no routine screening of international students for HIV at the point of admission into U.S. institutions, identification of people at risk among this population is difficult. It may be expected that the high-risk individuals among international students may opt for screening, the stigmatization associated with HIV screening may prevent them from accepting the screening.9 The purpose of the study was to determine the acceptability of HIV screening among international students and the predicting factors. Specifically, the study aimed to reveal the proportion of international students with high HIV screening acceptability and why. We hypothesized that there would be a high-knowledge driven HIV screening acceptability among the international students.
2. Methods
The study was conducted during the spring semester of 2017 for three months’ duration. We conducted a pilot test among 10% of the expected sample size (18 students). Responses from the pilot test were added to the overall data. The responses of the 18 students confirmed the clarity of the survey content (content validity) and reliability of the instrument. The sample size was calculated using the Kish Leslie formula.10 We calculated a sample size of 174 approximated to 180 participants using a power calculation based on an expected prevalence of 13% for HIV screening acceptance10 at a confidence interval of 95%.11 A detailed description of our data collection and the survey procedure had been previously described.11 Survey Monkey application was used to enhance easy access and responses to the questions.8 At the time of the study, there were 491 international students enrolled at Western Illinois University.2 They comprised of males and females aged between 15 and 35 years with younger students in the undergraduate programs and older students in the graduate programs. Participants were selected by convenience sampling. Participants were eligible if they were international students enrolled at the institution and signed the written informed consent to participate in the study. The survey response rate was 38% (185/491).
2.1. Study Variables
The questionnaire consisted of three-sections with 25-item responses selected from a drop-down list menu. The first section consisted of the independent variables, which are the sociodemographic information of the respondents. The dependent variable was the acceptance of HIV screening, while the covariates were the knowledge about HIV and factors influencing the acceptance. These variables were collected in the second, third and fourth sections of the survey.
2.2. Statistical Analysis
Data were analyzed using the Statistical Package for Social Sciences (SPSS) version 24.12 The baseline characteristics of the respondents were analyzed in a spreadsheet using a simple proportion of respondents. A chi-square test was used to explore associations between demographic characteristics, perceived knowledge, and acceptance of HIV testing. Logistic regression analysis was used to determine associations of the dependent variable (acceptance of HIV screening) with the independent variables. All levels of significance were set at p < 0.05. The results were presented with tables and a bar chart. Ethical approval was obtained from the Institutional Review Board (IRB) of Western Illinois University.
3. Result
3.1. Sociodemographic Characteristics
A total of 185 respondents participated in the online survey, which was 38% (185/491) response rate. The general knowledge of HIV infection was rated from very high to very low. About one-third of the respondents have very high general knowledge. Almost 60% of the respondents have high knowledge, while a majority of the study population would accept HIV screening if offered; they said they would do so because they know it is beneficial to their health.
3.2. Perceived Knowledge of HIV and HIV Screening
There were 107 (57.8%) males and 78 (42.8%) females. A hundred and seventy-nine respondents (97%) were aged between 15 and 34 years, while 100 (54.1%) respondents were aged between 25 and 34 years. 149 (80.5%) and 28 (15.1%) respondents were full-time graduate and undergraduate students, respectively. Most of the respondents were single and never-married (73.0%), and 94 (50.8%) of them were not sexually active. Most of the respondents were from Asia (64.9%) and Africa (24.9%). One-third (33.5%) of the respondents were international students from India, while 17.3% were from Nigeria, (Table 1).
| Sociodemographic variables | Frequency (N) | Percentage (%) | |
|---|---|---|---|
| Gender | Female | 79 | 42.7 |
| Male | 107 | 57.8 | |
| Age (Years) | 15 to 24 | 79 | 42.7 |
| 25 to 34 | 100 | 54.1 | |
| 35 to 44 | 5 | 2.7 | |
| 45 to 54 | 1 | .5 | |
| 55 or older | |||
| Graduate international student attendance status | Full time | 149 | 80.5 |
| Part-time | 5 | 2.7 | |
| Undergraduate international student attendance status | Full time | 28 | 15.1 |
| Part time | 1 | .5 | |
| Employment status | Employed, Graduate assistant | 54 | 29.2 |
| Employed, student worker | 59 | 31.9 | |
| Employed both Graduate assistant and student worker | 4 | 2.2 | |
| Not employed with the University but works within U.S. with another organization | 6 | 3.2 | |
| Not employed at all | 60 | 32.4 | |
| Sexually active | Yes | 88 | 47.6 |
| No | 94 | 50.8 | |
| Marital status | Married | 40 | 21.6 |
| Divorced | 1 | .5 | |
| In a domestic partnership or civil union | 3 | 1.6 | |
| Single, but cohabiting with a significant other | 5 | 2.7 | |
| Single, never married | 135 | 73.0 | |
| Continent of origin | Africa | 46 | 24.9 |
| Asia | 120 | 64.9 | |
| Australia | 1 | .5 | |
| Europe | 10 | 5.4 | |
| North America | 4 | 2.2 | |
| South America | 2 | 1.1 | |
| Academic departments | Natural Sciences | 33 | 17.8 |
| Social sciences | 10 | 5.4 | |
| Business | 24 | 13.0 | |
| Education | 15 | 8.1 | |
| Health Sciences | 21 | 11.4 | |
| Art | 3 | 1.6 | |
| Other | 77 | 41.6 |
The perceived knowledge about HIV was generally high among the respondents. Almost a third of the respondents have a very high perceived general knowledge about while 55% have high knowledge (Table 2).
| Perceived General Knowledge about HIV | Rating | Frequency (N) | Percentage (%) |
|---|---|---|---|
| How would you rate your perceived general knowledge of HIV and HIV screening | Very high | 59 | 32 |
| High | 102 | 55 | |
| Low | 10 | 5 | |
| Very low | 4 | 2 | |
| None | 3 | 1.6 |
Respondents expressed an impressive perceived knowledge about specific aspects of HIV screening (Table 3). Ninety-three percent of the respondents perceived that they know the mode of HIV transmission; 77% know about the use of screening for HIV diagnosis; 80% know that HIV infection can be prevented; 91% know about some possible complications of the infection. HIV screening was acknowledged as a preventive measure by 63% (117) of the respondents. Almost 80% (78.9%) of the respondents knew that screening is beneficial to them by helping them know their HIV status and helpful to their community. Many of the respondents (83.2%) knew that screening could be done by blood collection from their veins. Over two-third (67%) of the respondents knew that HIV screening is voluntary. Respondents from Asia and Africa region have more knowledge than people from other regions of the world (Figure 2).
| Specific aspects of HIV screening | Frequency (N) | Percentage (%) | |
|---|---|---|---|
| HIV is preventable | Yes | 148 | 80.0 |
| No | 19 | 10.3 | |
| Others | 13 | 7.0 | |
| HIV Infections are acquired through unprotected sexual intercourse, blood transfusion and needle-prick injuries | Yes | 172 | 93.0 |
| No | 4 | 2.2 | |
| Others | 4 | 2.2 | |
| HIV infections are diagnosed through the screening | Yes | 143 | 77.3 |
| No | 19 | 10.3 | |
| Others | 17 | 9.2 | |
| HIV screening is a voluntary test done after counselling and results are highly confidential | Yes | 136 | 73.5 |
| No | 23 | 12.4 | |
| Others | 20 | 10.8 | |
| Screening for HIV infection is one of the methods for preventing HIV transmission | Yes | 117 | 63.2 |
| No | 41 | 22.2 | |
| Others | 21 | 11.4 | |
| Screening for HIV infections will help people to know their HIV status | Yes | 146 | 78.9 |
| No | 16 | 8.6 | |
| Others | 16 | 8.6 | |
| Screening for HIV could be done by collecting a blood sample from you | Yes | 154 | 83.2 |
| No | 14 | 7.6 | |
| Others | 10 | 5.4 | |
| HIV screening is meant for everybody that wants to prevent HIV infection transmission, and it is done voluntarily after initial counseling | Yes | 124 | 67.0 |
| No | 31 | 16.8 | |
| Others | 23 | 12.4 | |
| Knowledge of HIV status after a screening is beneficial to an individual’s health and the general community | Yes | 148 | 80.0 |
| No | 15 | 8.1 | |
| Others | 14 | 7.6 | |
| There are HIV positive people who do not know their HIV status and they are more likely to infect others than those who already know their status | Yes | 143 | 77.3 |
| No | 22 | 11.9 | |
| Others | 14 | 7.6 |
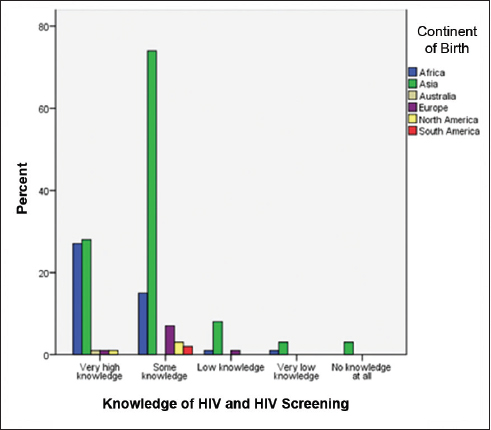
- Assessment of general knowledge of HIV by continents
3.3. HIV Screening Acceptability
One hundred and seventy-three respondents (74%) were willing to accept HIV screening if offered. Thus, the prevalence of HIV screening acceptability among the study population is 74%. Nonetheless, most HIV screening acceptability were from students born in Asia and Africa (Figure 3).
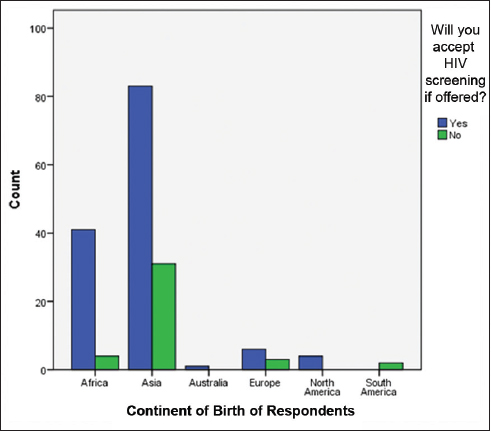
- Acceptance of HIV screening and continent of origin of the respondents
3.4. Reasons for HIV Screening Acceptability
Ninety percent (90%) of the respondents with high HIV screening acceptability perceived the screening as beneficial to their health while offering the test would encourage acceptability in 76%. The majority (83%) of those who reported that they would refuse HIV screening were not sexually active, and they do not think they can be susceptible to HIV infection.
3.5. Association Between Knowledge of HIV and Acceptability of the Screening
Among respondents with very high perceived knowledge of HIV, 78% would accept HIV screening while 22% would not. Among those with some knowledge of HIV, 78% would accept HIV screening while 22% would not. Among those with low knowledge of HIV, 70% would accept HIV screening while 30% would not. Among those with no knowledge about HIV, 67% would accept HIV screening if offered. The Pearson residual correlation shows a weak negative correlation between the level of knowledge and acceptability of HIV screening. A multivariate analysis of the association between the general knowledge of HIV and the acceptance of HIV screening shows no statistical significance (Table 4).
| Knowledge | Acceptability | Frequency | Pearson residual | Percentages | ||
|---|---|---|---|---|---|---|
| Observed | Predicted | Observed | Predicted | |||
| Very high | Yes | 46 | 47.2 | -0.38 | 78% | 80% |
| No | 13 | 11.8 | 0.38 | 22% | 20% | |
| Some knowledge | Yes | 79 | 76.8 | 0.52 | 78.2% | 76% |
| No | 22 | 24.2 | -0.52 | 21.8% | 24% | |
| Low knowledge | Yes | 7 | 7.2 | -0.11 | 70% | 71.6% |
| No | 3 | 2.8 | 0.11 | 30% | 28.4% | |
| Very low knowledge | Yes | 1 | 2.7 | -1.77 | 25% | 66.7% |
| No | 3 | 1.33 | 1.77 | 75% | 33.3% | |
| No knowledge at all | Yes | 2 | 1.2 | 1.12 | 100% | 61.4% |
| No | 0 | 0.8 | 1.12 | 0% | 38.6% | |
*The percentages are based on total observed frequencies in each subpopulation
4. Discussion
To our knowledge, our study is the first in the U.S. to determine the acceptability of HIV screening among international students. We observed that most of the international students who perceived that they have some knowledge of HIV came from Asian and African continents, where there is a high HIV prevalence. A previous study remarked that knowledge and awareness of HIV screening are high among the respondents from regions with high HIV prevalence.13 High knowledge likely implies more awareness about HIV among international students from high HIV prevalence countries. However, there is no statistically significant association between the continent of origin and the knowledge of HIV screening. The lack of statistical significance is likely because of the small sample size and predominance of the respondents by students from Asia and Africa, hence a skewed bar-graph (Figure 3). A future study with higher sample size may clarify if any association exists.
Moreover, we observed high acceptability of HIV screening among our respondents. Almost three-quarters of the study population accepted HIV screening, and this finding contrasted with the findings of Enosolease and Offor 10 that showed a low HIV screening acceptance rate (13%) despite good awareness of HIV/AIDS. This contrast might be because our participants were international students in a developed country as opposed to women seeking induced abortion in a developing country. Nevertheless, we could not establish a statistically significant association between the level of knowledge of the responders and the observed high acceptability. The willingness to accept HIV screening if offered, was high among our participants irrespective of their level of knowledge about HIV. Similarly, there was no statistical correlation between the screening acceptance and the country or region of origin of the participants. The lack of statistical significance may be because of insufficient statistical power from our small sample size. Since a previous study among 1200 students reported a statistically significant association between level of knowledge and voluntary testing of HIV,9 an increase in our study sample size may generate a significant finding.
Moreover, the primary reasons for the observed high HIV screening acceptability were the perceived benefit of the screening and the availability of the test. Perceived benefit is a construct of Health Belief Model that has been described to be associated with HIV screening acceptance.6,11 Nonetheless, those who said they would refuse the HIV screening if offered were not sexually active, and they did not perceive any benefit in the test.
Although a cross-sectional survey earlier reported stigmatization as a barrier to HIV screening, lack of sexual activity was the most significant reason for refusing HIV screening in our population.9 The observed unwillingness to be screened for HIV among those not sexually active reinforces the 2013 recommendation of the USPSTF. The USPSTF was against screening those who are not sexually active because HIV infection is transmitted mostly sexually.5
4.1. Limitations
A significant limitation of this study is the small sample size. Since this study is about international students, it is challenging to have all continents evenly distributed. Hence, a large sample size would be required to generate a statistical power for significant associations. The international students in our study setting are relatively few, and that also reflected on the difficulties faced in using a random sampling method, hence the convenience sampling. However, we anticipate that this report will inform the decisions of researchers to conduct a more robust study in larger institutions or a multi-center study. Due to the sampling limitation as mentioned above, we were unable to generate statistical power for our logistic regression analysis. We, therefore, deem it fit to report this finding to stimulate interest in this area of research. Further studies should give consideration to HIV screening among international students attending the U.S. colleges because such screening could enhance health promotion.
5. Conclusion and Global Health Implications
HIV screening continues to be an effective preventive strategy for HIV transmission. There is an increase in the awareness of HIV and HIV screening among international students from continents with high HIV prevalence, but further study may be needed to affirm if this translates to high knowledge of HIV screening. Our findings may inform the decision of researchers to conduct a more robust study that will lead to policy formulations for international studies in the United States.
Acknowledgements:
The lead author acknowledges the support of the graduate students at Western Illinois University during the 2017/2018 session while collecting the data for this study. The support of the Center for International Students at Western Illinois University is immensely appreciated.
Compliance with Ethical Standards
Conflicts of Interest: No conflicts of interest. Financial Disclosure: None of the authors received any form of financial benefit from this project.
Funding/Support: The publication of this article was partially supported by the Global Health and Education Projects, Inc. (GHEP) through the Emerging Scholars Grant Program (ESGP). The information, contents, and conclusions are those of the authors’ and should not be construed as the official position or policy of, nor should any endorsements be inferred by ESGP or GHEP
References
- Division of HIV/AIDS Prevention, National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention. HIV Basics Statistics. https: //www.cdc.gov/hiv/basics/statistics.html
- [Google Scholar]
- U.S. Statistics:Fast Facts. https: //www.hiv.gov/hiv-basics/overview/data-and-trends/statistics
- The spectrum of engagement in HIV care and its relevance to test-and-treat strategies for prevention of HIV infection. Clin Infect Dis. 2011;52(6):793-800.
- [Google Scholar]
- Optimizing the engagement of care cascade:a critical step to maximize the impact of HIV treatment as prevention. Curr Opin HIV AIDS. 2012;7(6):579-586.
- [Google Scholar]
- Screening for HIV:US preventive services task force recommendation statement. Ann Intern Med. 2013;159(1):51-60.
- [Google Scholar]
- Determinants of voluntary HIV/AIDS counseling and testing among community college students in the United States. Int J MCH AIDS. 2017;6(2):109.
- [Google Scholar]
- Fact Sheets and Infographics. https: //www.iie.org/Research-and-Insights/Open-Doors/Fact-Sheets-and-Infographics
- Map HIV Adult Prevalence. International HIV Data Web site. who.int/images/default-source/maps/hiv_adult_prevalence_2016. Published in 2020
- [Google Scholar]
- Knowledge of HIV/AIDS and predictors of uptake of HIV counselling and testing among undergraduate students of a privately owned university in Nigeria. BMC Research Notes. 2014;7(1):639.
- [Google Scholar]
- The Role of Health Belief Model in HIV Screening Decision among International Students in the United States: A Pilot Study. Int. J. Transl Med Res Public Health. 2020;4(1):4-12.
- [Google Scholar]
- Released 2016. In: IBM SPSS Statistics for Windows, Version 24.0. Armonk. NY: IBM Corp;
- [Google Scholar]
- Attitudes to HIV and HIV testing in high prevalence areas of China:informing the introduction of voluntary counselling and testing programmes. Sex Transm Infect. 2005;81(2):108-112.
- [Google Scholar]





